Alveoli are the tiny air sacs located at the end of the respiratory tree in the lungs. They are the site of gas exchange, where oxygen is taken up into the bloodstream and carbon dioxide is removed. Each alveolus is surrounded by a dense network of capillaries, allowing for efficient diffusion of gases across the thin alveolar-capillary membrane. The walls of the alveoli are composed of type I and type II alveolar cells, with type II cells producing surfactant that reduces surface tension and prevents the alveoli from collapsing during exhalation. Alveoli have a large surface area to facilitate gas exchange, with estimates ranging from 70-145 square meters in the human lung. Their structural integrity and proper functioning are crucial for maintaining adequate oxygenation and preventing respiratory disorders.
Anatomy of Alveoli
Structurally, alveoli are composed of a thin layer of remodeled haversian bone forming the socket, and cancellous bone filling the space between the socket and the jaw elements, collectively known as the arcus alveolaris. The alveolar lining layer, which includes surfactant and its aqueous subphase, is thin and continuous, averaging 0.2 microns in thickness, and serves to smooth the alveolar air-liquid interface. This lining layer submerges epithelial cell microvilli and intercellular junctional ridges, varying from a few nanometers to several micrometers in thickness. The alveoli also act as an anchoring attachment for the periodontal ligament and support the dentition, playing a role in tooth formation by mechanically constraining the developing crown, which influences the complexity of mammalian heterodonty.
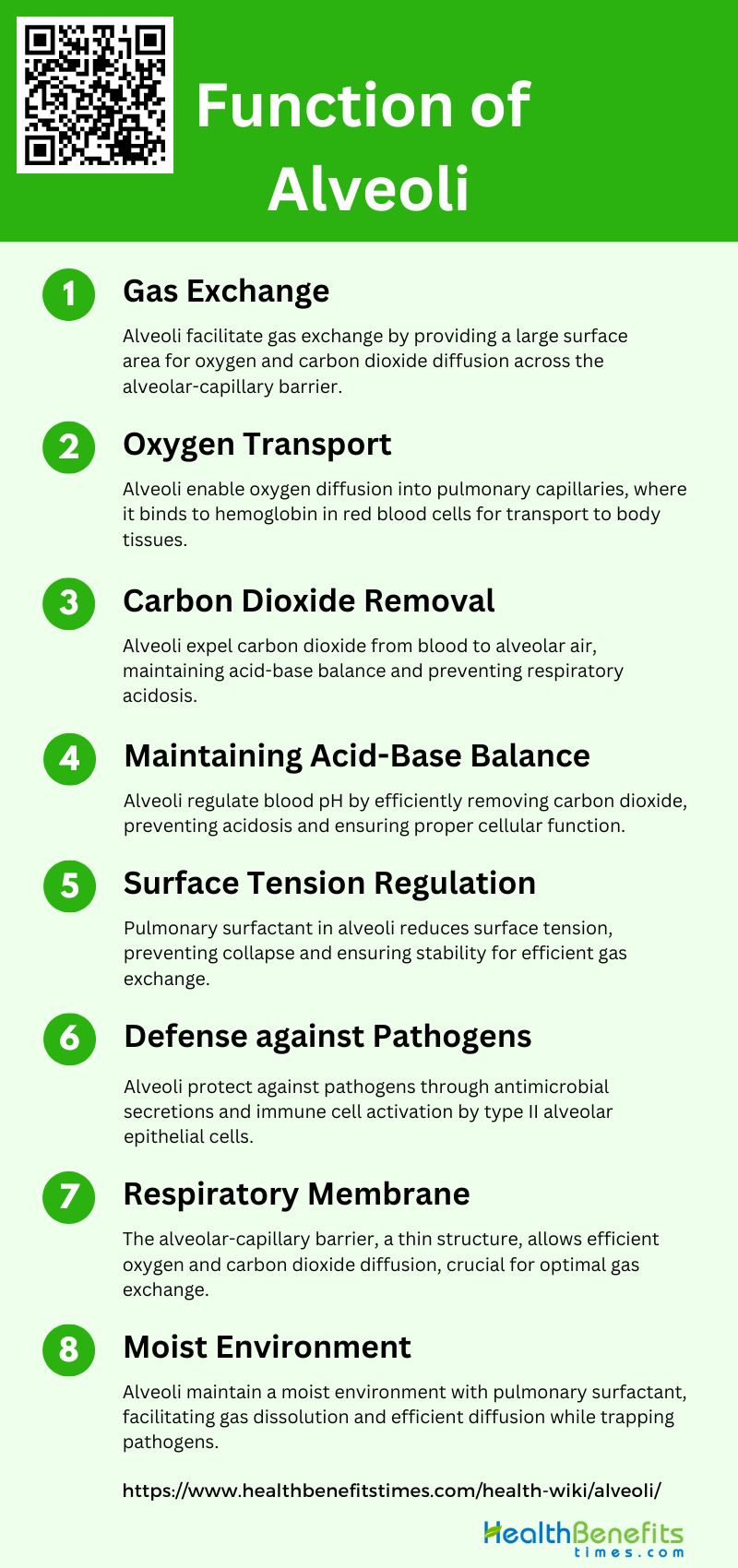
Function of Alveoli
The alveoli are tiny air sacs located in the lungs, and they play a crucial role in the respiratory system. Their primary function is to facilitate the exchange of gases between the air and the blood. Here are the key functions of alveoli:
1. Gas Exchange
The primary function of alveoli is gas exchange, which occurs through passive diffusion across the alveolar-capillary barrier. The alveoli provide a vast surface area, approximately 75 m² in humans, for the exchange of oxygen and carbon dioxide between the air and blood. This process involves a thin-walled continuous capillary, a dual basal lamina synthesized by endothelial and type I alveolar epithelial cells, and thin cytoplasmic extensions of type I alveolar epithelial cells. The efficient gas exchange is facilitated by the specialized structure of the alveolar septum, which ensures minimal diffusion distance and maximal surface area for gas transfer.
