Amelogenesis Imperfecta (AI) is a hereditary condition that affects the development of enamel, the hard outer layer of teeth. This disorder results in enamel that is abnormally thin, soft, or improperly formed, leading to teeth that are discolored, prone to rapid wear, and highly susceptible to damage and decay. AI can present in various forms, ranging from mild discoloration to severe structural defects, and it often requires comprehensive dental management to address both functional and aesthetic concerns. The condition is classified as a structural anomaly of the teeth and can significantly impact oral health and quality of life.
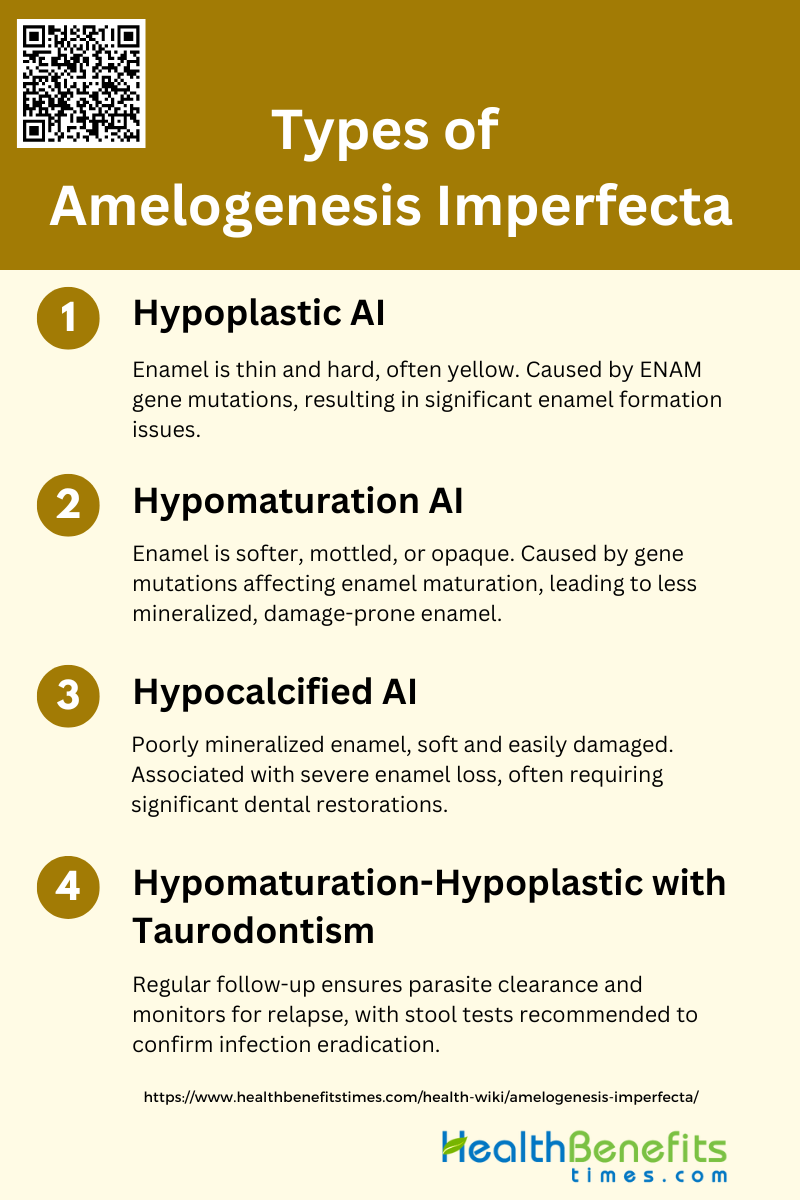
Types of Amelogenesis Imperfecta
Understanding the different types is crucial for accurate diagnosis and treatment planning. The following are the primary types of Amelogenesis Imperfecta:
1. Hypoplastic AI
Hypoplastic amelogenesis imperfecta (AI) is characterized by the formation of thin and hard enamel that is often yellow in color. This condition results from mutations in the enamelin (ENAM) gene, which plays a crucial role in enamel formation. For instance, a nonsense mutation in the ENAM gene has been identified as a cause of local hypoplastic autosomal dominant AI, leading to a truncated peptide that significantly impacts enamel formation. The enamel in affected individuals is typically smooth and thin, and the condition accounts for a significant proportion of autosomally inherited AI cases in certain populations. Additionally, another study identified a heterozygous single-G deletion at the exon-intron boundary of the ENAM gene, further supporting the role of ENAM mutations in hypoplastic AI.
