Amenorrhea is the medical term for the absence of menstrual periods in women of reproductive age. It is classified into two types: primary amenorrhea, where a girl has not started menstruating by age 15, and secondary amenorrhea, where a woman who previously had regular periods misses them for three or more consecutive months. The condition can be a symptom of various underlying issues, including hormonal imbalances, genetic disorders, extreme weight loss or gain, excessive exercise, stress, and certain medical treatments or conditions like polycystic ovary syndrome (PCOS) and thyroid disorders. Diagnosis typically involves a thorough medical history, physical examination, and various tests to identify the root cause. Treatment depends on the underlying cause and may include lifestyle changes, medication, or, in rare cases, surgery.
Types of amenorrhea
Amenorrhea can be classified into different types based on its underlying causes and characteristics. Understanding these types is crucial for accurate diagnosis and treatment. Below are the primary types of amenorrhea:
1. Primary Amenorrhea
Primary amenorrhea is defined as the absence of menstruation by the age of 15 in individuals who have not yet had their first period, despite normal growth and secondary sexual characteristics, or by age 13 if there are no signs of puberty such as breast development. This condition can be caused by genetic or anatomical abnormalities, such as Turner syndrome or Müllerian agenesis, and hormonal imbalances, including hypogonadotropic hypogonadism. Other contributing factors may include chronic illnesses, eating disorders, or excessive physical activity. Diagnosis typically involves a thorough medical history, physical examination, and various tests to evaluate hormone levels and anatomical structures.
2. Secondary Amenorrhea
Secondary amenorrhea occurs when an individual who has previously had regular menstrual cycles stops menstruating for three months or more, or for six months in those with irregular cycles. Common causes include pregnancy, hormonal imbalances such as polycystic ovary syndrome (PCOS), thyroid disorders, and hyperprolactinemia. Lifestyle factors like significant weight loss, excessive exercise, and stress can also contribute to this condition. Diagnosis involves ruling out pregnancy and conducting blood tests to check hormone levels, as well as imaging studies to identify any structural abnormalities. Treatment focuses on addressing the underlying cause, which may involve lifestyle changes, medication, or surgery.
Causes of Amenorrhea
Amenorrhea ranging from lifestyle choices to underlying medical conditions. Identifying the specific cause is essential for effective treatment and management. Below are some common causes of amenorrhea:
1. Hormonal Imbalances
Hormonal imbalances are a significant cause of amenorrhea, particularly secondary amenorrhea, which is the absence of menses for three consecutive cycles. Neuroendocrine disruptions, such as functional hypothalamic amenorrhea and hyperprolactinemia, are common culprits. These conditions often arise from perturbations in the hypothalamic-pituitary-adrenal axis, leading to disruptions in the hypothalamic-pituitary-ovarian axis. Such imbalances can result in hypoestrogenemia, which not only affects menstrual cycles but also has broader health implications, including bone mass loss.
2. Lifestyle Factors
Lifestyle factors, including stress, weight loss, and excessive exercise, can lead to functional hypothalamic amenorrhea. This condition is characterized by the suppression of the hypothalamic-pituitary-ovarian axis due to psychological stress, disordered eating, or a combination of these factors. The resulting estrogen deficiency can have widespread effects on the body, impacting cardiac, skeletal, psychological, and reproductive health. Addressing these lifestyle factors is crucial for the restoration of normal menstrual cycles and overall health.
3. Medications and Medical Conditions
Certain medications and medical conditions can also cause amenorrhea. For instance, the use of oral contraceptives has been linked to long-standing amenorrhea in some women. This condition, often referred to as post-pill amenorrhea, may result from prolonged inhibition of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) release. Additionally, medical conditions such as polycystic ovarian syndrome (PCOS) and primary ovarian insufficiency (POI) are frequent causes of secondary amenorrhea.
4. Pregnancy and Breastfeeding
Pregnancy is the most common cause of amenorrhea and must be ruled out before proceeding with further diagnostic evaluations. During pregnancy, the hormonal changes necessary to support fetal development naturally suppress the menstrual cycle. Similarly, breastfeeding can lead to lactational amenorrhea due to elevated prolactin levels, which inhibit the secretion of gonadotropin-releasing hormone (GnRH) and subsequently FSH and LH, preventing ovulation and menstruation.
