Amnioinfusion is a medical procedure in which sterile isotonic fluid, such as saline or lactated Ringer’s solution, is introduced into the amniotic cavity via the uterine cervix, typically during labor. This technique is primarily used to address complications arising from low amniotic fluid levels, known as oligohydramnios, which can lead to umbilical cord compression and variable decelerations in fetal heart rate. By increasing the volume of amniotic fluid, amnioinfusion helps to cushion the umbilical cord, thereby stabilizing the fetal heart rate and reducing the risk of oxygen deprivation. Additionally, it can be employed to improve visualization of fetal structures during ultrasound in cases of severe oligohydramnios and to prevent meconium aspiration syndrome, although its efficacy in the latter is debated. The procedure involves the insertion of a catheter into the uterus, through which the fluid is infused, and is monitored closely to ensure the well-being of both the mother and the fetus.
Types of Amnioinfusion
This technique is employed to address various complications and improve fetal outcomes. The different types of amnioinfusion include:
1. Transabdominal Amnioinfusion
Transabdominal amnioinfusion involves the infusion of a saline solution directly into the amniotic cavity through the abdominal wall. This method is particularly useful in cases of oligohydramnios, where the amniotic fluid volume is low, and in situations of umbilical cord compression. Studies have shown that transabdominal amnioinfusion can significantly reduce the incidence of fetal distress and improve neonatal outcomes. For instance, it has been associated with a reduction in neonatal death, neonatal sepsis, and pulmonary hypoplasia in preterm pregnancies complicated by fetal growth restriction and oligohydramnios. Additionally, it has been shown to prolong pregnancy in cases of preterm premature rupture of membranes, thereby allowing time for the administration of corticosteroids to enhance fetal lung maturity.
2. Transvaginal Amnioinfusion
Transvaginal amnioinfusion is performed by infusing a saline solution into the amniotic cavity through the cervix. This method is often used during labor to alleviate umbilical cord compression and reduce the incidence of variable fetal heart rate decelerations. Research indicates that transvaginal amnioinfusion can significantly lower the rates of cesarean sections performed for fetal distress, reduce the occurrence of meconium below the vocal cords, and improve short-term neonatal outcomes such as Apgar scores. It is also beneficial in cases of preterm premature rupture of membranes, where it can improve fetal umbilical artery pH at delivery and reduce persistent variable decelerations during labor.
3. Transcervical Amnioinfusion
Transcervical amnioinfusion involves the infusion of saline solution into the amniotic cavity through a catheter inserted via the cervix. This technique is particularly effective in managing umbilical cord compression during labor. Studies have demonstrated that transcervical amnioinfusion can reduce fetal heart rate decelerations, lower the incidence of cesarean sections for suspected fetal distress, and decrease the length of neonatal and maternal hospital stays. Additionally, it has been shown to reduce the risk of puerperal infection in women with ruptured membranes for more than six hours. This method is also beneficial in improving fetal outcomes in cases of preterm premature rupture of membranes by enhancing fetal umbilical artery pH and reducing the likelihood of neonatal sepsis and pulmonary hypoplasia.
