 Alveolitis, also known as hypersensitivity pneumonitis or extrinsic allergic alveolitis, is an inflammatory condition affecting the alveoli, the tiny air sacs in the lungs. It is often triggered by repeated inhalation of organic antigens, leading to a hypersensitivity response in sensitized individuals. This condition is characterized by the accumulation of inflammatory and immune cells within the alveolar structures, which can cause various interstitial lung diseases. Alveolitis can present in acute or chronic forms, with symptoms ranging from dyspnea, cough, and fever to more severe respiratory issues and interstitial fibrosis if exposure continues. The inflammation and immune response in the alveoli can be influenced by genetic factors, such as polymorphisms in the interleukin-1 receptor antagonist and tumor necrosis factor-alpha genes, which have been associated with an increased risk of fibrosing alveolitis
Alveolitis, also known as hypersensitivity pneumonitis or extrinsic allergic alveolitis, is an inflammatory condition affecting the alveoli, the tiny air sacs in the lungs. It is often triggered by repeated inhalation of organic antigens, leading to a hypersensitivity response in sensitized individuals. This condition is characterized by the accumulation of inflammatory and immune cells within the alveolar structures, which can cause various interstitial lung diseases. Alveolitis can present in acute or chronic forms, with symptoms ranging from dyspnea, cough, and fever to more severe respiratory issues and interstitial fibrosis if exposure continues. The inflammation and immune response in the alveoli can be influenced by genetic factors, such as polymorphisms in the interleukin-1 receptor antagonist and tumor necrosis factor-alpha genes, which have been associated with an increased risk of fibrosing alveolitis
Causes of Alveolitis
Alveolitis can be triggered by various factors. These causes range from environmental exposures to underlying medical conditions. Understanding these causes is crucial for effective prevention and treatment.
1. Infection
Infections can lead to alveolitis, particularly when the alveoli are invaded by pathogens such as bacteria, viruses, or fungi. These infections can cause inflammation and damage to the alveolar walls, leading to symptoms such as cough, fever, and difficulty breathing. For instance, hypersensitivity pneumonitis (HP) can be triggered by inhalation of various microorganisms, including fungi and bacteria, which induce an immune response in the alveoli. The presence of these pathogens can result in acute or chronic inflammation, depending on the duration and intensity of exposure.
2. Environmental and Occupational Exposures
Environmental and occupational exposures are significant causes of alveolitis. Workers exposed to organic dusts, such as those in farming or poultry farming, can develop hypersensitivity pneumonitis due to inhalation of antigens from moldy hay, bird droppings, or other organic materials. These exposures lead to an immune response in the lungs, causing inflammation and fibrosis over time. Occupational exposure to solvents and other chemicals has also been linked to fibrosing alveolitis, suggesting that environmental factors play a crucial role in the disease’s pathogenesis.
3. Autoimmune Disorders
Autoimmune disorders can cause alveolitis when the body’s immune system mistakenly attacks its own lung tissue. Conditions such as systemic sclerosis and rheumatoid arthritis are known to be associated with interstitial lung diseases, including alveolitis. The immune response in these disorders leads to chronic inflammation and fibrosis of the alveolar walls, resulting in symptoms like chronic cough and dyspnea. The relationship between autoimmune diseases and alveolitis underscores the importance of understanding the underlying immune mechanisms involved.
4. Allergic Reactions
Allergic reactions, particularly hypersensitivity pneumonitis, are a common cause of alveolitis. This condition arises from repeated inhalation of organic antigens, such as bird proteins or mold spores, leading to an immune-mediated inflammatory response in the alveoli. Symptoms can range from acute episodes of fever, cough, and dyspnea to chronic forms characterized by progressive lung fibrosis. Avoiding exposure to the offending antigen is crucial in managing allergic alveolitis, and corticosteroids may be used in severe cases.
