Amaurosis fugax is a medical condition characterized by a temporary, painless loss of vision in one or both eyes due to a lack of blood flow to the retina. This transient vision loss, which can last from seconds to minutes, is often described as a “curtain” descending over the field of vision. The condition is typically caused by an embolic event, where a blood clot or plaque blocks an artery supplying the retina, often originating from larger arteries such as the carotid artery. Amaurosis fugax can be a warning sign of more serious vascular issues, including an increased risk of stroke, and thus requires prompt medical evaluation and management to address underlying risk factors such as heart disease, high blood pressure, and diabetes.
Causes of Amaurosis Fugax
This temporary visual impairment is often a warning sign of more serious vascular issues. Understanding the causes is crucial for timely intervention and prevention of potential complications. Below are some of the primary causes of Amaurosis Fugax:
- Brain tumor
- Head injury
- History of multiple sclerosis
- History of systemic lupus erythematosus
- Migraine headaches
- Optic neuritis, an inflammation of the optic nerve
- Polyarteritis nodosa, a disease that affects the blood vessels
- Atherosclerosis
- Blood clots
- Hypertension
- Diabetes
Symptoms of Amaurosis Fugax
This condition can present with various symptoms that typically resolve within minutes. Key symptoms include:
1. Sudden Vision Loss: A rapid onset of vision loss in one eye, which can last from a few seconds to several minutes.
2. Curtain Effect: A sensation of a dark curtain or shadow descending over the field of vision.
3. Blurriness: Blurred or dim vision in one eye.
4. Complete Vision Loss: In some cases, there may be a complete loss of vision in the affected eye.
5. Transient Nature: The vision loss is usually temporary and vision often returns to normal after the episode.
Diagnosis of Amaurosis Fugax
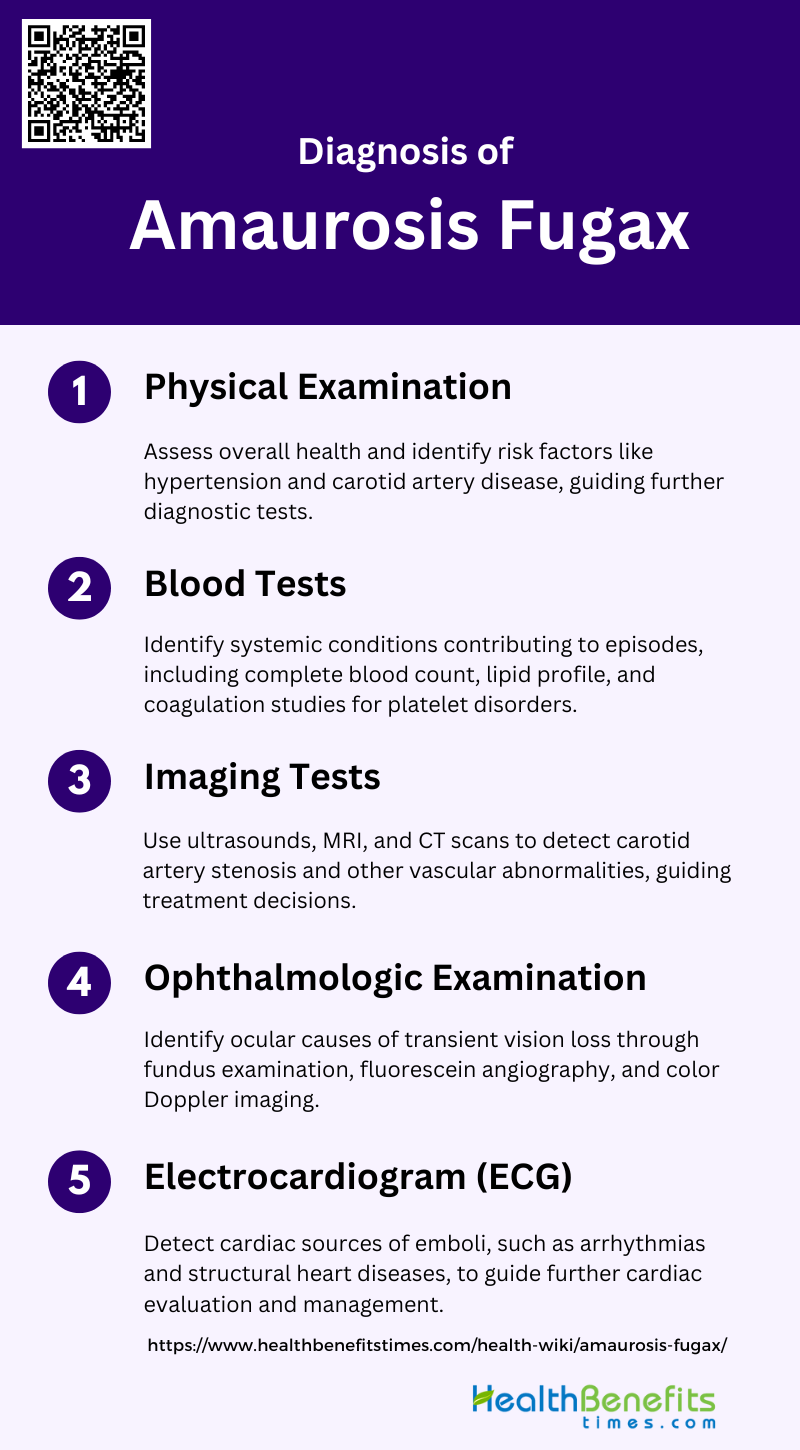
Diagnosing amaurosis fugax involves a comprehensive evaluation to identify the underlying cause of transient vision loss. Physicians typically conduct a detailed patient history and physical examination, followed by specific diagnostic tests. The following steps are commonly included in the diagnostic process:
1. Physical Examination