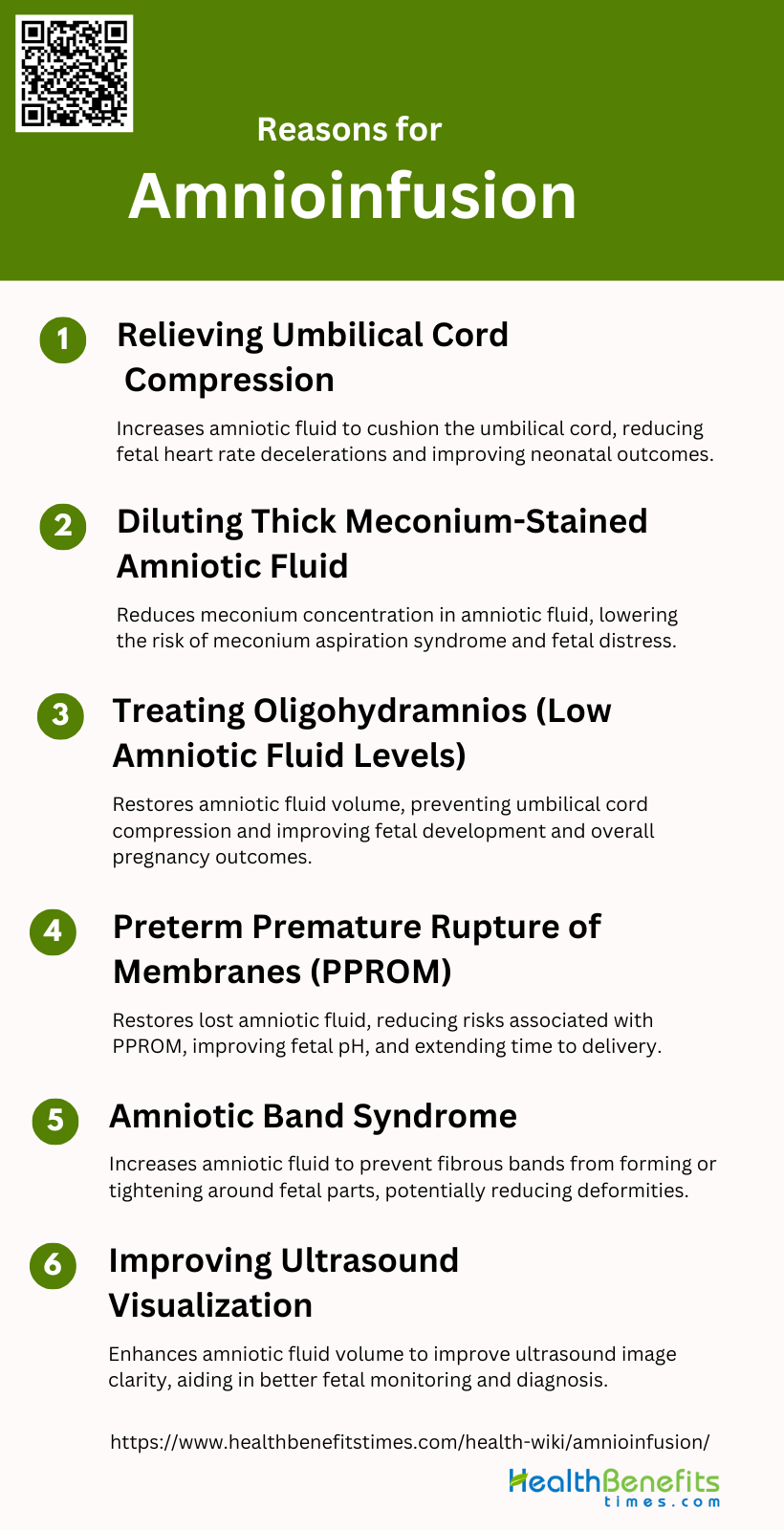
Reasons for Amnioinfusion
This procedure can help improve fetal outcomes and manage various conditions. The primary reasons for amnioinfusion include:
1. Relieving Umbilical Cord Compression
By infusing a solution into the uterine cavity, amnioinfusion increases the volume of amniotic fluid, thereby cushioning the umbilical cord and reducing compression. This intervention has been shown to decrease the frequency of fetal heart rate decelerations and improve neonatal outcomes, such as higher Apgar scores and reduced need for cesarean sections. Additionally, it can improve umbilical artery pH levels, indicating better oxygenation and reduced fetal distress.