5. Contraceptives
The use of combined oral contraceptives can lead to amenorrhea in some women. Studies have shown that a significant number of women experience long-standing amenorrhea after discontinuing oral contraceptives. This condition is often due to the prolonged suppression of the hypothalamic-pituitary-ovarian axis. While many women recover spontaneously, some may require hormonal treatments to resume normal ovulatory cycles.
6. Ovulation Problems
Ovulation problems, such as those seen in PCOS and POI, are common causes of amenorrhea. PCOS is characterized by hyperandrogenism and chronic anovulation, leading to irregular or absent menstrual cycles. POI, on the other hand, involves the premature depletion of ovarian follicles, resulting in hypoestrogenism and amenorrhea. Both conditions require careful evaluation and management to restore normal menstrual function and address associated symptoms.
7. Lot of Exercise
Excessive exercise is a well-documented cause of functional hypothalamic amenorrhea. High levels of physical activity, particularly in athletes, can lead to energy deficits and stress, which suppress the hypothalamic-pituitary-ovarian axis. This suppression results in reduced estrogen levels and the cessation of menstrual cycles. Addressing the underlying energy imbalance and reducing exercise intensity are essential steps in restoring normal menstrual function.
8. Thyroid Disorder
Thyroid disorders, including both hypothyroidism and hyperthyroidism, can lead to menstrual irregularities and amenorrhea. Hypothyroidism is often associated with elevated prolactin levels, which can inhibit GnRH secretion and disrupt the menstrual cycle. Hyperthyroidism, on the other hand, can lead to increased metabolism and hormonal imbalances that affect menstrual regularity. Proper diagnosis and management of thyroid disorders are crucial for restoring normal menstrual cycles.
9. Obesity
Obesity is a significant risk factor for amenorrhea, primarily due to weight-related androgen excess. Elevated levels of plasma androgens in obese women can disrupt normal ovulatory cycles, leading to amenorrhea. Weight loss has been shown to normalize plasma androgen levels and restore ovulation in affected individuals. Addressing obesity through lifestyle modifications, including diet and exercise, is essential for managing amenorrhea in obese women.
Symptoms of Amenorrhea
Amenorrhea can manifest through various symptoms due to hormonal imbalances and underlying health issues. Common symptoms include:
1. Milky Nipple Discharge: Milky nipple discharge, or galactorrhea, can occur in amenorrhea due to hormonal imbalances, particularly elevated prolactin levels, which interfere with the menstrual cycle.
2. Hair Loss: Hair loss in amenorrhea is often linked to hormonal imbalances, particularly reduced estrogen levels, which can affect hair growth cycles and lead to thinning hair.
3. Headache: Headaches in amenorrhea may result from hormonal fluctuations, particularly involving estrogen and progesterone, which can impact brain chemistry and blood vessel behavior.
4. Vision Changes: Vision changes in amenorrhea can be due to pituitary gland disorders, which affect hormone levels and may cause pressure on the optic nerve, altering vision.
5. Excess Facial Hair: Excess facial hair, or hirsutism, in amenorrhea is often due to increased androgen levels, which can disrupt normal menstrual cycles and promote male-pattern hair growth.
6. Pelvic Pain: Pelvic pain in amenorrhea can stem from underlying conditions like polycystic ovary syndrome (PCOS) or endometriosis, which affect menstrual regularity and cause discomfort.
7. Acne: Acne in amenorrhea is frequently caused by hormonal imbalances, particularly elevated androgens, which increase sebum production and lead to clogged pores and breakouts.
8. Hot Flashes: Hot flashes in amenorrhea are typically due to low estrogen levels, which affect the body’s temperature regulation and can cause sudden feelings of heat and sweating.
9. Vaginal Dryness: Vaginal dryness in amenorrhea is often a result of decreased estrogen levels, which affect the vaginal lining’s moisture and elasticity, leading to discomfort and irritation.
