Alveoplasty is a common pre-prosthetic surgical procedure aimed at reshaping and smoothing the jawbone (alveolar ridge) to create a more suitable anatomical environment for the placement of dentures or other dental prosthetics. This procedure involves the removal of any irregularities or sharp edges in the bone, which can improve the retention, stability, and comfort of the dentures. Alveoplasty is often performed after tooth extractions to ensure that the bone heals in a smooth and even manner, facilitating better support for the prosthetic devices. The procedure can be done using various techniques, including the use of surgical instruments or lasers, and is typically followed by suturing to promote proper healing of the soft tissues.
Who needs Alveoplasty?
It involves reshaping and smoothing the jawbone to ensure a better fit for these dental appliances. Here are some common scenarios where alveoplasty may be necessary:
1. Preparation for Dentures
Alveoplasty is often necessary for patients preparing to receive dentures. This pre-prosthetic surgical procedure aims to create a smooth and contoured alveolar ridge, which is essential for the proper fit and comfort of dentures. The procedure involves the recontouring of the alveolar bone to eliminate any irregularities, sharp edges, or undercuts that could interfere with the stability and retention of the dentures. Studies have shown that alveoplasty significantly improves the quality of the denture-bearing area, leading to better patient outcomes and satisfaction. Proper alveoplasty ensures that both the hard and soft tissues are in optimal condition, enhancing the patient’s ability to wear dentures comfortably and effectively.
2. Dental Implants
The success of dental implants largely depends on the quality and quantity of the alveolar bone. Alveoplasty helps in creating a stable and adequate bony base for implant placement, which is vital for the long-term success of the implants. Techniques such as alveolar ridge preservation and augmentation are often employed to maintain or enhance the alveolar ridge after tooth extraction, ensuring that there is sufficient bone volume for implant placement. These procedures not only improve the aesthetic outcomes but also reduce the need for additional augmentation procedures before implant placement.
3. Post-Extraction
After tooth extraction, alveoplasty may be performed to smooth and reshape the alveolar ridge. This is particularly important in cases where the extraction has left behind irregular bony spicules or sharp edges that could cause discomfort or complications during the healing process. Alveoplasty facilitates better wound healing and prepares the site for future prosthetic rehabilitation, such as dentures or implants. The procedure is often indicated in patients who have undergone multiple extractions or have significant bone loss, as it helps in creating a more favorable environment for subsequent dental treatments.
4. Bone Irregularities
Patients with bone irregularities, such as sharp ridges, undercuts, or non-vital bone, may require alveoplasty to correct these issues. These irregularities can cause discomfort, impede proper oral function, and complicate the placement of dental prosthetics. Alveoplasty addresses these concerns by recontouring the alveolar bone, ensuring a smoother and more uniform ridge. This procedure is particularly beneficial for patients with a history of antiresorptive treatment, as it helps in managing necrotic bone changes and improving the overall condition of the alveolar ridge. By addressing bone irregularities, alveoplasty enhances the patient’s oral health and prepares the site for future dental procedures.
Purpose of Alveoloplasty
Alveoloplasty is a surgical procedure designed to reshape and smooth the jawbone, typically performed after tooth extraction or in preparation for dentures. This procedure aims to enhance the fit and comfort of dental prosthetics, facilitate healing, and improve overall oral function. The primary purposes of alveoloplasty include:
1. Fitting for Dentures
This procedure helps in creating an optimal anatomical environment, which is essential for the stability and retention of dentures. By removing any irregularities, sharp ridges, or undercuts, alveoloplasty enhances the comfort and functionality of the dentures, thereby improving the patient’s ability to wear them effectively. Proper alveoloplasty ensures that the denture base has adequate bony support and proper soft tissue coverage, which are critical for successful denture fabrication and patient satisfaction.
2. Jaw Bone Reshaping
Jaw bone reshaping through alveoloplasty is performed to contour the alveolar bone, making it more uniform and smooth. This is particularly important after multiple tooth extractions, where the bone may have irregularities or sharp spicules that can cause discomfort or complications. The procedure involves the surgical removal or recontouring of the alveolar process to create a more favorable bone structure for future dental prosthetics or implants. This reshaping not only facilitates the construction of better-fitting dentures but also improves the overall oral health by preventing issues related to uneven bone surfaces.
3. To Repair Bone after Tooth Extractions
Alveoloplasty is often performed to repair and reshape the alveolar bone following tooth extractions. The procedure helps in minimizing the loss of alveolar ridge volume, which is a common consequence of tooth removal. By preserving the ridge height and width, alveoloplasty ensures that the bone structure remains suitable for future dental implants or prosthetic devices. This preservation is crucial for maintaining the integrity of the jawbone and preventing complications that could arise from significant bone loss, such as difficulties in prosthodontic rehabilitation.
