The ankle joint is a complex structure that is essential for mobility and stability. It is composed of the distal tibia, fibula, and talus, with the medial and lateral malleoli providing stability. Ankle injuries, which are common among both children and adults, can range from sprains to fractures, with physical fractures being a concern due to potential growth disturbances. The treatment of ankle injuries varies depending on the severity, with options including immobilization, surgery, or conservative management. Ankle foot orthoses (AFOs) play a significant role in assisting safe and efficient walking in stroke patients by providing stability and promoting proper gait patterns. Additionally, osteopathic techniques have shown promise in rehabilitating ankle injuries, particularly in restoring joint functions and reducing pain. Overall, a comprehensive understanding of the anatomy, mechanisms of injury, and treatment options for ankle injuries is crucial for effective management and optimal outcomes.
What is the ankle joint?
The ankle joint is a complex structure that plays a crucial role in human biomechanics. It consists of the articulation between the tibia, fibula, and talus bones, forming the ankle mortise, which allows for dorsiflexion and plantarflexion movements. The joint complex also includes the subtalar joint, contributing to a combination of rotation and translation over different articular surfaces simultaneously. Ligaments such as the deltoid ligament and the anterior and posterior talofibular ligaments provide stability to the ankle joint, with the deltoid ligament being the main medial stabilizer. Ankle biomechanics are intricate, involving movements around three planes or axes, crucial for absorbing forces and generating propulsion during activities like gait. Understanding the anatomy and biomechanics of the ankle joint is essential for addressing issues like arthritis, which can significantly impact gait and overall function.
Anatomy of Ankle
The ankle is a complex joint that is essential for weight-bearing activities. It consists of a network of osseous and soft tissue structures that maintain a balance between structure and function. Ligaments are crucial for stabilizing the ankle and subtalar joints, and injuries are often associated with ankle sprains caused by inversion or eversion mechanics that affect the ligamentous complexes. Anatomically, the ankle is a highly congruent synovial joint where the talus fits precisely into the mortise formed by the tibial plateau and malleoli. This allows movement primarily along the bimalleolar axis for dorsiflexion and plantarflexion motions. Understanding the intricate anatomy of the ankle, including ligaments and bony structures, is essential for effectively evaluating and treating athletic injuries involving this joint.
1. Muscular and Tendon Anatomy of Ankle
The anatomy of the ankle consists of a complex network of muscles and tendons that are essential for its function. The tendons around the ankle are divided into anterior, medial, posterior, and lateral groups, each with specific functions. Additionally, accessory muscles such as the peroneus tertius, tibiocalcaneus internus, and peroneocalcaneus internus may be present, affecting ankle biomechanics and potentially leading to conditions like tarsal tunnel syndrome. These structures work together to enable movements along the bimalleolar axis, allowing for dorsiflexion and plantarflexion within specific ranges of motion. Understanding the detailed muscular and tendon anatomy of the ankle is crucial for diagnosing and treating various ankle disorders, as well as for guiding therapeutic interventions and surgical procedures effectively.
2. Foot Anatomy
The anatomy of the ankle and foot is a complex yet crucial area for movement and stability. The foot is composed of 26 articulating bones, 31 joints, and 20 intrinsic muscles. The arch structure and key muscular functions are important for stability and resilience. The ankle is a synovial hinge-type joint that allows movement primarily through the bimalleolar axis, facilitating dorsiflexion and plantarflexion movements within specific ranges. Inflammatory pediatric arthritides can affect various structures in this region, making ultrasonography a valuable tool for precise assessment. The foot consists of 28 bones, 33 joints, and 112 ligaments, controlled by both extrinsic and intrinsic muscles, divided into hindfoot, midfoot, and forefoot regions. Understanding this detailed anatomy is essential for preventing injuries and enhancing balance and mobility.
- Hindfoot
The anatomy of the ankle and foot, particularly the hindfoot, is a complex and crucial area for weight-bearing and movement. The hindfoot is composed of the talus and calcaneus bones, which play a significant role in supporting body weight and facilitating bipedal movements. Fractures in the hindfoot, such as those in the calcaneus and talus, can lead to long-term issues like posttraumatic osteoarthritis, impacting daily activities due to pain and stiffness. Avulsion fractures in the ankle and hindfoot are diverse injuries that occur at various soft-tissue attachments, requiring a precise understanding of the relevant anatomy for accurate identification and treatment. Overall, a comprehensive understanding of the intricate structures and functions of the ankle and foot anatomy, especially the hindfoot, is essential for maintaining stability, preventing injuries, and optimizing movement capabilities.
- Midfoot
The midfoot is an important part of the complex anatomy of the foot, consisting of the cuboid, navicular, and three cuneiform bones, which are essential for foot function and stability. In cases of midfoot injury, such as Lisfranc sprain, timely and accurate treatment is necessary to prevent the development of chronic conditions with long-lasting symptoms. Magnetic resonance imaging (MRI) is a useful tool for evaluating midfoot anatomy, providing detailed information on normal structures and pathologies in the midfoot area. Furthermore, research comparing the anatomical structures of the midfoot in mice and humans has revealed similarities in key parameters, suggesting the potential for using mouse models to study midfoot functions and injuries. Understanding the anatomy and biomechanics of the midfoot is crucial for effectively managing injuries and conditions that affect this region.
- Forefoot
The anatomy of the forefoot, a critical region distal to the talus and calcaneus, plays a vital role in weight-bearing and movement. Comprising five metatarsal bones and corresponding toes, the forefoot is essential for supporting the foot arch, providing shock absorption, and converting vertical forces into horizontal propulsion. This complex structure is controlled by intrinsic and extrinsic muscles, with a total of 28 bones, 33 joints, and 112 ligaments contributing to its functionality. Understanding the biomechanics and alignment of the forefoot is crucial in diagnosing and managing a spectrum of acute, subacute, and chronic conditions that can lead to pain and decreased function. In cases of traumatic or overuse injuries in the forefoot, thorough evaluation through x-rays and potentially advanced imaging is necessary for appropriate diagnosis and management, which may include non-weight-bearing immobilization and referral to orthopedic specialists.