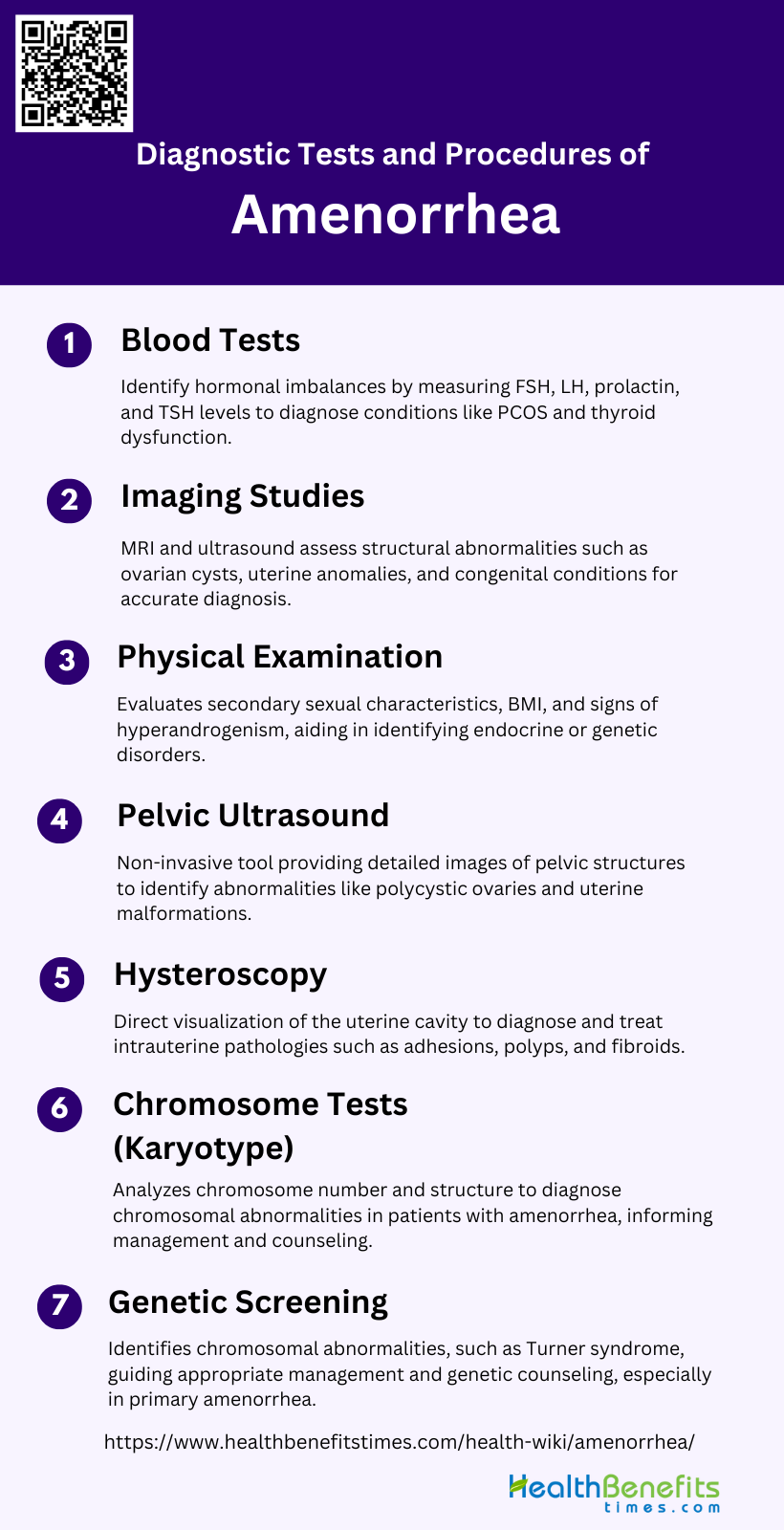
Diagnostic tests and procedures of Amenorrhea
Diagnosing amenorrhea involves a series of tests and procedures to determine the underlying cause. Key diagnostic methods include:
1. Blood Tests
Blood tests are fundamental in diagnosing amenorrhea, as they help identify hormonal imbalances and other underlying conditions. Key hormones measured include follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin, and thyroid-stimulating hormone (TSH). Elevated or decreased levels of these hormones can indicate various etiologies such as primary ovarian insufficiency, hypothalamic or pituitary disorders, and thyroid dysfunction. Additionally, serum androgen levels may be assessed to rule out hyperandrogenic conditions like polycystic ovary syndrome (PCOS). Blood tests are often the first step in a comprehensive diagnostic approach, guiding further investigations and management strategies.
