Amniocentesis is a prenatal diagnostic procedure typically performed between the 15th and 20th weeks of pregnancy to detect genetic abnormalities and other health conditions in the developing fetus. During the procedure, a thin needle is inserted through the pregnant woman’s abdomen and into the amniotic sac surrounding the fetus to extract a small sample of amniotic fluid. This fluid contains fetal cells and other substances that can be analyzed to check for chromosomal disorders like Down syndrome, genetic conditions such as cystic fibrosis, and neural tube defects like spina bifida. Amniocentesis is generally offered to women who are at higher risk of having a baby with certain birth defects, including those over 35 years old or with a family history of genetic disorders. While the procedure provides valuable diagnostic information, it does carry a small risk of complications, including miscarriage, which is why it is typically only recommended when there is a significant chance of detecting a problem.
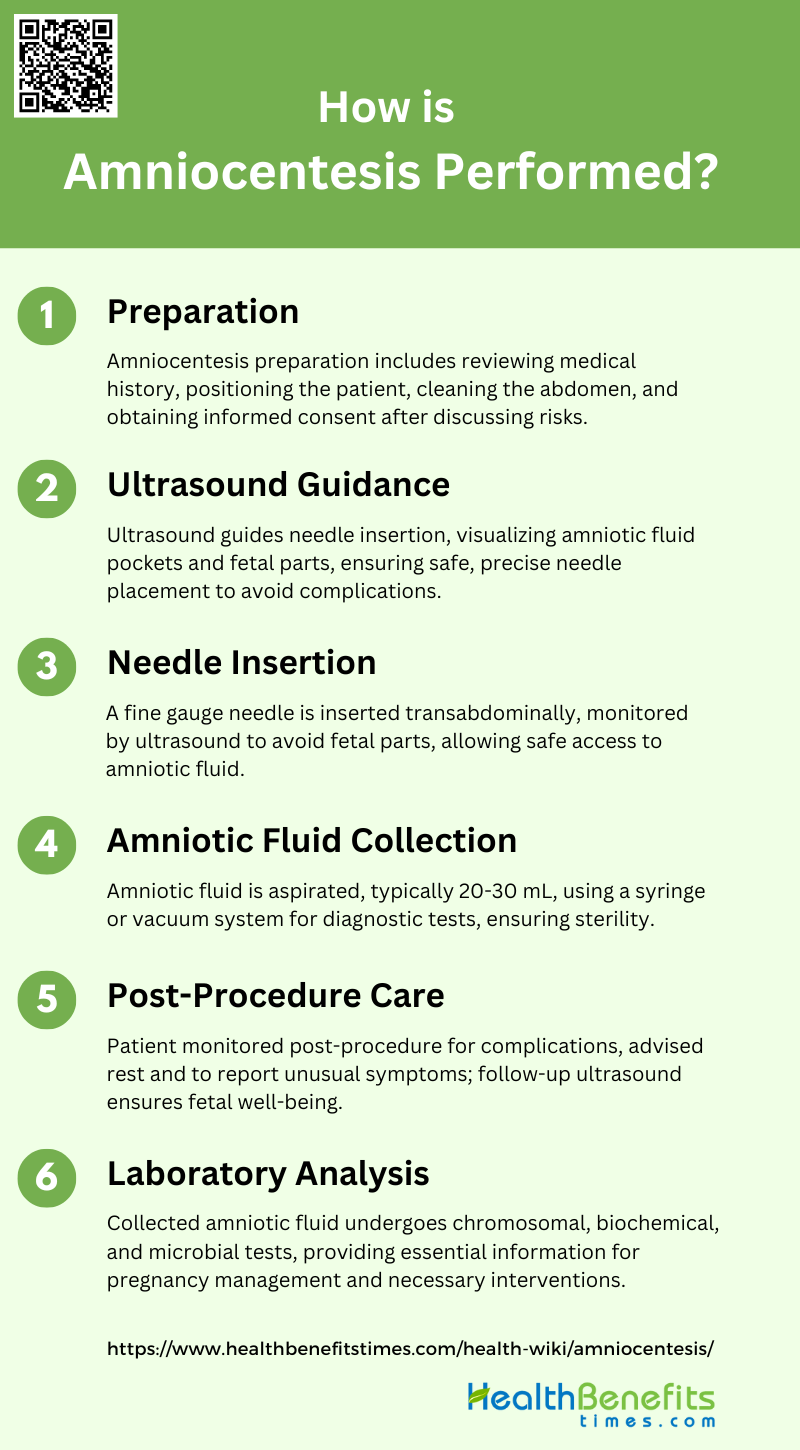
How is Amniocentesis Performed?