A thorough physical examination is crucial in diagnosing amaurosis fugax. This includes assessing the patient’s overall health and identifying any potential risk factors such as hypertension, hypercholesterolemia, and coronary artery disease, which are commonly associated with transient vision loss episodes. Additionally, the presence of carotid bruits during auscultation of the neck can suggest carotid artery disease, a significant cause of amaurosis fugax. Physical examination findings can guide further diagnostic testing and help differentiate between vascular and non-vascular causes of the symptoms.
2. Blood Tests
Blood tests are essential in the diagnostic workup of amaurosis fugax to identify underlying systemic conditions that may contribute to the episodes. These tests can include a complete blood count, lipid profile, and coagulation studies to detect platelet disorders or hypercoagulable states. Additionally, blood tests can help identify inflammatory markers that may indicate conditions such as giant cell arteritis, which can cause increased vessel resistance and amaurosis fugax. Identifying these systemic conditions is crucial for tailoring appropriate treatment strategies and preventing further episodes.
3. Imaging Tests
Imaging tests such as ultrasounds, MRI, and CT scans play a pivotal role in diagnosing amaurosis fugax. Carotid duplex ultrasound is commonly used to detect carotid artery stenosis, which is a significant cause of transient vision loss. Magnetic resonance angiography (MRA) and conventional arteriography can provide detailed images of the carotid and ophthalmic arteries, helping to identify atherosclerotic lesions or other vascular abnormalities. These imaging modalities are essential for determining the presence and extent of vascular occlusive disease, guiding treatment decisions such as surgical intervention or anticoagulation therapy.
4. Ophthalmologic Examination
An ophthalmologic examination is critical in diagnosing amaurosis fugax, as it helps to identify ocular causes of transient vision loss. Fundus examination can reveal Hollenhorst plaques, which are cholesterol emboli in the retinal arteries and are indicative of carotid artery disease. Fluorescein angiography can capture episodes of amaurosis fugax and provide insights into retinal blood flow and potential vasospasms. Additionally, color Doppler imaging can assess blood flow in the ophthalmic and central retinal arteries, helping to detect internal carotid artery stenosis. These findings are crucial for differentiating ocular from systemic causes of amaurosis fugax.