Important Structures of Ankles
The ankle joint is composed of a complex network of bone and soft tissue structures that are essential for weight-bearing activities and the gait cycle. Understanding ankle anatomy, biomechanics, and gender-related differences is crucial for evaluating and managing athletic injuries involving the ankle joint. The foot, which acts as the body’s connection to the ground during upright posture, must maintain a balance between stability and flexibility to support body weight and adapt to different terrains during movement. With 26 bones, 31 joints, and 20 intrinsic muscles, the foot and ankle play a key role in providing foundational support for standing, walking, and dancing, underscoring the importance of maintaining stability and resilience to prevent injuries and improve performance. Ultrasound assessments have revealed variations in the length and thickness of important ankle structures such as the anterior talofibular ligament in individuals with a history of lateral ankle sprains, underscoring the significance of these structures in ankle stability and injury prevention.
1. Bones and joints
The ankle is a complex joint that plays a crucial role in weight-bearing and movement. It is composed of three main bones: the tibia, fibula, and talus. The tibia and fibula are the two long bones of the lower leg, with the tibia being the larger and more weight-bearing bone. The talus is a small, irregularly shaped bone that sits between the tibia and fibula, forming the ankle joint. The ankle joint itself is a hinge joint, allowing for up and down movement of the foot, known as dorsiflexion and plantarflexion. The ankle also contains several important ligaments, such as the deltoid ligament on the medial side and the lateral collateral ligaments on the outer side, which provide stability and prevent excessive motion. Additionally, the ankle is surrounded by a complex network of tendons, including the Achilles tendon, which connects the calf muscles to the heel bone and is essential for walking, running, and jumping.
2. Ligaments and tendons
The ankle is a complex joint that is susceptible to injuries, with ligaments and tendons playing crucial roles in its stability and function. Ligaments, such as the lateral ligament complex, medial ligament complex, tibiofibular syndesmosis ligaments, and subtalar ligaments, are essential for maintaining ankle stability and preventing issues related to instability. Tendons in the ankle, such as the peroneal, flexor, extensor, plantar, and posterior tendons, facilitate connections between muscles and bones and translate joint movements. Despite their structural similarities, these collagenous connective tissues have distinct functions in the musculoskeletal system, with tendons transmitting muscle forces and ligaments providing joint stability and sensory feedback. Understanding the anatomy, biomechanics, and potential injuries of these ligaments and tendons is crucial for accurate diagnosis, treatment planning, and rehabilitation strategies in ankle-related pathologies.
3. Muscles
The ankle is surrounded by several important muscles that work together to provide movement and stability. The primary muscle groups involved in ankle function are the anterior compartment, lateral compartment, and posterior compartment. The anterior compartment contains the tibialis anterior, extensor digitorum longus, and extensor hallucis longus muscles, which are responsible for dorsiflexion (lifting the foot upward) and inversion (turning the sole of the foot inward). The lateral compartment includes the peroneus longus and peroneus brevis muscles, which aid in eversion (turning the sole of the foot outward) and plantarflexion (pointing the foot downward). The posterior compartment is divided into superficial and deep layers. The superficial layer contains the gastrocnemius and soleus muscles, which form the calf and are the primary plantarflexors of the ankle. The deep layer includes the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles, which help with inversion and plantarflexion. These muscle groups work in concert to provide the necessary forces for walking, running, and maintaining balance, while also helping to stabilize the ankle joint during various activities.
- Peroneal muscles (peroneus longus and peroneus brevis)
The peroneal muscles, specifically the peroneus longus and peroneus brevis, are important for ankle function. The peroneus longus helps stabilize the transverse arch of the foot and aids in plantar flexion. It originates from the lateral fibula and interosseous membrane. On the other hand, the peroneus brevis originates from the lower fibula and contributes to ankle eversion. Both muscles travel behind the lateral malleolus in a shared synovial sheath. The peroneus longus inserts on the medial cuneiform and the base of the first metatarsal, while the peroneus brevis attaches to the base of the fifth metatarsal. Understanding the detailed anatomy and functions of these peroneal muscles is crucial for effectively diagnosing and treating ankle pathologies.
- Calf muscles (gastrocnemius and soleus)
The calf muscles, specifically the gastrocnemius and soleus muscles, are important for ankle function and overall movement. The anatomical structures of the calf region, such as muscle thickness, fascicle angle, and length, have been shown to have a significant impact on anaerobic power and athletic performance. These muscles are necessary for activities like walking, running, and jumping, as they provide the power and stability needed for propulsion and shock absorption. The Achilles tendon, which connects these muscles to the heel bone, is crucial for transmitting forces and energy during movement. Understanding the complex relationship between the calf muscles, Achilles tendon, and ankle joint is important for predicting athletic performance and preventing injuries. Maintaining a balance between stability and flexibility in these structures is essential for optimal function of the ankle and foot complex.
- Posterior tibialis muscle
The posterior tibialis muscle (PTM) is an important muscle in the ankle region, playing a significant role in various conditions and diagnostic procedures. Research by Elleuch et al. demonstrated the importance of the PTM in diagnosing neurologic lesions that cause steppage gait, emphasizing its role in foot dorsiflexion. Additionally, Pérez-Bellmunt et al. conducted a cadaveric study showing the accuracy and safety of needling the PTM, highlighting its relevance in clinical procedures such as dry needling for spasticity management. Furthermore, Johnson et al. developed a reliable ultrasound technique to measure the cross-sectional area and thickness of the tibialis posterior muscle, providing valuable insights for assessing its morphologic characteristics in medical and research applications. This collective evidence emphasizes the anatomical and functional significance of the posterior tibialis muscle in the complex dynamics of the ankle region.
- Anterior tibialis muscle
The anterior tibialis muscle, an important structure in the ankle joint, is responsible for dorsiflexion and toe extension, playing a significant role in maintaining ankle stability. It is essential for dynamic stabilization during activities such as running and jumping, preventing excessive compensations that can lead to ankle instability and toe deformities. Studies have shown that the attachment site of the tibialis anterior muscle on the tibia differs between males and females, impacting its function in power exertion and ankle movements. In cases of chronic ankle instability, changes in muscle recruitment patterns of the anterior tibial muscle have been observed, potentially affecting functional limitations and the risk of recurrent sprains. Understanding the anatomy and function of the anterior tibialis muscle is crucial for effective ankle rehabilitation and injury prevention in both athletic and clinical settings.
4. Nerves
The ankle region contains important nerves that are essential for sensation and motor function. The sural nerve (SN) is a significant distal cutaneous nerve that provides sensation to the lateral foot and ankle. Its course and relationships to anatomical landmarks have been well-documented through in-vivo high-field MRI studies, which offer a more generalizable representation compared to cadaveric studies. Additionally, the deep peroneal nerve and superficial peroneal nerve play crucial roles in innervating the anterior ankle structures. Detailed assessments of their positions relative to tendons and vessels help quantify neurovascular risks during ankle arthroscopies. Furthermore, the posterior tibial nerve and artery bifurcate into various branches, including the plantar and calcaneal nerves and arteries, highlighting the complexity and variability of neurovascular structures on the medial side of the ankle. These intricate nerve distributions emphasize the importance of precise anatomical knowledge for clinical diagnosis and treatment of ankle-related pathologies.
