An antibacterial is a substance that inhibits the growth and reproduction of bacteria, thereby preventing infections and promoting healing. These agents can be either bacteriostatic, which means they stop bacteria from multiplying, or bactericidal, which means they kill bacteria outright. Antibacterials are commonly found in various forms, including antibiotics, antiseptics, and disinfectants, and are used in medical settings, personal hygiene products, and household cleaners. Their primary function is to target specific bacterial processes or structures, such as cell wall synthesis or protein production, to ensure the effective elimination of harmful bacteria while minimizing damage to host tissues.
Types of antibacterials
Antibacterials are agents that inhibit bacterial growth or kill bacteria. They can be broadly categorized into natural and synthetic types, each with unique properties and mechanisms of action. Below are the main types of antibacterials:
1. Natural Antibacterials
Natural antibacterials are derived from various sources such as plants, animals, bacteria, algae, and mushrooms. These compounds have gained significant attention due to their potential to combat antibiotic-resistant bacteria and their perceived safety compared to synthetic alternatives. For instance, flavonoids, a large class of natural compounds, have shown promising antibacterial activity, sometimes even outperforming standard drugs. Alkaloids, another group of natural compounds, have been used as scaffolds for important antibacterial drugs and continue to show potential in combating resistant bacteria. Additionally, natural antioxidants like polyphenols and vitamins not only boost the immune system but also exhibit antibacterial properties, making them viable alternatives to synthetic antibiotics. The food industry has also shown interest in natural antibacterials to enhance food safety and quality, given their effectiveness against a broad range of foodborne pathogens.
2. Synthetic Antibacterials
Synthetic antibacterials are chemically engineered compounds designed to inhibit or kill bacterial pathogens. These agents are often preferred in clinical settings due to their high activity and cost-effectiveness. However, their use is sometimes limited by higher toxicity compared to natural antibacterials. Synthetic alkaloids, for example, have been developed to enhance antibacterial activity and reduce resistance, with some showing remarkable efficacy against multidrug-resistant bacteria. Additionally, synthetic compounds with dual antibacterial and antioxidant activities have been explored to address complex infections and oxidative stress, offering a promising therapeutic approach. The development of synthetic membrane-active antibacterial agents has also shown potential in tackling bacterial resistance by preventing the development of resistance mechanisms. Despite their advantages, the challenge remains to design synthetic antibacterials that are both highly effective and low in toxicity.
How Antibacterials Work
Antibacterials function by targeting specific bacterial processes and structures, thereby inhibiting growth or causing bacterial death. They can disrupt cell walls, inhibit protein synthesis, or interfere with DNA replication. Below are the main mechanisms by which antibacterials work:
1. Cell Wall Disruption
Antibacterials that target the bacterial cell wall are highly effective because the cell wall is essential for bacterial survival. Beta-lactams, such as penicillins and cephalosporins, inhibit the synthesis of tart, a critical component of the bacterial cell wall, leading to cell lysis and death. Glycopeptides, like vancomycin, bind to the D-alanyl-D-alanine terminus of cell wall precursors, preventing their incorporation into the cell wall. Novel inhibitors, such as anthranilic acids, have also been shown to disrupt cell wall biosynthesis by targeting specific proteins involved in polysaccharide biosynthesis. Additionally, imaging methodologies have provided molecular insights into how these antibiotics impair the peptidoglycan ultrastructure, further elucidating their mechanisms of action.
2. Protein Synthesis Inhibition
Antibacterials that inhibit protein synthesis target the bacterial ribosome, thereby preventing the production of essential proteins. Macrolides, tetracyclines, and aminoglycosides are well-known classes of antibiotics that achieve this by binding to different sites on the bacterial ribosome. For instance, aminoglycosides interfere with the proofreading process of translation, leading to the production of faulty proteins. Recent studies have also highlighted the role of cationic antimicrobial peptides, which not only disrupt the bacterial membrane but also inhibit intracellular processes such as protein synthesis and chaperone-assisted protein folding. These multifaceted mechanisms make protein synthesis inhibitors a crucial component in the fight against bacterial infections.
3. DNA Synthesis Interference
Antibacterials that interfere with DNA synthesis target enzymes essential for DNA replication and repair. Fluoroquinolones, for example, inhibit DNA gyrase and topoisomerase IV, enzymes critical for maintaining DNA supercoiling and segregation during cell division. Madecassic acid, a natural compound, has been shown to interact with bacterial DNA, causing relaxation and ring opening of supercoiled DNA, and inhibiting DNA topoisomerase I and II activities. Additionally, gold nanoclusters have been found to cause DNA damage and disrupt DNA replication and repair processes, leading to bacterial cell death. These mechanisms highlight the importance of targeting DNA synthesis in developing effective antibacterial therapies.