Amniocentesis is a medical procedure used primarily in prenatal diagnosis of chromosomal abnormalities and fetal infections. The process involves extracting a small amount of amniotic fluid from the sac surrounding the fetus for testing. Here are the steps involved in performing amniocentesis:
1. Preparation
Amniocentesis is a prenatal diagnostic procedure typically performed during the second trimester of pregnancy, starting from 16 weeks onwards. The preparation involves a thorough review of the patient’s medical history and indications for the procedure, such as advanced maternal age, abnormal first-trimester screening results, or a history of genetic abnormalities in previous pregnancies. The patient is positioned in a supine position, and the abdomen is cleaned with an antiseptic solution to minimize the risk of infection. Informed consent is obtained after discussing the potential risks and benefits, including the small risk of fetal loss and other complications.
2. Ultrasound Guidance
Ultrasound guidance is crucial for the safe and effective performance of amniocentesis. It helps in identifying the optimal site for needle insertion by visualizing the placenta, amniotic fluid pockets, and fetal parts. Real-time ultrasound ensures that the needle avoids contact with the fetus and placenta, reducing the risk of complications such as fetal injury or placental hemorrhage. The use of Doppler ultrasound can further enhance safety by identifying blood vessels, thus minimizing the risk of vascular injury. Continuous ultrasound monitoring during the procedure allows for adjustments in needle trajectory as needed.
3. Needle Insertion
The needle insertion process involves the use of a fine gauge needle, typically ranging from 20 to 22 gauge, to penetrate the abdominal wall and uterine cavity to reach the amniotic sac. The needle is inserted transabdominally, and its progress is monitored in real-time using ultrasound to ensure it avoids fetal parts and major blood vessels. The choice of needle size can impact the rate of sample contamination, with smaller gauge needles (e.g., 20 G) being associated with lower contamination rates. The needle is advanced carefully until it reaches the amniotic cavity, where amniotic fluid can be aspirated.
4. Amniotic Fluid Collection
Once the needle is correctly positioned within the amniotic cavity, amniotic fluid is aspirated using a syringe or a vacuum aspiration system. The amount of fluid collected is usually around 20-30 mL, which is sufficient for various diagnostic tests, including chromosomal, biochemical, and microbial analyses. The use of a vacuum bottle aspiration system can facilitate the rapid collection of larger volumes of fluid, which is particularly useful in therapeutic amniocentesis. The collected fluid is then transferred to sterile containers for laboratory analysis.
5. Post-Procedure Care
After the procedure, the patient is monitored for a short period to ensure there are no immediate complications such as amniotic fluid leakage, bleeding, or signs of preterm labor. The puncture site is cleaned and covered with a sterile dressing. Patients are advised to avoid strenuous activities for at least 24 hours and to report any unusual symptoms such as severe abdominal pain, fever, or vaginal bleeding. Follow-up ultrasound may be performed to check for any complications and to ensure the well-being of the fetus.
6. Laboratory Analysis
The collected amniotic fluid is sent to the laboratory for various diagnostic tests. Chromosomal analysis, such as karyotyping or more advanced techniques like microarray analysis, can identify genetic abnormalities. Biochemical tests can assess fetal lung maturity, while molecular tests can detect specific genetic disorders. Microbial cultures may be performed to identify any intra-amniotic infections. The results of these tests provide valuable information for the management of the pregnancy and any necessary interventions.
Why is Amniocentesis Done?