2. Diluting Thick Meconium-Stained Amniotic Fluid
Amnioinfusion is also employed to dilute thick meconium-stained amniotic fluid, which can pose a risk of meconium aspiration syndrome (MAS) in newborns. By infusing saline or another solution into the amniotic cavity, the concentration of meconium is reduced, thereby lowering the risk of MAS and other complications. Studies have demonstrated that amnioinfusion significantly decreases the incidence of meconium aspiration, fetal distress, and the need for cesarean sections due to meconium-stained fluid. This intervention is particularly beneficial in settings with limited perinatal surveillance, where it can substantially improve neonatal outcomes.
3. Treating Oligohydramnios (Low Amniotic Fluid Levels)
Oligohydramnios, characterized by low levels of amniotic fluid, can lead to complications such as umbilical cord compression and impaired fetal development. Amnioinfusion helps to restore the amniotic fluid volume, thereby alleviating these risks. Research indicates that both prophylactic and therapeutic amnioinfusion can maintain adequate amniotic fluid levels, reduce the incidence of fetal heart rate decelerations, and improve overall pregnancy outcomes. Continuous amnioinfusion has also shown promise in prolonging the interval between membrane rupture and delivery, thereby enhancing neonatal survival rates.
4. Preterm Premature Rupture of Membranes (PPROM)
Preterm premature rupture of membranes (PPROM) is a significant cause of perinatal morbidity and mortality. Amnioinfusion aims to restore the amniotic fluid volume lost due to membrane rupture, thereby reducing the risks associated with PPROM. Studies have shown that amnioinfusion can improve fetal umbilical artery pH, reduce variable decelerations, and decrease the incidence of neonatal sepsis and pulmonary hypoplasia. Additionally, it can extend the latency period between membrane rupture and delivery, providing more time for fetal development and reducing perinatal mortality.
5. Amniotic Band Syndrome
Amniotic band syndrome is a rare condition where fibrous bands in the amniotic sac constrict fetal parts, leading to deformities or amputations. Amnioinfusion can be used to increase the amniotic fluid volume, thereby reducing the risk of these bands forming or tightening around fetal parts. Although specific studies on amnioinfusion for amniotic band syndrome are limited, the general principle of increasing amniotic fluid to prevent compression and improve fetal movement suggests potential benefits. Further research is needed to establish the efficacy of this intervention for amniotic band syndrome.
