Amblyopia, commonly known as “lazy eye,” is a visual development disorder where one eye fails to achieve normal visual acuity, even with prescription glasses or contact lenses. This condition typically arises during early childhood when the brain and eyes are developing. Amblyopia can result from various factors, including strabismus (misaligned eyes), significant differences in refractive errors between the two eyes (anisometropia), or visual deprivation due to conditions like cataracts. The brain starts to favor the stronger eye, leading to poor vision in the affected eye. Early diagnosis and treatment, such as patching the stronger eye or using corrective lenses, are crucial to prevent long-term visual impairment.
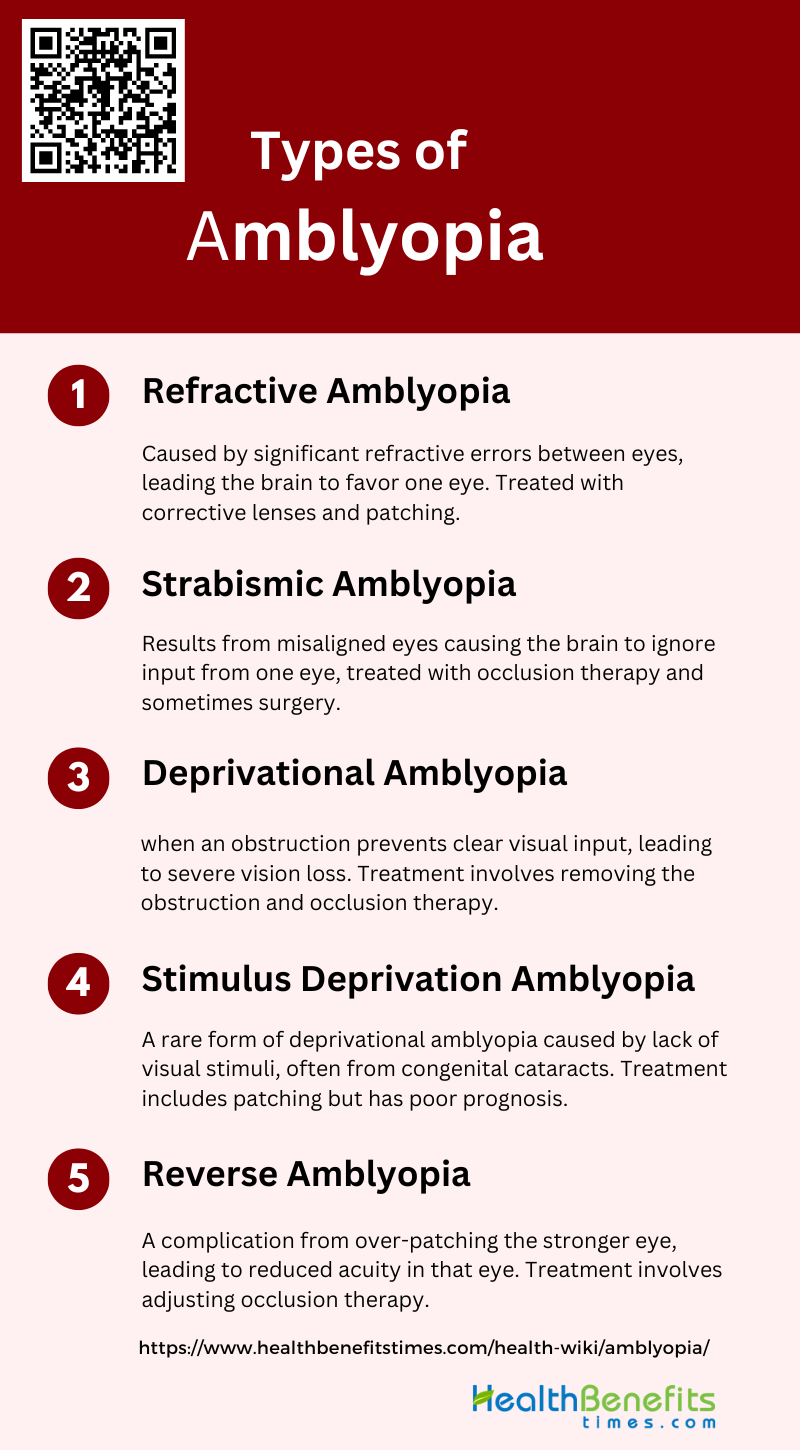
Types of amblyopia
Amblyopia each with distinct causes and characteristics. Understanding the different types is crucial for accurate diagnosis and effective treatment. Below are the primary types of amblyopia:
1. Refractive Amblyopia
Refractive amblyopia occurs when there is a significant difference in the refractive errors between the two eyes, known as anisometropia, or when both eyes have high refractive errors. This condition leads to the brain favoring one eye over the other, resulting in reduced visual acuity in the less favored eye. Unlike other forms of amblyopia, refractive amblyopia does not involve any visible abnormalities in the eye structure. Treatment typically involves correcting the refractive error with glasses or contact lenses, and sometimes patching the stronger eye to encourage use of the amblyopic eye.
