Antifungal agents are medications or substances used to treat fungal infections by either killing or inhibiting the growth of fungi. These drugs target various components of fungal cells, such as the cell membrane or cell wall, to disrupt their function and prevent the spread of infection. Antifungals come in different forms, including topical treatments (creams, ointments, powders), oral medications, and intravenous formulations. They are used to combat a wide range of fungal infections, from common superficial conditions like athlete’s foot and yeast infections to more severe systemic infections that can affect internal organs. Some well-known classes of antifungal drugs include azoles, polyenes, and echinocandins, each with its own mechanism of action. As fungal infections can be life-threatening in certain populations, such as immunocompromised individuals or transplant recipients, the development of new and more effective antifungal agents remains an important area of medical research.
Types of Antifungal Agents
Antifungal agents are medications designed to treat fungal infections, which can affect various parts of the body. These agents come in different forms and are used based on the severity and location of the infection. Below are the main types of antifungal agents:
1. Topical Antifungals
Topical antifungals are primarily used for treating superficial fungal infections such as tinea pedis, tinea corporis, and mild cases of tinea unguium. Commonly used topical agents include azoles like miconazole, clotrimazole, and newer agents such as efinaconazole, luliconazole, and sertaconazole. These medications are applied directly to the affected area, usually once or twice daily, and work by disrupting the fungal cell membrane, thereby inhibiting fungal growth. Topical antifungals are generally well-tolerated and have fewer systemic side effects compared to oral or intravenous antifungals, making them a preferred choice for localized infections.
2. Oral Antifungals
Oral antifungals are used for more severe or recalcitrant fungal infections that do not respond to topical treatments. Common oral antifungals include fluconazole, itraconazole, and terbinafine. These medications are effective against a wide range of fungal pathogens and are often used to treat conditions like oral candidiasis, onychomycosis, and systemic mycose. However, oral antifungals can have significant side effects, including hepatotoxicity and drug interactions, which necessitate careful monitoring during treatment. Newer oral agents like posaconazole and ravuconazole offer broad-spectrum activity and are being investigated for their efficacy and safety profiles.
3. Intravenous Antifungals
Intravenous antifungals are reserved for severe, invasive fungal infections, particularly in immunocompromised patients. Agents like amphotericin B, caspofungin, and voriconazole are commonly used in this setting. These drugs are highly effective but can be associated with significant toxicities, such as nephrotoxicity with amphotericin B and hepatotoxicity with voriconazole. Echinocandins like caspofungin, micafungin, and anidulafungin are newer intravenous options that offer potent antifungal activity with fewer side effects. The development of novel intravenous agents, such as isavuconazole and investigational drugs like CD101, aims to improve patient outcomes by offering better efficacy and safety profiles.
Common Antifungal Medications
Antifungal medications are essential for treating fungal infections, which can affect various parts of the body. These medications come in different forms, including topical, oral, and intravenous. Below is a list of some common antifungal medications used in clinical practice:
1. Azoles
Azoles, including fluconazole and ketoconazole, are a class of antifungal medications that target the cytochrome P450 enzyme lanosterol 14α-demethylase (CYP51). This enzyme is crucial for the biosynthesis of ergosterol, an essential component of fungal cell membranes. Azoles inhibit this enzyme by binding to its heme iron, thereby blocking ergosterol production and compromising the integrity of the fungal cell membrane, leading to cell death.
2. Echinocandins
Echinocandins, such as caspofungin and micafungin, are antifungal agents that inhibit the synthesis of β-1, 3-D-glucan, an essential component of the fungal cell wall. By targeting the enzyme β-1, 3-D-glucan synthase, echinocandins disrupt the cell wall structure, leading to osmotic instability and cell lysis. This mechanism is particularly effective against Candida and Aspergillus species.
