Amebiasis is an intestinal infection caused by the protozoan parasite Entamoeba histolytica. This parasite can live in the large intestine without causing harm, but in some cases, it invades the intestinal wall, leading to colitis, acute dysentery, or chronic diarrhea. The infection is most prevalent in tropical regions with poor sanitation, such as parts of Africa, Mexico, South America, and India. Transmission occurs through ingestion of contaminated food or water, or direct contact with fecal matter. Symptoms range from mild abdominal cramps and diarrhea to severe cases involving bloody stools and fever. If untreated, the parasite can spread to other organs, most commonly the liver, causing abscesses. Diagnosis typically involves stool tests and imaging, and treatment usually includes antibiotics.
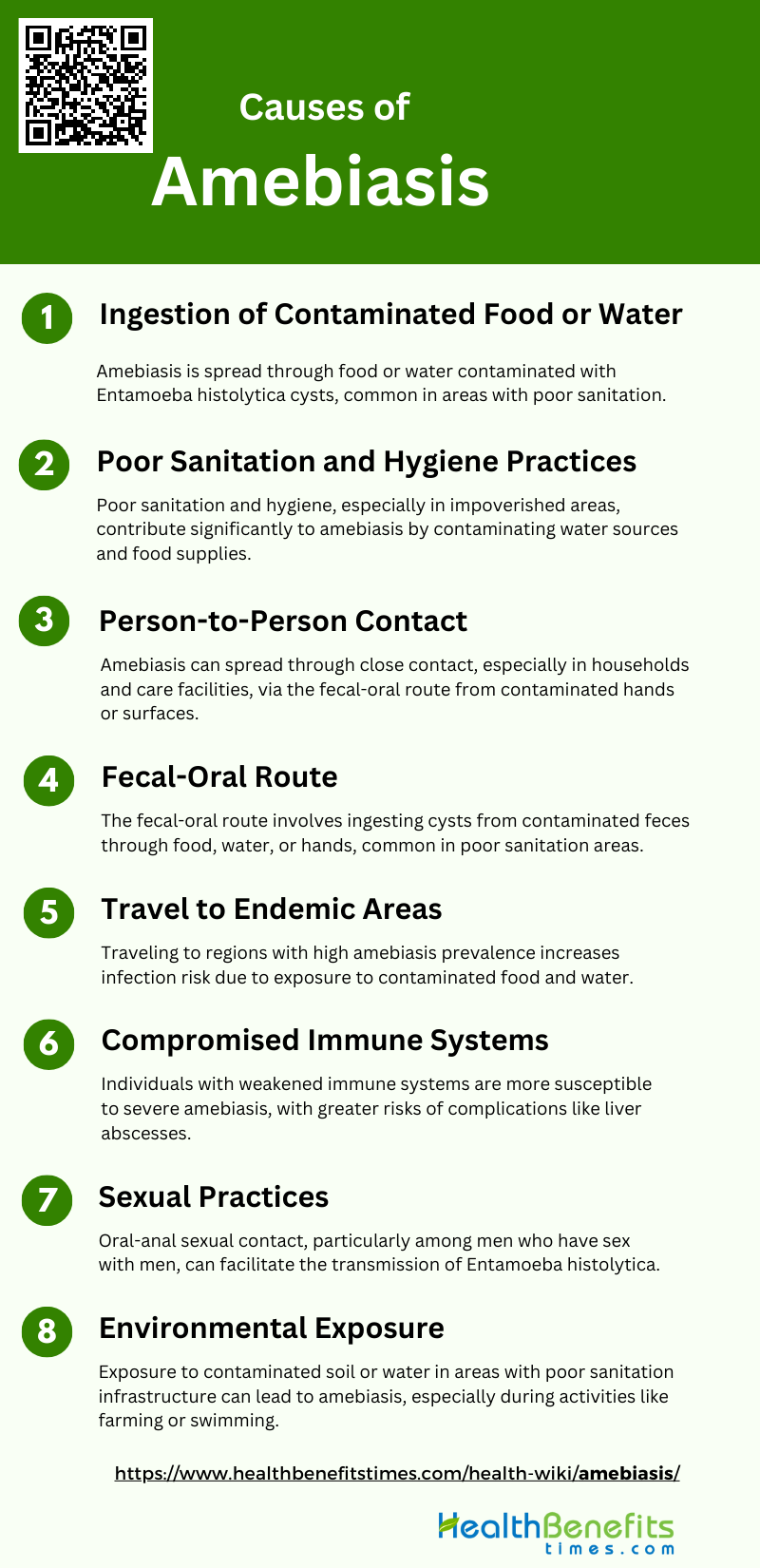
Causes of Amebiasis
Amebiasis infection is primarily spread through the ingestion of contaminated food or water. Several factors contribute to the transmission and development of amebiasis, including:
1. Ingestion of Contaminated Food or Water
This mode of transmission is particularly prevalent in developing countries where sanitation and water purification systems are inadequate. The cysts, which are the infective form of the parasite, can survive harsh environmental conditions and are resistant to stomach acid, allowing them to reach the intestines where they excyst and release trophozoites. These trophozoites then invade the intestinal mucosa, leading to symptoms such as diarrhea and dysentery. Improving water purification and food safety practices are crucial for reducing the incidence of amebiasis.
2. Poor Sanitation and Hygiene Practices
Poor sanitation and hygiene practices are significant contributors to the spread of amebiasis. In areas with inadequate waste disposal systems, human feces can contaminate water sources and food supplies, facilitating the transmission of E. histolytica. The lack of access to clean water and proper sanitation facilities exacerbates the problem, particularly in impoverished communities. Studies have shown that improving sanitation infrastructure and promoting good hygiene practices, such as regular handwashing with soap, can significantly reduce the incidence of amebiasis. Public health initiatives focusing on these areas are essential for controlling the spread of the disease.
3. Person-to-Person Contact