5. Chemical Exposure
Exposure to various chemicals, including solvents and isocyanates, can cause alveolitis. These chemicals can induce an inflammatory response in the alveoli, leading to conditions such as fibrosing alveolitis. Studies have shown that occupational exposure to solvents is associated with changes in lung tissue similar to those seen in fibrosing alveolitis, suggesting a potential link between chemical exposure and the disease. Preventing exposure to these harmful chemicals is essential in reducing the risk of developing alveolitis.
6. Radiation Therapy
Radiation therapy, particularly for cancers in the chest area, can lead to radiation-induced alveolitis. This condition occurs when the alveoli are damaged by radiation, resulting in inflammation and fibrosis. Patients undergoing radiation therapy for lung or breast cancer are at higher risk of developing this type of alveolitis. Symptoms typically include cough, dyspnea, and chest pain, and the condition can progress to chronic lung disease if not managed appropriately. Early detection and intervention are crucial in mitigating the effects of radiation-induced alveolitis.
7. Smoking
Cigarette smoking is a well-known cause of various lung diseases, including alveolitis. Smoking leads to chronic inflammation and damage to the alveolar macrophages, which are essential for maintaining lung homeostasis and immune defense. The dysregulation of alveolar macrophage function due to smoking can result in chronic lung inflammation, increased susceptibility to infections, and progression to chronic obstructive pulmonary disease (COPD) or other forms of interstitial lung disease. Smoking cessation is vital in preventing and managing smoking-related alveolitis.
8. Drug Reactions
Certain medications can cause drug-induced alveolitis as an adverse reaction. Drugs such as antibiotics, anti-inflammatory agents, and chemotherapeutic agents have been implicated in causing inflammation and damage to the alveoli. The mechanism often involves an immune-mediated response to the drug, leading to symptoms like cough, fever, and dyspnea. Identifying and discontinuing the offending drug is crucial in managing drug-induced alveolitis, and corticosteroids may be used to reduce inflammation in severe cases. Monitoring patients for respiratory symptoms during drug therapy is essential for early detection and intervention.
Types of Alveolitis
Alveolitis can be classified into several types based on its etiology and clinical presentation. Here are the main types of alveolitis:
1. Idiopathic Fibrosing Alveolitis
Idiopathic Fibrosing Alveolitis (IFA), also known as Idiopathic Pulmonary Fibrosis (IPF), is a progressive and usually fatal interstitial lung disease of unknown cause. It is characterized by sequential acute lung injury, scarring, and end-stage lung disease. The disease is marked by a histological pattern of usual interstitial pneumonia (UIP) on lung biopsy, which is associated with a poor prognosis and high mortality rate. The condition is often resistant to treatment, and survival rates are generally low, with a median survival of 3 to 6 years from the onset of symptoms.
2. Cryptogenic Fibrosing Alveolitis
Cryptogenic Fibrosing Alveolitis (CFA) is a subtype of idiopathic interstitial pneumonia with a similar clinical presentation to IFA. It can be subdivided into histopathologic patterns such as usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP), with UIP having a worse prognosis compared to NSIP. The presence of type III collagen in lung biopsies is associated with active disease and a better response to treatment. Additionally, Epstein-Barr virus (EBV) replication within pulmonary epithelial cells has been implicated as a potential contributing factor to CFA.
3. Alveolitis in SARS-CoV-2 Pneumonia
Alveolitis in SARS-CoV-2 pneumonia is characterized by severe inflammation and immune response within the alveolar structures. The condition is part of the broader spectrum of interstitial lung diseases (ILDs) and is marked by the accumulation of inflammatory and immune effector cells within the alveoli, leading to significant lung damage and fibrosis. The management of alveolitis in SARS-CoV-2 pneumonia remains challenging due to the progressive and often severe nature of the disease.
4. Sarcoidosis-Related Alveolitis
Sarcoidosis-related alveolitis is a form of interstitial lung disease where granulomas form in the lungs, leading to inflammation and fibrosis. This type of alveolitis is part of the broader category of interstitial lung diseases and is characterized by the accumulation of inflammatory cells within the alveolar structures. The disease can be progressive and may require long-term management to control symptoms and prevent further lung damage.