2. Imaging Studies
Imaging studies, particularly magnetic resonance imaging (MRI) and ultrasound, play a crucial role in evaluating structural abnormalities in patients with amenorrhea. MRI is highly accurate in diagnosing congenital anomalies such as Mayer-Rokitansky-Küster-Hauser syndrome and transverse vaginal septum, with excellent correlation to surgical findings. Ultrasound, including duplex/color Doppler sonography, is the imaging modality of choice for assessing the pelvic organs, helping to identify conditions like ovarian cysts, uterine anomalies, and outflow tract obstructions. These imaging techniques provide detailed anatomical information, essential for accurate diagnosis and treatment planning.
3. Physical Examination
A thorough physical examination is vital in the diagnostic process of amenorrhea. It includes assessing secondary sexual characteristics, body mass index (BMI), and signs of hyperandrogenism such as hirsutism and acne. The examination helps identify developmental anomalies, such as the absence of breast development or pubic hair, which may indicate underlying endocrine or genetic disorders. Additionally, a pelvic examination can reveal structural abnormalities like an imperforate hymen or vaginal septum. Physical findings, combined with patient history, guide further diagnostic testing and management.
4. Pelvic Ultrasound
Pelvic ultrasound is a non-invasive and highly informative diagnostic tool for evaluating amenorrhea. It provides detailed images of the uterus, ovaries, and other pelvic structures, helping to identify abnormalities such as polycystic ovaries, uterine malformations, and ovarian tumors. Ultrasound is particularly useful in distinguishing between primary and secondary amenorrhea by assessing the presence and development of reproductive organs. It also aids in monitoring the response to treatment and guiding further diagnostic procedures if necessary.
5. Hysteroscopy
Hysteroscopy involves the insertion of a thin, lighted tube into the uterus to directly visualize the uterine cavity. This procedure is particularly useful for diagnosing intrauterine pathologies such as adhesions (Asherman’s syndrome), polyps, and fibroids, which can cause amenorrhea. Hysteroscopy allows for both diagnosis and treatment, as therapeutic interventions like adhesiolysis or polypectomy can be performed during the same procedure. It is a valuable tool in the comprehensive evaluation and management of amenorrhea, especially when other diagnostic methods are inconclusive.
6. Genetic Screening
Genetic screening is essential in diagnosing amenorrhea, particularly in cases with suspected chromosomal abnormalities. Techniques such as G-banding and C-banding facilitate the identification of specific chromosomal anomalies, including Turner syndrome (45,X), mosaicism, and structural rearrangements. Genetic screening helps determine the underlying cause of amenorrhea, guiding appropriate management and counseling. It is especially important in primary amenorrhea, where chromosomal abnormalities are a common etiological factor.
7. Chromosome Tests (Karyotype)
Karyotype analysis is a critical diagnostic test for identifying chromosomal abnormalities in patients with amenorrhea. This test involves examining the number and structure of chromosomes in a patient’s cells. Studies have shown that a significant proportion of patients with primary amenorrhea have abnormal karyotypes, including Turner syndrome, sex chromosome mosaicism, and other structural anomalies. Karyotype analysis provides valuable information for diagnosis, management, and genetic counseling, helping to address the underlying causes of amenorrhea and associated health concerns.
Risk factors for amenorrhea
Amenorrhea can be influenced by various risk factors, ranging from lifestyle choices to medical conditions. Key risk factors include:
1. Family History of Amenorrhea or Early Menopause: A family history of amenorrhea or early menopause can increase your risk, as genetic factors may influence the onset and regulation of menstrual cycles.
2. Genetic or Chromosomal Condition That Affects Your Ovaries or Uterus: Genetic or chromosomal conditions, such as Turner syndrome, can impair ovarian or uterine function, leading to amenorrhea by disrupting normal hormonal and reproductive processes.
3. Obesity or Being Underweight: Both obesity and being underweight can disrupt hormonal balance, affecting the hypothalamic-pituitary-ovarian axis and leading to irregular or absent menstrual cycles.
4. Eating Disorder: Eating disorders like anorexia nervosa or bulimia can severely impact nutritional status and hormonal balance, often resulting in amenorrhea due to insufficient body fat and energy reserves.
5. Over-Exercising: Excessive physical activity can lead to amenorrhea by causing hormonal imbalances, particularly reduced estrogen levels, which can disrupt the menstrual cycle and reproductive function.