Person-to-person contact is another route through which amebiasis can spread, particularly in settings where individuals are in close proximity, such as households and long-term care facilities. The transmission often occurs through the fecal-oral route, where cysts are passed from an infected person to another individual via contaminated hands or surfaces. This mode of transmission underscores the importance of maintaining good personal hygiene and sanitation practices within households and communal living environments to prevent the spread of the infection.
4. Fecal-Oral Route
The fecal-oral route is a primary pathway for the transmission of E. histolytica. This occurs when cysts from fecal matter contaminate food, water, or hands, and are subsequently ingested. The cysts then excyst in the small intestine, releasing trophozoites that invade the colon. This route of transmission is particularly common in areas with poor sanitation and hygiene practices. Preventative measures such as proper handwashing, safe food handling, and the use of clean water are critical in breaking the cycle of transmission and reducing the incidence of amebiasis.
5. Travel to Endemic Areas
Travel to endemic areas is a significant risk factor for contracting amebiasis. Travelers to regions with high prevalence rates of E. histolytica, such as parts of Africa, Asia, and Latin America, are at increased risk due to exposure to contaminated food and water. Returning travelers often bring the infection back to non-endemic areas, contributing to its spread. It is recommended that travelers take precautions such as drinking bottled or boiled water, avoiding raw vegetables and fruits that cannot be peeled, and practicing good personal hygiene to minimize the risk of infection.
6. Compromised Immune Systems
Individuals with compromised immune systems are more susceptible to severe forms of amebiasis. Conditions such as HIV/AIDS, malnutrition, and the use of immunosuppressive drugs can weaken the immune response, making it easier for E. histolytica to invade and cause significant damage to the host tissues. In these individuals, the infection can lead to more severe complications, including liver abscesses and other extraintestinal manifestations. Understanding the host immune response and developing targeted immunotherapies are crucial for managing amebiasis in immunocompromised patients.