5. Electrocardiogram (ECG)
An electrocardiogram (ECG) is an important diagnostic tool in the evaluation of amaurosis fugax, particularly in identifying cardiac sources of emboli. Heart disease, including atrial fibrillation and other arrhythmias, can lead to embolic events that cause transient vision loss. An ECG can detect these arrhythmias and other cardiac abnormalities, guiding further cardiac evaluation and management. Additionally, echocardiography may be performed to identify structural heart diseases such as mitral valve prolapse, which has been observed in some patients with amaurosis fugax. Identifying cardiac sources of emboli is essential for preventing recurrent episodes and reducing the risk of stroke.
Treatment of Amaurosis Fugax
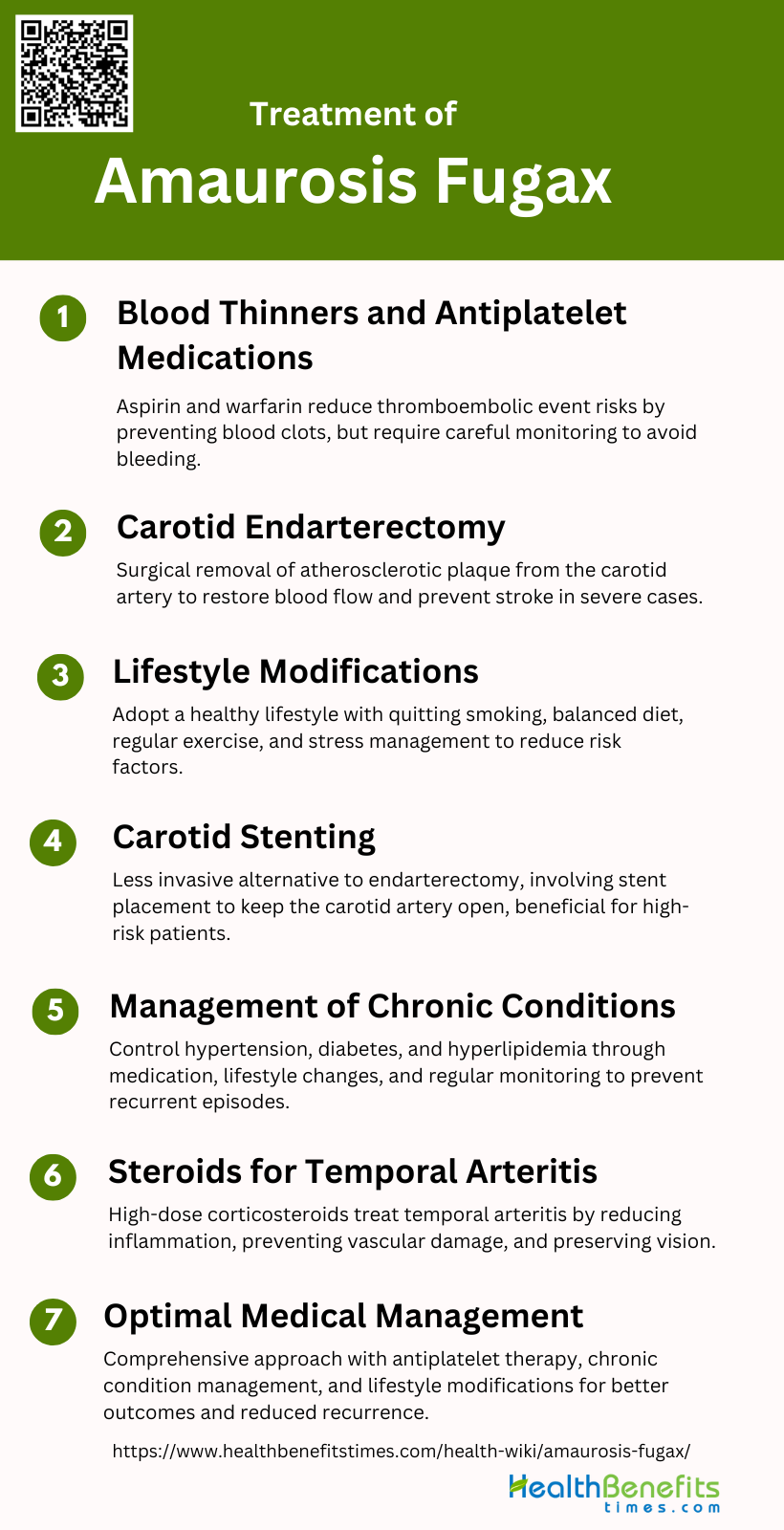
The treatment of amaurosis fugax focuses on addressing the underlying causes to prevent future episodes of transient vision loss. Management strategies may include lifestyle changes, medications, and surgical interventions. The following steps outline common treatment approaches:
1. Blood Thinners and Antiplatelet Medications
Blood thinners and antiplatelet medications are commonly used in the treatment of amaurosis fugax to prevent thromboembolic events. These medications, such as aspirin and warfarin, help reduce the risk of stroke by preventing blood clots from forming or growing. Studies have shown that anticoagulation therapy can be effective in managing symptoms and preventing further episodes of amaurosis fugax, especially in patients with underlying carotid artery disease. However, the effectiveness of these medications can vary, and careful monitoring is required to balance the benefits against the risk of bleeding complications.