2. Strabismic Amblyopia
Strabismic amblyopia arises from strabismus, a condition where the eyes are misaligned. This misalignment causes the brain to ignore the input from one eye to avoid double vision, leading to reduced visual acuity in the affected eye. Strabismus affects approximately 5% to 8% of the general population. Treatment often includes occlusion therapy, where the stronger eye is patched to force the use of the amblyopic eye, and may also involve surgical correction of the eye alignment. Studies have shown that combining occlusion therapy with near activities can improve visual outcomes.
3. Deprivational Amblyopia
Deprivational amblyopia, also known as deprivation amblyopia, occurs when an obstruction prevents clear visual input from reaching the retina during early childhood. Common causes include congenital cataracts, ptosis (droopy eyelid), or other media opacities. This type of amblyopia is particularly severe and often resistant to treatment, with a generally poor visual prognosis. The primary treatment is to remove the obstruction and then use occlusion therapy to stimulate the amblyopic eye. However, the effectiveness of these treatments can be limited, and further research is needed to optimize treatment protocols.
4. Stimulus Deprivation Amblyopia
Stimulus deprivation amblyopia (SDA) is a specific form of deprivational amblyopia where the deprivation is due to a lack of clear visual stimuli reaching the retina. This can be caused by conditions such as congenital cataracts or severe ptosis. SDA is rare, constituting less than 3% of all amblyopia cases. The main treatment involves patching the better-seeing eye to encourage use of the amblyopic eye, but the results are often disappointing. The prognosis for SDA is generally poor, and there is a need for more research to determine the most effective treatment strategies.
5. Reverse Amblyopia
Reverse amblyopia can occur as a complication of treatment for amblyopia, particularly when the stronger eye is patched for too long, leading to a decrease in its visual acuity. This condition underscores the importance of carefully monitoring and adjusting treatment protocols to avoid over-penalizing the stronger eye. The treatment for reverse amblyopia involves reducing or stopping the occlusion therapy and allowing the previously patched eye to recover its function. This highlights the delicate balance required in amblyopia treatment to ensure both eyes develop properly.