2. Oxygen Transport
Oxygen transport in the alveoli involves the diffusion of oxygen from the alveolar air into the blood within the pulmonary capillaries. The type I alveolar epithelial cells, which cover about 90% of the alveolar surface, play a crucial role in this process by providing a thin barrier for oxygen to diffuse through. The oxygen then binds to hemoglobin in red blood cells, which transport it to tissues throughout the body. The structural design of the alveoli, including the extensive capillary network and the thin alveolar walls, is optimized to facilitate efficient oxygen uptake and transport.
3. Carbon Dioxide Removal
The removal of carbon dioxide (CO₂) from the blood is another critical function of the alveoli. CO₂ diffuses from the blood into the alveolar air, where it is expelled from the body during exhalation. This process is facilitated by the same structural features that aid in oxygen transport, including the thin alveolar-capillary barrier and the extensive surface area provided by the alveoli. Efficient CO₂ removal is essential for maintaining the acid-base balance in the body and preventing respiratory acidosis.
4. Maintaining Acid-Base Balance
The alveoli play a vital role in maintaining the body’s acid-base balance by regulating the levels of CO₂ in the blood. By efficiently removing CO₂, a byproduct of cellular metabolism, the alveoli help to prevent the accumulation of carbonic acid in the blood, which can lead to acidosis. The balance between oxygen uptake and CO₂ removal is crucial for maintaining the pH of the blood within a narrow range, ensuring proper cellular function and metabolic processes.
5. Surface Tension Regulation
The regulation of surface tension within the alveoli is primarily managed by pulmonary surfactant, a complex mixture of lipids and proteins secreted by type II alveolar epithelial cells. Surfactant reduces the surface tension at the air-liquid interface, preventing alveolar collapse during exhalation and ensuring alveolar stability. This biophysical function of surfactant is essential for maintaining the structural integrity of the alveoli and facilitating efficient gas exchange. Additionally, surfactant has immunomodulatory properties that contribute to alveolar homeostasis and defense against pathogens.