4. Polyenes
Polyenes, including amphotericin B and nystatin, bind to ergosterol in the fungal cell membrane, forming pores that increase membrane permeability. This leads to leakage of essential intracellular components and ultimately cell death. The binding of polyenes to ergosterol is highly specific, making them effective against a broad range of fungal pathogens.
5. Allylamines
Allylamines, such as terbinafine, inhibit the enzyme squalene epoxidase, which is involved in the early steps of ergosterol biosynthesis. By blocking this enzyme, allylamines cause an accumulation of squalene and a deficiency of ergosterol, disrupting the fungal cell membrane and leading to cell death.
How Antifungals Work
These drugs work through various mechanisms to inhibit fungal growth and survival. Below is a list of how different classes of antifungals work:
1. Disruption of Fungal Cell Membrane
Antifungal drugs often target the fungal cell membrane to disrupt its integrity and function. Polyenes, such as amphotericin B, bind irreversibly to ergosterol, a key component of fungal cell membranes, leading to increased membrane permeability. This disruption causes leakage of essential intracellular components, resulting in metabolic dysfunction and cell death. Imidazole derivatives, another class of antifungals, inhibit the biosynthesis of ergosterol, thereby compromising the structural integrity of the cell membrane. This inhibition also affects the synthesis of triglycerides and phospholipids, leading to an accumulation of toxic hydrogen peroxide within the cell, which further contributes to cell necrosis.
2. Inhibition of Fungal Cell Wall Synthesis
The fungal cell wall is a critical structure for maintaining cell shape and integrity, making it an ideal target for antifungal therapy. Echinocandins, such as caspofungin, inhibit the synthesis of β(1,3)-D-glucan, an essential polysaccharide component of the fungal cell wall. This inhibition weakens the cell wall, leading to osmotic instability and cell lysis. Additionally, natural products like cyclic lipopeptides and glycolipids have shown potential in inhibiting cell wall synthesis by targeting glucan synthases and chitin synthases, enzymes responsible for the synthesis of β(1,3)-D-glucan and chitin, respectively. These inhibitors are particularly valuable as they exploit a structure absent in mammalian cells, thereby offering selective toxicity against fungal pathogens.
3. Inhibition of Fungal DNA Synthesis
Inhibiting fungal DNA synthesis is another effective strategy employed by antifungal agents. Flucytosine, for instance, is converted into 5-fluorouracil within the fungal cell, which is then incorporated into RNA, disrupting protein synthesis. Additionally, 5-fluorouracil inhibits thymidylate synthase, an enzyme crucial for DNA synthesis, thereby preventing cell replication. Alkaloids from the Amaryllidaceae family, such as lycorine and narciclasine, also exhibit antifungal properties by inhibiting both DNA and RNA synthesis. These compounds bind to fungal ribosomes, inhibiting peptide bond formation and thus protein synthesis, which indirectly affects DNA replication and cell division. This multifaceted approach ensures a comprehensive disruption of fungal cellular processes, leading to effective antifungal activity.
Common Uses of Antifungals
Antifungal medications are essential in treating a variety of fungal infections that can affect different parts of the body. These medications work by targeting and eliminating fungal pathogens, providing relief from symptoms and preventing the spread of infection. Below are some common uses of antifungals:
1. Treat Skin Infections
Antifungal medications are commonly used to treat various skin infections caused by fungi. These include athlete’s foot, jock itch, and ringworm. Topical antifungals like clotrimazole and miconazole are often effective for mild infections, while more severe cases may require oral antifungals such as terbinafine or fluconazole. The choice of treatment depends on the type and severity of the infection, as well as patient-specific factors like age and overall health.
2. Treat Vaginal Yeast Infections (Vulvovaginal Candidiasis)
Antifungals are available for both oral and intra-vaginal treatment of uncomplicated vulvovaginal candidiasis. Studies show no significant difference in clinical cure rates between oral and intra-vaginal antifungals for short-term and long-term follow-up. Oral treatments may improve mycological cure rates slightly over intra-vaginal treatments, and patient preference often leans towards oral administration due to convenience.