6. Improving Ultrasound Visualization
In cases of oligohydramnios or other conditions that reduce amniotic fluid volume, the clarity of ultrasound images can be compromised, making it difficult to assess fetal well-being and anatomy. By infusing a solution into the amniotic cavity, amnioinfusion enhances the fluid volume, thereby improving the quality of ultrasound images. This can facilitate better monitoring and diagnosis of fetal conditions, ultimately contributing to improved pregnancy management and outcomes.
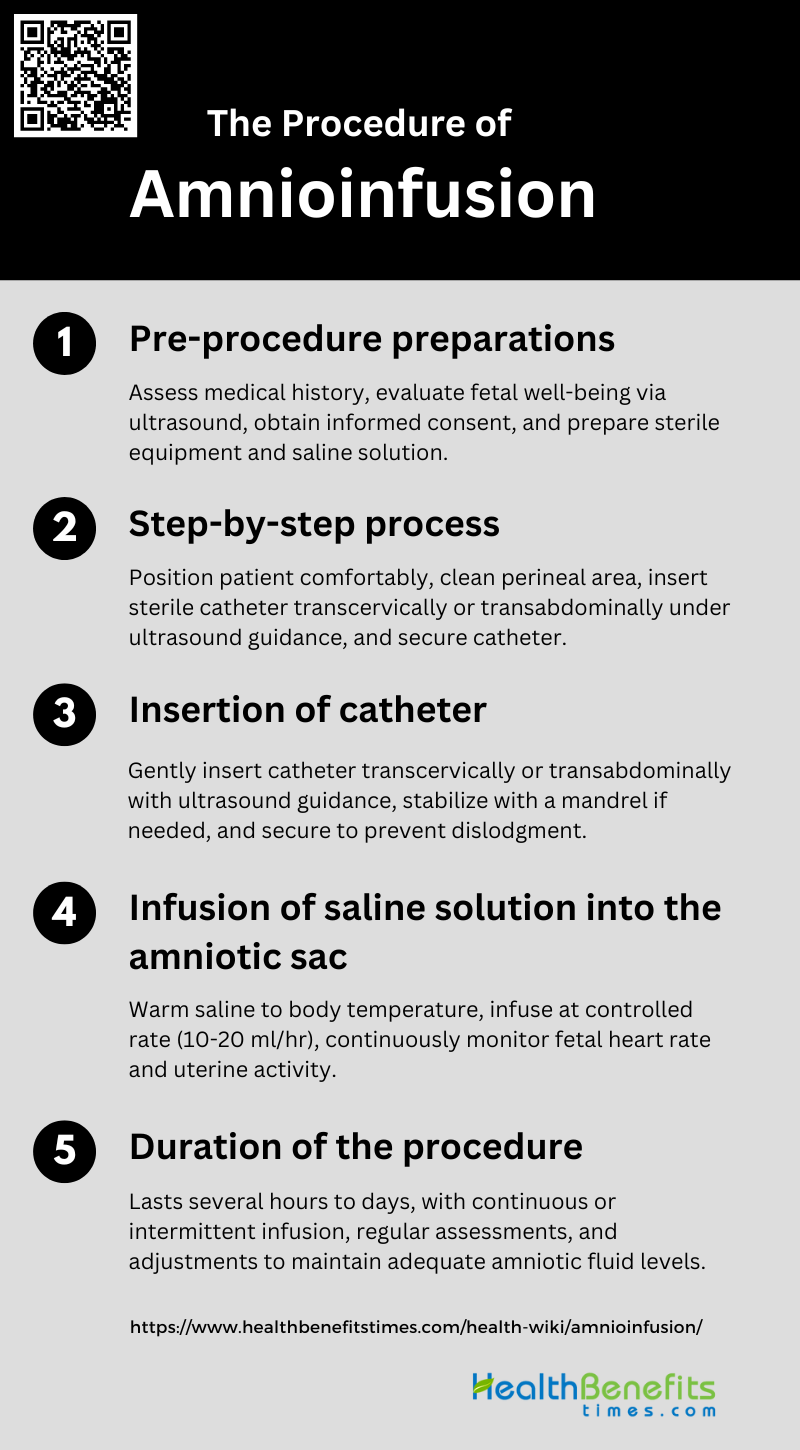
The Procedure of Amnioinfusion
The procedure involves several key steps to ensure its effectiveness and safety. These steps include:
1. Pre-procedure preparations
Before performing amnioinfusion, several preparatory steps are essential to ensure the safety and effectiveness of the procedure. First, a thorough assessment of the patient’s medical history and current pregnancy status is conducted, focusing on indications such as oligohydramnios, variable decelerations, or premature rupture of membranes. Ultrasound is used to evaluate the amniotic fluid volume and fetal well-being. Informed consent is obtained after discussing the potential benefits and risks, including infection and uterine contractions. Sterile technique is paramount, and all necessary equipment, including a sterile catheter and saline solution, is prepared in advance.
2. Step-by-step process
The amnioinfusion procedure involves several critical steps. Initially, the patient is positioned comfortably, usually in a semi-recumbent position, to facilitate access to the cervix or abdomen, depending on the chosen route for catheter insertion. The perineal area is cleaned with an antiseptic solution to minimize infection risk. A sterile catheter, often a Foley catheter, is then inserted transcervically or transabdominally into the amniotic cavity. The catheter is carefully advanced under ultrasound guidance to ensure proper placement and avoid injury to the fetus or uterine wall. Once the catheter is in place, it is secured to prevent dislodgment during the infusion process.