5. Interstitial Lung Diseases (ILD) Associated Alveolitis
Alveolitis associated with Interstitial Lung Diseases (ILDs) encompasses a wide range of conditions characterized by chronic inflammation and fibrosis of the lung interstitium. Common ILDs include those resulting from inhalation of inorganic or organic dusts, collagen-vascular disorders, and idiopathic pulmonary fibrosis. The concept of “alveolitis” has revolutionized the understanding and treatment of ILDs, highlighting the importance of early detection and management of inflammatory processes within the alveoli to prevent irreversible lung damage.
Symptoms of Alveolitis
Alveolitis, characterized by inflammation of the alveoli in the lungs, presents with a variety of symptoms that can range from mild to severe. Recognizing these symptoms early is essential for timely diagnosis and treatment. Below are the common symptoms associated with alveolitis:
1. Cough and Dyspnea: Patients with alveolitis often present with a persistent cough and shortness of breath (dyspnea). These symptoms are common across various forms of alveolitis, including extrinsic allergic alveolitis and fibrosing alveolitis.
2. Fever and Malaise: Fever and a general feeling of malaise or fatigue are frequently reported, especially in cases of hypersensitivity pneumonitis (a type of extrinsic allergic alveolitis). These symptoms typically appear a few hours after exposure to the offending antigen.
3. Weight Loss: Unintentional weight loss is another symptom observed in patients with alveolitis. This can be due to the chronic nature of the disease and the body’s ongoing inflammatory response.
4. Radiological Abnormalities: Radiological findings such as ground-glass opacities, nodular infiltrates, and fibrosis are common in alveolitis. High-resolution computed tomography (HRCT) scans often reveal these abnormalities, which correlate with the severity of the disease.
5. Pulmonary Function Impairment: Alveolitis often leads to impaired pulmonary function, characterized by restrictive lung disease. Pulmonary function tests (PFTs) typically show reduced lung volumes and decreased diffusion capacity, indicating compromised lung function.
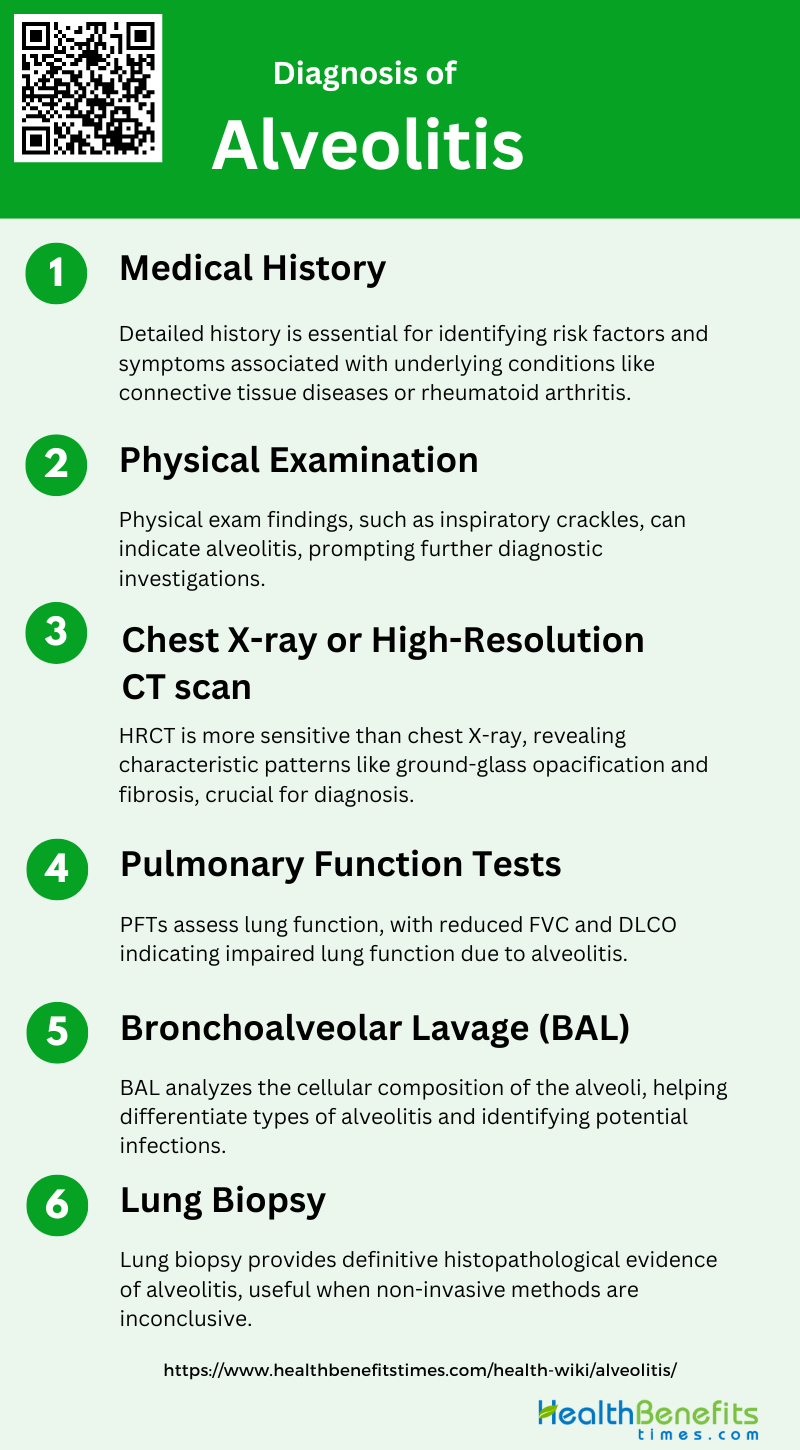
Diagnosis of Alveolitis
Diagnosing alveolitis involves a comprehensive evaluation of the patient’s medical history, symptoms, and clinical findings. Physicians typically employ a combination of diagnostic tests and imaging studies to confirm the presence and extent of the condition. The following steps outline the standard diagnostic approach:
1. Medical History
A thorough medical history is crucial in diagnosing alveolitis, particularly in patients with underlying conditions such as connective tissue diseases (CTDs) or rheumatoid arthritis (RA). Patients with CTDs often present with subclinical alveolitis, which can be detected even in the absence of symptoms. In RA, fibrosing alveolitis (FA) is a common complication, and a detailed history can help identify risk factors and symptoms associated with interstitial lung disease (ILD). Understanding the patient’s medical background, including any history of smoking, autoimmune diseases, or previous lung conditions, is essential for accurate diagnosis and management.
2. Physical Examination
Physical examination plays a pivotal role in the initial assessment of alveolitis. Key findings may include late inspiratory crackles, which are significantly associated with alveolitis in CTD patients. In patients with RA, bilateral basal chest crackles are often observed in those with HRCT evidence of fibrosing alveolitis. These physical signs, although not definitive, can prompt further diagnostic investigations and help in the early identification of alveolitis, guiding subsequent diagnostic and therapeutic steps.
3. Chest X-ray or High-Resolution CT scan
High-resolution computed tomography (HRCT) is superior to chest radiography in diagnosing alveolitis, offering higher sensitivity and specificity. HRCT can reveal characteristic patterns such as ground-glass opacification and fibrosis, which are indicative of alveolitis and ILD. In RA patients, HRCT is particularly useful, as it can detect fibrosing alveolitis even when chest radiographs are normal. The accuracy of HRCT in distinguishing fibrosing alveolitis from other diffuse lung diseases further reduces the need for invasive procedures like lung biopsy.
4. Pulmonary Function Tests
Pulmonary function tests (PFTs) are essential in evaluating the extent of lung involvement in alveolitis. Reduced forced vital capacity (FVC) and carbon monoxide diffusing capacity (DLCO) are common findings in patients with alveolitis, indicating impaired lung function. In CTD patients, a reduced FEV1 is specifically associated with granulocytic alveolitis. These tests not only help in diagnosing alveolitis but also in monitoring disease progression and response to treatment.