2. Hypomaturation AI
Hypomaturation AI is characterized by enamel that is softer than normal and may appear mottled or opaque. This type of AI often results from mutations in genes involved in the maturation stage of enamel formation. For example, a family with X-linked hypomaturation AI exhibited clinical and histopathological features consistent with this subtype, highlighting the genetic heterogeneity of the disorder. The enamel in hypomaturation AI is less mineralized, leading to increased susceptibility to wear and damage. The condition can be inherited in various patterns, including autosomal dominant, autosomal recessive, and X-linked, further complicating its diagnosis and management.
3. Hypocalcified AI
Hypocalcified AI is characterized by enamel that is poorly mineralized, leading to a soft and easily damaged surface. This subtype is often associated with severe enamel loss and discoloration. A study on a large family with hypocalcified AI revealed extensive post-eruptive enamel breakdown and a high treatment burden, with most affected individuals requiring significant dental restorations. The enamel in hypocalcified AI is typically yellow and lacks translucency, making it prone to rapid deterioration after tooth eruption. This condition is often inherited in an autosomal dominant pattern and can be associated with other dental anomalies, although these are rare.
4. Hypomaturation-Hypoplastic with Taurodontism
Hypomaturation-hypoplastic AI with taurodontism (AIHHT) is a rare subtype characterized by a combination of hypomature and hypoplastic enamel defects along with taurodontism, a condition where the molar teeth have enlarged pulp chambers. A case report described a boy with severely hypoplastic enamel and taurodontism, where many permanent teeth were already infected upon eruption. The clinical and radiological features of AIHHT can overlap with other syndromes, such as tricho-dento-osseous syndrome, making diagnosis challenging. Genetic analysis in such cases may not always reveal mutations in known AI-related genes, indicating the need for further research to understand the underlying genetic mechanisms.
