Blood glucose levels, also known as blood sugar levels, refer to the concentration of glucose present in the blood. Glucose is a crucial metabolic substrate that provides energy for tissue function and is tightly regulated by various hormones, including insulin, glucagon, and cortisol, to maintain homeostasis. Normal fasting blood glucose levels are typically defined as less than 100 mg/dL (5.55 mmol/L). After eating, blood glucose levels rise as the body breaks down food into glucose, which is then used for energy or stored for later use. Maintaining blood glucose within a normal range is essential for overall health, as deviations can lead to conditions such as hypoglycemia or hyperglycemia, and long-term imbalances are associated with diabetes and its complications. Monitoring and managing blood glucose levels are critical for individuals with diabetes to prevent complications and maintain metabolic control.
How blood glucose is produced and utilized in the body
Blood glucose is produced and utilized in the body through a complex interplay of various organs and regulatory mechanisms. The liver plays a central role in glucose production by balancing glycogenesis (storage of glucose as glycogen) and gluconeogenesis (production of glucose from non-carbohydrate sources). During fasting, the liver releases glucose into the bloodstream to maintain blood glucose levels, primarily through glycogenolysis and gluconeogenesis. In the postprandial state, increased insulin levels promote glucose uptake and storage in muscle and adipose tissues, while inhibiting hepatic glucose production. Glucose utilization is facilitated by specific glucose transporters present on cell membranes, which allow glucose to enter cells where it is used for energy production1. Hyperglycemia can stimulate glucose utilization and suppress glucose production, while conditions like diabetes can lead to dysregulation of these processes, resulting in either excessive glucose production or impaired glucose utilization.
The role of insulin in regulating blood glucose levels
Insulin is a crucial polypeptide hormone secreted by the β cells in the islets of Langerhans of the pancreas, playing a vital role in regulating blood glucose levels. It works in tandem with glucagon, where insulin promotes anabolic processes and glucagon supports catabolic functions. Insulin facilitates the uptake of glucose into cells, particularly in the liver, muscles, and adipose tissue, thereby reducing blood glucose levels and promoting glucose storage. This regulation is essential for maintaining glucose homeostasis, especially postprandially, where insulin ensures that excess glucose is stored and not left circulating in the bloodstream. Insulin’s action is mediated through its receptor, which triggers a cascade of intracellular signaling pathways that modulate various metabolic processes, including glucose, protein, and lipid metabolism. Dysregulation of insulin signaling can lead to insulin resistance, a hallmark of type 2 diabetes, where tissues become less responsive to insulin, resulting in elevated blood glucose levels and associated metabolic disorders. Understanding the molecular mechanisms of insulin action and its signaling pathways is critical for developing therapeutic strategies to manage diabetes and other insulin-resistant conditions.
Normal vs. Abnormal Blood Glucose Levels
Understanding the difference between normal and abnormal blood glucose levels is crucial for maintaining overall health and preventing chronic conditions like diabetes. Blood glucose levels fluctuate throughout the day, influenced by factors such as diet, exercise, and stress. Here are the key distinctions between normal and abnormal blood glucose levels:
1. Normal Blood Glucose Range
Normal blood glucose levels are essential for maintaining overall health and preventing complications associated with diabetes. For individuals without diabetes, the typical blood glucose range is between 70-100 mg/dL when fasting and less than 140 mg/dL two hours after eating. For those with diabetes, the target range is slightly broader, generally between 70-180 mg/dL, to account for the challenges in maintaining strict control. Keeping blood glucose within this range helps to avoid both short-term and long-term health issues, such as hypoglycemia and hyperglycemia, respectively. Regular monitoring and appropriate management strategies are crucial for maintaining these levels.
2. High Blood Glucose (Hyperglycemia)
Hyperglycemia, or high blood glucose, occurs when there is insufficient insulin in the body or when the body cannot effectively use the insulin it produces. This condition is common in individuals with diabetes, particularly when they fail to administer enough insulin or when their diet includes excessive carbohydrates. Other contributing factors include stress, illness, and lack of physical activity, which can all elevate blood glucose levels. In some cases, medications that affect insulin sensitivity or glucose metabolism can also lead to hyperglycemia. The symptoms of hyperglycemia can develop gradually and may include increased thirst, frequent urination, fatigue, and blurred vision. If left untreated, hyperglycemia can lead to more severe complications such as diabetic retinopathy, neuropathy, and nephropathy, which affect the eyes, nerves, and kidneys, respectively. In extreme cases, it can result in diabetic ketoacidosis, a life-threatening condition characterized by high levels of ketones in the blood. Therefore, recognizing and managing the symptoms early is crucial to prevent long-term damage.