3. Treat Oral Thrush (Oropharyngeal Candidiasis)
Oral thrush, caused by Candida species, is commonly treated with antifungal medications. Topical treatments like nystatin or clotrimazole lozenges are often used for mild cases, while systemic treatments such as fluconazole or itraconazole may be required for more severe or recurrent infections. The choice of treatment depends on the severity of the infection and patient-specific factors.
4. Treat Systemic Fungal Infections
Systemic fungal infections, which can affect internal organs, require potent antifungal medications. Commonly used systemic antifungals include amphotericin B, fluconazole, itraconazole, and voriconazole. These medications are often administered intravenously in a hospital setting due to the severity of the infections and the need for close monitoring of side effects and efficacy.
5. Treat Fungal Infections of the Scalp (Tinea Capitis)
Systemic antifungal therapy is required for treating tinea capitis, a common contagious fungal infection of the scalp in children. Studies indicate that newer treatments like terbinafine, itraconazole, and fluconazole are as effective as griseofulvin, with shorter treatment durations potentially improving adherence. However, griseofulvin remains a standard treatment, especially for Microsporum infections.
6. Treat Fungal Eye Infections like Fungal Keratitis
Fungal keratitis, an infection of the cornea, is treated with antifungal eye drops such as natamycin or amphotericin B. In severe cases, systemic antifungal therapy may be required. Early diagnosis and treatment are crucial to prevent complications and preserve vision. The choice of antifungal depends on the specific fungal pathogen and the severity of the infection.
7. Treatment of Severe Dandruff Caused by Fungal Overgrowth
Severe dandruff, often caused by the fungus Malassezia, can be treated with antifungal shampoos containing ketoconazole, selenium sulfide, or zinc pyrithione. These treatments help reduce fungal overgrowth and alleviate symptoms. In more persistent cases, oral antifungal medications like itraconazole may be prescribed.
8. Treat Fungal Sinus Infections