4. Enhancing Oral Health
Enhancing oral health is another significant purpose of alveoloplasty. By smoothing and reshaping the alveolar ridge, the procedure helps in eliminating areas where food particles and bacteria could accumulate, thereby reducing the risk of infections and periodontal diseases. Additionally, a well-contoured alveolar ridge supports better oral hygiene practices, as it is easier to clean and maintain. This contributes to the overall health of the oral cavity, ensuring that both hard and soft tissues are in optimal condition for any future dental treatments.
5. Improving Aesthetic Outcomes
Improving aesthetic outcomes is a key objective of alveoloplasty. The procedure helps in creating a more natural and aesthetically pleasing contour of the jawbone, which is particularly important for patients who require dental prosthetics or implants. A well-shaped alveolar ridge provides a better foundation for these devices, ensuring that they look and function more naturally. This not only enhances the patient’s appearance but also boosts their confidence and quality of life. The aesthetic improvements achieved through alveoloplasty are essential for achieving satisfactory long-term results in dental rehabilitation.
Types of Alveoloplasty
Here are the common types of Alveoloplasty:
1. Post-extraction Alveoloplasty
Post-extraction alveoloplasty is a surgical procedure performed immediately after tooth extraction to smooth and reshape the alveolar ridge. This technique is essential to ensure that the bone and soft tissues are in optimal condition for future prosthetic placement. The primary goal is to remove any sharp bony edges or irregularities that could interfere with the healing process or the fit of a dental prosthesis. Studies have shown that this procedure can significantly improve the comfort and functionality of dentures, as well as enhance the aesthetic outcome for patients.
2. Simple Alveoloplasty
Simple alveoloplasty involves the minimal reshaping of the alveolar ridge, typically performed when there are minor irregularities or sharp edges following tooth extraction. This procedure is less invasive compared to other types of alveoloplasty and is often done to facilitate the placement of dentures or other dental prosthetics. The simplicity of this technique makes it a preferred choice in many clinical situations, as it effectively prepares the alveolar ridge without extensive surgical intervention. Research indicates that simple alveoloplasty is effective in preserving the residual alveolar ridge and ensuring a better fit for dental prostheses.
3. Intraseptal (Dean’s) Alveoloplasty
Intraseptal alveoloplasty, also known as Dean’s alveoloplasty, involves the removal of the interseptal bone while preserving the labial and lingual cortical plates. This technique was first proposed by Sir O. T. Dean in 1936 and is particularly useful in cases where there is a need to reduce the height of the alveolar ridge without compromising the cortical bone. The procedure helps in maintaining the structural integrity of the alveolar ridge and provides a stable base for prosthetic placement. Studies have demonstrated the effectiveness of this technique in managing complex dental conditions and enhancing the outcomes of prosthetic rehabilitation.
4. Obwegeser’s Modification
Obwegeser’s modification of alveoloplasty is a more advanced technique that involves the use of guided surgery to achieve precise reshaping of the alveolar ridge. This method utilizes data from cone-beam computed tomography (CBCT) to create a surgical guide, allowing for accurate and controlled bone reduction. The technique is particularly beneficial in cases requiring extensive alveolar ridge modification, such as in the placement of implant-supported prostheses. Research has shown that Obwegeser’s modification can significantly improve the accuracy of alveoloplasty and enhance the overall success of dental implant procedures.
The Alveoplasty Procedure
Alveoplasty is a surgical procedure aimed at reshaping and smoothing the jawbone, typically performed to prepare the mouth for dentures or other dental prosthetics. This process ensures a better fit and comfort for the patient. Below are the steps involved in the alveoplasty procedure:
1. Preoperative Assessment
- Patient Evaluation: A thorough medical and dental history is taken.
- Radiographic Examination: X-rays or CT scans are used to assess the jawbone structure.
- Treatment Planning: Discuss the goals and expectations with the patient. Obtain informed consent.
2. Preparation
- Anesthesia: Local anesthesia is administered to numb the surgical area. In some cases, general anesthesia may be used for extensive procedures or anxious patients.
- Sterilization: The surgical site is cleaned and sterilized to prevent infection.
3. Incision
- Gingival Incision: A scalpel is used to make an incision in the gum tissue overlying the bone that needs reshaping.
- Flap Creation: The gum tissue is carefully reflected (pulled back) to expose the underlying bone.