3. Low Blood Glucose (Hypoglycemia)
Hypoglycemia, or low blood glucose, typically occurs when blood glucose levels drop below 70 mg/dL. This can happen if an individual skips a meal, consumes less food than usual, or engages in more physical activity than normal without adjusting their insulin dosage accordingly. Over-administration of insulin or other glucose-lowering medications can also precipitate hypoglycemia. It is essential for individuals, especially those with diabetes, to understand their personal triggers and manage their diet and medication to prevent episodes of low blood glucose. The symptoms of hypoglycemia can appear suddenly and vary from person to person. Common signs include shakiness, sweating, confusion, and drowsiness. In severe cases, hypoglycemia can lead to loss of consciousness or seizures if not promptly treated. Recognizing these symptoms early and taking immediate action, such as consuming fast-acting carbohydrates, can help restore normal blood glucose levels and prevent serious complications. Regular monitoring and personalized management plans are vital for individuals prone to hypoglycemia.
Factors Affecting Blood Glucose Levels
Blood glucose levels are influenced by a variety of factors that can either stabilize or disrupt this delicate balance. Understanding these factors is essential for effective blood sugar management and overall health. Below are the primary factors that can affect blood glucose levels:
1. Carbohydrates and Sugar Intake
Carbohydrates are a primary factor influencing blood glucose levels. The ingestion of carbohydrate-rich foods tends to raise blood glucose levels due to their rapid conversion into glucose during digestion. Studies have shown that higher carbohydrate intake is associated with increased glycemic variability and less time-in-range for blood glucose levels, particularly in individuals at high risk for diabetes. In women with gestational diabetes mellitus, a high-carbohydrate morning intake resulted in higher glycemic variability compared to a low-carbohydrate morning intake. Additionally, a high-protein, low-carbohydrate diet has been shown to significantly reduce blood glucose levels in people with type 2 diabetes, suggesting that carbohydrate intake should be carefully managed to maintain optimal blood glucose control.
2. Physical Activity and Exercise
Physical activity plays a crucial role in regulating blood glucose levels. Exercise increases glucose uptake by muscles, thereby lowering blood glucose levels. Moderate- to vigorous-intensity physical activity has been associated with reduced glycemic variability and better blood glucose control in individuals at high risk for diabetes. Additionally, prolonged exercise can lead to significant declines in glucose and insulin levels, although carbohydrate feeding during exercise can mitigate these effects. The impact of exercise on blood glucose can vary based on factors such as age, sex, and fitness level, indicating the need for personalized exercise recommendations for effective blood glucose management.
3. Stress and Emotional Factors
Stress and emotional factors can significantly impact blood glucose levels. Stressful life situations can lead to the release of hormones such as epinephrine and cortisol, which increase blood glucose levels as part of the body’s adaptive response. Physical stresses like infections and trauma also affect blood glucose regulation by triggering hormonal changes. Experimental evidence has shown that hyperglycemia can be induced in diabetic individuals during stressful events, highlighting the importance of stress management in maintaining stable blood glucose levels. Therefore, both psychological and physical stressors need to be considered in the management of blood glucose.
4. Common Medications that Impact Glucose
Several medications can influence blood glucose levels, either by increasing or decreasing them. Insulin and oral hypoglycemic agents are commonly used to lower blood glucose levels in diabetic patients. However, other medications, such as corticosteroids, can raise blood glucose levels by promoting gluconeogenesis and reducing insulin sensitivity. Additionally, the use of certain medications for other health conditions, such as beta-blockers and diuretics, can also impact blood glucose regulation. Therefore, it is essential to monitor blood glucose levels closely when taking medications that may affect glucose metabolism.