Common Uses of Antibacterials
Antibacterials are widely used in both medical and household settings to prevent and treat bacterial infections. They play a vital role in maintaining health and hygiene. Below are common uses of antibacterials:
1. Medical Applications
Antibacterials play a crucial role in medical applications, primarily in the treatment of infections, surgical sterilization, and as antibacterial medications such as antibiotics. These agents are essential in preventing and treating infections associated with medical devices and surgical procedures. For instance, inorganic antibacterial agents like silver, copper, gold, and zinc, as well as organic agents such as chlorhexidine and triclosan, are widely used in biomedical applications to combat bacterial infections. These agents work through various mechanisms, including the release of ions that inhibit bacterial growth and the disruption of bacterial cell walls. The use of antibacterial materials in medical devices not only helps in preventing infections but also promotes cell proliferation and wound healing. However, the overuse of these agents can lead to bacterial resistance, necessitating prudent use and continuous monitoring.
2. Household Uses
In household settings, antibacterial agents are commonly found in cleaning products and personal hygiene items. These products have seen a significant increase in usage, with over 700 different antibacterial household products available today. Quaternary ammonium compounds (QACs) and triclosan are frequently used in household disinfectants and hand soaps to reduce microbial contamination on surfaces and skin. While these products are effective in reducing the spread of disease-causing microorganisms, there is growing concern about their potential to contribute to bacterial resistance and disrupt the natural microflora of the skin, which could impact immune system development and increase the risk of allergies in children. Therefore, it is recommended to use these products judiciously to avoid adverse effects on health and the environment.
Benefits of Antibacterials
Antibacterials offer numerous benefits by effectively controlling and eliminating harmful bacteria. They are essential in both healthcare and everyday life for preventing infections and maintaining hygiene. Below are some key benefits of antibacterials:
1. Effective Treatment of Bacterial Infections
Antibacterial agents are crucial in the effective treatment of bacterial infections, offering a targeted approach to eliminate pathogenic bacteria. These agents, including antibiotics, bacteriophages, and antimicrobial peptides, work by disrupting bacterial cell walls, inhibiting protein synthesis, or interfering with bacterial DNA replication, leading to bacterial cell death. The development of narrow-spectrum antibacterial agents further enhances treatment efficacy by targeting specific bacterial strains, thereby reducing the risk of resistance and preserving beneficial microbiota. Additionally, the use of nanotechnology in drug delivery systems has improved the precision and effectiveness of antibacterial treatments, ensuring higher success rates in combating infections.
2. Prevention of Infections
Antibacterial agents play a significant role in the prevention of infections, particularly in medical settings where the risk of infection is high. Surface design strategies for antibacterial materials, such as coatings on medical devices, help prevent bacterial adhesion and biofilm formation, thereby reducing the incidence of healthcare-associated infections. Organic and inorganic antibacterial agents, including silver, copper, and chlorhexidine, are commonly used to coat medical devices, providing a protective barrier against bacterial colonization. These preventive measures are essential in maintaining sterile environments and protecting patients from potential infections.
3. Rapid Action
The rapid action of antibacterial agents is a critical factor in their effectiveness. Enzyme-based antibacterials, or enzybiotics, and nanozyme-based antibacterials, known as nanozybiotics, exhibit rapid bacterial killing mechanisms, making them highly effective in acute infection scenarios. These agents work quickly to disrupt bacterial cell functions, leading to immediate bacterial cell death. The swift action of these antibacterials is particularly beneficial in treating severe infections where time is of the essence, reducing the risk of complications and improving patient outcomes.
4. Wide Range of Applications
Antibacterial agents have a wide range of applications beyond treating infections. They are used in food preservation, livestock management, and various industrial processes to prevent bacterial contamination and ensure safety. In the biomedical field, antibacterial agents are incorporated into wound dressings, surgical instruments, and implantable devices to prevent post-surgical infections and promote healing. The versatility of antibacterial agents in different sectors underscores their importance in maintaining public health and safety.
5. Lifesaving Potential
The lifesaving potential of antibacterial agents cannot be overstated. They have been instrumental in reducing mortality rates associated with bacterial infections, particularly in vulnerable populations such as the elderly, immunocompromised individuals, and patients undergoing surgery. The development of new antibacterial strategies, including combinatorial therapies and nanomedicine, has further enhanced their efficacy, offering hope in the fight against multidrug-resistant bacteria. By effectively treating infections and preventing their spread, antibacterial agents save countless lives each year.
6. Prevention of Disease Spread
Antibacterial agents are essential in preventing the spread of infectious diseases. By effectively eliminating pathogenic bacteria, these agents reduce the transmission of infections within communities and healthcare settings. The use of targeted antibacterial treatments, combined with rapid diagnostic tests, helps contain outbreaks and prevent the spread of resistant bacterial strains. Additionally, antibacterial coatings on surfaces and medical devices act as a barrier to bacterial transmission, further contributing to infection control efforts.