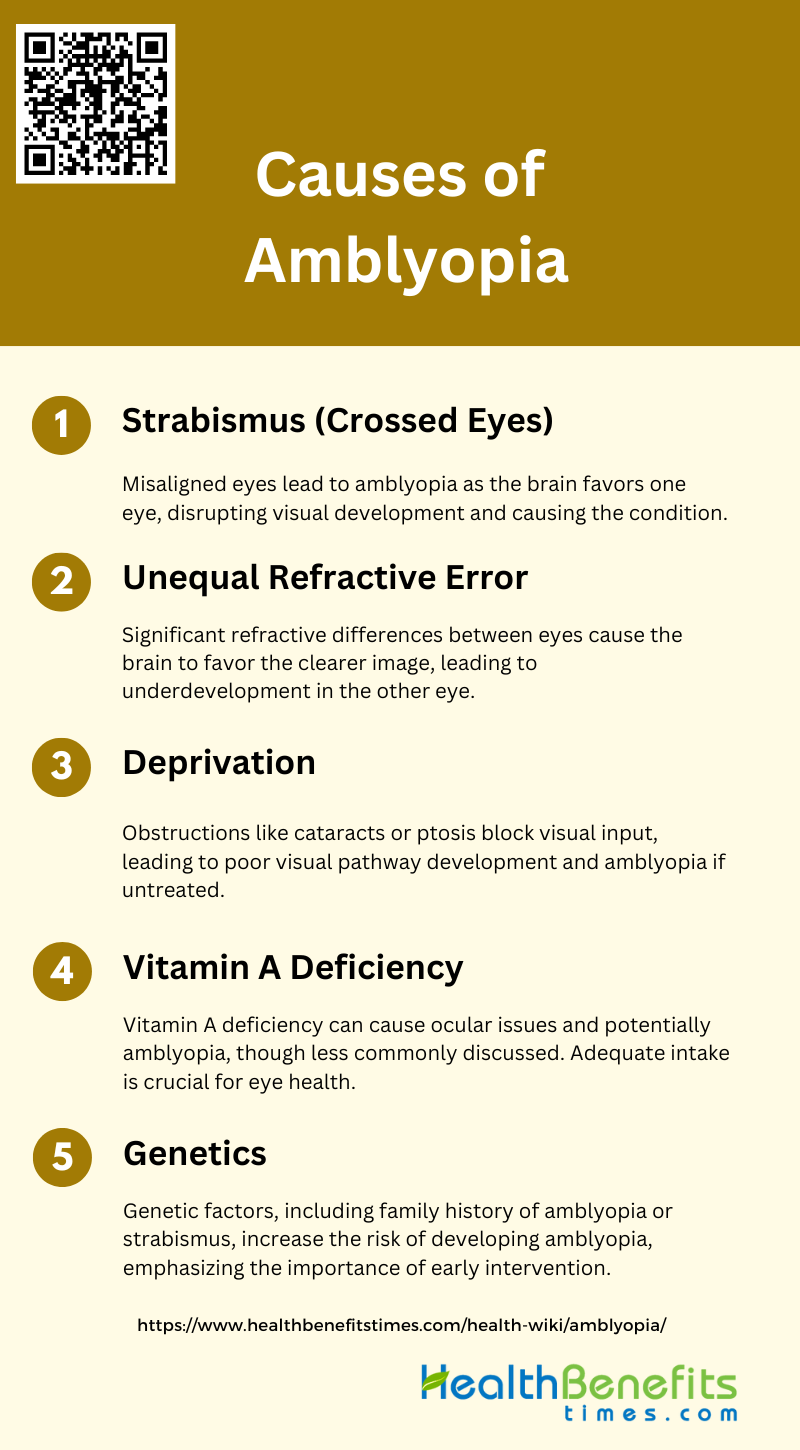
Causes of Amblyopia
Identifying these causes is essential for early intervention and effective treatment. Below are the primary causes of amblyopia:
1. Strabismus (Crossed Eyes)
Strabismus, commonly known as crossed eyes, is a significant cause of amblyopia. It occurs when the eyes are misaligned, leading to one eye focusing on an object while the other eye deviates. This misalignment disrupts the normal visual development, causing the brain to favor one eye over the other, which can result in amblyopia. Studies have shown that strabismus is a prevalent cause of amblyopia, with esotropia being the most frequent pattern observed. The condition can lead to a developmental disorder where the visual cortex does not receive proper stimulation from the misaligned eye, further contributing to the amblyopic condition.
2. Unequal Refractive Error
Unequal refractive error, or anisometropia, is another primary cause of amblyopia. This condition arises when there is a significant difference in the refractive power between the two eyes, causing one eye to focus better than the other. The brain tends to rely on the eye with the clearer image, leading to underdevelopment of the visual processing for the other eye. Research indicates that anisometropia is a major contributor to amblyopia, often resulting in a dose-dependent manner where the severity of the refractive error correlates with the degree of amblyopia. This condition can occur without any observable shrinkage of ocular dominance columns in the visual cortex, suggesting a complex neural basis for the amblyopic deficit.
3. Deprivation
Deprivation amblyopia occurs when there is an obstruction in the visual axis, such as cataracts, ptosis, or other conditions that block visual input to the eye during critical periods of visual development. This form of amblyopia is less common but can have severe consequences if not treated promptly. The lack of visual stimulation leads to poor development of the visual pathways and cortical areas responsible for vision. Studies have shown that form deprivation can result in significant visual impairment and is a critical factor in the development of amblyopia. Early detection and intervention are crucial to prevent long-term visual deficits associated with deprivation amblyopia.