5. Blood vessels
The anatomical structures of the ankle related to blood vessels are essential for understanding potential complications and surgical outcomes. Studies have emphasized the neurovascular structures of the medial ankle, including the branching patterns and points of the posterior tibial nerve and artery, as well as the calcaneal nerves and arteries, which may vary in number and origin. Additionally, research on the arterial supply of the talus has demonstrated the impact of total ankle replacement on the vascularization of the talus, particularly regarding potential vessel damage from specific implant designs. Understanding the intricate anatomy and biomechanics of the ankle, including the arterial supply and potential neurovascular structures encountered, is crucial for clinicians to minimize complications and achieve favorable surgical outcomes.
Common issues or conditions that affect ankles
Various foot deformities and pathologies can affect ankles, impacting individuals of all ages. These issues include congenital conditions such as clubfoot and cavus foot, as well as acquired problems like hallux valgus, hallux rigidus, and metatarsalgia. In children and adolescents, foot abnormalities like flatfoot, tarsal coalition, and juvenile hallux valgus can impede participation in sports activities. Additionally, ankle and foot biomechanical dysfunctions resulting from these deformities often cause pain, discomfort, and mobility challenges, affecting activities such as walking, running, and jumping. Timely diagnosis and appropriate management are essential to effectively address these issues and prevent long-term complications.
Different causes ankle disorders
There are various causes of ankle disorders, including:
1. Sprains and strains
Ankle disorders, particularly sprains and strains, can result from various causes such as direct athletic movements, repetitive motions, improper footwear, and underlying conditions such as rheumatoid arthritis, spondyloarthropathies, and complications related to diabetes. These injuries are common in sports, with ankle sprains alone accounting for a significant portion of sports-related injuries. To accurately diagnose and treat ankle sprains, a comprehensive approach involving evaluation of clinical history, physical examinations, and advanced imaging techniques such as Compressed Sensing MRI, 3D MRI, and CT arthrography is essential. While conservative management is often effective for ligament sprains, persistent symptoms may indicate more serious underlying conditions that require timely and appropriate intervention for optimal outcomes.
2. Fractures
Ankle fractures can occur due to various causes, resulting in a range of disorders and complications. Traumatic deformity, pseudoarthrosis, subluxation of the foot, contracture, and arthrosis are common outcomes of ankle fractures, often requiring surgical intervention. Sports-related injuries, both traumatic and degenerative, frequently affect the ankle due to the biomechanical stresses experienced during activities such as soccer, athletics, and basketball, leading to sprains, fractures, impingement syndrome, and tendon injuries. Additionally, chronic ankle joint injuries can present as osteoarthritis, hindfoot and midfoot issues like planovalgus deformity, and forefoot problems such as hallux valgus and metatarsalgia. Understanding the various causes and effects of ankle fractures is essential for accurate diagnosis and effective management to reduce long-term disability and improve patient outcomes.
3. Arthritis
Ankle disorders, particularly arthritis, can arise from various causes as outlined in research contexts. Post-traumatic changes, accounting for approximately 65-80% of cases, are a primary factor in the development of tibiotalar arthritis, often associated with chronic malalignment, chondral joint damage, chronic instability, and microinstability. Additionally, primary ankle arthritis, although rare, may be linked to underlying conditions such as haemochromatosis, while new cases of inflammatory arthritis in the ankle are more likely due to undifferentiated arthritis or spondyloarthritis rather than rheumatoid arthritis. Moreover, previous trauma to the ankle joint, such as fractures, recurrent sprains, and osteochondral injuries, significantly increases the risk of ankle osteoarthritis, with pain and functional limitations commonly presenting symptoms. Understanding these diverse causes is essential for accurate diagnosis and effective management of ankle arthritis.
4. Tendinitis
Ankle disorders, such as tendinitis, can arise from various causes, including overuse, trauma, degeneration, and inflammatory conditions. Tendinitis in the foot and ankle region can be caused by repetitive strain, inappropriate footwear, or underlying systemic diseases such as rheumatoid arthritis or spondyloarthropathies. Commonly affected tendons include the Achilles tendon and the peroneal tendons, with injuries ranging from tendinitis to complete ruptures. Treatment for tendinitis typically involves a combination of rest, physical therapy, orthotic support, and, in severe cases, surgical interventions. Accurate diagnosis through physical examination, imaging, and history-taking is essential to tailor the treatment plan to address the underlying cause and extent of the tendon injury.
5. Bursitis
Ankle bursitis can result from various causes, including chronic microtrauma, acute trauma/hemorrhage, inflammatory conditions such as gout or rheumatoid arthritis, and infections like septic bursitis. Mechanical damage from injury, gout, or excessive load on the ankle joint can also cause bursitis. Additionally, autoimmune processes may trigger ankle bursitis, leading to the use of corticosteroids for treatment. Foot pain, often associated with inappropriate footwear, can lead to chronic foot and ankle pain, with conditions like rheumatoid arthritis, spondyloarthropathies, and gout commonly affecting the foot. Furthermore, lateral premalleolar bursitis, although rare in English literature, can be linked to lateral ankle instability and may require surgical intervention for successful treatment.
6. Infection
Ankle disorders caused by infection can arise from various sources, as outlined in the literature. Infections can result in significant morbidity in the ankle joint, with conditions such as foot infections in diabetic patients and thrombophlebitis contributing to heel and rearfoot pain. Additionally, infectious causes of joint degeneration, including inflammatory conditions and infections, are recognized as secondary factors in the development of ankle osteoarthritis. Proper diagnosis and management of ankle infections are essential to prevent complications and ensure optimal outcomes. Understanding the diverse causes of ankle infections, ranging from diabetic foot problems to post-traumatic changes, is crucial for developing effective treatment strategies and improving patient quality of life.
