Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that primarily affects the upper and lower motor neurons, leading to muscle weakness, atrophy, and eventual paralysis. The disease typically manifests with symptoms such as muscle twitching, cramping, and stiffness, progressing to more severe impairments in speech, swallowing, and breathing. ALS is often fatal within three to five years of symptom onset due to respiratory muscle paralysis or lung infections. The exact cause of ALS remains unclear, though it is believed to involve a combination of genetic and environmental factors. Current treatments, including riluzole and edaravone, only modestly slow disease progression, and ongoing research is focused on identifying reliable biomarkers and exploring new therapeutic approaches, such as stem cell therapy and the role of gut microbiota in disease progression.
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that primarily affects the upper and lower motor neurons, leading to muscle weakness, atrophy, and eventual paralysis. The disease typically manifests with symptoms such as muscle twitching, cramping, and stiffness, progressing to more severe impairments in speech, swallowing, and breathing. ALS is often fatal within three to five years of symptom onset due to respiratory muscle paralysis or lung infections. The exact cause of ALS remains unclear, though it is believed to involve a combination of genetic and environmental factors. Current treatments, including riluzole and edaravone, only modestly slow disease progression, and ongoing research is focused on identifying reliable biomarkers and exploring new therapeutic approaches, such as stem cell therapy and the role of gut microbiota in disease progression.
Types of Amyotrophic lateral sclerosis
There are several types of ALS, each with distinct characteristics and progression patterns. Below are two types of ALS:
1. Sporadic ALS
Sporadic Amyotrophic Lateral Sclerosis (sALS) is the most common form of ALS, accounting for approximately 90% to 95% of all cases. It occurs without any known family history or genetic predisposition, making its exact cause difficult to pinpoint. Environmental factors, lifestyle choices, and random genetic mutations are believed to contribute to the development of sALS. Patients with sALS typically present with progressive muscle weakness, atrophy, and eventual paralysis. Despite extensive research, the pathogenesis of sALS remains largely unelucidated, complicating efforts to develop targeted therapies. The sporadic nature of the disease poses significant challenges for diagnosis, treatment, and genetic counseling.
2. Familial ALS
Familial Amyotrophic Lateral Sclerosis (fALS) constitutes about 5% to 10% of ALS cases and is characterized by a clear genetic component, often following an autosomal dominant inheritance pattern. This form of ALS is defined by the presence of at least one other affected first- or second-degree relative. Several genes, including SOD1, C9orf72, TARDBP, and FUS, have been implicated in fALS, with mutations in these genes leading to the disease. Genetic testing and counseling are crucial for families affected by fALS to understand their risks and manage the condition. Research into fALS has provided valuable insights into the molecular mechanisms of ALS, aiding in the development of potential therapeutic strategies.