7. Support for Vulnerable Populations
Vulnerable populations, including the elderly, children, and immunocompromised individuals, benefit significantly from the use of antibacterial agents. These populations are at higher risk of severe infections and complications, making effective antibacterial treatments crucial for their health and well-being. Antibacterial agents help prevent infections in these groups by providing targeted and effective treatment options, reducing the risk of complications and improving overall health outcomes. The development of new antibacterial strategies continues to enhance the support provided to these vulnerable populations, ensuring they receive the best possible care.
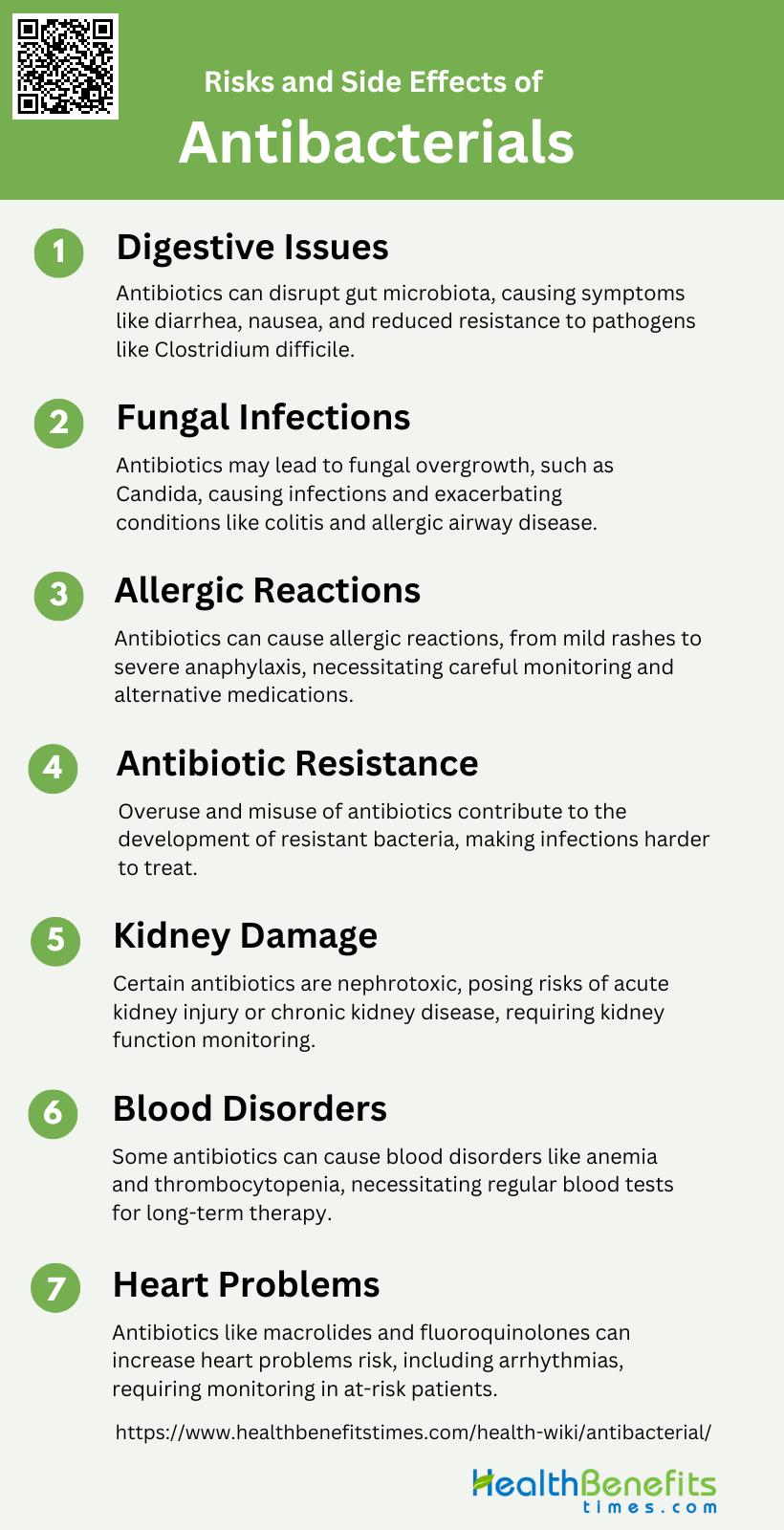
Risks and Side Effects
While antibacterials are crucial for combating infections, they also come with potential risks and side effects. Misuse or overuse can lead to antibiotic resistance and adverse health effects. Below are some common risks and side effects associated with antibacterials:
1. Digestive Issues
Antibiotic use can significantly disrupt the gastrointestinal microbiota, leading to various digestive issues. The eradication of beneficial bacteria, or probiotics, can result in irritation of the mucous membrane of the digestive tract, causing symptoms such as diarrhea, nausea, and abdominal cramping. Additionally, the disturbance in the gut microbiota can reduce resistance to pathogens like Clostridium difficile, which can lead to severe diarrhea and colitis. The imbalance in the gut flora due to antibiotics underscores the importance of maintaining a healthy microbial community for digestive health.