7. Nerve compression or injury
Ankle disorders resulting from nerve compression or injury can lead to chronic pain and disability. Peroneal nerve injuries, often caused by compression at the fibular head, can lead to foot drop, with prolonged immobility and habitual leg-crossing being common causes. Rare distal compressions of lower limb nerves, such as tarsal tunnel syndrome and entrapment of various nerves, require thorough evaluation through nerve conduction studies to distinguish them from other conditions like radiculopathies. Peroneal nerve compression, the most common lower limb neuropathy, typically occurs around the fibular head and can be effectively diagnosed using neurophysiological and neuroimaging methods, with conservative treatments like lifestyle modifications and kinesiotherapy often successful. Imaging techniques such as ultrasound and MRI play a crucial role in identifying primary and secondary causes of nerve entrapment in the ankle and foot, aiding in accurate diagnosis and management.
8. Biomechanical issues
Biomechanical issues are a significant cause of ankle disorders, as they can lead to abnormal stress and strain on the ankle joint and surrounding structures. Flat feet, also known as pes planus, is a common biomechanical problem characterized by a collapse of the foot’s arch, causing the entire sole to come into contact with the ground. This can lead to excessive pronation, putting undue stress on the ankle joint and increasing the risk of sprains, tendinitis, and other ankle disorders. On the other hand, high arches, or pes cavus, can result in supination, where the ankle rolls outward, causing instability and a higher risk of ankle sprains. Other biomechanical issues, such as leg length discrepancies, abnormal gait patterns, or poor footwear choices, can also contribute to ankle disorders by altering the normal alignment and function of the ankle joint.
9. Overuse injuries
Overuse injuries are a common cause of ankle disorders, particularly in sports-related activities. Various factors contribute to the onset of these injuries, including repetitive microdamage leading to pain in the affected tissues. In runners, the etiology of overuse injuries is multifactorial, with distance, terrain, footwear, previous injuries, and biomechanical changes such as increased dorsiflexion and eversion of the ankle playing significant roles. Ankle injuries in children, ranging from sprains to fractures, are also prevalent, with physical injuries being crucial to identify due to their potential long-term impact on growth and function. Studies on ankle and foot overuse injuries across various sports disciplines have highlighted common issues in methodology and reporting, emphasizing the need for clear case definitions, detailed assessment procedures, and adequate reporting of sample characteristics to enhance the quality of research in this area.
10. Systemic diseases
Systemic diseases can have a significant impact on the health and function of the ankle joint. Diabetes, for example, can cause peripheral neuropathy, a condition that damages nerves in the extremities, leading to numbness, tingling, and weakness in the ankles and feet. This can increase the risk of ankle injuries and make it more difficult for the body to heal after an injury. Peripheral artery disease, another complication of diabetes and other cardiovascular disorders, reduces blood flow to the ankles and feet, causing pain, cramping, and slow wound healing. Autoimmune disorders, such as rheumatoid arthritis or lupus, can cause systemic inflammation that affects multiple joints, including the ankles. This inflammation can lead to pain, stiffness, and joint damage over time. Other systemic conditions, such as osteoporosis or vitamin D deficiency, can weaken the bones in the ankle, increasing the risk of fractures. Proper management of these underlying systemic diseases is crucial for maintaining ankle health and preventing related disorders.
Sign and symptoms of ankle disorders
Ankle disorders can manifest with a variety of signs and symptoms, which depend on the specific condition and its severity. Common signs and symptoms include:
1. Pain
Ankle disorders manifest with a variety of signs and symptoms, with pain being a common and prominent feature. The pain associated with ankle disorders can range from mild discomfort to severe, debilitating pain. In conditions such as Complex Regional Pain Syndrome (CRPS), patients not only experience intense pain but also exhibit additional symptoms such as allodynia, hyperalgesia, and temperature asymmetry. Ankle pain can be triggered by various events such as sprains, fractures, surgery, or underlying conditions like osteoarthritis, rheumatoid arthritis, and diabetes. Proper diagnosis of ankle pain involves a comprehensive clinical assessment, including identifying the source of pain through physical examination, imaging techniques, and dynamic evaluations. Effective management of ankle pain requires a multidisciplinary approach that includes pharmacologic treatment, rehabilitation, and sometimes surgical interventions.
2. Swelling
Symptoms of ankle disorders, particularly swelling, can indicate various underlying conditions. Swelling in the ankles may be associated with venous disorders, as shown in a study demonstrating that leg discomfort and swelling are common symptoms in such cases. Additionally, foot and ankle disorders, such as osteoarthritis and ankle instability, can present with swelling in the affected area, often accompanied by pain and limited range of motion. In cases of acute painful swelling in both ankles, erythema nodosum may be a potential diagnosis, especially when accompanied by fever and a nodular erythematous eruption on the legs. Proper diagnosis of ankle swelling requires a comprehensive assessment of symptoms, physical examination, and potentially imaging techniques to identify the underlying cause and determine appropriate treatment strategies.
3. Stiffness
Ankle stiffness can be a significant symptom of various disorders, including stiff limb syndrome and stiff-person syndrome. Stiff limb syndrome is characterized by muscle stiffness, painful reflex spasms triggered by stimuli, and continuous motor unit activity in the affected limb. In contrast, stiff-person syndrome presents with ill-defined stiffness, exaggerated startle response, and marked hyperreflexia, often accompanied by plantar flexor signs. These conditions can lead to progressive difficulty in movement, such as walking on uneven surfaces, climbing stairs, and gait instability. Proper diagnosis is crucial, as ankle stiffness can also be associated with other disorders like osteoarthritis, rheumatoid arthritis, and Charcot’s joints, necessitating a thorough clinical assessment and management approach tailored to the specific underlying cause.
4. Instability
Ankle instability is characterized by various signs and symptoms that suggest damage to the ligaments. Chronic ankle instability (CAI) is defined by repeated instances of the ankle giving way, along with pain, swelling, weakness, limited range of motion, and persistent ankle sprains lasting more than a year after the initial injury. Patients with CAI may experience difficulties with balance and postural control, as well as a reduced quality of life, necessitating a comprehensive rehabilitation program that includes exercises to improve mobility, strength training, neuromuscular training, and cognitive behavioral therapy. Medial ankle instability is identified by tenderness, bruising, and swelling around the deltoid ligament, along with a characteristic valgus and pronation deformity that can be relieved by activating the posterior tibial muscle or standing on tiptoe. Accurate diagnosis using imaging techniques such as magnetic resonance imaging (MRI) is essential for identifying ligament damage and associated injuries, which can help guide appropriate treatment interventions.