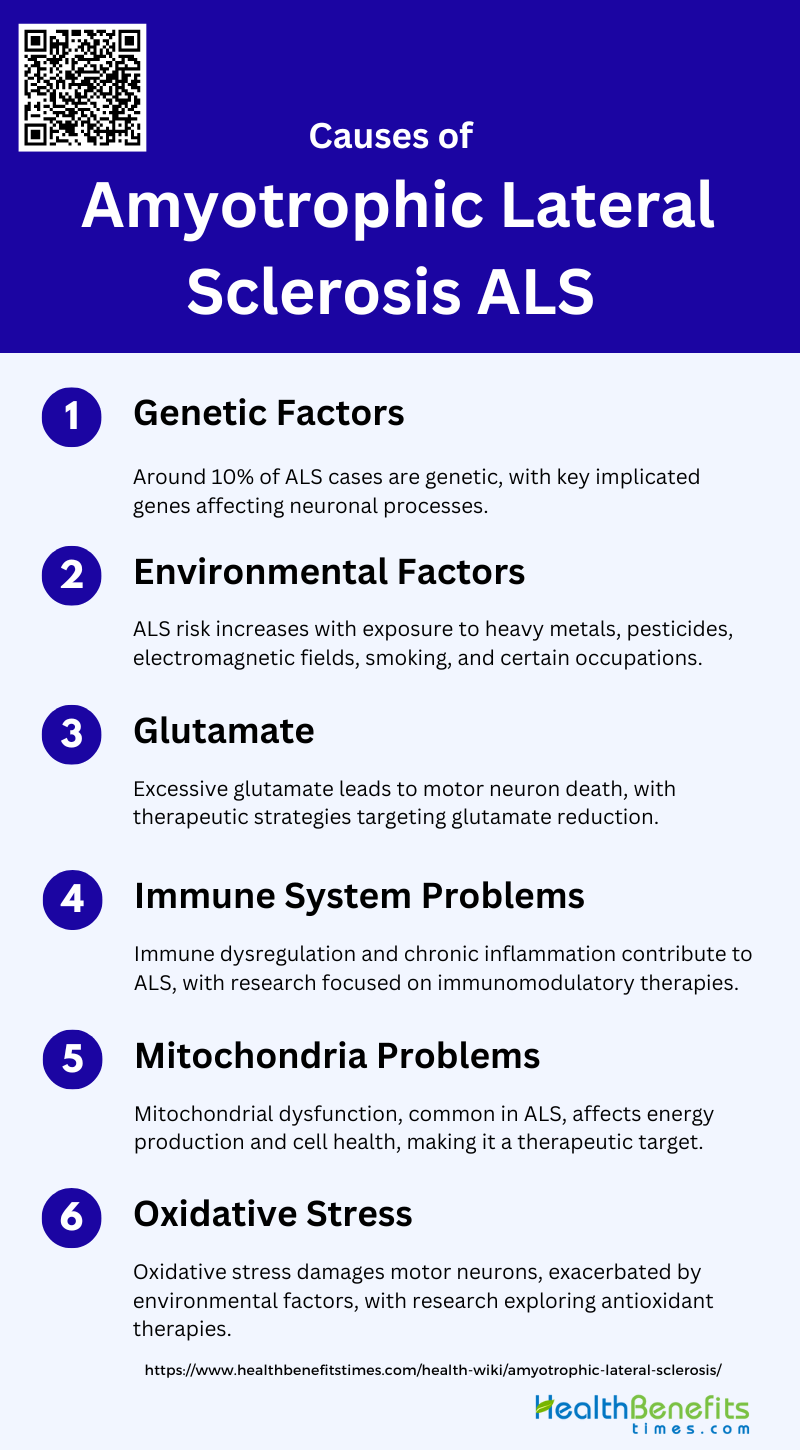
Causes and Risk Factors of Amyotrophic lateral sclerosis
While the exact cause remains unknown, research has identified several genetic and environmental risk factors that may increase the likelihood of developing ALS. Below is a list of the known causes and risk factors associated with ALS:
1. Genetic Factors
Genetic factors play a significant role in the development of amyotrophic lateral sclerosis (ALS). Approximately 10% of ALS cases are familial, with mutations in genes such as SOD1, C9orf72, and TARDBP being commonly implicated. Recent genome-wide association studies (GWAS) have identified 15 risk loci associated with ALS, highlighting the complex genetic architecture of the disease. These genetic variations can affect various cellular processes, including vesicle-mediated transport and autophagy, which are crucial for neuronal health. Understanding these genetic factors is essential for developing targeted therapies and improving disease prognosis.
2. Environmental Factors
Environmental factors are also crucial in the etiology of ALS. Exposure to heavy metals, pesticides, and electromagnetic fields has been linked to an increased risk of developing ALS. Occupational exposures, such as those experienced by military personnel and athletes, have also been associated with a higher incidence of the disease. Additionally, lifestyle factors like smoking and physical activity levels may contribute to ALS risk. While the exact mechanisms remain unclear, these environmental exposures likely interact with genetic predispositions to trigger neurodegeneration.
3. Glutamate
Glutamate excitotoxicity is a well-documented mechanism contributing to motor neuron death in ALS. Elevated levels of glutamate in the synaptic cleft can lead to excessive activation of glutamate receptors, resulting in increased intracellular calcium levels and subsequent neuronal damage. Genetic studies have shown that mutations affecting glutamate transport and metabolism can exacerbate this excitotoxicity, further implicating glutamate in ALS pathogenesis. Therapeutic strategies aimed at reducing glutamate levels or blocking its receptors is currently being explored to mitigate this harmful process.
4. Immune System Problems
Dysregulation of the immune system is another factor implicated in ALS. Inflammatory responses, including the activation of microglia and astrocytes, can exacerbate motor neuron damage. Elevated levels of pro-inflammatory cytokines have been observed in ALS patients, suggesting a role for chronic inflammation in disease progression. Genetic predispositions affecting immune system function may also contribute to ALS susceptibility, highlighting the need for further research into immunomodulatory therapies.
5. Mitochondria Problems
Mitochondrial dysfunction is a key contributor to the pathogenesis of ALS. Mitochondria are essential for energy production, calcium homeostasis, and the regulation of oxidative stress. In ALS, mitochondrial abnormalities, such as impaired calcium buffering and increased membrane permeability, lead to neuronal damage and cell death. These dysfunctions are believed to be a common pathway in both familial and sporadic ALS cases, making mitochondria a promising target for therapeutic intervention.