It is typically done to detect genetic disorders, chromosomal abnormalities, and infections. Here are some specific reasons why amniocentesis might be recommended:
1. Genetic Testing
Amniocentesis is primarily performed for genetic testing to diagnose chromosomal abnormalities and single-gene disorders in the fetus. This procedure is particularly useful for detecting conditions such as Down syndrome (Trisomy 21) and Trisomy 18, which are common reasons for undergoing amniocentesis. The procedure involves extracting amniotic fluid, which contains fetal cells, to perform karyotype analysis and other genetic tests. This allows for early detection and informed decision-making regarding the pregnancy.
2. Diagnosis of Fetal Infection
By analyzing the amniotic fluid, healthcare providers can detect the presence of infectious agents and assess the severity of the infection. This is crucial for managing conditions that could adversely affect fetal development and pregnancy outcomes. The procedure helps in identifying intra-amniotic infections and inflammation, enabling timely medical interventions.
3. Treatment
In addition to its diagnostic uses, amniocentesis can be therapeutic. For instance, it can be used to perform amnioreduction in cases of polyhydramnios, where there is an excess of amniotic fluid. This helps in relieving maternal discomfort and reducing the risk of preterm labor. The procedure can also be used to administer medications directly to the fetus or amniotic fluid, providing targeted treatment for various conditions.
4. Fetal Lung Testing
By measuring the levels of surfactant in the amniotic fluid, healthcare providers can determine whether the fetal lungs are developed enough to function outside the womb. This information is critical for making decisions about the timing of delivery and the need for interventions to enhance lung maturity.
5. Blood Disorders
Amniocentesis can diagnose blood disorders in the fetus, such as Rh incompatibility and other hematological conditions. By analyzing the amniotic fluid, healthcare providers can determine the fetal blood type and detect any incompatibilities that could lead to hemolytic disease of the newborn. Early diagnosis allows for appropriate management and treatment to prevent complications.
6. Paternity Testing
By extracting fetal cells from the amniotic fluid, DNA analysis can be performed to establish paternity. This is particularly useful in legal and personal contexts where paternity needs to be confirmed before the birth of the child. The procedure provides a reliable method for obtaining fetal DNA without waiting for postnatal testing.
Benefits of Amniocentesis
It is a valuable prenatal diagnostic tool that provides critical information about the health and development of a fetus. It helps in detecting genetic disorders, assessing fetal lung maturity, and identifying infections. Here are some specific benefits of amniocentesis:
1. Early Detection of Genetic Disorders
Amniocentesis is a crucial procedure for the early detection of genetic disorders. By extracting amniotic fluid, which contains fetal cells, it allows for the identification of chromosomal abnormalities such as Down’s syndrome, Pompe’s disease, and other genetic conditions. This early detection is particularly beneficial for high-risk pregnancies, enabling parents to make informed decisions about the pregnancy and prepare for the potential needs of their child. The procedure is typically performed between the 13th and 18th weeks of gestation, providing timely information for early intervention.
2. Accurate Diagnosis
The procedure involves culturing fetal cells from the amniotic fluid, which can then be analyzed for chromosomal and biochemical abnormalities. This method is highly reliable, with a low risk of false positives or negatives, making it a trusted tool in prenatal diagnostics. The accuracy of amniocentesis is further enhanced when combined with ultrasound guidance, which helps in precisely locating the amniotic sac and avoiding complications.
3. Detection of Fetal Infections
Amniocentesis is also valuable for detecting fetal infections, such as congenital toxoplasmosis. By performing polymerase chain reaction (PCR) tests on the amniotic fluid, healthcare providers can identify infections that may not be apparent through other diagnostic methods. This early detection allows for timely therapeutic interventions, potentially reducing the risk of severe complications for both the mother and the fetus. In cases of premature rupture of membranes, amniocentesis can help identify occult intrauterine infections, guiding appropriate clinical management.
4. Informed Decision-Making
The information obtained from amniocentesis empowers parents to make informed decisions regarding their pregnancy. Knowing the genetic and health status of the fetus allows parents to consider various options, including potential medical interventions, lifestyle adjustments, or even the difficult decision of pregnancy termination in severe cases. This informed decision-making process is crucial for preparing emotionally and logistically for the birth and care of a child with special needs.