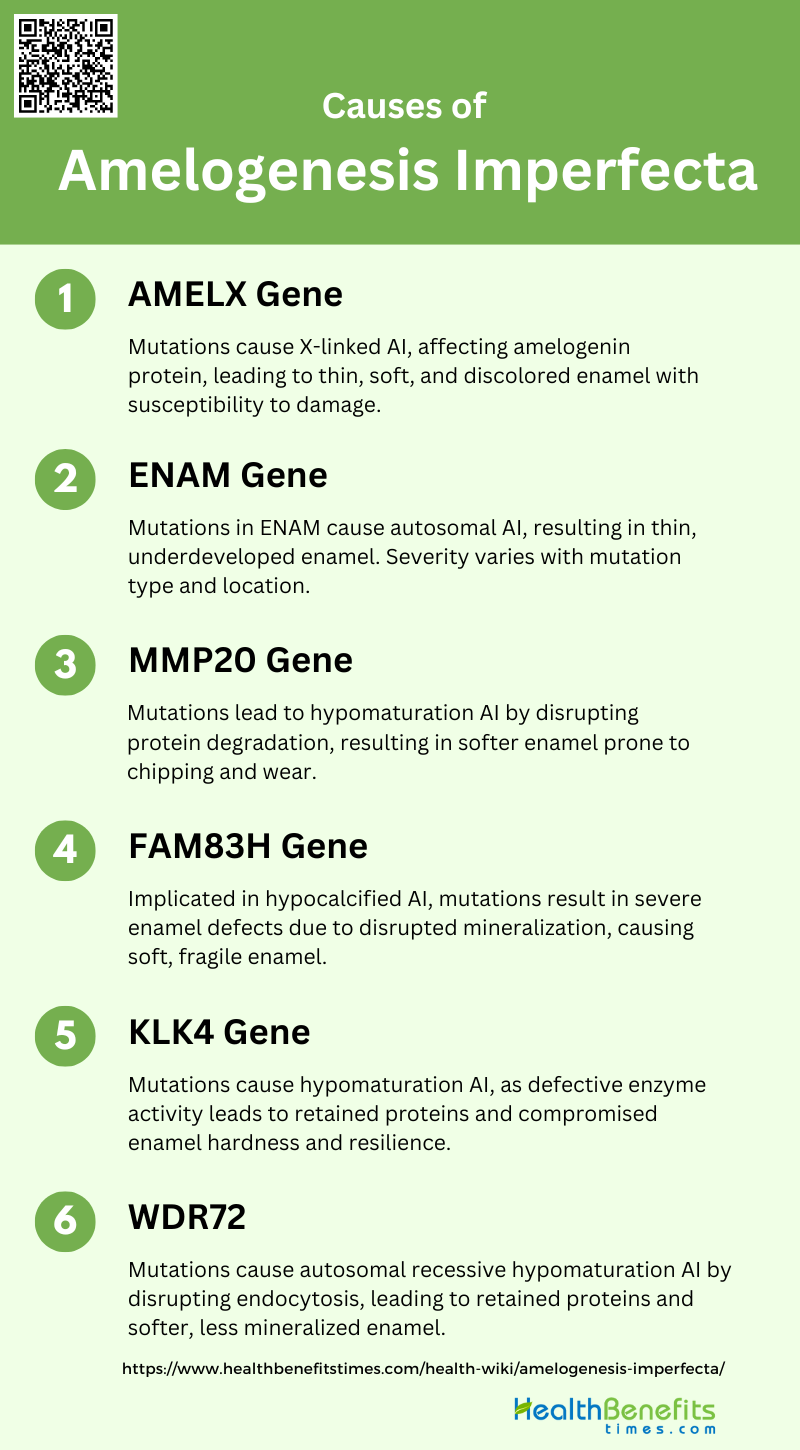
Causes of Amelogenesis Imperfecta
Amelogenesis Imperfecta is caused by genetic mutations that affect the proteins involved in enamel formation. These mutations can be inherited in an autosomal dominant, autosomal recessive, or X-linked manner. The following are the primary genetic causes:
1. AMELX Gene
The AMELX gene encodes amelogenin, a critical extracellular matrix protein secreted by ameloblasts during enamel formation. Mutations in AMELX are a well-documented cause of X-linked amelogenesis imperfecta (AI), leading to defects in enamel thickness and mineralization. These mutations can result in hypoplastic, hypomineralized, or combined types of AI, characterized by abnormally thin, soft, and discolored enamel. The altered protein structure or its absence disrupts the normal enamel formation process, making teeth more susceptible to damage and decay.
2. ENAM Gene
The ENAM gene encodes enamelin, a protein essential for the proper formation of dental enamel. Mutations in ENAM are associated with autosomal dominant and recessive forms of AI. These mutations often result in hypoplastic AI, where the enamel is thin and underdeveloped. Specific mutations, such as nonsense or insertion mutations, can lead to truncated enamelin proteins, severely affecting enamel formation. The phenotypic expression can vary from localized enamel defects to generalized hypoplasia, depending on the nature and location of the mutation.
3. MMP20 Gene
The MMP20 gene encodes matrix metalloproteinase-20, an enzyme crucial for the degradation of enamel proteins during the maturation stage of enamel formation. Mutations in MMP20 disrupt this process, leading to the retention of enamel proteins and resulting in a softer, less mineralized enamel. This condition manifests as hypomaturation AI, where the enamel is prone to chipping and wear. The role of MMP20 in enamel formation underscores the importance of protein degradation in achieving proper enamel hardness and resilience.