5. Bronchoalveolar Lavage (BAL)
Bronchoalveolar lavage (BAL) is a critical diagnostic tool for alveolitis, providing valuable information on the cellular composition of the alveolar space. BAL can differentiate between types of alveolitis, such as lymphocytic or granulocytic, which is crucial for determining the appropriate treatment. In systemic sclerosis, BAL findings correlate with disease severity and can predict pulmonary deterioration, making it an essential component of the diagnostic workup. Additionally, BAL can identify infections that may mimic or complicate alveolitis.
6. Lung Biopsy
Lung biopsy, although invasive, may be necessary when non-invasive methods are inconclusive. It provides definitive histopathological evidence of alveolitis and helps in differentiating it from other lung diseases. However, the superior diagnostic accuracy of HRCT and BAL often reduces the need for lung biopsy. In cases where HRCT and BAL results are ambiguous, a biopsy can confirm the diagnosis and guide targeted therapy, ensuring optimal patient management.
Treatment for Alveolitis
Treating alveolitis requires a multifaceted approach tailored to the severity and underlying cause of the condition. The primary goals are to reduce inflammation, manage symptoms, and prevent further lung damage. The following steps outline the standard treatment protocol:
1. Avoiding Triggers
Avoiding triggers is a fundamental strategy in managing alveolitis, particularly in cases of allergic alveolitis. This condition is often triggered by chronic inhalation of antigens, commonly found in occupational or home environments. Early diagnosis and prompt elimination of the offending antigen can lead to a good prognosis, with acute symptoms typically resolving within 24-48 hours after exposure cessation. In chronic cases, continuous exposure can lead to severe dyspnea and chronic cough, eventually progressing to pulmonary fibrosis and respiratory insufficiency. Therefore, identifying and avoiding these triggers is crucial for preventing disease progression and improving patient outcomes.
2. Medications
Medications play a critical role in the treatment of alveolitis. Corticosteroids, such as prednisolone, are commonly used to reduce inflammation and improve lung function. Mycophenolate mofetil (MMF) has shown promise as an effective and well-tolerated alternative to cyclophosphamide for treating scleroderma-associated alveolitis, improving pulmonary function and reducing symptoms. Additionally, high-dose N-acetylcysteine (NAC) has been found to enhance antioxidant defenses and improve pulmonary function in patients with fibrosing alveolitis. These medications, often used in combination, can help manage symptoms and slow disease progression.
3. Oxygen Therapy
Oxygen therapy is often employed in the management of alveolitis to alleviate hypoxia and improve the quality of life. Patients with severe pulmonary alveolar proteinosis, for instance, may benefit from inhaled recombinant human GM-CSF, which has been shown to improve arterial oxygen tension and reduce lung field density on CT scans. Oxygen therapy can be particularly beneficial for patients experiencing significant breathlessness and hypoxia, helping to maintain adequate oxygen levels in the blood and reduce the strain on the heart and lungs.
4. Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive intervention designed to improve the physical and emotional well-being of patients with chronic respiratory diseases, including alveolitis. This program typically includes exercise training, nutritional counseling, and education on managing the disease. Pulmonary rehabilitation has been shown to enhance exercise capacity, reduce symptoms, and improve the overall quality of life for patients with fibrosing alveolitis and other interstitial lung diseases. By addressing both physical and psychological aspects, pulmonary rehabilitation helps patients better cope with their condition and maintain a higher level of independence.
5. Environmental and Exposure Control
Environmental and exposure control is essential in managing alveolitis, particularly in cases triggered by occupational or environmental antigens. For example, patients with allergic alveolitis should avoid exposure to known allergens, such as moldy hay in farmer’s lung or bird droppings in bird fancier’s lung. Implementing measures such as improving ventilation, using protective equipment, and changing work or living environments can significantly reduce the risk of exposure and prevent disease exacerbation. Effective environmental control is a key component of a comprehensive management plan for alveolitis.