5. Assessment of Fetal Lung Maturity
By measuring the lecithin/sphingomyelin (L/S) ratio in the amniotic fluid, healthcare providers can determine whether the fetal lungs are developed enough for the baby to breathe independently after birth. This information is critical for deciding whether to administer corticosteroids to accelerate lung development or to plan for immediate neonatal care post-delivery.
6. Management of Blood Disorders
For pregnancies at risk of inherited bleeding disorders, amniocentesis can be performed in the third trimester to guide delivery management. By identifying the presence of bleeding disorders, healthcare providers can plan for safer delivery methods to minimize the risk of intracranial hemorrhage in the fetus. This targeted approach ensures that both the mother and the baby receive the most appropriate care during delivery, reducing the risk of complications.
7. Therapeutic Interventions
Amniocentesis not only aids in diagnosis but also facilitates therapeutic interventions. For instance, in cases of fetal anemia, the procedure can be used to assess the severity of the condition and guide intrauterine transfusions if necessary. Additionally, it can help in the management of other conditions like Rh incompatibility by monitoring bilirubin levels in the amniotic fluid. These interventions can significantly improve fetal outcomes and reduce the risk of long-term complications.
8. Paternity Testing
This is particularly useful in legal and personal contexts where paternity needs to be established before the birth of the child. The procedure provides a reliable and accurate method for determining paternity, which can have significant implications for child support, custody, and inheritance issues.
9. Psychological Reassurance
Undergoing amniocentesis can provide psychological reassurance to expectant parents, especially those with a history of genetic disorders or previous pregnancy complications. The detailed information obtained from the procedure can alleviate anxiety by confirming the health status of the fetus or by preparing parents for any necessary medical interventions. This reassurance can contribute to a more positive pregnancy experience and better mental health for the parents.
Risks of Amniocentesis
While amniocentesis can provide valuable information about the health of a fetus, it is not without risks. These risks can range from minor complications to more serious concerns. Here are some potential risks associated with amniocentesis:
1. Bleeding or Leaking Amniotic Fluid
Amniotic fluid leakage is a recognized risk following amniocentesis, particularly when the procedure is performed before 15 weeks of gestation. Studies indicate that early amniocentesis increases the likelihood of significant amniotic fluid loss, which can compromise the pregnancy and lead to complications such as respiratory disorders, skeletal malformations, and premature birth. Conservative management, including bed rest, is often recommended to mitigate these risks. Persistent leakage beyond two weeks is associated with poor outcomes, necessitating a thorough discussion with the couple regarding the risks of continuing the pregnancy.
2. Miscarriage
The risk of miscarriage following amniocentesis is a significant concern. Research indicates that the procedure-related pregnancy loss rate varies, with some studies reporting a rate of 1.0% and others suggesting a lower rate of 0.6% when concurrent ultrasound guidance is used. Factors such as maternal hypertension, increased body mass index, and multiple needle insertions have been identified as predictors of fetal loss. Early amniocentesis, particularly before 13 weeks of gestation, is associated with a higher risk of miscarriage compared to mid-trimester procedures.
3. Needle Injury
Needle injury to the fetus is a rare but possible complication of amniocentesis. The risk is minimized with the use of concurrent ultrasound guidance, which helps in accurately positioning the needle and avoiding fetal contact. Despite this, there have been case reports of presumed fetal needle trauma, although direct evidence is often lacking. The incidence of such injuries is likely underreported due to diagnostic challenges and the absence of consistent sequelae.
4. Rh Sensitization
Rh sensitization can occur if fetal blood cells enter the maternal circulation during amniocentesis, particularly in Rh-negative women. This can lead to the production of antibodies against the fetal Rh-positive cells, potentially causing hemolytic disease of the newborn in subsequent pregnancies. Preventive measures, such as administering Rh immunoglobulin to Rh-negative women following the procedure, are recommended to mitigate this risk.
5. Infection
Infection is a potential risk associated with amniocentesis, although it is relatively rare. The procedure involves inserting a needle through the abdominal wall and into the amniotic sac, which can introduce bacteria and lead to intra-amniotic infection. Symptoms may include fever, abdominal pain, and uterine tenderness. The use of sterile techniques and concurrent ultrasound guidance can help reduce the risk of infection.