6. Defense against Pathogens
The alveoli are equipped with several defense mechanisms to protect against inhaled pathogens. Type II alveolar epithelial cells secrete antimicrobial factors, cytokines, and chemokines that activate and modulate the activity of immune cells, such as alveolar macrophages. These immune cells play a crucial role in phagocytosing pathogens and apoptotic cells, as well as modulating inflammatory responses. The coordinated action of alveolar epithelial cells and macrophages is essential for maintaining lung homeostasis and preventing infections.
7. Respiratory Membrane
The respiratory membrane, also known as the alveolar-capillary barrier, is a thin structure that facilitates gas exchange between the alveolar air and the blood. It consists of the alveolar epithelium, the interstitial space, and the capillary endothelium. The thinness of this membrane, combined with the extensive surface area of the alveoli, allows for efficient diffusion of oxygen and CO₂. The integrity of the respiratory membrane is crucial for optimal gas exchange and is maintained by the structural and functional properties of the alveolar epithelial cells.
8. Moist Environment
The alveoli are lined with a thin layer of fluid that maintains a moist environment, essential for efficient gas exchange. This liquid lining is regulated by pulmonary surfactant, which reduces surface tension and prevents the alveoli from drying out. The moist environment facilitates the dissolution of gases, allowing for their efficient diffusion across the alveolar-capillary barrier. Additionally, the fluid layer helps to trap and clear inhaled particles and pathogens, contributing to the overall defense mechanisms of the respiratory system.
Common Causes Damage to the Alveoli
Damage to the alveoli, the tiny air sacs in the lungs, can result from various factors that impair respiratory function. Understanding these causes is crucial for preventing and managing respiratory diseases. Here are some common causes of alveolar damage:
1. Mechanical Ventilation
Mechanical ventilation while lifesaving, can cause significant damage to the alveoli, a condition known as ventilator-induced lung injury (VILI). High inflation pressures and low positive end-expiratory pressure (PEEP) can lead to alveolar instability and mechanical stress, resulting in alveolar over distension and repetitive opening and closing of alveoli. This mechanical stress can cause structural damage, inflammation, and surfactant dysfunction, ultimately leading to lung injury 5. Studies have shown that even in the absence of pre-existing lung conditions, prolonged mechanical ventilation can induce apoptosis, inhibit alveolar septation, and impair angiogenesis, contributing to chronic lung disease.
2. Surfactant Dysfunction
Surfactant dysfunction is a critical factor in the pathogenesis of various lung injuries, including acute respiratory distress syndrome (ARDS) and idiopathic pulmonary fibrosis (IPF). Surfactant inactivation leads to alveolar collapse (derecruitment) and collapse induration, which are associated with decreased lung compliance and increased mechanical stress on alveolar walls. The degradation of the alveolar epithelial glycocalyx, a layer of glycosaminoglycans, has been implicated in surfactant dysfunction, contributing to microatelectasis and decreased lung compliance in ARDS patients. Additionally, surfactant dysfunction can result from mechanical ventilation, which alters the distribution and activity of surfactant phospholipid aggregates, exacerbating lung injury.
3. Exposure to Harmful Substances
Exposure to harmful substances such as high concentrations of oxygen (hyperoxia), pollutants, and toxic chemicals can cause diffuse alveolar damage. Hyperoxia, often used in mechanical ventilation, can induce oxidative stress, leading to the upregulation of pro-fibrotic genes and down regulation of surfactant proteins, resulting in alveolar dysfunction and fibrosing alveolitis. In neonatal chronic lung disease, prolonged exposure to oxygen and mechanical ventilation can impair lung development, causing defective alveolar septation and angiogenesis. Additionally, exposure to harmful substances can trigger inflammatory responses, leading to alveolar inflammation and damage.