4. FAM83H Gene
The FAM83H gene is implicated in autosomal dominant hypocalcified AI. Although the exact function of the FAM83H protein in enamel formation is not fully understood, mutations in this gene lead to severe enamel defects. These mutations often result in a truncated protein, which is believed to interfere with the normal mineralization process of enamel. The enamel in affected individuals is typically very soft and prone to rapid wear and breakage, highlighting the critical role of FAM83H in maintaining enamel integrity.
5. KLK4 Gene
The KLK4 gene encodes kallikrein-4, a serine protease involved in the final stages of enamel maturation. Mutations in KLK4 result in hypomaturation AI, characterized by enamel that is not fully hardened and is thus more susceptible to damage. The enzyme’s role in degrading enamel matrix proteins is crucial for the removal of organic material and the proper mineralization of enamel. Defective KLK4 activity leads to the retention of these proteins, compromising the enamel’s structural integrity.
6. WDR72
The WDR72 gene is associated with autosomal recessive hypomaturation AI. The protein encoded by WDR72 is believed to play a role in the endocytosis process during enamel maturation. Mutations in WDR72 disrupt this process, leading to the retention of enamel matrix proteins and resulting in softer, less mineralized enamel. The exact mechanisms by which WDR72 mutations cause AI are still under investigation, but its role in cellular processes during enamel formation is evident from the phenotypic manifestations observed in affected individuals.
Signs and Symptoms of Amelogenesis Imperfecta
Amelogenesis Imperfecta presents with a variety of dental abnormalities that can affect both the appearance and function of teeth. These signs and symptoms can vary depending on the type and severity of the condition. The following are common signs and symptoms:
- Yellow, Brown, Grey, or White Discoloration of Teeth: Teeth may appear yellow, brown, grey, or white due to abnormal enamel formation, affecting aesthetics and self-esteem.
- Thin, Soft, or Brittle Enamel: Enamel is often thin, soft, or brittle, making teeth more susceptible to damage and increasing the risk of decay.
- Unusual Tooth Growth: Teeth may grow in unusual shapes or sizes, leading to functional issues and complicating dental treatments and orthodontics.
- Uneven, Lumpy, or Ridged Teeth: Teeth surfaces can be uneven, lumpy, or ridged, causing discomfort, difficulty in chewing, and aesthetic concerns.
- Extreme Tooth Sensitivity: Affected individuals often experience extreme tooth sensitivity to hot, cold, or sweet stimuli, impacting daily comfort and diet.
- Open Bite (Misaligned Jaws): An open bite, where the upper and lower teeth do not meet properly, can result from misaligned jaws, affecting speech and chewing.
- Dental Cavities (Caries): Due to compromised enamel, individuals are more prone to dental cavities, necessitating frequent dental interventions and care.
- Tooth Wear, Cracking, and Chipping: Teeth are more likely to wear down, crack, or chip easily, leading to further dental complications and the need for restorations.
- Excess Tartar Build-Up: There is often an excess build-up of tartar, increasing the risk of gum disease and requiring regular professional cleanings.
- Large or Swollen Gums (Gingival Hyperplasia): Gums may become large or swollen, a condition known as gingival hyperplasia, which can cause discomfort and complicate oral hygiene.
- Tooth Rot: Tooth rot can occur due to the compromised enamel, leading to severe decay and the potential loss of affected teeth.
- Infection of the Tissues and Bone Surrounding Teeth: Infections can develop in the tissues and bone surrounding teeth, leading to pain, swelling, and potential systemic health issues.
Diagnosis of Amelogenesis Imperfecta
Diagnosing Amelogenesis Imperfecta involves a combination of clinical examination, family history, and radiographic imaging. Genetic testing may also be utilized to confirm the diagnosis.