6. Infection Transmission
This is particularly concerning in cases where the mother has a known infection, such as HIV or hepatitis. The procedure can facilitate the transfer of infectious agents into the amniotic fluid, posing a risk to the fetus. Careful consideration and alternative diagnostic methods may be warranted in such cases to avoid this risk.
7. Cramping and Spotting
Cramping and spotting are common minor complications following amniocentesis. These symptoms are usually transient and resolve without intervention. However, they can be distressing for the patient and may require reassurance and monitoring. Reducing physical activity for two weeks post-procedure is recommended to minimize these symptoms and prevent further complications.
8. Injury to the Fetus
Fetal injury during amniocentesis is a rare but serious complication. The risk is mitigated by using continuous ultrasound guidance to ensure accurate needle placement and avoid contact with the fetus. Despite these precautions, there have been reports of fetal injuries, including limb deformities and other trauma. The incidence of such injuries is low, but they underscore the importance of skilled technique and careful monitoring during the procedure.
9. Increased Risk of Clubfoot
There is evidence suggesting an increased risk of clubfoot (talipes equinovarus) following early amniocentesis. This risk is particularly associated with procedures performed before 13 weeks of gestation. The exact mechanism is unclear, but it may be related to the disruption of amniotic fluid dynamics or direct injury to the developing fetus. This finding highlights the importance of timing and technique in minimizing the risk of adverse outcomes.
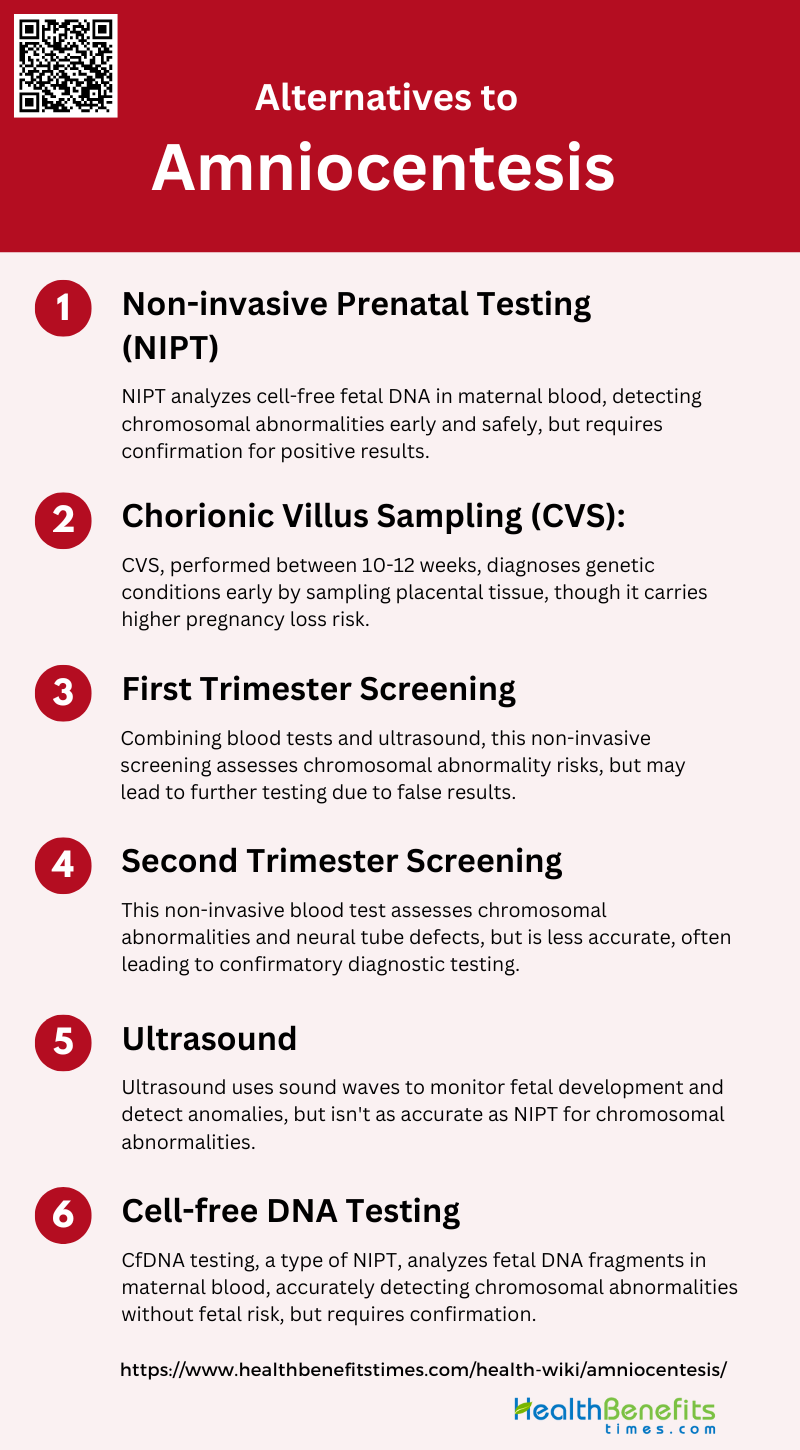
Alternatives to Amniocentesis
For those seeking less invasive options, there are several alternatives to amniocentesis that can provide valuable prenatal information. These alternatives often carry fewer risks and can still offer insights into the health of the fetus. Here are some common alternatives to amniocentesis:
1. Non-invasive Prenatal Testing (NIPT)