4. Bone Recontouring
- Removal of Bony Protrusions: Using a surgical bur, bone file, or rongeurs, the surgeon removes any sharp edges or bony projections.
- Smoothing the Bone: The bone is then smoothed and contoured to achieve a uniform surface. This step ensures a stable and comfortable fit for dental prosthetics.
5. Irrigation
- Wound Cleaning: The surgical site is irrigated with sterile saline solution to remove bone debris and minimize the risk of infection.
6. Closure
- Repositioning the Gum Flap: The gum tissue is repositioned over the reshaped bone.
- Suturing: The incision is closed with sutures. Absorbable sutures may dissolve on their own, while non-absorbable sutures will need to be removed after a week or so.
7. Postoperative Care
- Pain Management: Prescribe pain relief medications if necessary.
- Antibiotics: An antibiotic regimen may be prescribed to prevent infection.
- Instructions: Provide the patient with detailed postoperative care instructions, including oral hygiene practices and dietary recommendations.
- Follow-Up: Schedule follow-up appointments to monitor healing and address any complications.
Post-Operative Care and Recovery of Alveoplasty
Proper post-operative care is crucial for a smooth recovery following an alveoplasty procedure. Adhering to the recommended guidelines can help minimize complications and promote healing. Below are the key steps for post-operative care and recovery:
1. Pain Management
Effective pain management is crucial for enhanced recovery after alveoplasty. A multimodal approach combining paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and local anesthetics can provide effective analgesia while minimizing side effects. This strategy not only improves the quality of recovery but also reduces the stress response, facilitates mobilization, and allows for the resumption of oral intake. Additionally, early intervention with multimodal analgesia and stress reduction techniques, such as regional anesthesia, can significantly enhance recovery and decrease hospital stay.
2. Diet
Post-operative diet management is essential for recovery after alveoplasty. Patients should initially consume a soft diet to avoid disturbing the surgical site and gradually progress to a normal diet as tolerated. Studies have shown that patients who received moxifloxacin (MXF) postoperatively were able to tolerate a diet of normal consistency sooner compared to those who received amoxicillin and clavulanic acid (AMX-CLV). Proper nutritional management, including early oral feeding, can significantly reduce hospital stay and promote early recovery. Patients and caregivers often have questions about the type, consistency, and temperature of food, which should be addressed during preoperative consultations.
3. Oral Hygiene
Maintaining oral hygiene post-operatively is critical to prevent infections and promote healing. Patients should be instructed on gentle brushing and the use of antiseptic mouth rinses, such as chlorhexidine, to keep the surgical site clean. Non-compliance with oral hygiene instructions is a common issue, and follow-up phone calls can significantly improve adherence to these recommendations. Preoperative oral care by a dentist can also reduce the risk of postoperative complications, such as pneumonia, by preventing the aspiration of oral and pharyngeal secretions.
4. Follow-Up Appointment
Follow-up appointments are vital to monitor the healing process and address any complications that may arise. Regular follow-ups help in assessing pain levels, oral function, and overall recovery. Studies have shown that follow-up phone calls can enhance patient compliance with postoperative care instructions, leading to better outcomes. Additionally, follow-up visits allow healthcare providers to evaluate the recovery of sensitivity and function, ensuring that any temporary disturbances are resolved.
5. Lifestyle Changes
Post-operative lifestyle changes are necessary to ensure a smooth recovery. Patients should avoid strenuous physical activities and sun exposure during the convalescence period to prevent complications such as bleeding and edem. Smoking cessation is particularly important as it can significantly impact healing and increase the risk of complications. Educating patients about these lifestyle changes during preoperative consultations can help in planning and implementing effective postoperative care, ultimately favoring the rehabilitation process.
Benefits of Alveoplasty
Alveoplasty offers several advantages that enhance both dental function and aesthetics. By reshaping and smoothing the jawbone, this procedure ensures a better fit for dentures and other dental prosthetics, leading to increased comfort and oral health. Below are the key benefits of alveoplasty:
1. Improved Fit of Dentures
Alveoplasty, a surgical procedure to reshape the alveolar ridge, significantly enhances the fit of dentures. By smoothing and contouring the bone, it creates a more stable and retentive base for dentures, reducing the need for frequent adjustments and relines. This improved fit leads to better comfort and functionality for the patient, as the dentures are less likely to shift or cause irritation. Studies have shown that patients who undergo alveoplasty experience fewer issues with denture stability and retention compared to those who do not undergo the procedure.