2. Carotid Endarterectomy
Carotid endarterectomy is a surgical procedure that removes atherosclerotic plaque from the carotid artery to restore normal blood flow and prevent stroke. This procedure is particularly beneficial for patients with significant carotid stenosis and those who have experienced amaurosis fugax due to ulcerated plaques. Studies have demonstrated that carotid endarterectomy can significantly reduce the risk of recurrent amaurosis fugax and other ischemic events, making it a recommended treatment for patients with severe carotid artery disease. The procedure has been shown to have a low perioperative risk and favorable long-term outcomes.
3. Lifestyle Modifications
Lifestyle modifications play a crucial role in the management and prevention of amaurosis fugax. Patients are advised to adopt a healthy lifestyle, which includes quitting smoking, maintaining a balanced diet, engaging in regular physical activity, and managing stress. These changes can help reduce the risk factors associated with carotid artery disease, such as hypertension, diabetes, and hyperlipidemia. By addressing these underlying conditions, patients can lower their risk of recurrent episodes and improve their overall cardiovascular health.
4. Carotid Stenting
Carotid stenting is a less invasive alternative to carotid endarterectomy, involving the placement of a stent to keep the carotid artery open. This procedure is particularly useful for patients who are at high surgical risk or have contraindications to surgery. Studies have shown that carotid stenting can be effective in reducing the risk of stroke and managing symptoms of amaurosis fugax. However, the choice between stenting and endarterectomy should be individualized based on the patient’s overall health, anatomy of the carotid lesion, and the presence of comorbid conditions.
5. Management of Chronic Conditions
Effective management of chronic conditions such as hypertension, diabetes, and hyperlipidemia is essential in preventing amaurosis fugax and reducing the risk of stroke. Patients with these conditions should work closely with their healthcare providers to achieve optimal control through medication, lifestyle changes, and regular monitoring. Proper management of these risk factors can help stabilize atherosclerotic plaques and prevent the progression of carotid artery disease, thereby reducing the likelihood of recurrent episodes of amaurosis fugax.
6. Steroids for Temporal Arteritis
In cases where amaurosis fugax is caused by temporal arteritis, corticosteroids are the treatment of choice. Temporal arteritis, an inflammatory condition affecting the blood vessels, can lead to vision loss if not promptly treated. High-dose corticosteroids can reduce inflammation and prevent further vascular damage, thereby preserving vision. Early diagnosis and treatment are crucial, as delayed intervention can result in permanent visual impairment. Patients with suspected temporal arteritis should be referred to a specialist for further evaluation and management.
7. Optimal Medical Management
Optimal medical management involves a comprehensive approach to treating amaurosis fugax, addressing both the immediate symptoms and the underlying causes. This includes the use of antiplatelet or anticoagulant therapy, management of chronic conditions, and lifestyle modifications. Regular follow-up and monitoring are essential to assess the effectiveness of the treatment plan and make necessary adjustments. By adopting a holistic approach, healthcare providers can help patients achieve better outcomes and reduce the risk of recurrent episodes and associated complications.