6. Poor Diet: A poor diet lacking essential nutrients can affect overall health and hormonal balance, potentially leading to amenorrhea by impairing the body’s ability to maintain regular menstrual cycles.
7. Stress: Chronic stress can influence the hypothalamus, which regulates hormones essential for menstruation, potentially leading to amenorrhea by disrupting the normal hormonal signals.
8. Chronic Illness: Chronic illnesses, such as diabetes or celiac disease, can interfere with hormonal balance and reproductive health, increasing the risk of amenorrhea due to systemic health impacts.
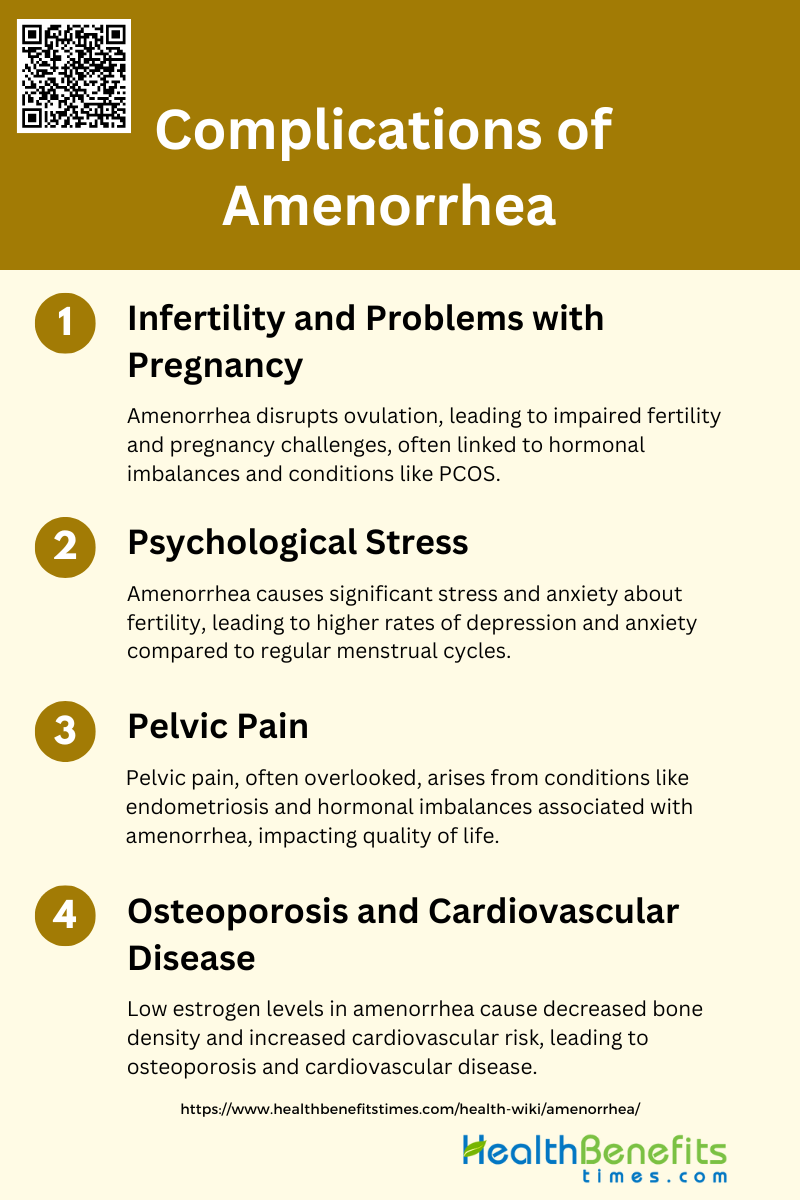
Complications of Amenorrhea
Amenorrhea can lead to several health complications if left untreated, affecting various aspects of physical and reproductive health. Potential complications include:
1. Infertility and Problems with Pregnancy
Amenorrhea, the absence of menstrual periods, can significantly impact fertility and pregnancy outcomes. Women with amenorrhea often experience impaired fertility due to hormonal imbalances that disrupt ovulation. This condition is particularly concerning for women of reproductive age, as it can lead to difficulties in conceiving and maintaining a pregnancy. For instance, a study on women with spinal cord injuries found that 41.4% experienced post-injury amenorrhea, which was transient in most cases, but still posed challenges for pregnancy. Additionally, amenorrhea can be associated with conditions like polycystic ovarian syndrome (PCOS), which further complicates fertility and increases the risk of endometrial hyperplasia and carcinoma. Therefore, early diagnosis and management are crucial to mitigate these reproductive challenges.