Fungal sinus infections, though less common than bacterial ones, can be serious and require antifungal treatment. Amphotericin B, itraconazole, and voriconazole are commonly used antifungals for treating invasive fungal sinusitis. Treatment often involves a combination of surgical debridement and antifungal therapy to effectively manage the infection.
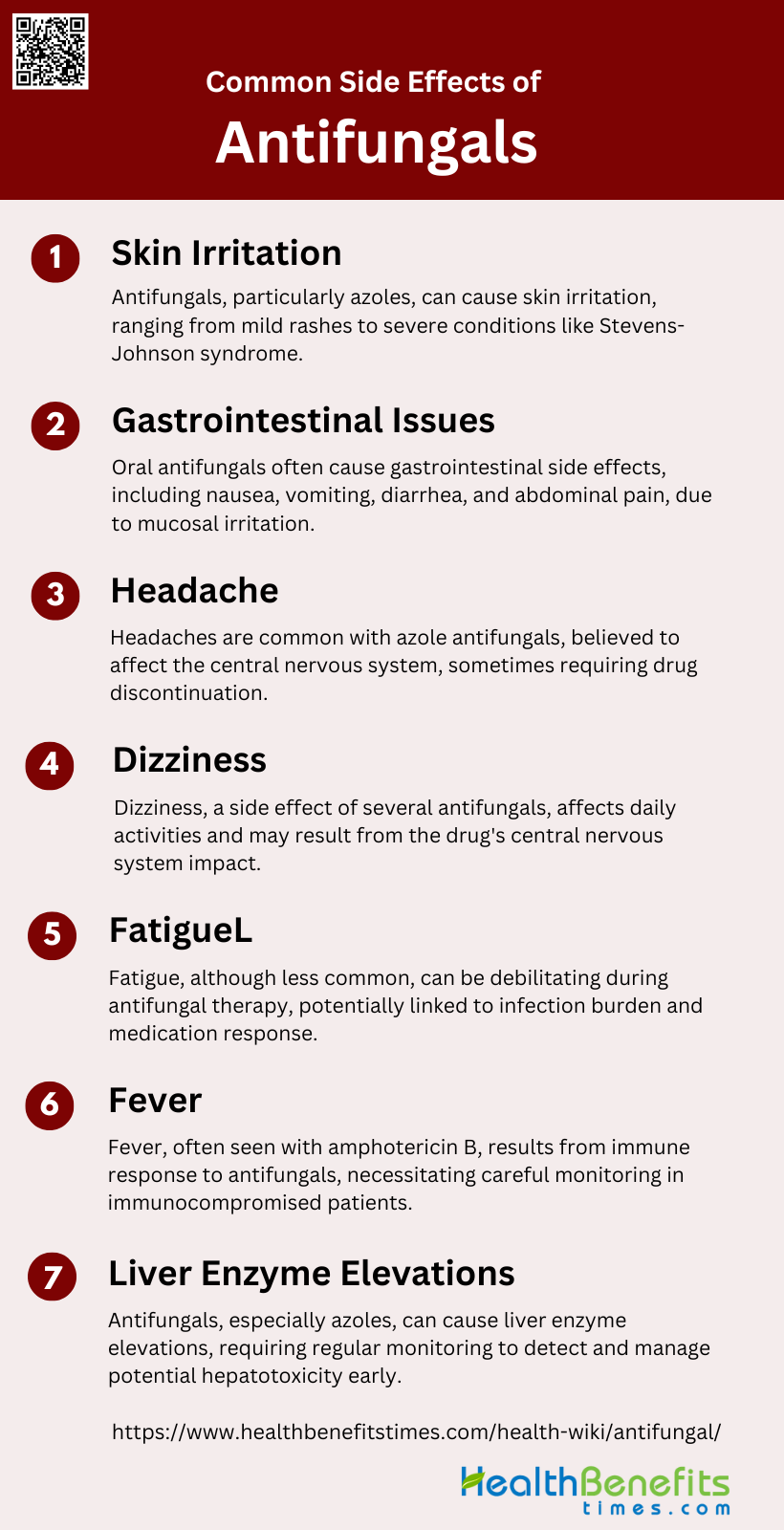
Common Side Effects of Antifungal
These side effects vary depending on the type of antifungal used and the individual’s response to the medication. Below are some common side effects of antifungals:
1. Skin Irritation
Skin irritation is a common side effect associated with antifungal agents, particularly azoles. These reactions can range from mild rashes to severe conditions such as Stevens-Johnson syndrome and toxic epidermal necrolysis. The hypersensitivity reactions are often T-cell mediated and can manifest as fixed drug eruptions, localized or generalized dermatitis, and acute generalized exanthematous pustulosis. Immediate-type reactions such as urticaria and angioedema have also been reported, although they are less frequent. The pathomechanisms and risk factors for these reactions are not well understood, making diagnosis and management challenging.
2. Gastrointestinal Issues
Gastrointestinal issues are frequently reported side effects of oral antifungal agents. These can include nausea, vomiting, diarrhea, and abdominal pain. The incidence of these side effects varies among different antifungal classes. For instance, azoles like itraconazole and fluconazole are known to cause gastrointestinal upset. These side effects are generally mild but can lead to discontinuation of therapy in some cases. The gastrointestinal disturbances are thought to be due to the direct irritant effect of the drug on the gastrointestinal mucosa.
3. Headache
Headache is another common side effect associated with antifungal therapy. This is particularly noted with the use of azole antifungals such as fluconazole and itraconazole. The exact mechanism by which these drugs cause headaches is not well understood, but it is believed to be related to their effect on the central nervous system. In most cases, the headaches are mild and transient, but they can be severe enough to necessitate discontinuation of the drug in some patients.