7. Sexual Practices
Certain sexual practices, particularly those involving oral-anal contact, can facilitate the transmission of E. histolytica. This mode of transmission is notably observed among men who have sex with men (MSM) and can lead to outbreaks of amebiasis in this population. Studies have documented clusters of sexually transmitted amebiasis, highlighting the need for awareness and preventive measures within these communities. Safe sexual practices and regular screening for sexually transmitted infections, including amebiasis, are important for reducing transmission rates.
8. Environmental Exposure
Environmental exposure to contaminated soil or water can also be a source of amebiasis. In areas where sanitation infrastructure is lacking, E. histolytica cysts can contaminate the environment, posing a risk to individuals who come into contact with contaminated surfaces or water bodies. Activities such as farming, swimming in contaminated water, or living in flood-prone areas can increase the risk of exposure. Public health measures aimed at improving environmental sanitation and educating communities about the risks of environmental exposure are essential for preventing amebiasis.
Symptoms of Amebiasis
Amebiasis can lead to a range of gastrointestinal symptoms. These symptoms can vary in severity and may include the following:
1. Diarrhea (may be bloody): Amebiasis often causes diarrhea, which can sometimes be bloody, indicating the presence of intestinal inflammation or ulceration.
2. Abdominal cramps and pain: Patients with amebiasis frequently experience abdominal cramps and pain due to the parasitic infection irritating the intestinal lining.
3. Nausea and vomiting: Nausea and vomiting are common symptoms of amebiasis, resulting from the body’s response to the parasitic infection in the gut.
4. Fever: Amebiasis can trigger a fever as the body’s immune system reacts to fight off the parasitic infection causing inflammation.
5. Loss of appetite: Loss of appetite is a typical symptom of amebiasis, often due to the discomfort and digestive disturbances caused by the infection.
6. Rectal Pain during Bowel Movements: Rectal pain during bowel movements is a symptom of amebiasis, often due to inflammation and ulceration in the rectal area.
7. Unintentional Weight Loss: Unintentional weight loss can occur in amebiasis patients due to chronic diarrhea, loss of appetite, and nutrient malabsorption.