2. Psychological Stress
The psychological impact of amenorrhea is profound, often leading to significant stress and anxiety. Women with amenorrhea frequently worry about their fertility and the potential for unexpected ovulation and undesired pregnancy. The condition is also linked to higher rates of depression and anxiety compared to women with regular menstrual cycles. The stress associated with amenorrhea can stem from various factors, including the uncertainty of diagnosis, the implications for future fertility, and the social and personal pressures related to reproductive health. Addressing the psychological aspects of amenorrhea is essential for comprehensive care, as untreated psychological stress can exacerbate the condition and lead to further health complications.
3. Osteoporosis and Cardiovascular Disease
Amenorrhea, particularly when associated with low estrogen levels, has significant long-term health implications, including osteoporosis and cardiovascular disease. Prolonged estrogen deficiency leads to decreased bone mineral density, increasing the risk of osteoporosis and fractures. This condition is particularly concerning for young women, as early bone loss can have lasting effects on skeletal health. Additionally, amenorrhea adversely affects lipid profiles, contributing to an increased risk of cardiovascular events. The metabolic changes associated with amenorrhea, such as altered glucose and fat metabolism, further compound these risks. Therefore, addressing the hormonal imbalances and ensuring adequate estrogen levels are critical to preventing these severe complications.
4. Pelvic Pain
Pelvic pain is a common but often overlooked complication of amenorrhea. The absence of regular menstrual cycles can lead to various underlying conditions that cause pelvic discomfort. For example, endometriosis, a condition where tissue similar to the lining inside the uterus grows outside it, can be both a cause and a consequence of amenorrhea, leading to significant pelvic pain. Additionally, hormonal imbalances associated with amenorrhea can result in conditions like endometrial hyperplasia, which also contributes to pelvic pain. Effective management of amenorrhea requires addressing these underlying conditions to alleviate pain and improve the quality of life for affected women.
Treatment Options for Amenorrhea
Treating amenorrhea involves addressing the underlying cause through various medical and lifestyle interventions. Common treatment options include:
1. Treating Underlying Conditions
Treating the underlying conditions causing amenorrhea is crucial for effective management. For instance, in cases of amenorrhea induced by chemotherapy for breast cancer, addressing the specific chemotherapy regimen and its impact on menstrual cycles is essential. Studies have shown that the likelihood of amenorrhea varies based on the chemotherapy regimen and the patient’s age. Additionally, the use of oral contraceptives during chemotherapy has been associated with a higher likelihood of menstrual cycle return post-treatment. Therefore, a thorough evaluation of the underlying cause is necessary to tailor the treatment effectively.
2. Hormonal Therapies
Hormonal therapies are a common and effective treatment for amenorrhea, particularly when it is of endocrine origin. Estrogen and progesterone therapies have been shown to induce bleeding and improve secondary sexual characteristics in patients with amenorrhea. For example, the use of transvaginal progesterone gel has demonstrated high efficacy in inducing withdrawal bleeding and improving endometrial morphology in women with secondary amenorrhea. Additionally, high dosage progesterone therapy, sometimes combined with estrogen, has been effective in inducing bleeding and even achieving pregnancy in some cases.
3. Surgical Interventions
Surgical interventions may be necessary for amenorrhea caused by structural abnormalities or severe cases unresponsive to hormonal treatments. Hysteroscopic surgery, for instance, can be employed to address intrauterine adhesions or other anatomical issues that may be causing amenorrhea. While the provided data does not specifically mention hysteroscopic surgery, it is a recognized treatment option in clinical practice. Surgical interventions are typically considered when less invasive treatments have failed or when there is a clear anatomical cause for the amenorrhea.