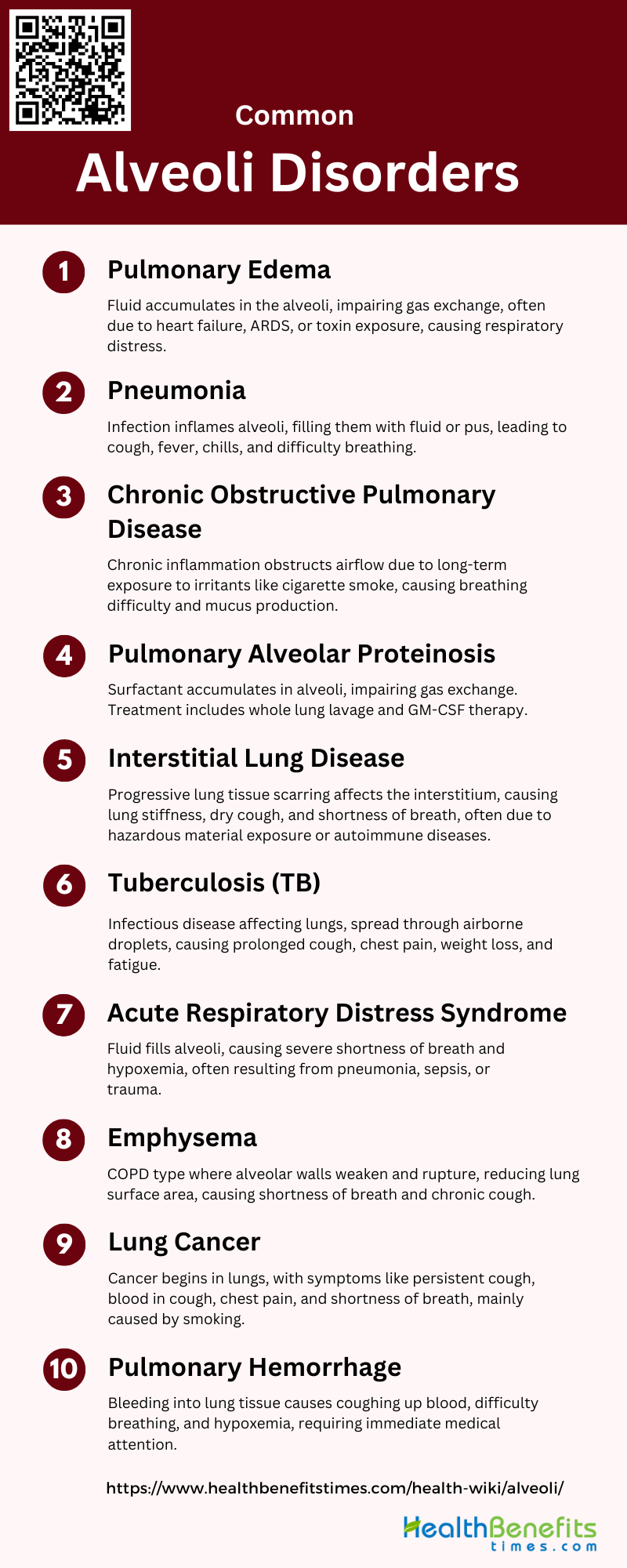
Common Alveoli Disorders
Alveoli are tiny air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place. Various disorders can affect the alveoli, leading to respiratory issues and compromised lung function. Below is a list of common alveoli disorders:
1. Pulmonary Edema
Pulmonary edema is a condition characterized by the accumulation of fluid in the alveoli, leading to impaired gas exchange and respiratory distress. This condition can result from various causes, including heart failure, acute respiratory distress syndrome (ARDS), and exposure to toxins. The fluid buildup in the alveoli prevents oxygen from being absorbed into the bloodstream, causing symptoms such as shortness of breath, coughing, and chest pain. Treatment typically involves addressing the underlying cause, using diuretics to remove excess fluid, and providing oxygen therapy to improve oxygenation.
2. Pneumonia
Pneumonia is an infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus. This condition can be caused by bacteria, viruses, or fungi. Symptoms include cough with phlegm or pus, fever, chills, and difficulty breathing. Pneumonia can range in seriousness from mild to life-threatening, and it is particularly dangerous for infants, young children, and the elderly. Treatment depends on the cause of pneumonia and may include antibiotics, antiviral medications, or antifungal treatments, along with supportive care such as rest and fluids.
3. Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. It is primarily caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. COPD includes conditions such as emphysema and chronic bronchitis. Symptoms include breathing difficulty, cough, mucus (sputum) production, and wheezing. COPD is a progressive disease that can lead to severe disability and is associated with an increased risk of developing heart disease, lung cancer, and other conditions. Management includes smoking cessation, bronchodilators, steroids, and pulmonary rehabilitation.
4. Pulmonary Alveolar Proteinosis (PAP)
Pulmonary Alveolar Proteinosis (PAP) is a rare lung disease characterized by the accumulation of surfactant in the alveoli, leading to impaired gas exchange and respiratory distress. The condition can be idiopathic, autoimmune, or secondary to other diseases. The most effective treatment is whole lung lavage, which involves washing out the surfactant material from the lungs. Recent advances have identified the role of granulocyte-macrophage colony-stimulating factor (GM-CSF) in the pathogenesis of PAP, leading to new therapeutic approaches such as GM-CSF therapy and rituximab.
5. Interstitial Lung Disease
Interstitial Lung Disease (ILD) encompasses a large group of disorders characterized by progressive scarring of lung tissue, which affects the interstitium, the tissue and space around the air sacs of the lungs. This scarring leads to stiffness in the lungs, making it difficult to breathe and get oxygen into the bloodstream. Causes of ILD include long-term exposure to hazardous materials, autoimmune diseases, and certain medications. Symptoms include a dry cough and shortness of breath. Diagnosis and management are challenging due to the heterogeneity of the diseases, but early detection and treatment are crucial to slow disease progression.
6. Tuberculosis
Tuberculosis (TB) is a potentially serious infectious disease that mainly affects the lungs. The bacteria that cause TB are spread from person to person through tiny droplets released into the air via coughs and sneezes. Symptoms of active TB include coughing that lasts three or more weeks, coughing up blood, chest pain, unintentional weight loss, fatigue, fever, night sweats, and chills. TB can be treated with a course of antibiotics over six to nine months. The disease can be fatal if not treated properly, and drug-resistant strains of TB are a growing concern.
7. Acute Respiratory Distress Syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition that occurs when fluid fills up the alveoli in the lungs. This fluid prevents the lungs from filling with enough air, leading to severe shortness of breath and hypoxemia. ARDS can result from various causes, including pneumonia, sepsis, trauma, and inhalation of harmful substances. Treatment typically involves mechanical ventilation to support breathing and addressing the underlying cause. Despite advances in treatment, ARDS has a high mortality rate and can lead to long-term lung damage.
8. Emphysema
Emphysema is a type of COPD that involves damage to the alveoli (air sacs) in the lungs. Over time, the inner walls of the alveoli weaken and rupture, creating larger air spaces instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches the bloodstream. Emphysema is most often caused by long-term exposure to airborne irritants, including tobacco smoke, air pollution, chemical fumes, and dust. Symptoms include shortness of breath, a chronic cough, and difficulty breathing during physical activities. There is no cure, but treatments can help relieve symptoms and slow the progression of the disease.
9. Lung Cancer
Lung cancer is a type of cancer that begins in the lungs. The two main types are small cell lung cancer and non-small cell lung cancer. Smoking is the leading cause of lung cancer, but it can also occur in people who have never smoked. Symptoms include a persistent cough, coughing up blood, chest pain, hoarseness, weight loss, and shortness of breath. Treatment options depend on the type and stage of cancer and may include surgery, radiation therapy, chemotherapy, targeted drug therapy, and immunotherapy. Early detection is crucial for improving survival rates.
10. Pulmonary Hemorrhage
Pulmonary hemorrhage is a condition characterized by bleeding into the lung tissue, which can lead to coughing up blood, difficulty breathing, and hypoxemia. Causes of pulmonary hemorrhage include trauma, infections, autoimmune diseases, and certain medications. The condition can be life-threatening and requires immediate medical attention. Treatment involves stabilizing the patient, stopping the bleeding, and addressing the underlying cause. In severe cases, mechanical ventilation and blood transfusions may be necessary. Pulmonary hemorrhage can lead to significant morbidity and mortality if not promptly and effectively managed.