Prevention of Amaurosis Fugax
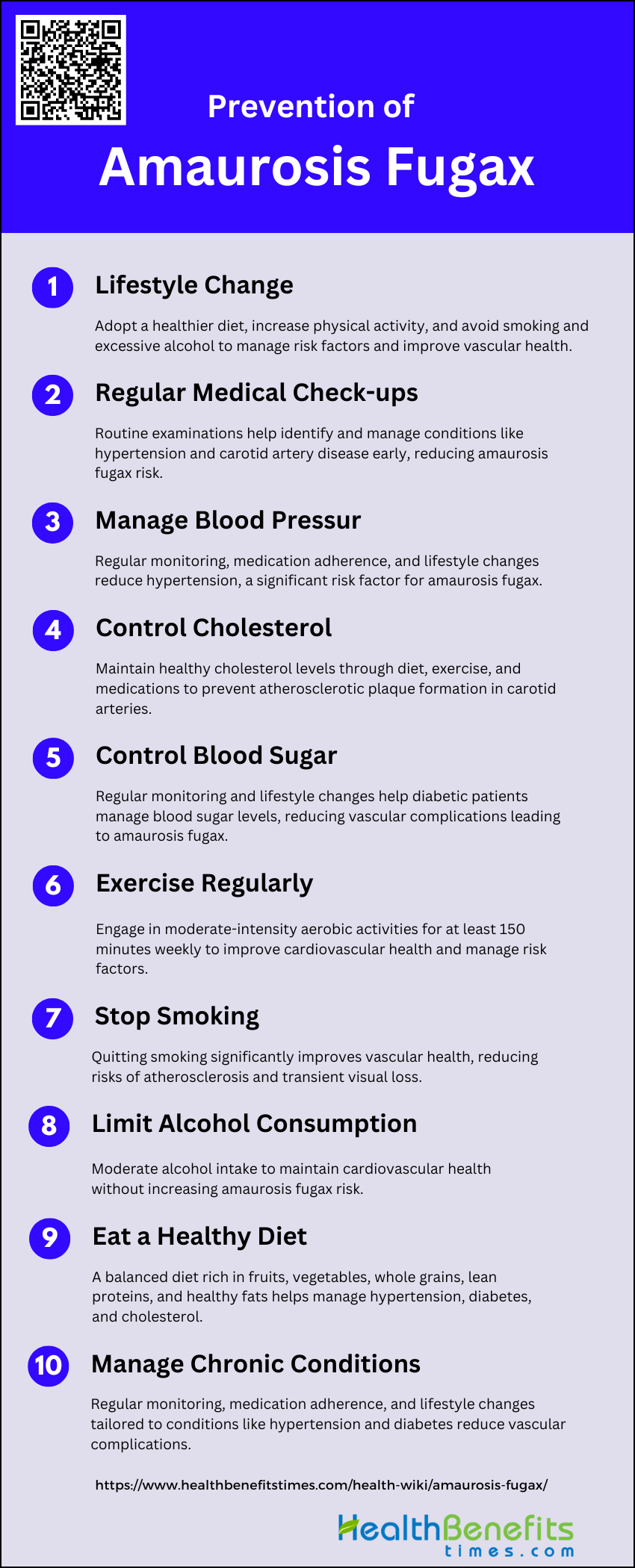
Preventing amaurosis fugax involves managing risk factors and underlying conditions that may contribute to transient vision loss. This can include lifestyle modifications, medical treatments, and regular monitoring. The following steps are commonly recommended for prevention:
1. Lifestyle Changes
Implementing lifestyle changes can significantly reduce the risk of amaurosis fugax. These changes include adopting a healthier diet, increasing physical activity, and avoiding smoking and excessive alcohol consumption. Studies have shown that lifestyle modifications can help manage underlying conditions such as hypertension, diabetes, and hypercholesterolemia, which are known risk factors for amaurosis fugax. Additionally, maintaining a healthy weight and managing stress levels can further contribute to overall vascular health, potentially reducing the frequency and severity of amaurosis fugax episodes.