5. Weakness
Ankle weakness can present as a symptom of various disorders, including conversion disorder, entrapment neuropathy, and other common foot and ankle issues. In conversion disorder, unilateral weakness is linked to a specific neural activation pattern, indicating more complex mental activity compared to simulated weakness in healthy individuals. Entrapment neuropathy of the common peroneal nerve can result in ankle weakness, often following sprains or inversion injuries, with successful decompression providing relief. Additionally, foot and ankle disorders such as osteoarthritis, osteochondral lesions, and instability can contribute to ankle weakness, underscoring the importance of accurate diagnosis and personalized treatment approaches based on symptom severity and patient expectations. Understanding the various causes and neural connections of ankle weakness is essential for effective management and improved patient outcomes.
6. Numbness or tingling
Numbness or tingling in the ankle region can be indicative of various underlying disorders. These symptoms may arise from neuropathies caused by mechanical compression of nerves within osteofibrous tunnels or near ligaments and muscles, as highlighted in a review of nerve entrapments in the lower extremity using diagnostic imaging techniques such as ultrasound and magnetic resonance imaging. Additionally, foot and ankle disorders, including neuropathies, are common and can lead to chronic pain and disability, with pinpointing the source of pain being crucial for diagnosis and subsequent treatment decisions. Furthermore, foot pain, a prevalent issue often seen in women due to inappropriate footwear, can result from overuse, repetitive strain, or conditions like rheumatoid arthritis and spondyloarthropathies, emphasizing the importance of a comprehensive evaluation to identify the root cause of symptoms.
7. Bruising
Ankle disorders that present with bruising often result from various underlying conditions. In youth sports, ankle injuries are common, with ankle sprains being the most frequently occurring acute injury. Unique fracture patterns such as Salter-Harris growth plate fractures are also frequently seen. In cases of acute ankle injuries in children, persistent pain and swelling may indicate non-radiographically evident injuries, with hindfoot bone bruising being a common “occult” lesion diagnosed through MRI. Additionally, chronic foot and ankle pain, particularly in women, can be caused by overuse, repetitive strain, and minor injuries. Conditions like rheumatoid arthritis and spondyloarthropathies often affect the foot. Accurate diagnosis is essential for appropriate treatment, whether through conservative measures or surgical intervention, to effectively address ankle disorders presenting with bruising.
8. Popping or cracking sounds
Ankle disorders that present with popping or cracking sounds can have various underlying causes. While a history of hearing or feeling a crack in the ankle may not necessarily indicate a fracture, it is important to consider other potential issues. For example, snapping of the popliteus tendon in the knee can cause lateral popping and may be mistaken for more common sources of mechanical symptoms. Ultrasound (US) imaging is a crucial tool in evaluating ankle pain, particularly in tendons, ligaments, and nerves, as it offers benefits such as dynamic evaluation and stress testing. Additionally, US is a valuable tool for diagnosing foot and ankle injuries related to sports or overuse, providing a noninvasive and readily available method for assessing conditions such as tendinosis, tenosynovitis, and ligament tears.
9. Difficulty walking
Ankle disorders can present with a variety of signs and symptoms that may result in difficulty walking. Common symptoms include pain, numbness, burning sensations in the feet, bunions, structural deformities, calluses, osteoarthritis in the hindfoot and midfoot, heel pain, and deformities, as well as foot and ankle issues related to high pressure on the metatarsal bones and increased walking time. These conditions can impact mobility, particularly in older individuals, for whom maintaining healthy feet is crucial for independent walking and overall well-being. Clinical manifestations of ankle disorders such as lateral ankle instability, hallux valgus, and osteochondral lesions of the talus can further hinder walking, highlighting the importance of accurate diagnosis and treatment to address the root causes. Recognizing these signs and symptoms is vital for timely intervention and management to enhance walking ability in individuals affected by ankle disorders.
10. Visible deformity
Ankle disorders that present with visible deformities can manifest through various signs and symptoms. These may include congenital conditions such as clubfoot, metatarsus adductus, and tarsal coalition, which are common causes of foot and ankle deformities in children. Additionally, adult ankle disorders such as osteoarthritis, osteochondral lesions, and hindfoot problems like planovalgus or cavovarus deformities can lead to noticeable deformities and pain. Radiologically, anomalies such as ball-and-socket ankle joints, congenital vertical talus, and talo-calcaneal synostosis can also contribute to visible deformities and functional impairments. Furthermore, medial ankle instability can be indicated by valgus and pronation deformities that are accentuated during specific movements, along with tenderness and pain upon palpation. These visible signs play a crucial role in diagnosing and managing ankle disorders effectively.
How are ankle disorders diagnosed?
Ankle disorders, which encompass a wide range of acute and chronic conditions, are diagnosed using a comprehensive approach that combines clinical assessment with advanced imaging techniques. The initial step typically involves a detailed medical history and physical examination, which are crucial for identifying the nature of the ankle pathology, whether it is acute, posttraumatic, or due to overuse. Radiography (X-ray) is essential for diagnosing major ankle pathologies, particularly for detecting fractures and assessing joint alignment. However, for a more detailed view of the ankle’s intricate anatomy, including ligaments, tendons, and cartilage, Magnetic Resonance Imaging (MRI) is highly valuable. Traditional two-dimensional MRI provides good image signal and contrast, but three-dimensional MRI offers superior resolution and the ability to capture images with isotropic voxel size, allowing for a detailed examination of even the smallest anatomical structures and abnormalities. Ultrasound (US) is another important tool, especially useful for its dynamic evaluation capabilities, making it particularly effective for assessing tendons, ligaments, and nerves. In cases where more detailed information is required, computed tomography (CT) and hybrid imaging techniques, which combine anatomical and functional imaging, can provide additional insights into the complex biomechanics and pathology of the foot and ankle. Additionally, the use of telerehabilitation technologies has shown promise in enabling remote musculoskeletal assessments of the ankle, demonstrating high validity and reliability compared to in-person assessments. To gain a comprehensive understanding of ankle articulation pathologies, the development of specialized medical devices aimed at quantifying motions has also been explored, complementing traditional diagnostic methods. Overall, these diagnostic strategies, supported by clinical expertise and technological advancements, help in accurate diagnosis and guide effective management of ankle disorders.
How are ankle disorders treated?