1. Intra-Oral Examination
Intra-oral examination is crucial for diagnosing Amelogenesis Imperfecta (AI), as it allows for the direct observation of enamel defects. AI is characterized by a range of enamel abnormalities, including hypoplastic, hypomature, and hypocalcified enamel, which can present as thin, soft, fragile, pitted, or discolored enamel. These defects can lead to functional and aesthetic issues, such as early tooth loss, eating difficulties, and severe embarrassment. Additionally, intra-oral examination can reveal other dental anomalies associated with AI, such as abnormal crown morphology, poor oral hygiene, and malocclusions like open bite. Identifying these phenotypic variations is essential for accurate diagnosis and treatment planning.
2. Dental Radiographs (X-rays)
Dental radiographs are indispensable in diagnosing AI, as they provide detailed images of the teeth and jawbone, revealing abnormalities not visible during a clinical examination. Panoramic radiographs can detect supernumerary teeth, dental agenesis, microdontia, taurodontism, and mandibular hypoplasia, which are more prevalent in AI patients compared to non-AI individuals. Radiographic analysis also helps in assessing dental maturation and comparing it with non-AI children, ensuring accurate age estimation and understanding of tooth development. These radiographic findings are critical for comprehensive diagnosis and effective management of AI.
3. Genetic Testing (if necessary)
Genetic testing plays a pivotal role in diagnosing AI, especially when clinical and radiographic findings are inconclusive. AI is a genetically heterogeneous condition, with mutations in at least 18 genes known to cause nonsyndromic AI and many more implicated in syndromic forms. Genetic testing can identify specific mutations, such as those in the AMELX, ENAM, and MMP20 genes, which are associated with different AI phenotypes. Next-generation sequencing (NGS) has significantly improved the diagnostic rate, enabling the identification of pathogenic variants and providing insights into the molecular mechanisms underlying AI. This information is invaluable for accurate diagnosis, personalized treatment, and genetic counseling.
Treatment Options for Amelogenesis Imperfecta
Treatment for Amelogenesis Imperfecta aims to enhance dental function and aesthetics while preventing further enamel damage. Various approaches are tailored to the patient’s specific needs and severity of the condition.
1. Dental Bonding
Dental bonding is a common treatment for amelogenesis imperfecta (AI), particularly for improving the aesthetics of anterior teeth. This method involves the application of a tooth-colored resin material to the affected teeth, which is then hardened using a special light. Although dental bonding can provide immediate aesthetic improvements, its longevity is often limited, especially in patients with AI. Studies have shown that indirect restorations, such as crowns, offer superior predictability and longevity compared to direct bonding techniques. Therefore, while dental bonding can be a useful interim solution, it is generally recommended to transition to more durable restorative options as soon as feasible.
2. Full Crown Restoration
Full crown restoration is a highly effective treatment for AI, offering both functional and aesthetic benefits. Ceramic crowns, such as Procera and IPS e.max Press, have shown excellent survival and success rates in young patients with AI, with minimal adverse events and significant reductions in tooth sensitivity. Long-term studies have demonstrated that these crowns maintain their quality and integrity over several years, making them a reliable option for managing severe forms of AI. Additionally, full crown restoration can significantly improve the oral health-related quality of life (OHRQoL) for patients, reducing dental fear and enhancing social interactions.
3. Orthodontic Treatment
Orthodontic treatment can be an essential component of managing AI, particularly in cases where malocclusion or misalignment is present. Orthodontic interventions can help in achieving a functional bite and improving overall dental aesthetics. In some cases, orthodontic treatment is combined with restorative procedures, such as the placement of crowns or veneers, to achieve optimal results. A comprehensive treatment plan that includes both orthodontic and restorative approaches can address the complex dental issues associated with AI, leading to improved oral function and patient satisfaction.
4. Good Dental Hygiene
Maintaining good dental hygiene is crucial for patients with AI to prevent secondary complications such as dental caries and gingivitis. Regular dental check-ups, professional cleanings, and meticulous home care routines, including brushing with fluoride toothpaste and flossing, are essential. Preventive care can help manage the increased susceptibility to dental issues in AI patients and prolong the longevity of restorative treatments. Educating patients and caregivers about the importance of oral hygiene and providing tailored advice can significantly improve oral health outcomes in individuals with AI.