5. Health Conditions Affecting Blood Glucose
Various health conditions can affect blood glucose levels. Diabetes mellitus is the most well-known condition, characterized by chronic hyperglycemia due to insulin deficiency or resistance. Other conditions, such as infections, trauma, and hormonal disorders, can also impact blood glucose regulation. For instance, conditions that affect the endocrine system, such as Cushing’s syndrome or hyperthyroidism, can lead to elevated blood glucose levels. Additionally, the presence of comorbidities like obesity and cardiovascular disease can complicate blood glucose management, necessitating a comprehensive approach to treatment. Understanding the interplay between different health conditions and blood glucose levels is crucial for effective management and prevention of complications.
Monitoring Blood Glucose Levels
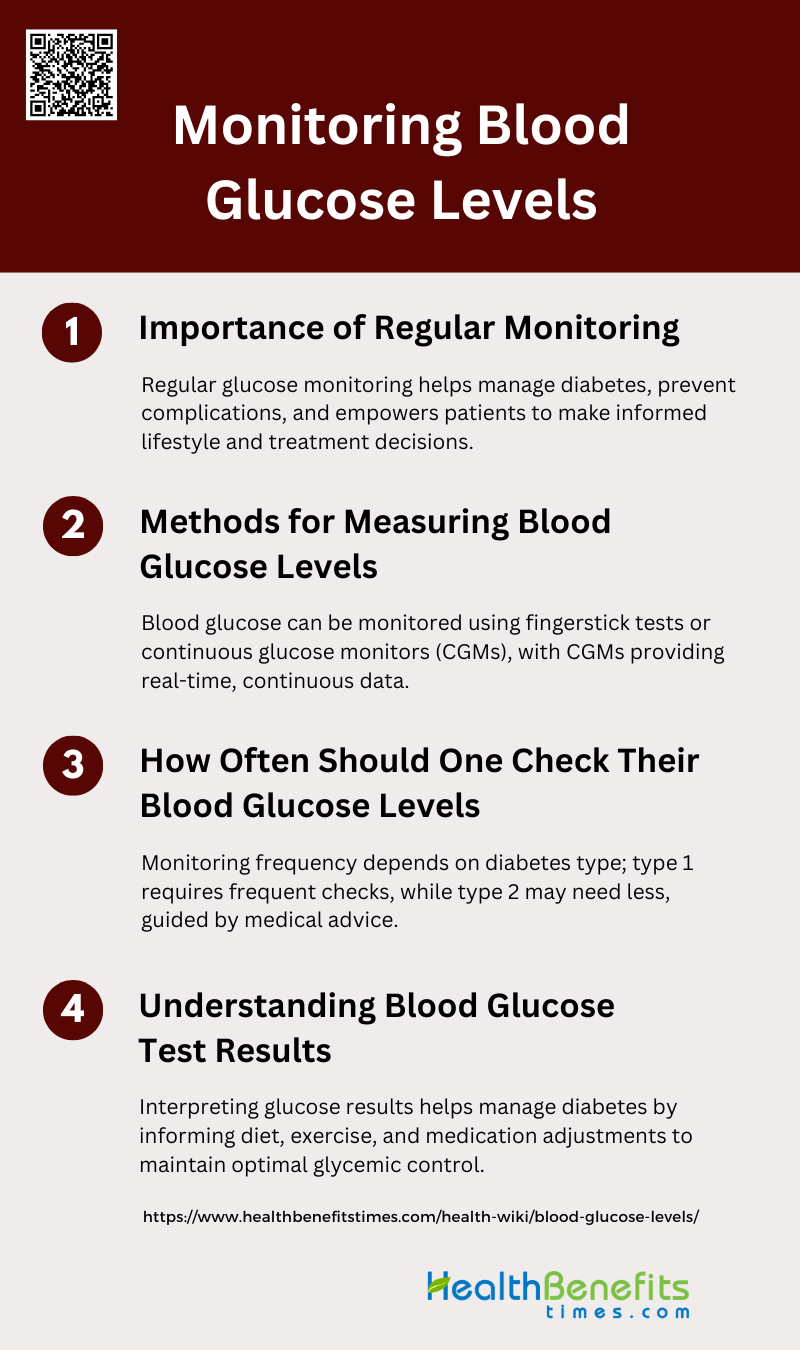
Regular monitoring of blood glucose levels is vital for managing diabetes and maintaining optimal health. It helps individuals understand how different factors impact their blood sugar and make informed decisions about their lifestyle and treatment. Here are the key methods for monitoring blood glucose levels:
1. Importance of Regular Monitoring
Regular monitoring of blood glucose levels is crucial for managing diabetes effectively. It helps in maintaining glycemic control, which is essential to prevent both microvascular and macrovascular complications associated with diabetes. Continuous glucose monitoring (CGM) systems provide real-time data, allowing for better management of blood glucose levels and reducing the risk of hypoglycemia and hyperglycemia. Regular monitoring also empowers patients to make informed decisions about their diet, exercise, and medication, thereby improving their overall quality of life. Moreover, it aids healthcare providers in tailoring treatment plans to individual needs, enhancing patient outcomes.