4. Vitamin A Deficiency
Vitamin A deficiency, although less commonly discussed in the context of amblyopia, can contribute to visual impairment. Vitamin A is essential for maintaining healthy vision, and its deficiency can lead to a range of ocular problems, including night blindness and xerophthalmia. In severe cases, prolonged deficiency can cause damage to the retina and other parts of the eye, potentially leading to amblyopia. While the direct link between vitamin A deficiency and amblyopia is not as well-documented as other causes, ensuring adequate vitamin A intake is important for overall eye health and preventing conditions that could indirectly contribute to amblyopia.
5. Genetics
Genetics play a role in the predisposition to amblyopia, with certain genetic factors increasing the risk of developing the condition. Family history of amblyopia, strabismus, or significant refractive errors can indicate a higher likelihood of these conditions occurring in offspring. Genetic studies have shown that hereditary factors can influence the development of the visual system and the likelihood of amblyopia. Understanding the genetic basis of amblyopia can help in early identification and intervention, potentially reducing the impact of this condition on affected individuals.
Common symptoms of amblyopia
Early detection is crucial for effective treatment and to prevent long-term vision problems. Recognizing the common symptoms can help in seeking timely medical advice. Below are some of the most frequently observed symptoms of amblyopia:
- Squinting or closing one eye
- Head tilting or turning
- Poor depth perception
- Eye strain or headaches
- Eye wanders inward or outward
- Abnormal results of vision screening tests
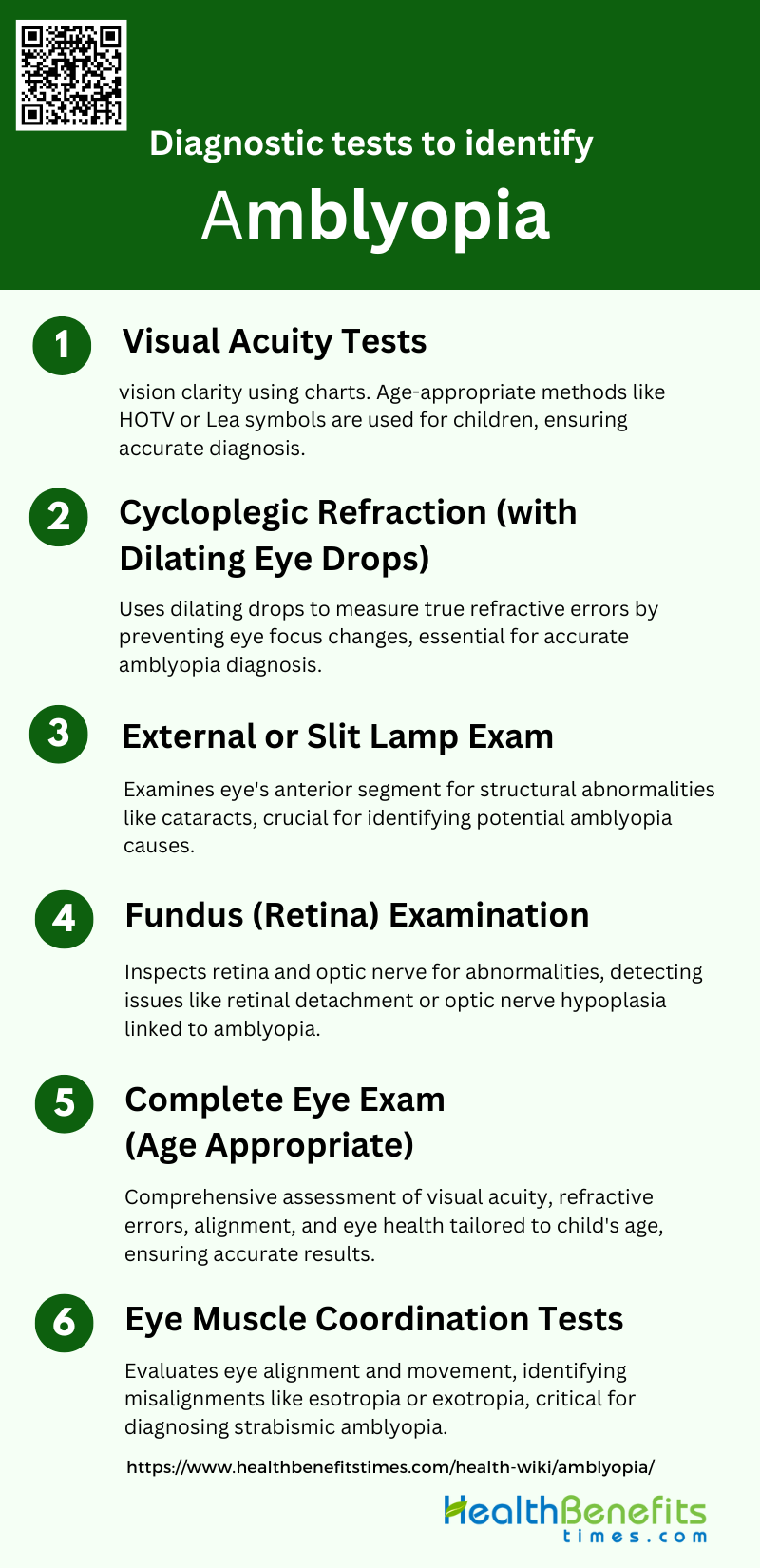
Diagnostic tests to identify amblyopia
Diagnosing amblyopia involves a series of specialized tests to evaluate visual acuity and eye alignment. Early detection through these diagnostic tests is crucial for effective treatment and preventing long-term vision problems. Below are the primary diagnostic tests used to identify amblyopia:
1. Visual Acuity Tests
Visual acuity tests are fundamental in diagnosing amblyopia, as they measure the clarity or sharpness of vision. These tests typically involve reading letters or symbols from a chart at a specific distance. In children, age-appropriate methods such as the HOTV or Lea symbols are used. Studies have shown that visual acuity tests are effective in identifying amblyopia, especially when there is a significant difference in vision between the two eyes. The accuracy of these tests can be influenced by the child’s age and cooperation, making it essential to use engaging and straightforward methods for younger children.
2. Cycloplegic Refraction (with Dilating Eye Drops)