3. Insertion of catheter
The insertion of the catheter is a delicate part of the amnioinfusion procedure. For transcervical insertion, a Foley bladder catheter is commonly used. The catheter is gently introduced through the cervix into the amniotic cavity, often requiring stabilization by a mandrel for easier insertion. In cases where a transabdominal approach is preferred, the catheter is inserted through the abdominal wall under continuous ultrasound guidance to ensure accurate placement and avoid complications. The catheter is then secured to prevent movement, which could disrupt the infusion process or cause discomfort to the patient.
4. Infusion of saline solution into the amniotic sac
Once the catheter is correctly positioned, the infusion of saline solution begins. The saline is typically warmed to body temperature to prevent inducing uterine contractions. The infusion rate is carefully controlled, usually between 10 to 20 ml/hr, to gradually increase the amniotic fluid volume without causing rapid changes that could stress the fetus or uterus. Continuous monitoring of the fetal heart rate and uterine activity is essential throughout the infusion to detect any adverse reactions promptly. The goal is to maintain an adequate amniotic fluid level, improving fetal well-being and reducing complications such as variable decelerations.
5. Duration of the procedure
The duration of the amnioinfusion procedure can vary depending on the clinical situation and the response to the infusion. Typically, the procedure may last from several hours to a few days, with continuous or intermittent infusion as needed to maintain adequate amniotic fluid levels. In some cases, the infusion may be maintained until delivery if the underlying condition, such as oligohydramnios, persists. Regular assessments are conducted to monitor the amniotic fluid volume and fetal condition, adjusting the infusion rate as necessary to ensure optimal outcomes. The procedure is generally well-tolerated, with minimal complications reported.
Benefits of Amnioinfusion
Amnioinfusion is a procedure performed during labor to introduce fluid into the amniotic sac, offering several advantages for both the mother and the fetus. This intervention can help manage complications and improve overall outcomes. The key benefits of amnioinfusion include:
1. Potential to Reduce Fetal Distress: Amnioinfusion is associated with a decreased risk of fetal distress, particularly by reducing variable fetal heart rate decelerations during labor.
2. Decreased Risk of Meconium Aspiration Syndrome: Amnioinfusion can dilute meconium in the amniotic fluid, reducing the risk of meconium aspiration syndrome, especially in settings with limited perinatal surveillance.
3. Improved Outcomes in Certain High-Risk Pregnancies: In pregnancies complicated by oligohydramnios or preterm premature rupture of membranes, amnioinfusion has shown to improve neonatal outcomes by reducing variable decelerations and improving umbilical arterial pH.
4. Reduction in the Incidence of Cesarean Sections: Amnioinfusion has been linked to a reduction in the overall rate of cesarean sections, particularly in cases of suspected umbilical cord compression and fetal distress.
5. Reduction of Variable Fetal Heart Rate Decelerations: The procedure significantly decreases the incidence and severity of variable fetal heart rate decelerations during both the first and second stages of labor.
6. Improved Neonatal Outcomes: Amnioinfusion is associated with better short-term neonatal outcomes, including higher Apgar scores and reduced need for neonatal intensive care unit admission.
7. Management of Oligohydramnios: Prophylactic amnioinfusion in cases of oligohydramnios has been shown to reduce the frequency and severity of variable decelerations and improve umbilical arterial pH at delivery.
8. Reduction in Maternal Postpartum Endometritis: The procedure has been associated with a lower incidence of maternal postpartum endometritis, although the evidence is limited and further research is needed.
Risks or complications of amnioinfusion
Amnioinfusion, while beneficial in many cases, carries certain risks and potential complications that must be carefully considered. These risks can affect both the mother and the fetus, necessitating close monitoring during and after the procedure. The primary risks or complications of amnioinfusion include:
1. Infection Risk
The procedure involves introducing a solution into the uterine cavity, which can potentially introduce pathogens. Studies have shown that while amnioinfusion can reduce neonatal sepsis and puerperal sepsis in some cases, the risk of infection remains a significant concern. For instance, one study noted a reduction in neonatal sepsis with transabdominal amnioinfusion, but the overall risk of infection during pregnancy and puerperium was not significantly higher in the amnioinfusion group compared to the control group. However, the potential for introducing bacteria during the procedure necessitates careful monitoring and sterile techniques to mitigate this risk.