4. Dizziness
Dizziness is a reported side effect of several antifungal agents, including azoles and echinocandins. This side effect can be particularly troublesome for patients, affecting their daily activities and quality of life. The mechanism behind dizziness induced by antifungal agents is not well elucidated, but it may be related to the drug’s impact on the central nervous system or its interaction with other medications. Monitoring and managing this side effect is crucial, especially in patients who are on long-term antifungal therapy.
5. Fatigue
Fatigue is a less commonly reported but significant side effect of antifungal therapy. It can be particularly debilitating for patients who are already dealing with severe infections and other comorbidities. The exact cause of fatigue in patients taking antifungal agents is not well understood, but it may be related to the overall burden of the infection and the body’s response to the medication. Clinicians should be aware of this potential side effect and manage it appropriately to improve patient compliance and quality of life.
6. Fever
Fever is a known side effect of antifungal therapy, particularly with agents like amphotericin B. This side effect is often a result of the body’s immune response to the drug and can be accompanied by chills and rigors. Fever can be particularly concerning in immunocompromised patients, as it may be difficult to distinguish between drug-induced fevers and fever due to an underlying infection. Careful monitoring and supportive care are essential to manage this side effect effectively.
7. Liver Enzyme Elevations
Elevations in liver enzymes are a significant concern with the use of antifungal agents, especially azoles like itraconazole and voriconazole. Hepatotoxicity can range from mild, asymptomatic increases in liver enzymes to severe liver damage requiring discontinuation of the drug. Regular monitoring of liver function tests is recommended for patients on long-term antifungal therapy to detect and manage hepatotoxicity early. In most cases, liver enzyme elevations are reversible upon discontinuation of the offending agent.
Natural Antifungal Remedies
Natural antifungal remedies offer an alternative approach to combating fungal infections using ingredients found in nature. These remedies can be effective in treating mild to moderate infections and often come with fewer side effects compared to conventional medications. Below are some common natural antifungal remedies:
1. Tea Tree Oil
Tea tree oil has been extensively studied for its antifungal properties, particularly against Candida albicans and dermatophytes. Several clinical trials have demonstrated its effectiveness in treating fungal infections, with positive outcomes reported in all trials reviewed. The oil’s active components, such as terpinen-4-ol, contribute to its antifungal activity by disrupting the cell membrane of fungi, leading to cell death. Despite its promise, further rigorous clinical trials are needed to fully establish its efficacy and safety profile.
2. Garlic
Garlic is known for its broad-spectrum antimicrobial properties, including antifungal activity. The primary antifungal component in garlic is allicin, which has been shown to inhibit the growth of various fungal pathogens, including Candida species. Allicin disrupts the lipid bilayer of fungal cell membranes, leading to cell lysis. Studies have indicated that garlic extracts can be effective in both in vitro and in vivo settings, making it a potential natural remedy for fungal infections. However, more clinical trials are necessary to confirm these findings and determine optimal dosages.
3. Oregano Oil
Oregano oil contains high levels of phenolic compounds such as carvacrol and thymol, which exhibit strong antifungal properties. These compounds work by disrupting the integrity of fungal cell membranes and inhibiting the growth of fungi. Research has shown that oregano oil is effective against a variety of fungal pathogens, including Candida albicans. Its antifungal activity is comparable to that of some conventional antifungal agents, making it a promising alternative treatment. Further studies are needed to explore its full potential and safety in clinical settings.
4. Apple Cider Vinegar
Apple cider vinegar (ACV) has been traditionally used for its antimicrobial properties, including antifungal effects. The acetic acid in ACV is believed to inhibit fungal growth by lowering the pH of the environment, making it inhospitable for fungi. Some studies have shown that ACV can be effective against Candida species and other fungal pathogens. However, the evidence is mostly anecdotal, and more scientific research is required to validate its efficacy and safety as an antifungal remedy.