2. Faster Healing Time
The procedure minimizes sharp bony edges and irregularities that can delay healing and cause discomfort. By providing a smoother surface, alveoplasty reduces the risk of complications such as infection and promotes quicker tissue regeneration. This expedited healing process allows for earlier denture placement and improved patient outcomes.
3. Reduced Risk of Bone Resorption
One of the significant benefits of alveoplasty is the reduction in the risk of bone resorption. By reshaping the alveolar ridge, the procedure helps maintain the bone’s structural integrity and prevents excessive resorption that typically follows tooth extraction. This preservation of bone volume is crucial for future dental implant placement and overall oral health. Studies have indicated that alveoplasty, combined with other bone preservation techniques, can significantly mitigate the loss of alveolar bone.
4. Improved Oral Functions
Alveoplasty enhances oral functions by providing a more stable and supportive foundation for dentures. This stability improves masticatory efficiency, allowing patients to chew and process food more effectively. Additionally, the procedure can enhance speech by ensuring that dentures fit snugly and do not move during talking. Improved oral functions contribute to better overall health and quality of life for patients, as they can maintain a more varied and nutritious diet.
5. Aesthetic Improvement
Aesthetic improvement is another key benefit of alveoplasty. By creating a more even and contoured alveolar ridge, the procedure enhances the appearance of the gums and the overall fit of the dentures. This results in a more natural and pleasing smile, boosting the patient’s confidence and self-esteem. The aesthetic benefits of alveoplasty are particularly important for patients who are concerned about the visual aspects of their dental prosthetics.
6. Facilitates Immediate Denture Placement
This immediate placement is beneficial for patients who require a quick transition from natural teeth to dentures, minimizing the period without teeth. The procedure ensures that the dentures fit well from the outset, reducing the need for subsequent adjustments and enhancing patient satisfaction with the immediate denture service.
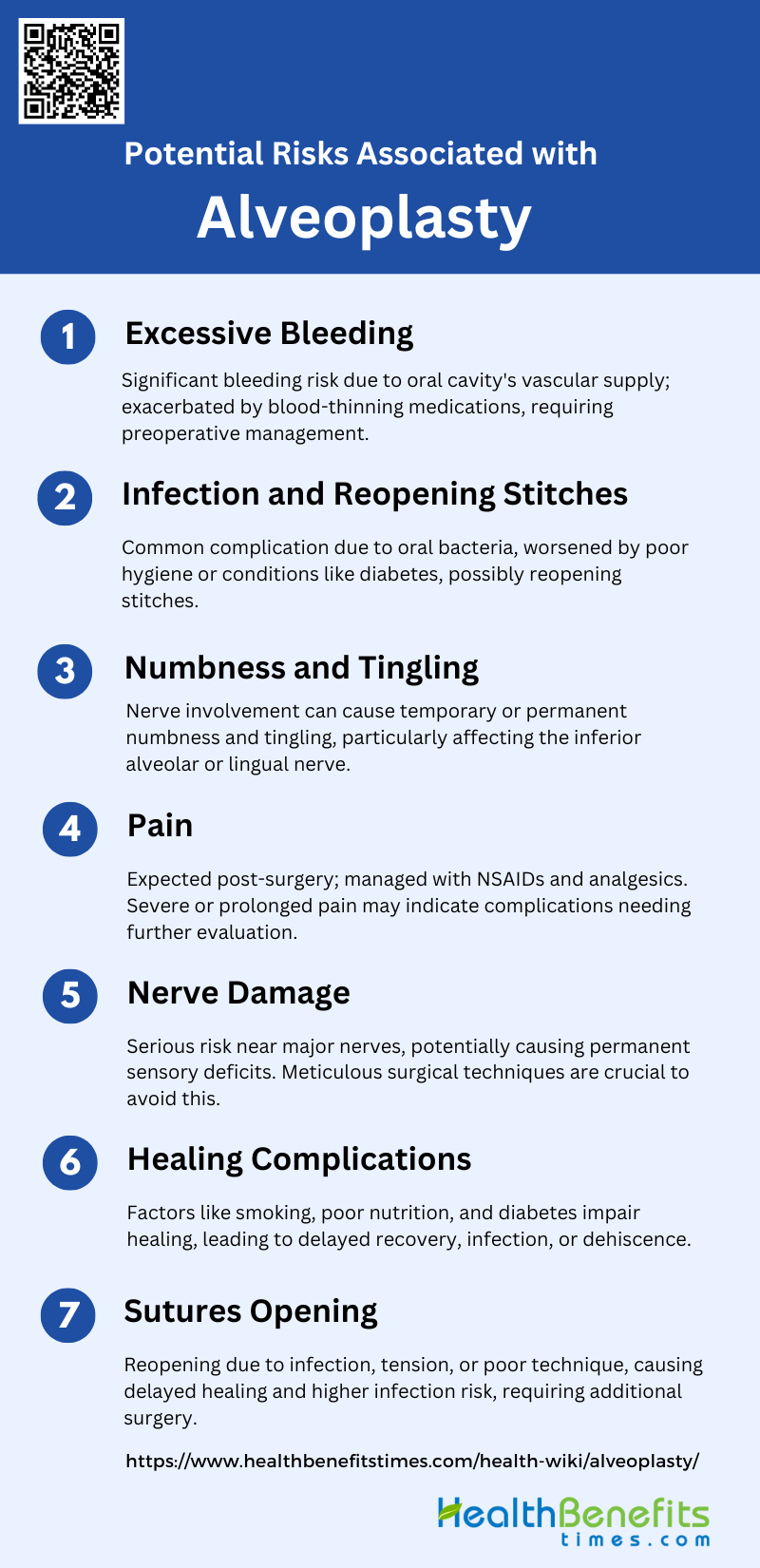
Potential risks associated with alveoplasty
While alveoplasty is generally a safe procedure, it is not without potential risks. Understanding these risks can help patients make informed decisions and take necessary precautions. Below are some of the potential risks associated with alveoplasty:
1. Excessive Bleeding
Excessive bleeding is a significant risk associated with alveoplasty. This can occur due to the rich vascular supply in the oral cavity and the invasive nature of the procedure. Patients on blood-thinning medications such as Warfarin, Aspirin, or Clopidogrel are particularly at risk, as these drugs can exacerbate bleeding tendencies. In some cases, excessive bleeding may necessitate a return to the operating room for further intervention. Proper preoperative assessment and management of anticoagulant therapy are crucial to minimize this risk.
2. Infection and Reopening Stitches