2. Premature Rupture of Membranes
Premature rupture of membranes (PROM) is a critical complication associated with amnioinfusion. The procedure aims to restore amniotic fluid volume, but it can inadvertently cause or exacerbate membrane rupture. Research indicates that while amnioinfusion can delay delivery and improve neonatal outcomes in cases of preterm PROM, it does not significantly reduce perinatal mortality. Additionally, the procedure’s effectiveness in prolonging pregnancy and improving outcomes in cases of second-trimester PROM remains unproven, with studies showing no significant reduction in perinatal mortality. Therefore, the risk of PROM must be carefully weighed against the potential benefits of amnioinfusion.
3. Uterine Overdistension
Uterine overdistension is another potential complication of amnioinfusion. The infusion of large volumes of fluid into the uterine cavity can lead to excessive stretching of the uterine walls, which may cause discomfort, uterine contractions, or even preterm labor. Studies have shown that while amnioinfusion can improve fetal heart rate patterns and reduce the incidence of variable decelerations, it must be performed with caution to avoid overdistension. Proper monitoring of the infusion volume and the patient’s response is crucial to prevent this complication and ensure the safety of both the mother and the fetus.
4. Fetal Heart Rate Abnormalities
Fetal heart rate abnormalities are a significant concern during amnioinfusion. The procedure aims to alleviate umbilical cord compression and improve fetal heart rate patterns, but it can also introduce new risks. Research has demonstrated that amnioinfusion can reduce the frequency of variable and late decelerations, thereby improving neonatal outcomes. However, the procedure must be carefully managed to avoid exacerbating fetal distress. Continuous fetal monitoring during amnioinfusion is essential to detect and address any abnormalities promptly, ensuring the well-being of the fetus throughout the procedure.
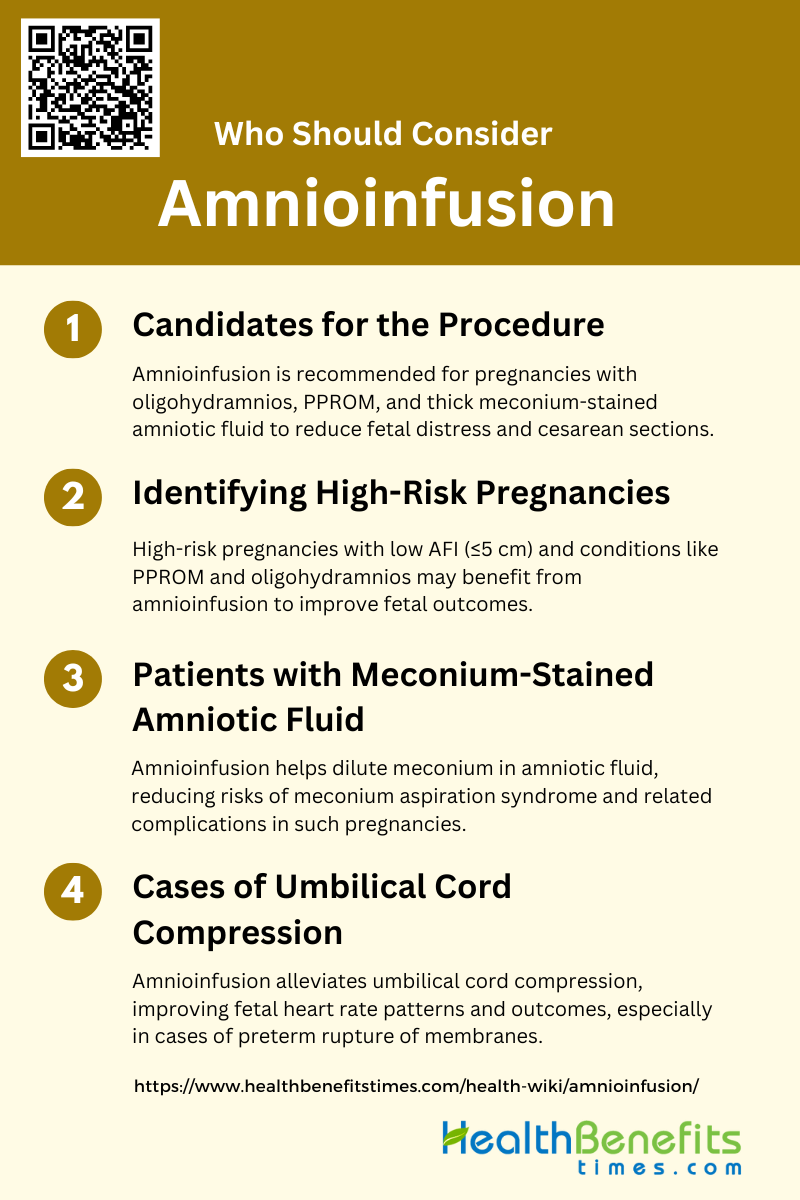
Who Should Consider Amnioinfusion?