6. Lung Transplantation
Lung transplantation may be considered for patients with advanced alveolitis who do not respond to conventional treatments and experience severe, progressive respiratory failure. Although it is a complex and high-risk procedure, lung transplantation can offer a chance for prolonged survival and improved quality of life for selected patients. In cases of cryptogenic fibrosing alveolitis, for instance, even a modest increase in survival time can be crucial, providing patients with the opportunity to undergo transplantation and achieve better long-term outcomes. Careful patient selection and thorough pre-transplant evaluation are essential to optimize the success of this intervention.
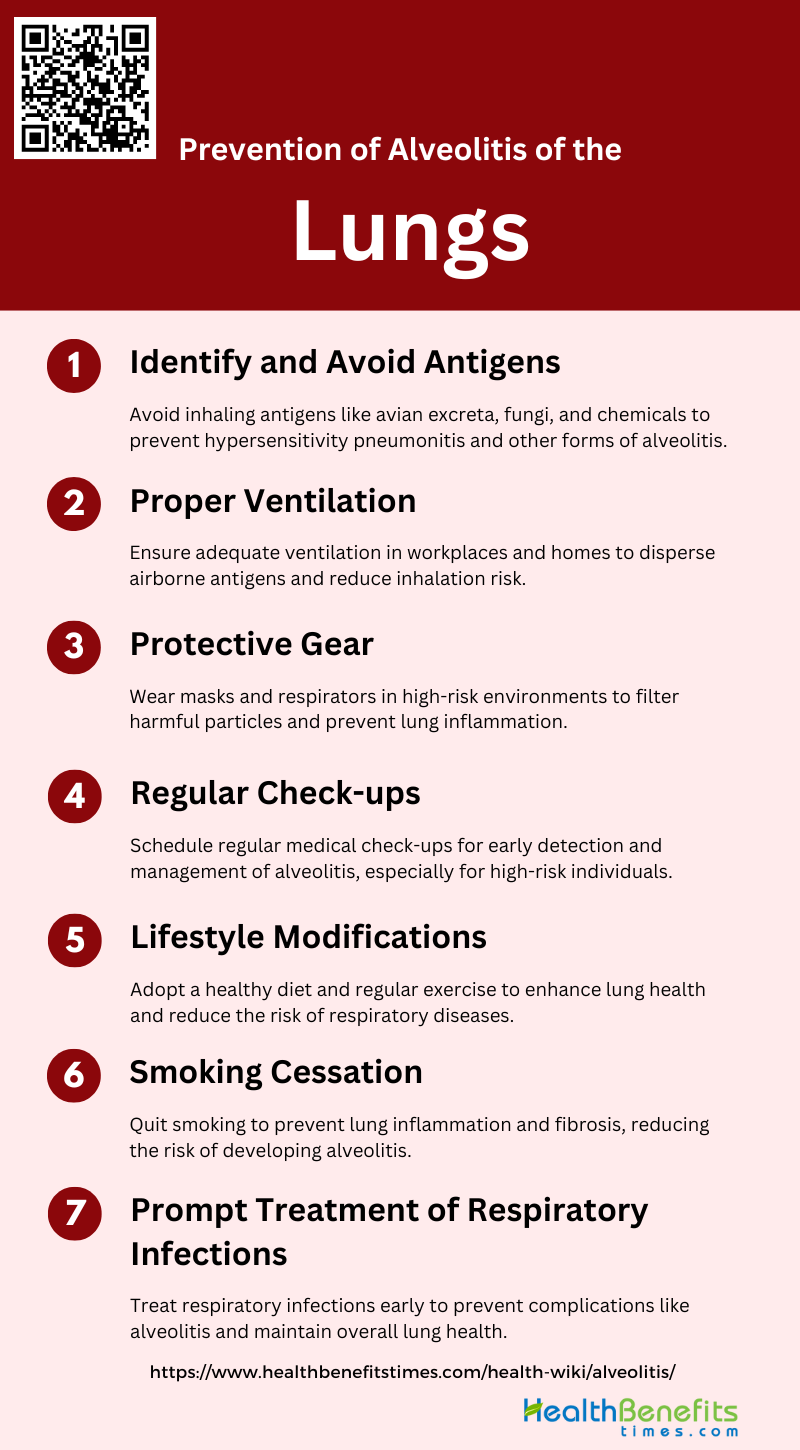
Prevention of Alveolitis of the Lungs
Preventing alveolitis involves minimizing exposure to known environmental and occupational irritants that can trigger lung inflammation. Implementing protective measures and lifestyle changes can significantly reduce the risk. The following steps outline effective prevention strategies:
1. Identify and Avoid Antigens
Identifying and avoiding antigens is crucial in preventing alveolitis of the lungs. Hypersensitivity pneumonitis, a type of alveolitis, is caused by inhalation of various antigens such as avian excreta, fungi, and reactive chemicals found in the workplace. Early diagnosis and avoidance of these antigens can prevent the progression of the disease. For instance, avoiding exposure to moldy hay or bird droppings can significantly reduce the risk of developing extrinsic allergic alveolitis. Therefore, understanding and mitigating exposure to specific antigens is a primary preventive measure.