Ankle disorders encompass a wide range of conditions that can significantly impact mobility and quality of life, requiring a comprehensive approach to treatment. For soft tissue disorders, such as ligament and tendon injuries, non-surgical management is often the initial treatment option, focusing on rehabilitation to promote functional recovery and prevent complications. This may involve various rehabilitation techniques tailored to the patient’s specific impairments and symptoms. In cases where conservative treatments are ineffective, surgical interventions may be considered, especially for conditions like osteoarthritis, osteochondral lesions of the talus, and severe ankle instability. Thermal energy delivery systems, such as monopolar radiofrequency systems, have shown promise in treating ligamentous laxity by inducing collagen shrinkage and promoting new collagen growth, providing an alternative to traditional surgical or non-surgical treatments. Robotic devices have been developed for rehabilitation to offer more intensive and cooperative therapy sessions, addressing the limitations of traditional physiotherapy. The complex structure of the human foot and ankle, consisting of bones, joints, muscles, and ligaments, requires a thorough understanding of biomechanics and pathology for effective treatment of various deformities and conditions. Treatment decisions are influenced by factors such as the source of pain, symptom severity, patient expectations, and the presence of comorbid conditions like diabetes mellitus or rheumatoid arthritis, which may require specialized care. Physical treatments, including cryotherapy, magnetic field therapy, and laser therapy, are also used, particularly in the acute stage of injury, to reduce inflammation and pain.
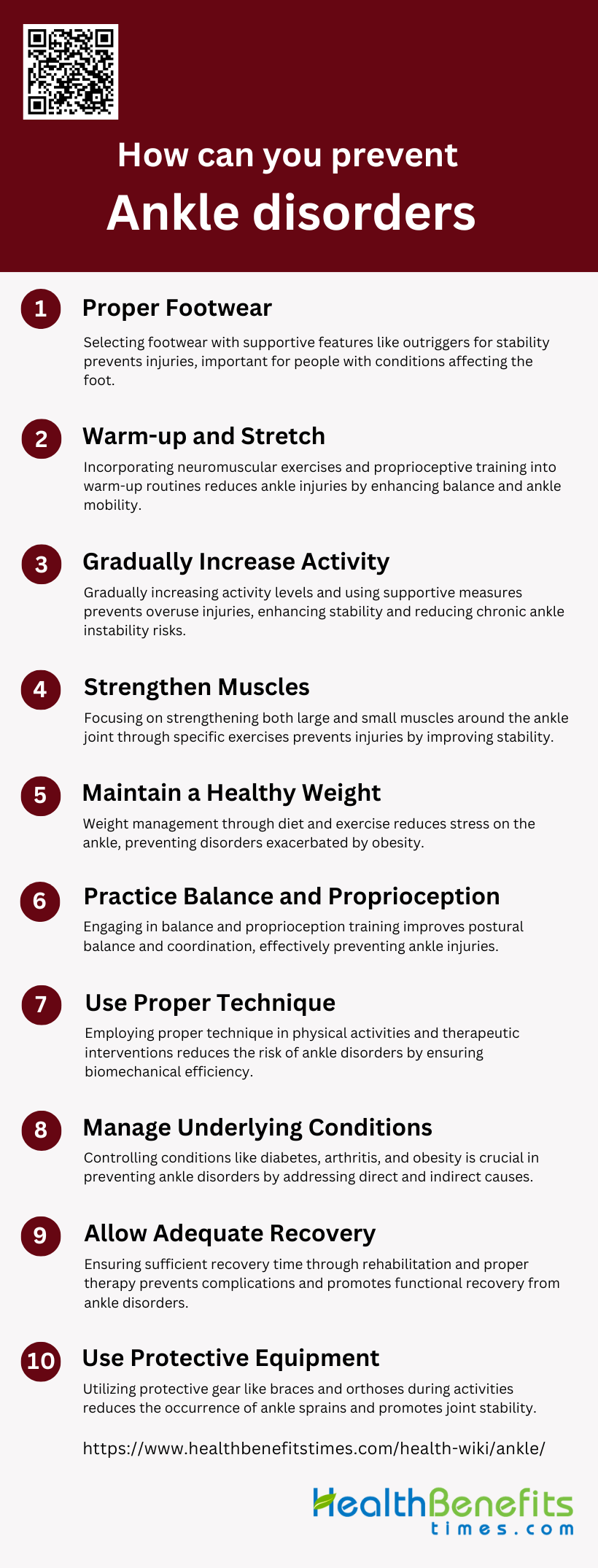
How can you prevent ankle disorders?
Preventing ankle disorders involves a combination of strategies aimed at reducing risk factors and promoting overall ankle health. Some effective prevention methods include:
1. Proper footwear
Preventing ankle disorders effectively requires a comprehensive approach, with a significant focus on selecting and using appropriate footwear. Ankle stability footwear, which includes an outrigger to reduce foot roll, provides lateral mechanical support while maintaining mobility, thus preventing ankle injuries. It is important to note that foot pain and ankle disorders can result from wearing improper footwear, with conditions such as rheumatoid arthritis and gout commonly affecting the foot. Innovative solutions, such as footwear pressure sensors combined with machine learning techniques, have shown promise in predicting ankle angles and preventing injuries in workplace settings by accurately anticipating risky movements. Research has also demonstrated the effectiveness of preventive measures like ankle braces, tape, and proprioceptive training in reducing the occurrence of ankle sprains, particularly in individuals with recurrent ankle issues. Ergonomic considerations, such as using shoe orthoses for arch and metatarsal support, can help mitigate risks associated with prolonged standing and walking. Sport footwear with insoles designed for ankle protection and ventilation can promote ankle stability and prevent excessive twisting that may lead to sprains. Foot and ankle surgeons often recommend specific brands known for their supportive features, emphasizing the importance of professional guidance in selecting appropriate footwear. Advanced footwear designs that incorporate limit elements for selective movement inhibition can provide tailored support and protection for the ankle. Understanding the various foot and ankle disorders is crucial for choosing suitable footwear, and the use of removable devices that attach externally to the leg and footwear can offer additional support to prevent injuries. Overall, these strategies highlight the critical role of proper footwear and supportive devices in preventing ankle disorders and maintaining foot health.
2. Warm-up and stretch
Preventing ankle disorders involves a comprehensive approach that highlights the importance of warm-up and stretching routines. Research has shown that specific warm-up programs, such as those incorporating neuromuscular exercises and proprioceptive training, can significantly decrease the occurrence of ankle injuries in sports like basketball by enhancing balance and ankle range of motion. For example, a new multicomponent neuromuscular warm-up program was found to notably reduce ankle sprain rates among basketball players, demonstrating the effectiveness of targeted warm-up routines in injury prevention. Additionally, integrating movement preparation into warm-up routines has been shown to not only lower sports injuries but also improve flexibility, balance, and performance, further emphasizing the preventive advantages of a comprehensive warm-up. Stretching, especially when combined with aerobic warm-up exercises, has been proven to reduce muscle stiffness and increase joint range of motion, which are essential factors in preventing ankle disorders. However, the effectiveness of warm-up interventions in the workplace for preventing work-related musculoskeletal disorders (WMSDs) remains uncertain, indicating the need for additional high-quality research in this area. Nevertheless, the overall body of evidence supports the use of structured warm-up and stretching routines as effective strategies for decreasing the risk of ankle disorders, enhancing joint function, and improving quality of life among individuals prone to such injuries.