Non-invasive prenatal testing (NIPT) is a screening method that analyzes cell-free fetal DNA circulating in the maternal blood. This technique has significantly improved the accuracy of detecting chromosomal abnormalities such as Down syndrome, Edwards syndrome, and Patau syndrome, with a lower risk of false positives compared to traditional screening methods. NIPT can be performed as early as the 10th week of pregnancy and poses no risk to the fetus, making it a safer alternative to invasive procedures like amniocentesis and chorionic villus sampling (CVS). However, it is important to note that NIPT is a screening test and not diagnostic, so positive results often require confirmation through invasive testing.
2. Chorionic Villus Sampling (CVS)
Chorionic villus sampling (CVS) is an invasive diagnostic test that involves obtaining a small sample of placental tissue, usually between the 10th and 12th weeks of gestation. CVS can be performed either transabdominally or transcervically, depending on the location of the placenta and the preference of the healthcare provider. While CVS allows for earlier diagnosis of genetic conditions compared to amniocentesis, it is associated with a higher risk of pregnancy loss and other complications such as sampling and technical failures. Despite these risks, CVS remains a valuable option for early prenatal diagnosis, especially when rapid results are needed.
3. First Trimester Screening
First trimester screening combines a blood test and an ultrasound examination to assess the risk of chromosomal abnormalities in the fetus. This screening is typically performed between the 11th and 14th weeks of pregnancy and measures levels of specific proteins and hormones in the mother’s blood, along with the nuchal translucency (NT) measurement from the ultrasound. While first trimester screening is non-invasive and poses no risk to the fetus, it is not as accurate as NIPT and may result in false positives or negatives. Positive results from first trimester screening often lead to further diagnostic testing, such as CVS or amniocentesis, to confirm the findings.
4. Second Trimester Screening
Second trimester screening, also known as the quad screen, involves a blood test that measures four specific substances in the mother’s blood: alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), estriol, and inhibin-A. This screening is typically performed between the 15th and 20th weeks of pregnancy and assesses the risk of chromosomal abnormalities and neural tube defects. While second trimester screening is non-invasive and poses no risk to the fetus, it is less accurate than NIPT and may result in false positives or negatives. Positive results from second trimester screening often lead to further diagnostic testing, such as amniocentesis, to confirm the findings.