5. Coconut Oil
Coconut oil has demonstrated antifungal activity, particularly against Candida albicans. The medium-chain fatty acids in coconut oil, such as lauric acid, are responsible for its antifungal properties. These fatty acids disrupt the cell membrane of fungi, leading to cell death. In vitro studies have shown that coconut oil can inhibit the growth of Candida species, although its effectiveness is lower compared to conventional antifungal agents like clotrimazole. Further research is needed to establish its clinical efficacy and potential as a natural antifungal treatment.
6. Yogurt and Probiotics
Yogurt and probiotics contain beneficial bacteria that can help maintain a healthy microbial balance, potentially preventing fungal overgrowth. Probiotics such as Lactobacillus species produce lactic acid and other antimicrobial substances that inhibit the growth of pathogenic fungi, including Candida albicans. Studies have shown that probiotics can be effective in reducing the incidence of fungal infections, particularly in the oral and vaginal regions. However, more clinical trials are needed to confirm these findings and determine the most effective strains and dosages.
7. Turmeric
Turmeric, particularly its active component curcumin, has shown promising antifungal properties. Curcumin disrupts fungal cell membranes and inhibits the growth of various fungal pathogens. Studies have demonstrated that turmeric essential oil can enhance the antifungal activity of conventional antifungal creams, suggesting a synergistic effect. This makes turmeric a potential candidate for combination therapies in the treatment of fungal infections. Further research is required to fully understand its mechanisms of action and clinical efficacy.
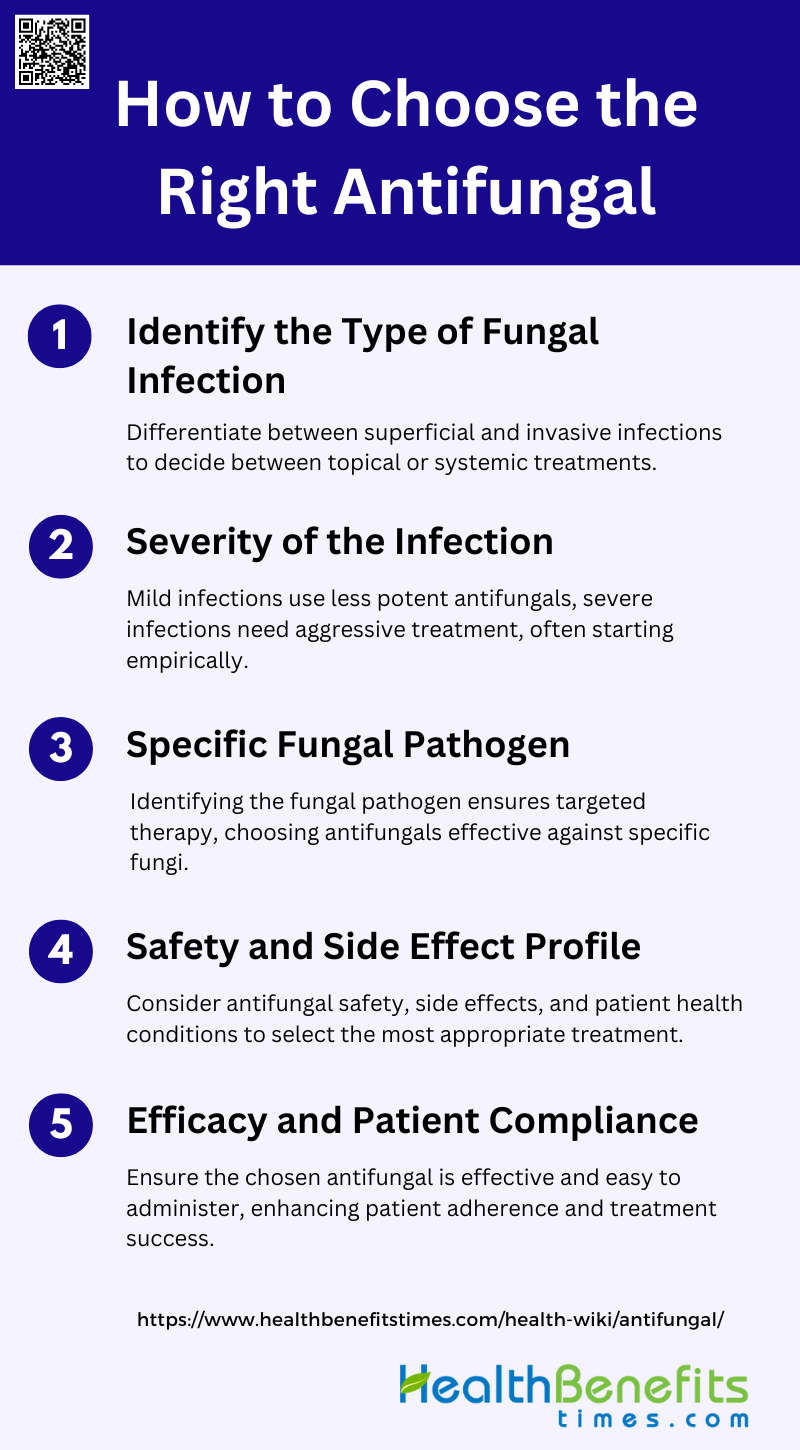
How to Choose the Right Antifungal
Selecting the appropriate antifungal medication is crucial for effectively treating fungal infections. The choice depends on various factors, including the type of infection, its severity, and individual health conditions. Below are some guidelines on how to choose the right antifungal:
1. Identify the Type of Fungal Infection
The first step in choosing the right antifungal is to identify the type of fungal infection. This involves distinguishing between superficial and invasive fungal infections. Superficial infections, such as those affecting the skin or nails, often require topical treatments, while invasive infections, which can affect internal organs, necessitate systemic therapy. For instance, invasive fungal infections in critically ill patients are often caused by Candida spp., which require prompt and appropriate systemic antifungal therapy to reduce morbidity and mortality.