3. Gradually increase activity
Preventing ankle disorders involves a comprehensive approach that focuses on gradually increasing activity to prevent overuse and strain. It is important to incorporate exercises that strengthen the muscles and joints around the ankle to enhance dynamic joint stability and reduce the risk of chronic ankle instability (CAI). Utilizing thermal energy delivery systems, such as low-power radiofrequency (RF) energy, can help treat mild injuries and promote collagen growth to strengthen the ankle. For individuals who engage in activities that involve prolonged standing or walking, using shoe orthoses with a medial longitudinal arch and metatarsal pad can help alleviate metatarsal pressure and reduce the risk of foot and ankle disorders. Engaging in weight-bearing activities is particularly important for the elderly to maintain mobility and prevent osteopenia and osteoporosis, which can lead to serious ankle and foot problems. Specific exercises aimed at preventing ankle joint injuries, especially in high-impact activities, can be beneficial. For those recovering from severe ankle injuries, using a multi-planar motorized wobble board can help improve passive mobility and aid in the healing process. Addressing ergonomic and psychosocial factors, such as job dissatisfaction and physical demands, is also important in preventing ankle and foot disorders. Taking a holistic approach that includes proper diagnosis, effective therapy, and preventive strategies like physiotherapy and orthoses is essential for both treatment and preventing further complications from biomechanical chain reactions.
4. Strengthen muscles
Preventing ankle disorders through muscle strengthening involves a comprehensive approach that targets both the large and small muscles surrounding the ankle joint. The intrinsic and extrinsic muscles of the foot and ankle play critical roles in maintaining biomechanical functions, which, when disrupted by pathological deformities, can lead to pain and mobility difficulties. A bottom-up approach, focusing on strengthening the small muscles crossing the ankle joint, has been suggested to reduce movement and loading at the ankle, knee, and hip, potentially preventing running injuries more effectively than strategies focusing solely on larger muscle groups. This is supported by evidence demonstrating the effectiveness of eccentric strengthening exercises for the gastroc-soleus muscles in relieving pain and improving function in patients with Achilles tendon dysfunction. Additionally, proprioception and balance training are crucial for protecting the articular cartilage of the ankle and preventing recurrent injuries, highlighting the importance of a comprehensive strengthening regimen. External supports such as athletic tape, lace-up stabilizers, and semirigid orthoses have also been identified as effective external methods for preventing ankle injuries by improving flexibility, strength, and proprioception. Moreover, the implementation of neuromuscular training programs, delivered through innovative methods like mobile applications, has shown promise in reducing the number of recurrent ankle sprains, although challenges in program compliance and implementation remain. The integration of biomechanical and neurophysiological adaptations into preventive measures can lead to clinical and functional improvements, ultimately aiding in the prevention of ankle sprain recurrence. Therefore, a comprehensive approach that includes muscle strengthening, proprioception training, and the use of external supports, tailored to the individual’s needs and facilitated by accessible delivery methods, is essential for the effective prevention of ankle disorders.
5. Maintain a healthy weight
Maintaining a healthy weight is a crucial strategy in preventing ankle disorders, as the increased prevalence of obesity has been directly linked to a rise in musculoskeletal disorders, including those affecting the hindfoot and ankle. Overweight individuals demonstrate a significantly higher prevalence of tendinous and ligamentous pathologies in these areas compared to their non-overweight counterparts, underscoring the impact of body mass on the structural integrity of the ankle and foot. The human foot, with its complex structure comprising bones, joints, muscles, ligaments, and other components, bears the weight of the entire body, facilitating movements such as walking, running, and jumping. When this biomechanical function is disrupted by excessive weight, it can lead to pain, deformities, and mobility difficulties. Furthermore, weight-bearing CT scans have improved the understanding of foot and ankle deformities, revealing that conditions like adult-acquired flatfoot deformity are exacerbated by obesity, highlighting the importance of weight management in preventing such disorders. Additionally, the use of technology, such as mobile applications offering neuromuscular training programs, has shown promise in preventing ankle sprain recurrences, a common ankle disorder. These programs, when adhered to, can significantly reduce the risk of recurrence by up to 50%, demonstrating the potential of targeted exercises in conjunction with weight management to maintain ankle health. Therefore, maintaining a healthy weight through a balanced diet and regular exercise is not only beneficial for overall health but is also a key preventive measure against ankle disorders, as it alleviates undue stress on the foot and ankle structures, reducing the risk of pathology and enhancing mobility and quality of life.
6. Practice balance and proprioception
Preventing ankle disorders effectively involves engaging in balance and proprioception training, as supported by a substantial body of research demonstrating its benefits across various athletic disciplines. Proprioceptive training, which aims to enhance perception and maintenance of postural balance through dynamic exercises, has been proven to be highly effective in both preventing joint injuries and aiding in athlete rehabilitation. Protocols lasting at least three weeks have shown significant improvements in postural balance, coordination, and functional performance. Specifically, in martial arts athletes, combining ankle strength training with proprioceptive exercises has been shown to improve dynamic and static balance, effectively preventing ankle injuries. Elite rhythmic gymnasts have also experienced positive effects on postural balance from an 8-week proprioceptive program, although longer durations may be necessary for more conclusive results. Research conducted at the Olmedo Sports Center has demonstrated that proprioception methods significantly reduce ankle discomfort among athletes, while another study found that balance training using sandals improves static balance and proprioception in patients with chronic ankle instability. A case validation study among secondary school basketball players showed that a proprioceptive training program reduced the number of lateral ankle sprains. Quantitative analysis has indicated a correlation between proprioception level and postural control ability, suggesting that proprioception facilitation exercises could positively impact functional balance rehabilitation interventions. Conditioning of the triceps surae muscles, through methods such as muscle cooling and stretching, has been found to influence the perception of ankle joint position, which is essential for maintaining balance. Furthermore, proprioceptive training has been shown to significantly enhance static body balance in healthy individuals, and balance training has been observed to improve ankle joint proprioception in soccer players, indicating its potential in reducing injury risk.