6. Oxidative Stress
Oxidative stress plays a central role in the degeneration of motor neurons in ALS. It results from an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to detoxify these harmful compounds. Elevated oxidative stress markers have been found in the cerebrospinal fluid, plasma, and urine of ALS patients, indicating systemic involvement. Factors such as smoking, heavy metal exposure, and physical exertion can exacerbate oxidative stress, further contributing to motor neuron damage. Addressing oxidative stress through antioxidants and other therapeutic strategies is a critical area of ongoing research.
Symptoms of Amyotrophic lateral sclerosis
The symptoms of ALS can vary widely among individuals, but they generally follow a pattern of gradual worsening. Below is a list of common symptoms associated with ALS:
1. Muscle Weakness and Paralysis: ALS is characterized by the degeneration of both upper and lower motor neurons, leading to progressive muscle weakness and eventual paralysis.
2. Spasticity: Symptoms of upper motor neuron degeneration include spasticity, which is an abnormal increase in muscle tone or stiffness.
3. Fasciculations and Muscle Cramps: Lower motor neuron degeneration is indicated by fasciculations (muscle twitching) and muscle cramps.
4. Cognitive and Behavioral Changes: ALS can also affect cognitive and behavioral functions, leading to symptoms such as personality changes, irritability, obsessions, poor insight, and deficits in executive function.
5. Non-Motor Symptoms: There is increasing evidence that ALS impacts non-motor functions, including cognition, behavior, sleep, pain, and fatigue. These non-motor symptoms can significantly affect the overall survival and quality of life of patients.
6. Speech and Swallowing Difficulties: Dysarthria (difficulty in speaking) and dysphagia (difficulty in swallowing) are common symptoms due to the involvement of bulbar muscles.
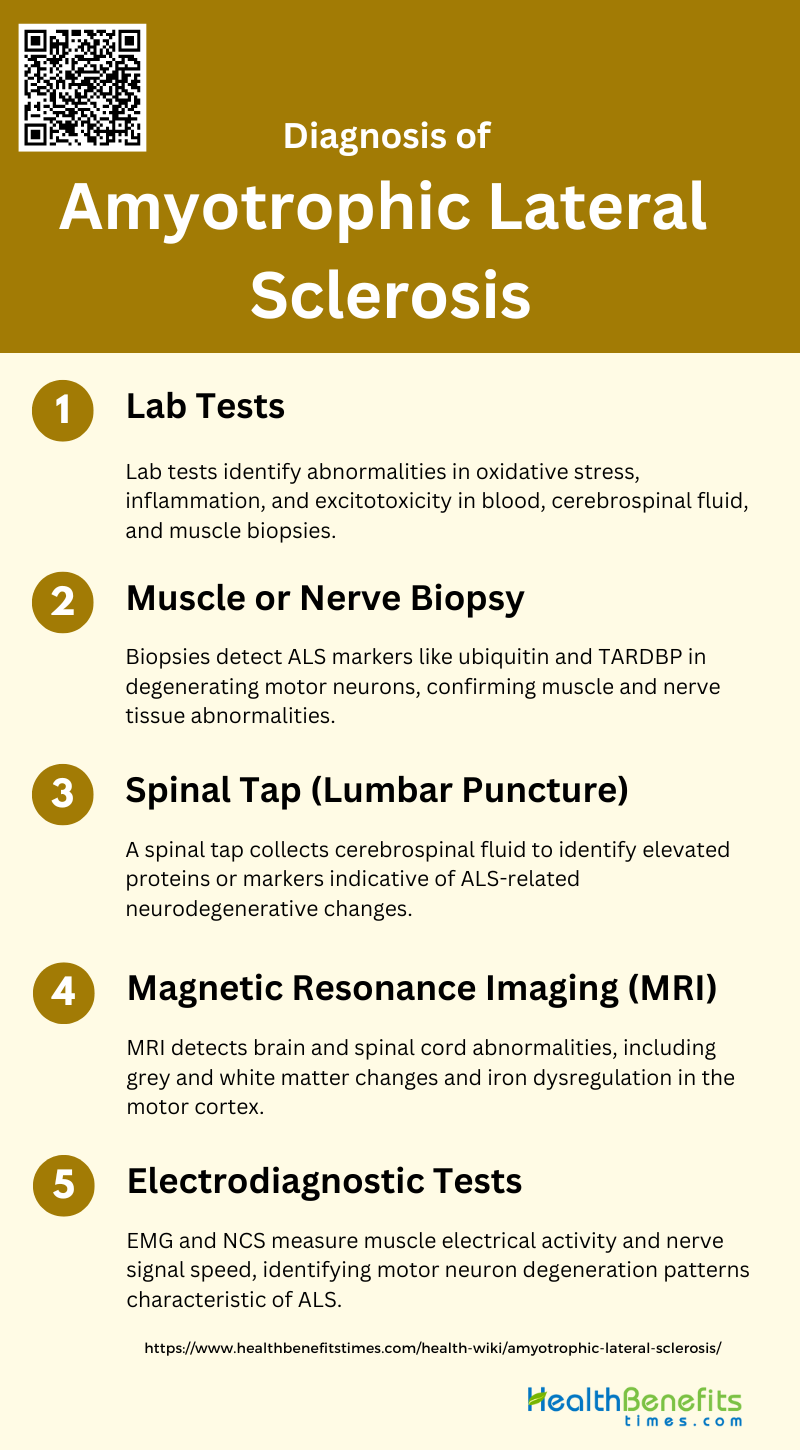
Diagnosis of Amyotrophic lateral sclerosis
Diagnosing amyotrophic lateral sclerosis (ALS) involves a comprehensive evaluation of medical history, neurological examinations, and various diagnostic tests. Since ALS symptoms can mimic other conditions, a thorough and accurate diagnosis is crucial. Below is a list of the key steps and tests involved in diagnosing ALS:
1. Lab Tests
Lab tests for diagnosing ALS often focus on identifying abnormalities in various physiopathologic pathways. These include oxidative stress, inflammation, and excitotoxicity, which can be detected in blood, cerebrospinal fluid, and muscle biopsies. Additionally, neurofilaments in fluid biomarkers are being intensely researched to increase diagnostic accuracy and reduce diagnostic delays.
2. Muscle or Nerve Biopsy
Muscle or nerve biopsies can reveal specific markers of ALS, such as inclusions staining positively for ubiquitin and TAR DNA-binding protein (TARDBP) in degenerating motor neurons. These biopsies help in identifying abnormalities in muscle and nerve tissues, which are crucial for confirming the diagnosis of ALS.
3. Spinal Tap (Lumbar Puncture)