5. Ultrasound
Ultrasound is a non-invasive imaging technique that uses sound waves to create images of the fetus inside the womb. It is commonly used throughout pregnancy to monitor fetal development, assess the risk of chromosomal abnormalities, and detect structural anomalies. Ultrasound can be performed at various stages of pregnancy, with the first trimester ultrasound focusing on nuchal translucency measurement and the second trimester ultrasound, also known as the anatomy scan, providing a detailed assessment of fetal anatomy. While ultrasound is a valuable tool for prenatal screening, it is not as accurate as NIPT for detecting chromosomal abnormalities and may require further diagnostic testing for confirmation.
6. Cell-free DNA Testing
Cell-free DNA testing, also known as cfDNA testing, is a type of NIPT that analyzes small fragments of fetal DNA circulating in the maternal blood. This test can be performed as early as the 10th week of pregnancy and has a high accuracy rate for detecting chromosomal abnormalities such as Down syndrome, Edwards syndrome, and Patau syndrome. cfDNA testing poses no risk to the fetus and has a lower false-positive rate compared to traditional screening methods. However, it is important to note that cfDNA testing is a screening test and not diagnostic, so positive results often require confirmation through invasive testing such as CVS or amniocentesis.
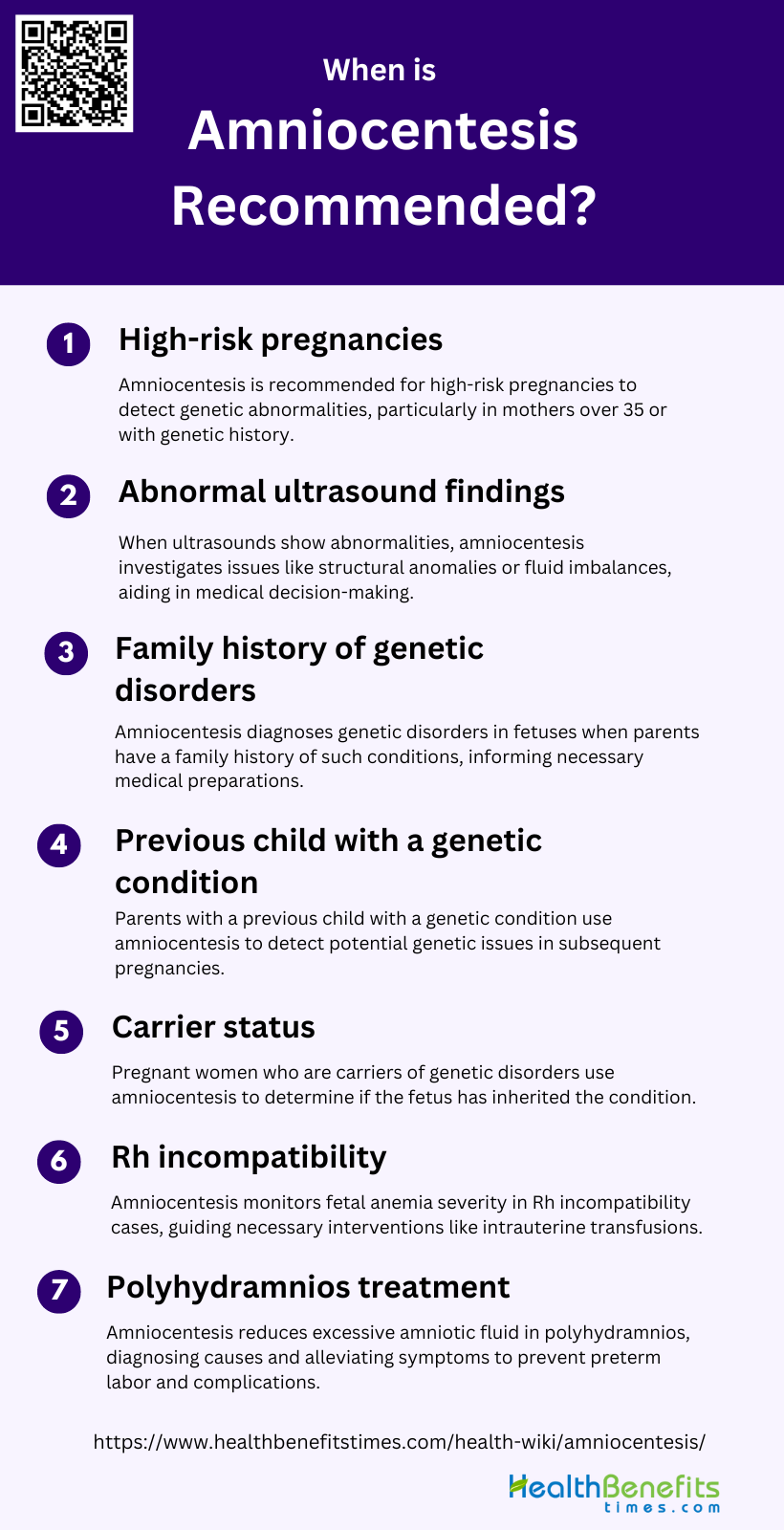
When is Amniocentesis Recommended?