5. Low-Sugar Diet
A low-sugar diet is recommended for patients with AI to minimize the risk of dental caries, which they are more prone to due to the compromised enamel. Reducing the intake of sugary foods and beverages can help in maintaining better oral health and reducing the frequency of dental visits. A balanced diet rich in essential nutrients supports overall dental health and can complement other treatment modalities for AI. Dietary counseling should be an integral part of the management plan for AI patients to ensure they adopt and maintain healthy eating habits.
6. Dentures or Overlay Dentures
In cases where teeth are severely compromised, dentures or overlay dentures can be considered as a treatment option for AI. These prosthetic devices can restore function and aesthetics, providing a significant improvement in the quality of life for patients. Overlay dentures, which fit over the remaining natural teeth, can offer additional stability and comfort compared to conventional dentures. This approach can be particularly beneficial for older patients or those with extensive tooth loss, offering a non-invasive solution to restore oral function.
7. Dental Implants
Dental implants are a viable option for replacing missing teeth in patients with AI, offering a permanent and stable solution. Implants can support crowns, bridges, or dentures, providing excellent functional and aesthetic outcomes. Studies have shown that dental implants can be successfully used in AI patients, although careful planning and consideration of the patient’s overall oral health are essential. The use of implants can significantly enhance the quality of life for AI patients, offering a durable and reliable alternative to traditional prosthetic options.
Preventive measures of Amelogenesis Imperfecta
Preventive measures for Amelogenesis Imperfecta focus on maintaining oral health and minimizing enamel damage. These strategies can help manage symptoms and improve overall dental well-being.
1. Maintain Good Oral Hygiene
Maintaining good oral hygiene is crucial for individuals with Amelogenesis Imperfecta (AI) to prevent secondary complications such as dental caries and gingivitis. Regular brushing with a soft-bristled toothbrush and fluoride toothpaste, along with flossing, can help remove plaque and reduce the risk of decay and gum disease. Studies have shown that patients with AI often have fair to poor oral hygiene, which can exacerbate their condition. Therefore, meticulous oral care routines are essential to manage the symptoms and improve overall oral health.
2. Regular Dental Visits
Regular dental visits are essential for early diagnosis and management of AI. Frequent check-ups allow for timely interventions, such as the application of fluoride varnishes or the placement of protective restorations, which can help mitigate the effects of AI. These visits also provide an opportunity for dental professionals to monitor the progression of the condition and adjust treatment plans as necessary. Studies indicate that patients with AI require more frequent dental visits compared to the general population to maintain oral health and manage complications.
3. Use of Fluoride
The use of fluoride is a well-documented preventive measure for managing AI. Fluoride helps in remineralizing enamel and reducing tooth sensitivity, which is a common issue in AI patients. Topical fluoride applications, such as varnishes and gels, can be particularly beneficial. In cases where fluoride alone is insufficient, combining it with other desensitizing agents like cyanoacrylate has shown promising results in reducing tooth sensitivity and improving the quality of life for AI patients.
4. Protective Dental Treatments
Protective dental treatments, such as the application of crowns and other restorative materials, play a significant role in managing AI. Indirect restorations, such as ceramic crowns, have been shown to provide superior longevity and predictability compared to direct restorations. These treatments not only improve the aesthetics and function of the teeth but also protect the underlying dentin from further damage. Long-term studies have demonstrated the effectiveness of ceramic crowns in reducing tooth sensitivity and enhancing the overall oral health of AI patients.
5. Dietary Modifications
Dietary modifications are an important aspect of managing AI. Patients should avoid foods and beverages that are highly acidic or sugary, as these can exacerbate enamel erosion and increase the risk of dental caries. A balanced diet rich in calcium and other essential nutrients can help support overall dental health. Additionally, avoiding hard foods that can cause mechanical damage to the already fragile enamel is recommended. These dietary changes, combined with other preventive measures, can significantly improve the oral health outcomes for individuals with AI.