8. Fatigue: Fatigue is a common symptom of amebiasis, resulting from the body’s ongoing battle against the parasitic infection and nutrient loss.
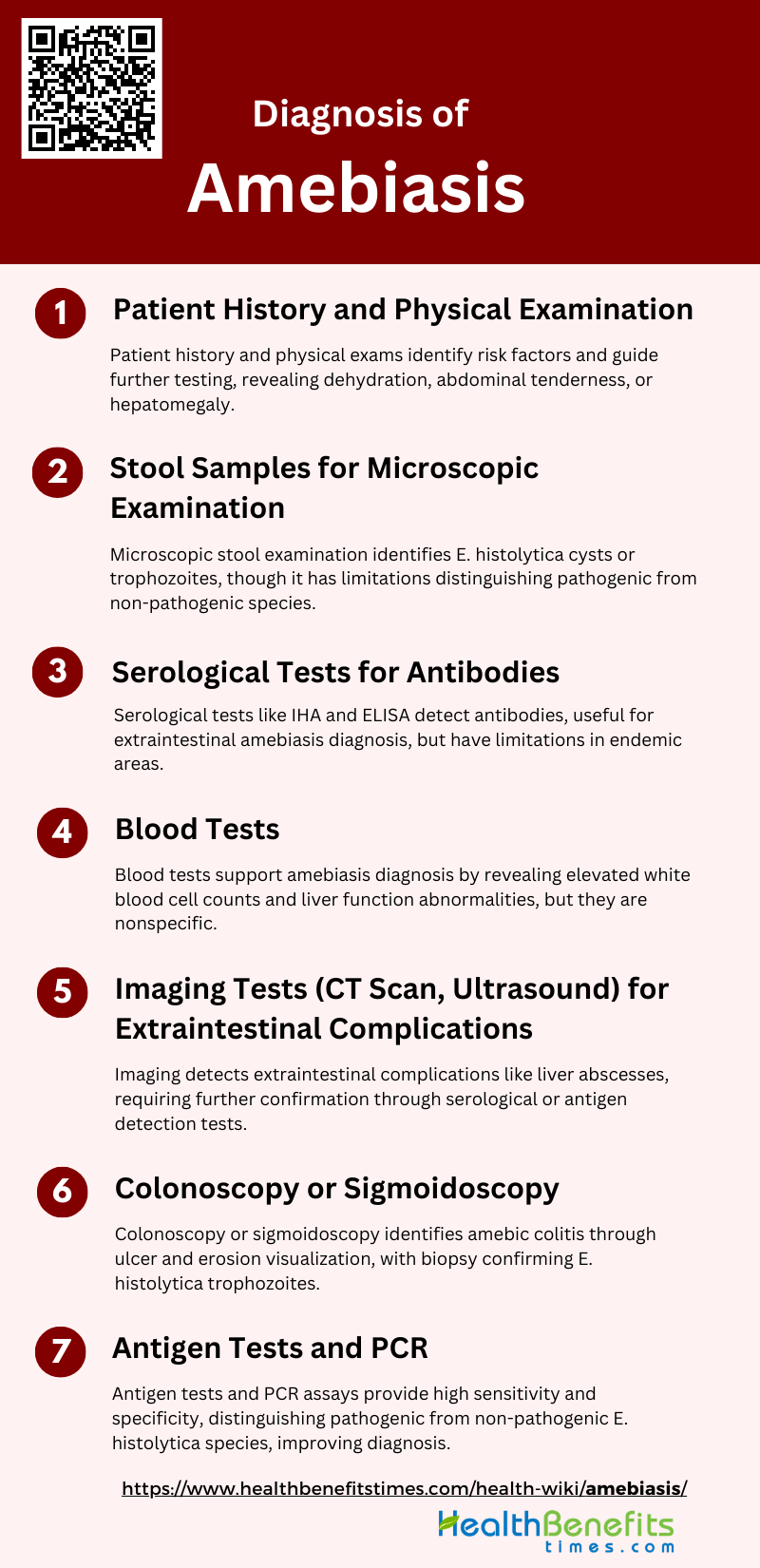
Diagnosis of Amebiasis
Diagnosis of amebiasis involves a combination of clinical evaluation, laboratory testing, and imaging studies to confirm the presence of Entamoeba histolytica. Accurate diagnosis is crucial for effective treatment and management of the infection. The following steps outline the diagnostic process:
1. Patient History and Physical Examination
A thorough patient history and physical examination are crucial initial steps in diagnosing amebiasis. Patients often present with nonspecific gastrointestinal symptoms such as abdominal pain, diarrhea, and weight loss, which can complicate the diagnosis. A detailed history should include questions about recent travel to endemic areas, exposure to potentially contaminated food or water, and any previous episodes of similar symptoms. Physical examination may reveal signs of dehydration, abdominal tenderness, or hepatomegaly in cases of extraintestinal amebiasis. These initial steps help to identify patients who are at higher risk and guide further diagnostic testing.
2. Stool Samples for Microscopic Examination
Microscopic examination of stool samples is a traditional method for diagnosing amebiasis, involving the identification of cysts or trophozoites of Entamoeba histolytica. However, this method has limitations, including low sensitivity and the inability to distinguish E. histolytica from non-pathogenic species like E. dispar and E. moshkovskii. Despite these limitations, stool microscopy remains a valuable tool, especially in resource-limited settings, and can be enhanced by concentration techniques such as the formol-ether method to improve detection rates.
3. Serological Tests for Antibodies
Serological tests, such as the indirect hemagglutination (IHA) and enzyme-linked immunosorbent assay (ELISA), are used to detect antibodies against E. histolytica. These tests are particularly useful for diagnosing extraintestinal amebiasis, where stool samples may not contain the parasite. Serological tests have high sensitivity and specificity, but their utility is limited in endemic areas due to the high prevalence of asymptomatic carriers. Additionally, serological tests can remain positive for months to years after infection, which may complicate the interpretation of results.