Amniocentesis is typically recommended in specific situations where detailed information about the fetus’s health is needed. This procedure can help diagnose genetic disorders, assess fetal development, and manage potential risks. Here are some common scenarios when amniocentesis might be advised:
1. High-risk pregnancies
High-risk pregnancies include those where the mother is over 35 years old, has a history of genetic disorders, or has had previous pregnancies with complications. The procedure involves extracting a small amount of amniotic fluid to analyze fetal cells for chromosomal abnormalities and genetic disorders. Studies have shown that amniocentesis can provide critical information for managing high-risk pregnancies, enabling parents and healthcare providers to make informed decisions about the pregnancy and delivery.
2. Abnormal ultrasound findings
When an ultrasound reveals abnormal findings, such as structural anomalies or abnormal fluid levels, amniocentesis may be recommended to further investigate these issues. Abnormal findings can include polyhydramnios, oligohydramnios, or specific fetal malformations. Amniocentesis allows for the analysis of amniotic fluid to detect genetic abnormalities, infections, or other conditions that might explain the ultrasound findings. This additional diagnostic step can help in planning appropriate medical or surgical interventions and in making decisions about the continuation of the pregnancy.
3. Family history of genetic disorders
A family history of genetic disorders is a significant reason for recommending amniocentesis. If one or both parents are carriers of genetic mutations, there is a risk that the fetus may inherit these conditions. Amniocentesis can diagnose a range of genetic disorders, such as Down syndrome, Tay-Sachs disease, and cystic fibrosis, by analyzing fetal cells from the amniotic fluid. This information is crucial for parents to understand the genetic health of their unborn child and to prepare for any necessary medical care or interventions after birth.
4. Previous child with a genetic condition
Parents who have previously had a child with a genetic condition may opt for amniocentesis in subsequent pregnancies to determine if the current fetus is affected. This procedure can detect chromosomal abnormalities and other genetic disorders early in the pregnancy, allowing parents to make informed decisions about their options. The ability to diagnose conditions like Down syndrome or metabolic disorders through amniocentesis provides valuable information for managing the pregnancy and preparing for the needs of the child.
5. Carrier status
Carrier status can be determined through genetic testing before or during pregnancy. If a woman is a carrier of an X-linked recessive disorder, for example, amniocentesis can help determine the sex of the fetus and whether it has inherited the disorder. This information is essential for planning the appropriate medical care and interventions needed for the child and for making informed reproductive choices.
6. Rh incompatibility
In cases of Rh incompatibility, where the mother is Rh-negative and the fetus is Rh-positive, amniocentesis can be used to monitor the severity of fetal anemia. The procedure involves measuring the levels of bilirubin in the amniotic fluid, which can indicate the degree of hemolysis occurring in the fetus. This information helps in deciding whether interventions such as intrauterine transfusions are necessary to manage the condition and prevent complications like hydrops fetalis or fetal death.
7. Polyhydramnios treatment
Polyhydramnios, an excessive accumulation of amniotic fluid, can be associated with various fetal anomalies and maternal conditions. Amniocentesis can be performed to reduce the volume of amniotic fluid and to analyze it for potential causes of polyhydramnios, such as infections or genetic disorders. This procedure not only helps in diagnosing the underlying cause but also alleviates symptoms and reduces the risk of preterm labor and other complications associated with polyhydramnios.