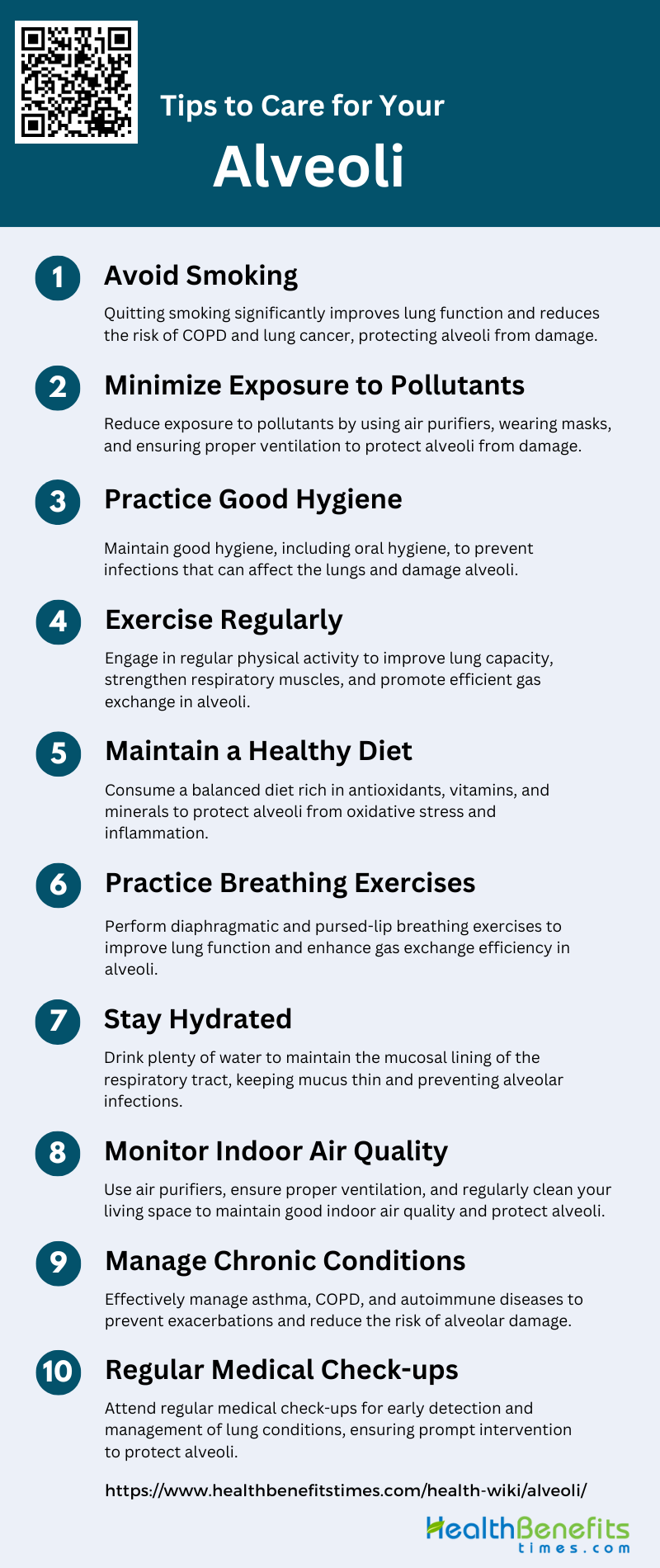
Tips to care alveoli
Maintaining healthy alveoli is crucial for optimal lung function and overall respiratory health. Simple lifestyle changes and proactive measures can significantly improve the condition of your alveoli. Below are some essential tips to care for your alveoli:
1. Avoid Smoking
Smoking is a major risk factor for various lung diseases, including chronic obstructive pulmonary disease (COPD) and lung cancer. It causes inflammation and damage to the alveoli, the tiny air sacs in the lungs where gas exchange occurs. Studies have shown that smoking cessation can significantly improve lung function and reduce the risk of developing severe respiratory conditions. By avoiding smoking, you can protect your alveoli from the harmful effects of tobacco smoke and maintain better overall lung health.