4. Blood Tests
Blood tests can provide supportive evidence for amebiasis, especially in cases of extraintestinal infection. Elevated white blood cell counts and liver function abnormalities may be observed in patients with amebic liver abscess. However, these findings are nonspecific and must be interpreted in conjunction with other diagnostic tests. Blood tests are not definitive for diagnosing amebiasis but can help in assessing the overall health status of the patient and identifying potential complications.
5. Imaging Tests (CT Scan, Ultrasound) for Extraintestinal Complications
Imaging studies such as ultrasound and computed tomography (CT) scans are essential for diagnosing extraintestinal complications of amebiasis, particularly liver abscesses. These imaging modalities can reveal characteristic findings such as single or multiple hypoechoic lesions in the liver. However, imaging alone cannot differentiate amebic abscesses from pyogenic abscesses, necessitating further diagnostic confirmation through serological or antigen detection tests. Imaging is also useful for monitoring the response to treatment and detecting any complications.
6. Colonoscopy or Sigmoidoscopy
Colonoscopy or sigmoidoscopy can be valuable in diagnosing amebic colitis, especially when stool tests are inconclusive. Colonoscopic findings may include ulcers, erosions, and edematous mucosa, particularly in the cecum and rectum. Biopsy and microscopic examination of colonic tissue can confirm the presence of E. histolytica trophozoites, providing a definitive diagnosis. This method is particularly useful in differentiating amebic colitis from other causes of colitis, such as inflammatory bowel disease or ischemic colitis.
7. Antigen Tests and PCR
Antigen detection tests and polymerase chain reaction (PCR) assays are modern diagnostic tools that offer high sensitivity and specificity for detecting E. histolytica. Antigen tests, such as the TechLab E. histolytica-specific antigen detection test, are rapid and simple to perform, making them suitable for use in both developed and developing countries. PCR assays, which amplify specific DNA sequences of E. histolytica, provide excellent sensitivity and can distinguish between pathogenic and non-pathogenic species. However, PCR is often limited by its cost and the need for specialized equipment. Combining antigen tests with PCR can enhance diagnostic accuracy, especially in challenging cases.
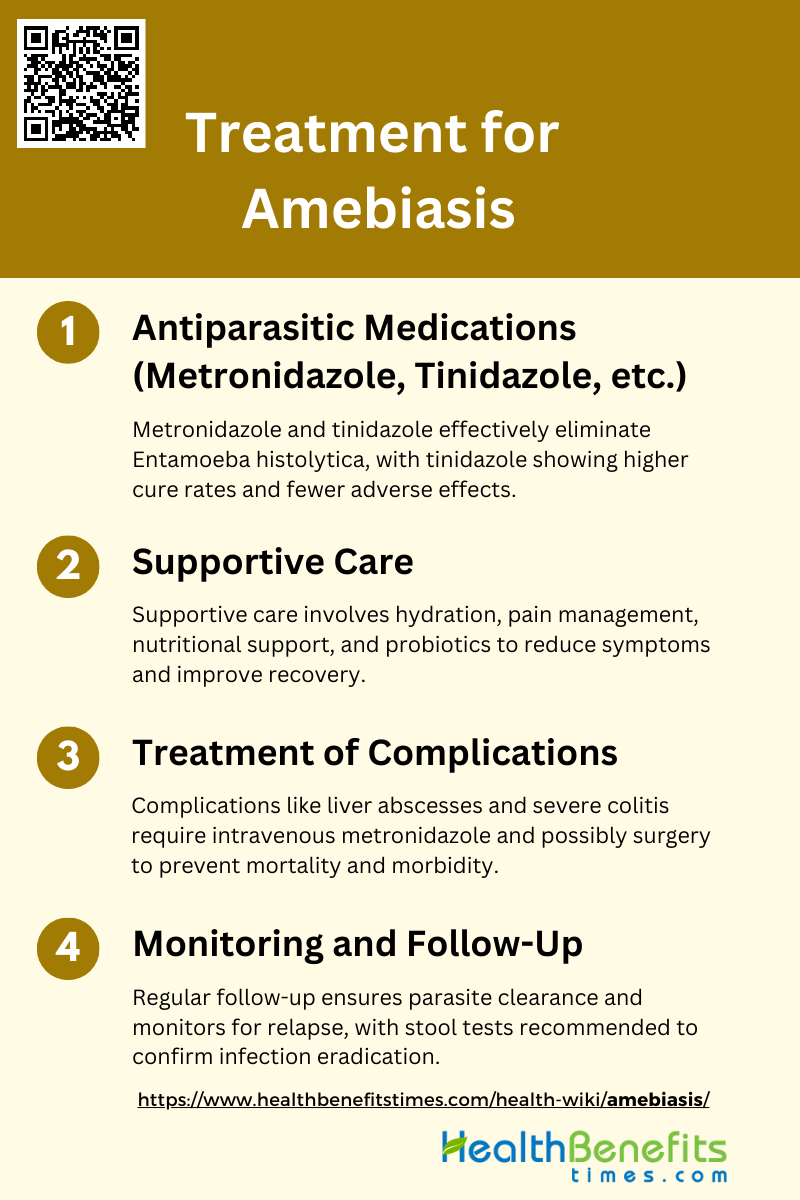
Treatment for Amebiasis
Treatment for amebiasis typically involves the use of specific medications to eliminate the parasite and manage symptoms. Prompt and accurate treatment is essential to prevent complications and ensure recovery. The following steps outline the treatment process:
1. Antiparasitic Medications (Metronidazole, Tinidazole, etc.)
Antiparasitic medications are the cornerstone of amebiasis treatment. Metronidazole and tinidazole are commonly used due to their efficacy in eliminating the parasite Entamoeba histolytica. Studies have shown that tinidazole may be more effective than metronidazole, with higher cure rates and fewer adverse effects. In cases where these medications fail, diloxanide furoate has been shown to be highly effective, achieving parasitological cure rates of up to 93% in asymptomatic patients. Additionally, combining metronidazole with probiotics like Saccharomyces boulardii can enhance treatment outcomes by reducing the duration of symptoms and improving cyst clearance.
2. Supportive Care
Supportive care is essential in managing amebiasis, particularly in severe cases. This includes maintaining hydration, managing pain, and addressing nutritional needs. Intravenous fluids may be necessary for patients with severe diarrhea or dehydration. In children, the addition of probiotics such as Saccharomyces boulardii to the treatment regimen has been shown to significantly reduce the duration of bloody diarrhea and enhance the clearance of amebic cysts. Supportive care also involves monitoring for potential complications and providing symptomatic relief to improve patient comfort and recovery.
3. Treatment of Complications
Complications of amebiasis, such as amebic liver abscesses and severe colitis, require prompt and aggressive treatment. Intravenous metronidazole is often used for moderate-to-severe cases and has been shown to be effective and well-tolerated. Surgical intervention may be necessary in cases of intestinal perforation or abscess drainage. In HIV-1-infected individuals, the clinical presentation of invasive amebiasis can be severe, and treatment with metronidazole or tinidazole has been successful, although recurrence is possible. Addressing complications promptly is crucial to prevent mortality and long-term morbidity.
4. Monitoring and Follow-Up
Monitoring and follow-up are critical components of amebiasis management to ensure treatment efficacy and prevent recurrence. Patients should be re-evaluated periodically to confirm the clearance of the parasite and to monitor for any signs of relapse. Follow-up stool tests are recommended to ensure that the infection has been fully eradicated. In high-risk populations, such as those with HIV-1, continuous monitoring is essential due to the higher likelihood of recurrence and re-infection. Effective follow-up care helps in managing long-term outcomes and preventing the spread of the disease.