2. Proper Ventilation
Proper ventilation is essential in reducing the risk of alveolitis by minimizing the concentration of airborne antigens. In environments where exposure to antigens is inevitable, such as farms or workplaces with reactive chemicals, ensuring adequate ventilation can help disperse these particles and reduce inhalation. Effective ventilation systems can prevent the accumulation of harmful substances, thereby lowering the incidence of hypersensitivity pneumonitis and other forms of alveolitis. This is particularly important in occupational settings where continuous exposure to antigens is a risk factor.
3. Protective Gear
Wearing protective gear, such as masks and respirators, is an effective strategy to prevent alveolitis, especially in high-risk environments. Protective equipment can filter out harmful particles and antigens, reducing the likelihood of inhalation and subsequent lung inflammation. For example, farmers exposed to moldy hay or bird handlers can benefit significantly from using respirators to prevent extrinsic allergic alveolitis. Consistent use of protective gear is a practical approach to safeguard against occupational lung diseases.
4. Regular Check-ups
Regular medical check-ups are vital for early detection and management of alveolitis. Routine monitoring can help identify early signs of lung inflammation and facilitate prompt intervention. For individuals at high risk, such as those with occupational exposure to antigens, periodic lung function tests and imaging studies can detect changes indicative of alveolitis before severe damage occurs. Early diagnosis through regular check-ups can lead to timely treatment and better outcomes.
5. Lifestyle Modifications
Lifestyle modifications, including maintaining a healthy diet and regular exercise, can enhance overall lung health and reduce the risk of alveolitis. A balanced diet rich in antioxidants and anti-inflammatory foods can support immune function and reduce inflammation. Regular physical activity can improve lung capacity and resilience against respiratory diseases. Additionally, avoiding exposure to known environmental triggers and pollutants can further protect lung health. These lifestyle changes contribute to a holistic approach to preventing alveolitis.
6. Smoking Cessation
Smoking cessation is critical in preventing alveolitis and other lung diseases. Cigarette smoke has been shown to impair alveolar macrophage function, leading to chronic lung disease and increased susceptibility to infections. Studies have demonstrated that exposure to cigarette smoke exacerbates lung inflammation and fibrosis, worsening conditions like allergic alveolitis. Quitting smoking can significantly reduce the risk of developing alveolitis and improve overall lung health, making it a key preventive measure.
7. Prompt Treatment of Respiratory Infections
Prompt treatment of respiratory infections is essential to prevent complications such as alveolitis. Infections can trigger or exacerbate lung inflammation, leading to conditions like eosinophilic alveolitis. Early and effective treatment of infections can prevent the progression to chronic lung diseases. For instance, managing viral infections promptly can reduce the risk of developing cryptogenic fibrosing alveolitis, which has been associated with viral triggers like Epstein-Barr virus. Timely medical intervention for respiratory infections is crucial in preventing alveolitis and maintaining lung health.