A spinal tap, or lumbar puncture, is used to collect cerebrospinal fluid (CSF) for analysis. Abnormalities in CSF, such as elevated levels of specific proteins or markers, can indicate the presence of ALS. This method is part of the broader diagnostic approach to identify neurodegenerative changes associated with the disease.
4. Magnetic Resonance Imaging (MRI)
MRI is a valuable tool in diagnosing ALS, providing insights into brain and spinal cord changes. Structural and functional MRI can detect abnormalities in cerebral grey and white matter, as well as iron dysregulation in the motor cortex. MRI biomarkers are increasingly used for diagnostic and prognostic purposes, offering a non-invasive method to monitor disease progression.
5. Electrodiagnostic Tests (EMG and NCS)
Electrodiagnostic tests, such as electromyography (EMG) and nerve conduction studies (NCS), are essential in diagnosing ALS. These tests measure the electrical activity of muscles and the speed of nerve signals, helping to identify the characteristic patterns of motor neuron degeneration seen in ALS.
Complications of Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) is a progressive disease that not only affects motor function but also leads to various complications as it advances. These complications can significantly impact the quality of life and require comprehensive management. Below is a list of common complications associated with ALS:
1. Breathing Problems
Breathing problems are a significant complication in amyotrophic lateral sclerosis (ALS) due to the progressive degeneration of motor neurons that control respiratory muscles. As the disease advances, patients often experience respiratory muscle weakness, leading to difficulties in breathing and an increased risk of respiratory infections. This respiratory failure is a primary cause of mortality in ALS patients, typically limiting survival to 2-5 years after disease onset. Management of respiratory issues often involves non-invasive ventilation and other supportive measures to improve quality of life and extend survival.
2. Communication Difficulties
Communication difficulties in ALS arise from the degeneration of motor neurons that control the muscles involved in speech. This leads to dysarthria, characterized by slurred or slow speech that can be difficult to understand. As the disease progresses, patients may lose the ability to speak altogether, necessitating the use of alternative communication methods such as speech-generating devices or eye-tracking technology. Effective management of communication difficulties is crucial for maintaining social interactions and quality of life.
3. Eating Problems
Eating problems in ALS are primarily due to the weakening of the muscles involved in chewing and swallowing, a condition known as dysphagia. This can lead to malnutrition, dehydration, and an increased risk of aspiration pneumonia, which occurs when food or liquid enters the lungs. Nutritional support, including the use of feeding tubes, is often necessary to ensure adequate caloric intake and to prevent complications associated with dysphagia. Multidisciplinary care teams play a vital role in managing these issues to improve patient outcomes.