4. Lifestyle and Alternative Treatments
Lifestyle modifications and alternative treatments can also play a role in managing amenorrhea. Stress reduction, maintaining a healthy weight, and ensuring adequate nutrition are important factors. In some cases, alternative treatments such as acupuncture or herbal supplements may be explored, although their efficacy varies and should be approached with caution. The data provided does not extensively cover lifestyle and alternative treatments, but these approaches are often recommended as part of a holistic treatment plan for amenorrhea.
5. Medications
Various medications can be used to treat amenorrhea, depending on its cause. For example, gonadotropic hormones have been used to induce bleeding in patients with amenorrhea of endocrine origin. Additionally, medications such as diethylstilbestrol combined with chorionic gonadotropin have shown promise in treating amenorrhea, particularly in cases where other hormonal treatments have failed. The choice of medication should be based on a thorough evaluation of the patient’s specific condition and underlying causes.
6. Hysteroscopic Surgery
Hysteroscopic surgery is a minimally invasive procedure used to diagnose and treat intrauterine pathologies that may cause amenorrhea, such as adhesions, polyps, or fibroids. This surgical approach allows for direct visualization and treatment of the uterine cavity, often resulting in the restoration of normal menstrual function. While the provided data does not specifically mention hysteroscopic surgery, it is a well-established treatment option in gynecological practice. This procedure is particularly beneficial for patients with structural abnormalities that are not responsive to hormonal or medical treatments.
Prevention and Management of Amenorrhea
Preventing and managing amenorrhea involves adopting healthy lifestyle habits and addressing underlying medical conditions. Key strategies for prevention and management include:
1. Lifestyle Modifications
Lifestyle modifications are crucial in the prevention and management of amenorrhea. Functional hypothalamic amenorrhea, often caused by stress, weight loss, or excessive exercise, can be managed by addressing these lifestyle factors. Reducing stress, ensuring adequate nutrition, and moderating exercise intensity can help restore normal menstrual function. Additionally, increasing caloric intake has shown promising results in recovering menstrual function in women with exercise-associated amenorrhea. These modifications not only help in resuming menses but also improve overall health by addressing the underlying causes of amenorrhea.
2. Regular Medical Check-ups
Regular medical check-ups are essential for early detection and management of amenorrhea. A thorough medical history and physical examination can help identify potential causes such as hormonal imbalances, chronic diseases, or structural abnormalities. Routine assessments, including pregnancy tests and hormone level evaluations, are recommended to monitor the patient’s condition and adjust treatment plans accordingly. Early recognition and intervention can prevent long-term complications such as osteoporosis and cardiovascular issues associated with prolonged hypoestrogenism.
3. Awareness and Education
Raising awareness and providing education about amenorrhea are vital for both patients and healthcare providers. Understanding the potential causes, symptoms, and long-term health implications of amenorrhea can lead to timely medical consultation and appropriate management. Educational programs should emphasize the importance of maintaining a balanced lifestyle, recognizing early signs of menstrual irregularities, and seeking medical advice when necessary. This proactive approach can help mitigate the adverse effects of amenorrhea on reproductive and overall health.
4. Maintain a Healthy Weight
Maintaining a healthy weight is a key factor in preventing amenorrhea, particularly weight loss-related amenorrhea. Sudden or excessive weight loss can disrupt the hypothalamic-pituitary-ovarian axis, leading to menstrual irregularities. Ensuring a balanced diet and avoiding extreme dieting practices can help maintain hormonal balance and regular menstrual cycles. Weight management should be approached holistically, considering both physical and psychological aspects to support overall well-being and reproductive health.
5. Exercise Moderately
Moderate exercise is beneficial for overall health but excessive physical activity can lead to exercise-associated amenorrhea. Athletes and individuals engaging in high-intensity training should be aware of the risks and monitor their menstrual cycles closely. Reducing exercise intensity and increasing caloric intake have been shown to help in the recovery of menstrual function in amenorrheic athletes. Incorporating rest days and ensuring adequate nutrition can prevent the onset of amenorrhea and support long-term health.
6. Manage Stress
Stress management is crucial in preventing and treating functional hypothalamic amenorrhea. Chronic stress can disrupt the hormonal balance necessary for regular menstrual cycles. Techniques such as mindfulness, meditation, and counseling can help reduce stress levels and improve overall mental health. Addressing psychological stressors and providing emotional support are important components of a comprehensive treatment plan for amenorrhea. Effective stress management can lead to the resumption of normal menstrual function and enhance quality of life.