Amnioinfusion is a medical procedure used during labor to introduce fluid into the amniotic sac, primarily to address specific complications and improve fetal outcomes. It is typically recommended for certain high-risk pregnancies and specific conditions. Individuals who should consider amnioinfusion include:
1. Candidates for the Procedure
Amnioinfusion is primarily considered for pregnancies complicated by conditions such as oligohydramnios, preterm premature rupture of membranes (PPROM), and thick meconium-stained amniotic fluid. For instance, in cases of oligohydramnios at term, transabdominal amnioinfusion has been shown to reduce the incidence of fetal distress and cesarean sections due to fetal distress. Additionally, amnioinfusion is used in pregnancies with PPROM before 26 weeks of gestation to improve perinatal outcomes by reducing the risk of chorioamnionitis and increasing the latency period between membrane rupture and delivery. Therefore, candidates for amnioinfusion include those with oligohydramnios, PPROM, and meconium-stained amniotic fluid.
2. Identifying High-Risk Pregnancies
High-risk pregnancies that may benefit from amnioinfusion include those with a low amniotic fluid index (AFI) of ≤5 cm, which is often associated with adverse perinatal outcomes. However, studies have shown that high-risk pregnancies with an AFI of ≤5 cm do not necessarily have higher rates of intrapartum complications compared to those with an AFI >5 cm. Nonetheless, in cases of PPROM, amnioinfusion has been associated with improved fetal outcomes, such as reduced neonatal sepsis and pulmonary hypoplasia. Therefore, identifying high-risk pregnancies involves assessing AFI and the presence of conditions like PPROM and oligohydramnios.
3. Patients with Meconium-Stained Amniotic Fluid
This procedure helps dilute the meconium, thereby reducing the risk of meconium aspiration syndrome and other related complications. Studies have shown that amnioinfusion in cases of thick meconium-stained liquor is associated with a reduction in heavy meconium staining, variable fetal heart rate decelerations, and overall cesarean sections. Additionally, it has been found to decrease the incidence of meconium aspiration syndrome and neonatal hypoxic-ischemic encephalopathy, especially in settings with limited perinatal surveillance. Thus, patients with meconium-stained amniotic fluid are prime candidates for amnioinfusion.
4. Cases of Umbilical Cord Compression
The infusion of saline into the amniotic cavity helps to cushion the umbilical cord, thereby alleviating compression and improving fetal heart rate patterns. For example, in pregnancies with preterm rupture of membranes, amnioinfusion has been shown to reduce the number of severe fetal heart rate decelerations during labor. Additionally, it has been associated with improved fetal umbilical artery pH at delivery and reduced persistent variable decelerations during labor. Therefore, amnioinfusion is a valuable intervention in cases of umbilical cord compression to improve fetal outcomes.