2. Severity of the Infection
The severity of the infection plays a crucial role in antifungal selection. Mild infections might be managed with less potent antifungals, whereas severe or life-threatening infections require more aggressive treatment. In critically ill patients, the severity of the infection can dictate the need for immediate empirical therapy even before pathogen identification, as delays can lead to worse outcomes. For example, in cases of severe invasive candidiasis, echinocandins or high-dose azoles are often preferred due to their broad spectrum and efficacy.
3. Specific Fungal Pathogen
Identifying the specific fungal pathogen is essential for targeted therapy. Different fungi have varying susceptibilities to antifungal agents. For instance, Candida albicans is typically susceptible to azoles, while non-albicans species may require echinocandins or polyenes due to resistance patterns. Species identification can guide the choice of antifungal, ensuring the selected drug is effective against the pathogen. In cases where the pathogen is unknown, broad-spectrum antifungals may be used initially.
4. Safety and Side Effect Profile
The safety and side effect profile of antifungal agents must be considered, especially in patients with comorbidities or those receiving multiple medications. For example, amphotericin B, while effective, is associated with significant nephrotoxicity, making it less suitable for patients with renal impairment. Echinocandins and newer azoles like posaconazole and voriconazole offer better safety profiles and fewer drug interactions, making them preferable in many cases. Monitoring for adverse effects and adjusting therapy as needed is crucial for patient safety.
5. Efficacy and Patient Compliance
Efficacy and patient compliance are critical factors in antifungal therapy. The chosen antifungal must not only be effective against the pathogen but also be administered in a manner that ensures patient adherence. Oral formulations are generally preferred for outpatient settings due to ease of administration, while intravenous formulations may be necessary for severe infections or hospitalized patients. Ensuring appropriate dosing and considering pharmacokinetic properties, such as absorption and distribution, can enhance treatment efficacy and patient compliance.