Cycloplegic refraction involves the use of dilating eye drops to temporarily paralyze the ciliary muscle, preventing the eye from changing focus during the examination. This method provides an accurate measurement of refractive errors, which are common causes of amblyopia, such as anisometropia and hyperopia. Cycloplegic refraction is crucial for diagnosing amblyopia because it reveals the true refractive state of the eye, which can be masked by the eye’s focusing ability. This test is particularly important in young children, where accurate assessment of refractive errors is essential for effective treatment.
3. External or Slit Lamp Exam
An external or slit lamp exam is used to examine the anterior segment of the eye, including the cornea, iris, and lens. This test helps identify any structural abnormalities or opacities that could contribute to amblyopia, such as cataracts or corneal scars. The slit lamp provides a magnified view, allowing for detailed inspection of the eye’s structures. Identifying and addressing these issues is crucial for preventing or treating amblyopia, as untreated structural problems can lead to permanent vision loss7.
4. Fundus (Retina) Examination
A fundus examination involves inspecting the retina, optic disc, and blood vessels at the back of the eye. This test is essential for ruling out retinal or optic nerve abnormalities that could cause or contribute to amblyopia. Conditions such as retinal detachment, optic nerve hypoplasia, or retinal dystrophies can be detected through this examination. Early identification of these issues is vital for appropriate management and treatment, which can help prevent the progression of amblyopia.
5. Complete Eye Exam (Age Appropriate)
A complete eye exam tailored to the child’s age includes a comprehensive assessment of visual acuity, refractive errors, ocular alignment, and eye health. This holistic approach ensures that all potential causes of amblyopia are identified and addressed. Age-appropriate techniques and tools are used to engage the child and obtain accurate results. Regular comprehensive eye exams are recommended for early detection and treatment of amblyopia, which is crucial for preventing long-term visual impairment.
6. Eye Muscle Coordination Tests
Eye muscle coordination tests evaluate the alignment and movement of the eyes, which are critical for diagnosing strabismic amblyopia. These tests include cover tests, Hirschberg test, and motility assessments, which help identify misalignments such as esotropia or exotropia. Proper eye alignment is essential for binocular vision and depth perception. Identifying and correcting misalignments early can significantly improve the outcomes of amblyopia treatment, as strabismus is a common cause of this condition.