4. Dementia
Dementia, particularly frontotemporal dementia (FTD), is a recognized complication in a subset of ALS patients. Up to 15% of ALS patients meet the clinical criteria for FTD, which is characterized by changes in behavior, personality, and executive function. The overlap between ALS and FTD is supported by genetic and pathological evidence, with mutations in genes such as C9orf72 being implicated in both conditions. Understanding the cognitive and behavioral aspects of ALS is essential for providing comprehensive care and support to patients and their families.
5. Mobility Issues
Mobility issues are a hallmark of ALS, resulting from the progressive loss of motor neurons that control voluntary muscle movements. This leads to muscle weakness, atrophy, and eventual paralysis, significantly impacting a patient’s ability to perform daily activities. As the disease progresses, patients often require assistive devices such as wheelchairs, walkers, and other mobility aids to maintain independence and quality of life. Physical therapy and occupational therapy are crucial components of the multidisciplinary care approach to manage mobility issues in ALS.
6. Cognitive Changes
Cognitive changes in ALS can range from mild executive dysfunction to more severe impairments that overlap with frontotemporal dementia. These changes may include difficulties with planning, decision-making, and social conduct, as well as personality changes and irritability. Neuroimaging and genetic studies have shown that non-motor systems are also affected in ALS, contributing to these cognitive deficits. Recognizing and addressing cognitive changes is important for providing holistic care and improving the overall quality of life for ALS patients.
Treatment Options for Amyotrophic lateral sclerosis
While there is no cure for ALS, various treatment options can help manage symptoms and improve quality of life. Below are some of the primary treatment options available for ALS patients:
1. Medications
Medications for Amyotrophic Lateral Sclerosis (ALS) primarily focus on slowing disease progression and managing symptoms. Riluzole is the only FDA-approved drug that modestly extends survival by 3-6 months. Edaravone, another approved drug, has shown benefits in a limited population of ALS patients by reducing oxidative stress. Additionally, symptomatic treatments such as muscle relaxants for spasticity and medications for managing pseudobulbar affect are commonly used. Despite these options, the need for more effective disease-modifying therapies remains critical.
2. Physical Therapy
Physical therapy plays a crucial role in managing ALS by maintaining muscle strength and mobility, reducing spasticity, and preventing joint contractures. Regular physical therapy can help slow the progression of muscle weakness and improve the quality of life for ALS patients. Tailored exercise programs, including stretching and low-impact aerobic exercises, are recommended to maintain functional independence for as long as possible. However, the intensity and type of exercises should be carefully monitored to avoid overexertion and fatigue.
3. Assistive Devices
Assistive devices are essential for enhancing the quality of life and independence of ALS patients. These devices range from simple tools like canes and walkers to more advanced technologies such as powered wheelchairs and communication aids. Speech-generating devices and eye-tracking systems can significantly improve communication for patients with severe speech impairments. The timely introduction of these devices can help manage the progressive loss of motor functions and support daily activities.
4. Nutritional Counseling
Nutritional counseling is vital for ALS patients, as maintaining adequate nutrition can impact disease progression and quality of life. Dysphagia, or difficulty swallowing, is a common issue that can lead to malnutrition and weight loss. Nutritional interventions, including the use of high-calorie supplements and modified food textures, are recommended to ensure sufficient caloric intake. In some cases, the placement of a gastrostomy tube may be necessary to provide adequate nutrition and hydration.
5. Speech Therapy
Speech therapy is crucial for ALS patients experiencing dysarthria, a common symptom characterized by slurred or slow speech. Speech therapists work with patients to develop strategies to improve speech clarity and communication. Techniques may include exercises to strengthen the muscles involved in speech, the use of alternative communication methods, and the introduction of speech-generating devices. Early intervention can help maintain effective communication for as long as possible.
6. Assistive Devices (Duplicate Heading)
As previously mentioned, assistive devices are critical in managing ALS. These devices not only aid in mobility but also support daily living activities and communication. The use of adaptive equipment, such as specialized eating utensils and dressing aids, can help patients maintain independence. The integration of these devices into the patient’s care plan should be personalized and regularly updated to match the progression of the disease.
7. Special Equipment
Special equipment, including non-invasive ventilation (NIV) and cough assist devices, plays a significant role in managing respiratory complications in ALS patients. NIV has been shown to improve survival and quality of life by supporting respiratory function. Cough assist devices help clear secretions and prevent respiratory infections, which are common in ALS due to weakened respiratory muscles. The use of these specialized devices should be part of a comprehensive care plan tailored to the patient’s needs.