2. Minimize Exposure to Pollutants
Exposure to environmental pollutants, such as industrial emissions, vehicle exhaust, and indoor pollutants, can lead to respiratory issues and damage the alveoli. Research indicates that minimizing exposure to these pollutants can help maintain lung health and prevent conditions like fibrosing alveolitis. Using air purifiers, wearing masks in polluted areas, and ensuring proper ventilation indoors are effective strategies to reduce pollutant exposure and protect your alveoli.
3. Practice Good Hygiene
Maintaining good hygiene, especially oral hygiene, can prevent infections that may affect the lungs. A study found that proper plaque control significantly reduced the incidence of alveolitis sicca dolorosa, a painful condition affecting the alveoli. Regular handwashing, avoiding close contact with sick individuals, and keeping your living environment clean can also help prevent respiratory infections and protect your alveoli.
4. Exercise Regularly
Regular physical activity is beneficial for lung health as it improves lung capacity and promotes efficient gas exchange in the alveoli. Exercise increases the strength and endurance of respiratory muscles, enhancing overall lung function. Studies have shown that physical activity can help in the recruitment of collapsed alveoli, improving gas exchange and arterial oxygenation. Incorporating aerobic exercises like walking, running, and swimming into your routine can significantly benefit your alveoli.
5. Maintain a Healthy Diet
A balanced diet rich in antioxidants, vitamins, and minerals supports overall lung health and helps protect the alveoli from oxidative stress and inflammation. Nutrients such as vitamin C, vitamin E, and omega-3 fatty acids have been shown to have protective effects on lung tissue. A healthy diet can also support the immune system, reducing the risk of infections that can damage the alveoli. Including a variety of fruits, vegetables, whole grains, and lean proteins in your diet is essential for maintaining healthy alveoli.
6. Practice Breathing Exercises
Breathing exercises, such as diaphragmatic breathing and pursed-lip breathing, can improve lung function and enhance the efficiency of gas exchange in the alveoli. These exercises help in maintaining lung compliance and reducing atelectasis, which is the collapse of alveoli. Regular practice of breathing exercises can strengthen respiratory muscles, increase lung capacity, and improve overall respiratory health.
7. Stay Hydrated
Adequate hydration is crucial for maintaining the mucosal lining of the respiratory tract, which helps in trapping and expelling pollutants and pathogens. Staying hydrated ensures that the mucus in the lungs remains thin and can be easily cleared, preventing infections and inflammation in the alveoli. Drinking plenty of water and consuming fluids like herbal teas and soups can help keep your respiratory system hydrated and functioning optimally.
8. Monitor Indoor Air Quality
Indoor air quality can significantly impact lung health. Poor indoor air quality, due to factors like mold, dust, and chemical pollutants, can lead to respiratory issues and damage the alveoli. Using air purifiers, maintaining proper ventilation, and regularly cleaning your living space can help improve indoor air quality. Monitoring and controlling indoor air pollutants can prevent respiratory conditions and protect your alveoli from damage.
9. Manage Chronic Conditions
Managing chronic conditions such as asthma, COPD, and autoimmune diseases is essential for protecting the alveoli. Effective management of these conditions can prevent exacerbations and reduce the risk of complications that can damage the alveoli. Treatments like inhalers, medications, and lifestyle modifications can help control symptoms and maintain lung health. Regular follow-ups with healthcare providers are crucial for managing chronic conditions effectively.
10. Regular Medical Check-ups
Regular medical check-ups are important for early detection and management of lung conditions that can affect the alveoli. Routine screenings and pulmonary function tests can help identify issues before they become severe. Early intervention and appropriate treatment can prevent further damage to the alveoli and improve overall lung health. Consulting with healthcare professionals regularly ensures that any potential problems are addressed promptly.