2. Regular Medical Check-ups
Regular medical check-ups are crucial for the early detection and management of conditions that may lead to amaurosis fugax. Routine examinations can help identify risk factors such as hypertension, diabetes, and hypercholesterolemia, allowing for timely intervention. Regular monitoring can also detect early signs of carotid artery disease, which is a common cause of amaurosis fugax. By keeping up with scheduled medical appointments, patients can receive appropriate treatments and lifestyle recommendations to prevent the occurrence of amaurosis fugax and related complications.
3. Manage Blood Pressure
Managing blood pressure is essential in preventing amaurosis fugax, as hypertension is a significant risk factor for this condition. High blood pressure can lead to the development of atherosclerosis, which can cause transient ischemic attacks and amaurosis fugax. Effective blood pressure management involves regular monitoring, medication adherence, and lifestyle changes such as reducing salt intake, maintaining a healthy weight, and engaging in regular physical activity. Controlling blood pressure can reduce the risk of vascular complications and improve overall ocular health.
4. Control Cholesterol
Controlling cholesterol levels is vital in preventing amaurosis fugax, as high cholesterol can lead to the formation of atherosclerotic plaques in the carotid arteries, which can cause transient visual loss. Patients should aim to maintain healthy cholesterol levels through a balanced diet low in saturated fats and cholesterol, regular exercise, and, if necessary, cholesterol-lowering medications. Regular lipid profile tests can help monitor cholesterol levels and guide treatment decisions, reducing the risk of amaurosis fugax and other cardiovascular events.
5. Control Blood Sugar
Controlling blood sugar levels is crucial for patients with diabetes, as uncontrolled diabetes can increase the risk of amaurosis fugax. High blood sugar levels can damage blood vessels, leading to vascular complications that may result in transient visual loss. Effective blood sugar management involves regular monitoring, medication adherence, and lifestyle changes such as a healthy diet and regular physical activity. By maintaining optimal blood sugar levels, patients can reduce the risk of amaurosis fugax and improve overall vascular health.
6. Exercise Regularly
Regular exercise is an important preventive measure for amaurosis fugax, as it helps improve cardiovascular health and manage risk factors such as hypertension, diabetes, and high cholesterol. Engaging in moderate-intensity aerobic activities, such as walking, cycling, or swimming, for at least 150 minutes per week can enhance blood circulation and reduce the risk of atherosclerosis. Exercise also helps maintain a healthy weight and reduces stress, further contributing to the prevention of amaurosis fugax and other vascular conditions.
7. Stop Smoking
Smoking cessation is critical in preventing amaurosis fugax, as smoking is a major risk factor for atherosclerosis and vascular diseases. Smoking damages blood vessels, increases blood pressure, and raises cholesterol levels, all of which can contribute to the development of amaurosis fugax. Quitting smoking can significantly improve vascular health and reduce the risk of transient visual loss and other cardiovascular events. Support programs, medications, and lifestyle changes can aid in smoking cessation and promote long-term health benefits.
8. Limit Alcohol Consumption
Limiting alcohol consumption is important in preventing amaurosis fugax, as excessive alcohol intake can contribute to hypertension, high cholesterol, and other vascular risk factors. Moderate alcohol consumption, defined as up to one drink per day for women and up to two drinks per day for men, can help maintain cardiovascular health without increasing the risk of amaurosis fugax. Patients should be advised to monitor their alcohol intake and seek support if they have difficulty reducing their consumption.
9. Eat a Healthy Diet
Eating a healthy diet is essential in preventing amaurosis fugax, as it helps manage risk factors such as hypertension, diabetes, and high cholesterol. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can improve vascular health and reduce the risk of atherosclerosis. Patients should be encouraged to limit their intake of saturated fats, trans fats, cholesterol, and sodium to maintain optimal cardiovascular health and prevent transient visual loss.
10. Manage Chronic Conditions
Managing chronic conditions such as hypertension, diabetes, and hypercholesterolemia is crucial in preventing amaurosis fugax. Effective management involves regular monitoring, medication adherence, and lifestyle changes tailored to each condition. By controlling these underlying health issues, patients can reduce the risk of vascular complications that may lead to amaurosis fugax. Comprehensive care plans that address all aspects of a patient’s health can help prevent transient visual loss and improve overall quality of life.