Treatment Options for amblyopia
Amblyopia can be effectively managed through various treatment methods aimed at improving the visual acuity of the affected eye and ensuring proper eye coordination. Early intervention is key to successful outcomes. Below are some common treatment options for amblyopia:
1. Corrective Eyewear (Glasses or Contact Lenses)
Corrective eyewear, such as glasses or contact lenses, is often the first line of treatment for amblyopia, particularly in cases of anisometropic amblyopia where there is a significant difference in refractive error between the two eyes. Studies have shown that early initiation and consistent use of spectacle correction can significantly improve visual acuity in the amblyopic eye, sometimes even resolving the condition entirely. However, compliance with wearing glasses can be challenging, especially in young children who may find them uncomfortable or visually unappealing. Despite these challenges refractive correction remains a cornerstone of amblyopia treatment due to its non-invasive nature and effectiveness.
2. Wearing an Eye Patch
Patching the dominant eye is a traditional and widely used method to treat amblyopia. By occluding the stronger eye, the weaker eye is forced to work harder, thereby improving its visual acuity. The effectiveness of patching has been well-documented, with studies indicating significant improvements in visual acuity in the amblyopic eye. However, adherence to patching regimens can be problematic, as children often find wearing an eye patch uncomfortable and socially stigmatizing. Despite these compliance issues, patching remains a highly effective treatment, especially when combined with other therapies such as atropine drops.
3. Atropine Eye Drops
Atropine eye drops are used as an alternative to patching, particularly in cases where compliance with patching is poor. Atropine works by temporarily blurring vision in the dominant eye, thereby encouraging the use of the amblyopic eye. Research has shown that atropine is as effective as patching in improving visual acuity in children with moderate amblyopia. Long-term studies have demonstrated that the benefits of atropine treatment are maintained over time, with many children achieving good visual acuity in the amblyopic eye. However, like patching, atropine treatment also faces compliance challenges and potential side effects such as light sensitivity and difficulty with near vision tasks.
4. Vision Therapy Exercises
Vision therapy exercises are designed to improve the coordination and focusing abilities of the eyes. These exercises can include activities such as tracking moving objects, focusing on near and far objects, and using computer-based programs that present visual stimuli to both eyes. Recent studies have explored the use of perceptual learning and video gaming as part of vision therapy, showing promising results in improving visual acuity and binocular function. However, these newer approaches are still under investigation, and more robust clinical trials are needed to establish their efficacy compared to traditional treatments.
5. Surgical Interventions (if applicable)
Surgical interventions are generally considered when other treatments have failed or are not feasible. Surgical options may include procedures to correct strabismus (misalignment of the eyes) or refractive surgery to correct significant differences in refractive error between the eyes. Studies have shown that surgical correction can be effective in improving visual acuity, particularly in cases where glasses and patching have not been successful. However, surgery carries inherent risks and is usually reserved for specific cases where non-surgical treatments have proven inadequate. The decision to proceed with surgery is typically made on a case-by-case basis, considering the individual needs and circumstances of the patient.
Potential risks and side effects of treatments
While treatments for amblyopia are generally effective, they can come with certain risks and side effects. It’s important to be aware of these potential issues to manage them appropriately and ensure the best possible outcome. Below are some common risks and side effects associated with amblyopia treatments:
1. Reverse Amblyopia
Reverse amblyopia, also known as occlusion amblyopia, can occur when the treatment for amblyopia, such as patching the dominant eye, leads to a decrease in visual acuity in the previously stronger eye. This condition is particularly concerning in younger children, where the visual system is still developing. Studies have shown that while patching is effective in improving the amblyopic eye, there is a risk of inducing amblyopia in the patched eye if not monitored carefully. Therefore, it is crucial to balance the duration and intensity of patching to avoid this adverse effect.
2. Skin Irritation or Allergic Reactions
Skin irritation or allergic reactions are common side effects associated with the use of adhesive eye patches in amblyopia treatment. The prolonged use of these patches can lead to skin redness, itching, and even blistering in some cases. Studies have highlighted the importance of using hypoallergenic materials and ensuring proper skin care to mitigate these side effects. Additionally, alternative treatments such as atropine drops can be considered to avoid skin-related issues altogether.
3. Eye Irritation from Atropine Drops
Atropine drops, used as an alternative to patching, can cause eye irritation, including redness, stinging, and photophobia. These side effects are dose-dependent, with higher concentrations leading to more pronounced symptoms. Research indicates that lower concentrations of atropine (e.g., 0.01%) are effective in treating amblyopia while minimizing adverse effects. However, even at low doses, some children may still experience discomfort, necessitating careful monitoring and possible adjustment of treatment.