2. Methods for Measuring Blood Glucose Levels
There are primarily two methods for measuring blood glucose levels: fingerstick tests and continuous glucose monitors (CGMs). Fingerstick tests involve pricking the finger to obtain a blood sample, which is then analyzed using a glucose meter. This method has been the standard for decades and is widely used due to its simplicity and reliability. On the other hand, CGMs use a sensor inserted under the skin to continuously measure glucose levels in the interstitial fluid. CGMs provide real-time data and can alert users to high or low blood glucose levels, offering a more comprehensive picture of glucose trends. Emerging non-invasive methods, such as touch-based fingertip sensors, are also being explored for their potential to simplify glucose monitoring further.
3. How Often Should One Check Their Blood Glucose Levels
The frequency of blood glucose monitoring depends on the type of diabetes and the treatment regimen. For individuals with type 1 diabetes, the American Diabetes Association (ADA) recommends self-monitoring of blood glucose (SMBG) at least three to four times daily. For those with type 2 diabetes who are not on insulin, monitoring may be less frequent, typically once a day or as advised by a healthcare provider. Continuous glucose monitors (CGMs) offer the advantage of providing continuous data, which can be particularly beneficial for those requiring intensive glucose management. Regular monitoring is essential for adjusting treatment plans and maintaining optimal glycemic control.
4. Understanding Blood Glucose Test Results
Interpreting blood glucose test results is vital for effective diabetes management. Blood glucose levels are typically measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Normal fasting blood glucose levels range from 70 to 100 mg/dL (3.9 to 5.6 mmol/L), while postprandial (after meal) levels should be below 140 mg/dL (7.8 mmol/L). Continuous glucose monitoring (CGM) systems provide additional insights into glucose trends and variability, helping to identify patterns such as nocturnal hypoglycemia or postprandial hyperglycemia. Understanding these results allows patients and healthcare providers to make informed decisions about diet, exercise, and medication adjustments, ultimately improving glycemic control and reducing the risk of complications.
Importance of Maintaining Healthy Blood Glucose Levels
Maintaining healthy blood glucose levels is essential for preventing chronic diseases and ensuring overall well-being. Proper blood sugar control can reduce the risk of complications such as heart disease, nerve damage, and vision problems. Here are the key reasons why it’s important to keep blood glucose levels in check:
1. Short-term and Long-term Health Impacts of High and Low Blood Glucose Levels
High blood glucose levels (hyperglycemia) can lead to long-term complications such as diabetic retinopathy, neuropathy, and nephropathy, which are significant causes of morbidity and mortality in diabetic patients. Short-term impacts of hyperglycemia include symptoms like frequent urination, increased thirst, and fatigue. On the other hand, low blood glucose levels (hypoglycemia) can cause immediate and severe symptoms such as drowsiness, shakiness, confusion, and even loss of consciousness or seizures. Both conditions require careful management to avoid these adverse health outcomes.
2. Risks Associated with Uncontrolled Blood Glucose Levels, Including Diabetes
Uncontrolled blood glucose levels are a major risk factor for the development of diabetes-related complications. High glucose concentrations can lead to damage to blood vessels, heart disease, blindness, stroke, and kidney failure. Additionally, poorly controlled diabetes can result in glycemic swings, which are particularly harmful as they can induce nitrosative stress and impair endothelial function, further exacerbating cardiovascular risks. Therefore, maintaining controlled blood glucose levels is crucial to mitigate these risks and prevent the progression of diabetes-related complications.
3. Benefits of Maintaining Stable Blood Glucose Levels
Maintaining stable blood glucose levels has numerous benefits, including the reduction of long-term complications associated with diabetes. Intensive blood glucose control has been shown to delay the onset and slow the progression of diabetic retinopathy, nephropathy, and neuropathy. Stable blood glucose levels also help in reducing the risk of cardiovascular diseases and improve overall quality of life. Furthermore, a well-managed blood glucose level can prevent the occurrence of severe hypoglycemia and hyperglycemia, thereby reducing immediate health risks and enhancing daily functioning.