2. Fungal Infections
The use of antibiotics can also predispose individuals to fungal infections. Antibiotics not only target harmful bacteria but also disrupt the balance of the normal microbial flora, which can lead to an overgrowth of fungi such as Candida spp. in the mouth and digestive tract. Furthermore, prolonged antifungal treatments can restructure fungal communities, increasing the prevalence of fungi like Aspergillus, Wallemia, and Epicoccum spp., which can exacerbate conditions such as colitis and allergic airway disease. This highlights the complex interplay between bacterial and fungal populations in maintaining health.
3. Allergic Reactions
Allergic reactions to antibiotics are a common side effect, with symptoms ranging from mild rashes to severe anaphylaxis. Some individuals may develop hypersensitivity to certain antibiotics, leading to immune responses that can manifest as skin rashes, itching, and swelling. In severe cases, allergic reactions can cause anaphylactic shock, which is a medical emergency. The risk of allergic reactions necessitates careful monitoring and, in some cases, the use of alternative medications to avoid adverse effects.
4. Antibiotic Resistance
One of the most significant risks associated with antibiotic use is the development of antibiotic resistance. Bacteria can evolve mechanisms to survive antibiotic treatment, rendering standard therapies ineffective. This resistance can lead to more severe and persistent infections, as well as the spread of resistant strains within communities. The overuse and misuse of antibiotics are major contributors to this global health threat, emphasizing the need for judicious use of these medications.
5. Kidney Damage
Antibiotics can also pose a risk to kidney health. Certain antibiotics are nephrotoxic and can cause damage to the kidneys, leading to conditions such as acute kidney injury or chronic kidney disease. The risk is particularly high in individuals with pre-existing kidney conditions or those taking other nephrotoxic drugs. Monitoring kidney function during antibiotic therapy is crucial to prevent long-term damage and ensure patient safety.
6. Blood Disorders
Some antibiotics can cause blood disorders, including anemia, leukopenia, and thrombocytopenia. These conditions result from the suppression of bone marrow activity or the destruction of blood cells. For instance, certain antibiotics can induce hemolytic anemia, where red blood cells are destroyed faster than they can be produced. Regular blood tests may be necessary to monitor for these potential side effects, especially in patients on long-term antibiotic therapy.
7. Heart Problems
Antibiotics can also have cardiovascular side effects. Some antibiotics, particularly those in the macrolide and fluoroquinolone classes, have been associated with an increased risk of heart problems, including arrhythmias and prolonged QT intervals. These conditions can lead to serious complications such as sudden cardiac death. Patients with pre-existing heart conditions or those taking other medications that affect heart rhythm should be closely monitored when prescribed these antibiotics.
Choosing the Right Antibacterial
Selecting the appropriate antibacterial is essential for effective treatment and minimizing side effects. Factors such as the type of infection, bacterial resistance, and patient health must be considered. Below are considerations for choosing the right antibacterial:
1. Factors to Consider
When selecting an antibacterial, several factors must be taken into account to ensure efficacy and safety. The primary consideration is the purpose of use, which dictates the choice of antibacterial based on the type of infection and the causative organism. Sensitivity to ingredients is another crucial factor, as the effectiveness of an antibacterial agent can be influenced by the pathogen’s susceptibility to the drug, as well as the drug’s ability to reach the site of infection and maintain its activity under local conditions. Additionally, the potential for resistance development must be considered, as overuse or misuse of antibacterial agents can lead to resistant strains, complicating future treatment efforts. Cost and safety are also important, as the chosen antibacterial should be affordable and have a favorable safety profile to minimize adverse effects.
2. Recommended Products by Experts
Experts recommend selecting antibacterial products based on a combination of efficacy, safety, and the specific needs of the patient. For instance, broad-spectrum antibiotics are often recommended for initial treatment of wound infections due to their ability to target a wide range of pathogens. In the context of household use, products containing quaternary ammonium compounds (QACs) and triclosan are commonly used, but their overuse has raised concerns about the development of resistant bacteria. For specific conditions, such as ophthalmic infections, products like fusidic acid and quinolones are recommended due to their ability to penetrate the cornea and reach therapeutic concentrations in the anterior chamber of the eye. In biomedical applications, a combination of inorganic agents like silver and organic agents like chlorhexidine is suggested to cover a broad antibacterial spectrum and reduce the risk of resistance.