7. Use proper technique
Preventing ankle disorders requires a comprehensive approach that focuses on proper technique, understanding of biomechanics, and the use of supportive interventions. The application of thermal energy, as discussed by Amir M. Khan and Gary S. Fanton, emphasizes the importance of controlled procedures in treating ligament laxity, highlighting the significance of precision in interventions to prevent further injury. Géza Bálint et al. stress the importance of accurate diagnosis and effective therapy, including surgery and physiotherapy, which rely on the correct application of techniques to avoid worsening foot disorders. Advances in arthroscopy techniques for ankle disorders, as described by Carlan K. Yates and William A. Grana, further emphasize the need for meticulous technique in both diagnosis and treatment to reduce complications. Sami F. Rifat and Douglas B. McKeag highlight the role of internal methods such as improving flexibility, strength, and proprioception, as well as external methods like athletic tape and orthoses, in preventing ankle sprains, which are directly linked to proper technique in physical activities. The integration of anatomical and functional imaging for accurate diagnosis, as discussed by R. García Jiménez et al., is crucial for identifying the exact source of pain and guiding the application of appropriate therapeutic techniques. Managing common foot and ankle deformities, as explored by Ganesan Balasankar and Luximon Ameersing, involves understanding the biomechanics of the foot and ankle to apply correct non-operative or surgical management techniques. M. van Reijen and Evert Verhagen’s discussion on preventing ankle injuries in football through specific preventive measures further highlights the importance of technique in avoiding acute lateral ligament injury. William C. Hamilton’s historical perspective on classifying ankle injuries by mechanism reinforces the value of technique in understanding and managing ankle injuries. Heeyoune Jung’s focus on rehabilitation approaches, including proprioception and balance training, underscores the role of technique in promoting functional recovery and preventing recurring injury. Lastly, Dimitrios Stasinopoulos’s study on the effectiveness of technical training in preventing ankle sprains in volleyball players demonstrates the critical role of proper technique in injury prevention. Overall, these insights emphasize the crucial importance of employing proper technique in various aspects of preventing ankle disorders, from diagnosis and treatment to rehabilitation and supportive interventions.
8. Manage underlying conditions
Preventing ankle disorders requires a comprehensive approach that addresses both direct and indirect causes of these conditions. Managing underlying health conditions is a crucial aspect of this strategy. For example, individuals with diabetes mellitus are at a higher risk for foot problems, which can lead to severe ankle disorders if not properly managed. Therefore, controlling blood sugar levels and regularly inspecting the feet are essential preventive measures. Similarly, rheumatoid arthritis and osteoarthritis can cause foot deformities and ankle pain, highlighting the importance of appropriate medical treatment and possibly the use of orthoses to reduce stress on the joints. Obesity has also been identified as a risk factor for foot and ankle disorders, indicating that weight management through diet and exercise could play a preventive role. Engaging in specific rehabilitation exercises and proprioception training can protect the ankle from injury by improving joint stability and function, especially in individuals with a history of ankle injuries or those participating in high-risk activities like football. Addressing biomechanical factors, such as high metatarsal pressure with the use of shoe orthoses, can help reduce the risk of developing foot and ankle disorders. Managing vascular disorders or osteoporosis is crucial for preventing the worsening of foot and ankle problems in individuals with a history of these conditions. Finally, for individuals who spend a significant amount of time walking or standing, especially in occupational settings, ergonomic interventions and supportive footwear can be beneficial in preventing the onset of ankle disorders. Overall, these strategies highlight the importance of a comprehensive approach to managing underlying health conditions and lifestyle factors to effectively prevent ankle disorders.
9. Allow adequate recovery
Preventing ankle disorders requires a comprehensive approach that emphasizes allowing sufficient recovery time, among other strategies. Rehabilitation plays a critical role in promoting functional recovery and preventing complications, with a three-phase system (acute, recovery, and functional phase) tailored to the patient’s condition being particularly effective. Additionally, the significance of adequate rehabilitation following ankle fractures cannot be overstated, as it ensures the complete restoration of support and movement, utilizing methods such as physiotherapy, hydrotherapy, and exercise therapy. The emergence of telerehabilitation offers a promising solution to bridge the service delivery gap, especially in remote areas, ensuring patients have access to necessary rehabilitation services. Furthermore, addressing foot pain and disorders through accurate diagnosis and effective therapy, including physiotherapy and orthoses, is crucial for preventing biomechanical chain reactions that could worsen ankle disorders. The use of ankle recovery devices that facilitate both active and passive exercises can significantly assist in the recovery process. Additionally, the application of thermal energy delivery systems has shown promise in treating ligamentous laxity and promoting new collagen in-growth, which could be beneficial in the recovery phase. Implementing preventive measures, particularly in sports settings, is essential to avoid injuries that could lead to ankle disorders. Factors such as work activity, floor surface characteristics, and the use of shoe orthoses should also be considered to reduce the risk of developing foot and ankle disorders. Complementary ankle training has been shown to effectively prevent injuries in soccer players, underscoring the importance of targeted exercises in prevention strategies. Finally, an anatomical approach to diagnosis and treatment, tailored to the specific needs of the patient, such as the elderly, is essential for effectively preventing and managing ankle disorders.
10. Use protective equipment
Preventing ankle disorders effectively requires a comprehensive approach that includes the use of protective equipment in conjunction with other preventive measures. Various types of protective equipment, such as semi-rigid orthoses, air-cast braces, and high-top shoes, have been shown to significantly reduce the occurrence of ankle sprains, particularly in individuals involved in high-risk sports like soccer and basketball. This reduction is more significant in those with a history of previous ankle sprains, but benefits are also seen in individuals without prior incidents. The design of protective equipment varies, from ankle guards with expansion cloth sleeves and external strengthening cushions to climbing shoes with rubber blocks that limit excessive ankle movement. Innovative designs include devices that connect the leg and foot with a tension device for ankle joint protection without restricting movement, as well as systems with gasbags for impact absorption during falls. Considerations such as floor surface characteristics and shoe orthoses with a medial longitudinal arch are important for reducing foot and ankle disorders in workplace settings. Additionally, the integration of impact-dampening pads in protective gear can provide targeted protection to vulnerable areas around the foot and ankle. While protective equipment is crucial, it is also essential to incorporate preventive strategies like flexibility, strength, and proprioception training, as well as participate in a comprehensive injury prevention program that includes education on injury awareness. By combining the use of protective equipment with physical training and ergonomic practices, individuals can effectively prevent ankle disorders and promote overall well-being during physical activities.