4. Psychological Impact
The psychological impact of amblyopia treatment, particularly patching, can be significant. Children may experience social stigma, reduced self-esteem, and emotional distress due to the visible nature of the treatment. Studies have shown that these psychological effects can affect treatment adherence and overall quality of life. It is essential to provide psychological support and counseling to both children and their families to address these issues and improve treatment outcomes.
5. Difficulty with Depth Perception
This can affect a child’s ability to perform tasks that require precise hand-eye coordination, such as sports and certain school activities. Research suggests that while treatments like patching and atropine can improve visual acuity, they may not fully restore binocular vision and depth perception. Therefore, additional therapies focusing on binocular vision may be necessary.
6. Reduced Vision Improvement in Older Children
The effectiveness of amblyopia treatment decreases with age, with older children showing less improvement in visual acuity compared to younger children. Studies have demonstrated that early intervention is crucial for optimal outcomes, as the visual system is more plastic and responsive to treatment in younger children. However, recent research indicates that some degree of improvement is still possible in older children, suggesting that treatment should not be entirely ruled out based on age alone.
7. Risk of Permanent Vision Loss
In rare cases, amblyopia treatment can lead to permanent vision loss if not properly managed. This risk is particularly associated with aggressive or prolonged patching, which can cause irreversible damage to the visual system. Long-term studies have shown that while most children achieve significant improvement, a small percentage may experience adverse outcomes. Continuous monitoring and individualized treatment plans are essential to minimize this risk and ensure the best possible visual outcomes.
Prevention of amblyopia
Preventing amblyopia involves early detection and addressing risk factors that can impair visual development in children. Regular eye examinations and prompt treatment of underlying conditions are essential. Below are some key strategies for preventing amblyopia:
1. Regular Eye Examinations
Regular eye examinations are crucial in the early detection and prevention of amblyopia. Early identification of risk factors such as refractive errors, strabismus, or other ocular conditions can significantly improve treatment outcomes. Studies have shown that early intervention, particularly before the age of five, can lead to better visual acuity outcomes and reduce the prevalence of amblyopia. Regular screenings allow for timely initiation of treatments such as corrective lenses or occlusion therapy, which are essential in preventing the progression of amblyopia.
2. Addressing Refractive Errors
Addressing refractive errors is a fundamental step in preventing amblyopia. Corrective lenses can significantly improve visual acuity in children with anisometropic amblyopia or ametropic amblyopia. Research indicates that consistent use of spectacles alone can resolve amblyopia in a majority of cases, especially when initiated early. For those who do not respond to glasses alone, additional treatments such as patching or atropine penalization can be effective. Ensuring that children adhere to their prescribed refractive correction is essential for the success of these interventions.
3. Educating Parents and Caregivers
Educating parents and caregivers about the importance of early detection and treatment of amblyopia is vital. Parental awareness and involvement can significantly influence treatment adherence and outcomes. Studies have shown that compliance with treatments such as patching or atropine drops is higher when parents are well-informed and actively involved in the treatment process. Providing educational resources and support can help parents understand the necessity of regular eye exams and adherence to prescribed treatments, ultimately improving the prognosis for children with amblyopia.
4. Treating Eye Conditions
Treating underlying eye conditions that contribute to amblyopia, such as strabismus or cataracts, is essential for preventing the condition. Surgical interventions or other treatments to correct these conditions can prevent the development of amblyopia or improve outcomes when combined with other therapies. Early and effective treatment of these conditions can help ensure that both eyes develop properly, reducing the risk of amblyopia and improving overall visual health.
5. Use of Atropine or Patching
The use of atropine drops or patching of the dominant eye are well-established methods for treating amblyopia. Both treatments aim to stimulate the amblyopic eye by temporarily reducing the visual input from the dominant eye. Research has shown that these methods are equally effective in improving visual acuity in children with amblyopia, with long-term benefits maintained up to 15 years of age. However, adherence to these treatments can be challenging, and ongoing support and monitoring are necessary to ensure their effectiveness. Recent studies also explore novel approaches such as binocular treatments, which may offer additional benefits and improve adherence.