Tips for Managing Blood Glucose Levels
Effectively managing blood glucose levels is crucial for preventing complications and maintaining overall health, especially for individuals with diabetes. By adopting certain lifestyle habits and monitoring techniques, you can keep your blood sugar within a healthy range. Here are some practical tips for managing blood glucose levels:
1. Dietary Recommendations
Managing blood glucose levels effectively involves strategic dietary choices. Incorporating insoluble and moderately fermentable cereal-based fiber and mono-unsaturated fatty acids can improve glucose homeostasis by delaying carbohydrate absorption. Additionally, low glycemic index (GI) diets have been shown to significantly decrease glycated hemoglobin (HbA1c) levels, thus improving glycemic control without increasing hypoglycemic events. Personalized diets, tailored to individual responses, can also help in managing postprandial blood glucose levels more effectively.
2. Exercise and Physical Activity Guidelines
Exercise is crucial for managing blood glucose levels, but it requires careful planning, especially for individuals with type 1 diabetes. Increasing carbohydrate intake before and after exercise and adjusting insulin doses can help mitigate the risk of hypoglycemia. Structured algorithms for carbohydrate and insulin adjustments during exercise have shown to be effective in maintaining glucose levels within a safe range. Regular physical activity, combined with continuous glucose monitoring, can further aid in stabilizing blood glucose levels.
3. Stress Management Techniques
Stress can significantly impact blood glucose levels, making stress management an essential component of diabetes care. Techniques such as mindfulness, meditation, and deep-breathing exercises can help reduce stress and improve overall well-being. Regular physical activity also serves as a stress reliever, contributing to better glycemic control. Support from family and healthcare providers can further alleviate stress, making it easier to manage diabetes effectively.
4. Monitor Blood Sugar Levels
Regular monitoring of blood glucose levels is vital for effective diabetes management. Using continuous glucose monitoring (CGM) systems can provide real-time data, helping individuals make informed decisions about their diet, exercise, and medication. Maintaining logbooks for blood glucose, physical activity, and dietary intake can also help in identifying patterns and making necessary adjustments to improve glycemic control.
5. Manage Carbohydrate Intake
Carbohydrate counting is a recommended strategy for managing blood glucose levels in diabetes. Learning to count carbohydrates accurately can help in adjusting insulin doses and maintaining stable blood glucose levels. Low-carbohydrate diets have been shown to reduce high blood glucose levels effectively and can be a primary approach in diabetes management. Personalized dietary plans can further optimize carbohydrate intake based on individual responses.
6. Increase Fiber Intake
Increasing fiber intake, particularly viscous soluble fiber, can help in managing blood glucose levels by slowing down the absorption of carbohydrates. High-fiber foods such as whole grains, fruits, vegetables, and legumes should be included in the diet to improve glycemic control. Fiber-rich diets not only help in stabilizing blood glucose levels but also contribute to overall digestive health.
7. Stay Hydrated
Staying hydrated is essential for maintaining optimal blood glucose levels. Dehydration can lead to higher blood glucose concentrations, making it harder to manage diabetes. Drinking adequate amounts of water throughout the day helps in flushing out excess glucose through urine and maintaining overall health. It is recommended to avoid sugary drinks and opt for water, herbal teas, or other non-caloric beverages.
8. Eat Moderate Portions
Eating moderate portions can help in preventing spikes in blood glucose levels. Overeating, especially high-carbohydrate foods, can lead to significant increases in blood glucose. Portion control, combined with balanced meals that include proteins, healthy fats, and fiber, can help in maintaining stable blood glucose levels. Mindful eating practices, such as eating slowly and paying attention to hunger cues, can also aid in portion control.
9. Get Adequate Sleep
Adequate sleep is crucial for effective blood glucose management. Poor sleep can lead to insulin resistance and higher blood glucose levels. Establishing a regular sleep routine, ensuring a comfortable sleep environment, and avoiding stimulants like caffeine before bedtime can help improve sleep quality. Good sleep hygiene practices contribute to better overall health and more stable blood glucose levels.