Prevention for Amebiasis
Preventing amebiasis involves adopting good hygiene practices, ensuring safe food and water consumption, and maintaining proper sanitation. These measures are essential to reduce the risk of infection and spread of the parasite. The following steps outline key prevention strategies:
1. Improved Sanitation and Hygiene
Improved sanitation and hygiene are critical in preventing amebiasis, a disease caused by the protozoan parasite Entamoeba histolytica. The parasite is primarily transmitted through contaminated food and water, making sanitation a key preventive measure. Enhancing sanitation facilities and promoting good hygiene practices can significantly reduce the incidence of amebiasis. Studies have shown that better sanitation and hygiene can decrease the prevalence of various parasitic infections, including amebiasis, by limiting the transmission routes of the parasite. Therefore, investing in sanitation infrastructure and public health education on hygiene practices is essential for controlling the spread of this disease.
2. Use Safe Water
Access to safe water is paramount in preventing amebiasis. Contaminated water is a major transmission route for Entamoeba histolytica. Ensuring that communities have access to clean and safe drinking water can drastically reduce the incidence of amebiasis. Water treatment methods, such as boiling, filtrations, and chlorination, are effective in eliminating the parasite from drinking water sources. Studies have demonstrated that improved water quality is associated with a lower prevalence of parasitic infections, including amebiasis. Therefore, implementing water purification systems and promoting safe water practices are crucial steps in preventing this disease.
3. Eat Safe Foods
Consuming safe foods is another important preventive measure against amebiasis. The parasite can be transmitted through food that has been contaminated with fecal matter. Ensuring that food is properly cooked and handled can prevent the ingestion of Entamoeba histolytica. Public health campaigns that educate communities about safe food handling practices, such as washing fruits and vegetables thoroughly and avoiding raw or undercooked foods, can help reduce the risk of infection. By promoting food safety, the spread of amebiasis can be effectively controlled.
4. Avoiding Risky Sexual Practices
Avoiding risky sexual practices is essential in preventing the transmission of amebiasis, particularly among men who have sex with men (MSM). The parasite can be transmitted through oral-anal contact, making certain sexual behaviors high-risk for infection. Public health initiatives that promote safe sexual practices, such as the use of barriers like dental dams and condoms, can help reduce the transmission of Entamoeba histolytica. Educating at-risk populations about the modes of transmission and preventive measures is crucial in controlling the spread of amebiasis in these communities.
5. Frequent Handwashing
Frequent handwashing is a simple yet effective measure to prevent amebiasis. The parasite can be transmitted through direct contact with contaminated surfaces or fecal matter. Regular handwashing with soap and water, especially before eating and after using the toilet, can significantly reduce the risk of infection. Studies have shown that handwashing is an effective intervention in reducing the incidence of various parasitic infections, including amebiasis. Public health campaigns that promote hand hygiene can play a vital role in preventing the spread of this disease.
6. Avoid Fecal Exposure
Avoiding fecal exposure is crucial in preventing amebiasis. The parasite is transmitted through the fecal-oral route, making it important to minimize contact with fecal matter. This can be achieved by improving sanitation facilities, promoting the use of toilets, and ensuring proper disposal of human waste. Public health initiatives that focus on reducing open defecation and improving waste management can help prevent the transmission of Entamoeba histolytica. By reducing fecal exposure, the risk of amebiasis can be significantly decreased.
7. Be Cautious When Traveling
Travelers to areas where amebiasis is endemic should take precautions to avoid infection. This includes drinking only bottled or boiled water, avoiding ice in drinks, eating only well-cooked foods, and avoiding raw fruits and vegetables unless they can be peeled. Travelers should also practice good hand hygiene and avoid risky sexual practices. Public health advisories and travel health clinics can provide valuable information and resources to help travelers protect themselves from amebiasis. By being cautious and informed, travelers can reduce their risk of contracting the disease.
8. Sanitation Infrastructure
Investing in sanitation infrastructure is essential for the long-term prevention of amebiasis. This includes building and maintaining clean water supply systems, sewage treatment facilities, and public toilets. Improved sanitation infrastructure can reduce the transmission of Entamoeba histolytica by minimizing contact with contaminated water and fecal matter. Studies have shown that communities with better sanitation infrastructure have lower rates of parasitic infections, including amebiasis. Governments and organizations should prioritize the development and maintenance of sanitation infrastructure to protect public health and prevent the spread of amebiasis.