Infection is another common complication following alveoplasty. The oral cavity is naturally populated with bacteria, making it susceptible to postoperative infections. Factors such as poor oral hygiene, smoking, and systemic conditions like diabetes can increase the risk of infection. In severe cases, infection can lead to the reopening of stitches, requiring additional surgical intervention and prolonged antibiotic therapy. Ensuring sterile surgical techniques and providing postoperative care instructions are essential to mitigate this risk.
3. Numbness and Tingling
Numbness and tingling are potential complications due to nerve involvement during alveoplasty. The procedure can inadvertently affect the sensory nerves in the oral cavity, leading to temporary or, in rare cases, permanent numbness and tingling. This is particularly concerning if the inferior alveolar nerve or lingual nerve is involved. Patients should be informed about this risk preoperatively, and careful surgical techniques should be employed to avoid nerve damage.
4. Pain
Postoperative pain is an expected outcome of alveoplasty due to the invasive nature of the procedure. Pain management is crucial for patient comfort and recovery. Nonsteroidal anti-inflammatory drugs (NSAIDs) and other analgesics are commonly prescribed to manage pain. However, severe or prolonged pain may indicate complications such as infection or nerve damage, necessitating further evaluation and treatment. Effective pain management strategies and patient education on pain expectations are essential components of postoperative care.
5. Nerve Damage
Nerve damage is a serious risk associated with alveoplasty, particularly when the procedure involves areas close to major nerves. Damage to the inferior alveolar nerve or lingual nerve can result in permanent sensory deficits, including numbness, tingling, or even loss of function in the affected area. This can significantly impact the patient’s quality of life. Surgeons must employ meticulous techniques and have a thorough understanding of the anatomical landmarks to minimize the risk of nerve damage.
6. Healing Complications
Healing complications can arise from various factors, including patient-related issues such as smoking, poor nutrition, and systemic conditions like diabetes. These factors can impair the body’s natural healing processes, leading to delayed wound healing, infection, or dehiscence. Proper patient selection, preoperative optimization, and postoperative care are essential to promote effective healing and reduce the risk of complications. Monitoring the healing process and addressing any issues promptly can help ensure a successful recovery.
7. Sutures Opening
The reopening of sutures, or dehiscence, is a potential complication that can occur due to infection, excessive tension on the wound, or poor surgical technique. This can lead to delayed healing, increased risk of infection, and the need for additional surgical intervention. Ensuring proper suture techniques, minimizing tension on the wound, and providing clear postoperative care instructions can help prevent this complication. Regular follow-up appointments are crucial to monitor the wound and address any issues promptly.