Alveolectomy is a surgical procedure involving the removal of a portion of the alveolar bone, which is the part of the jawbone that contains the tooth sockets. This procedure is typically performed to facilitate the extraction of teeth, particularly when dealing with impacted or diseased teeth, and to ensure proper healing and preparation of the jaw for future dental prosthetics, such as dentures or implants. Alveolectomy can be executed using various techniques, including distolingual alveolectomy and external alveolectomy, each tailored to specific clinical needs and anatomical considerations. The procedure aims to smooth and reshape the alveolar ridge, thereby improving the fit and function of dental prosthetics and enhancing overall oral health outcomes.
Purpose of Alveolectomy
An alveolectomy is a surgical procedure that involves the removal of a portion of the alveolar ridge, which is the bone that supports the teeth. The purposes of an alveolectomy include:
1. Preparation for Dentures
This procedure ensures that the denture fits more comfortably and securely, reducing the risk of irritation and improving the overall aesthetic outcome. Alveolectomy can be particularly beneficial in cases where multiple teeth have been extracted, as it helps to eliminate sharp bony edges and undercuts that could interfere with the fit of the denture. This surgical intervention is crucial for enhancing the denture-bearing areas of the intraoral cavity, ultimately leading to better patient satisfaction and comfort.
2. Treatment of Dental Issues
Alveolectomy is also employed in the treatment of various dental issues, such as the prevention of radionecrosis in patients undergoing radiotherapy for oral cancer. By removing diseased teeth and performing alveolectomy to eliminate sharp interdental septa, the risk of infection and subsequent necrosis of the irradiated gingivae and jawbone is significantly reduced. This procedure is essential in managing the condition of the teeth and surrounding bone before, during, and after radiation therapy, thereby minimizing severe complications associated with osteoradionecrosis.
3. Extraction Site Management
Managing extraction sites is another critical purpose of alveolectomy. After tooth extraction, the alveolar ridge can undergo significant changes, including bone resorption and the formation of sharp bony edges. Alveolectomy helps in reshaping the alveolar ridge to create a more favorable environment for healing and future dental procedures, such as implant placement. This surgical intervention can also prevent complications like delayed healing and soft tissue irritation, ensuring a smoother recovery process and better long-term outcomes for the patient.
4. Orthodontic Reasons
In orthodontics, alveolectomy can be used to facilitate tooth movement and improve the overall alignment of the teeth. For instance, alveolar corticotomy, a form of alveolectomy, has been shown to accelerate orthodontic tooth movement, particularly in the retraction of upper canines. This procedure can significantly reduce the time required for orthodontic treatment while also addressing issues related to pain and discomfort during the process. By modifying the alveolar bone, orthodontists can achieve more efficient and effective tooth movement, leading to better treatment outcomes.
5. Support for Implants
Before implant placement, the alveolar ridge may need to be augmented and reshaped to provide a solid bony base for the implant. This preparation is crucial for the long-term success of the implant, as it enhances the stability and integration of the implant with the surrounding bone. By preserving and optimizing the alveolar ridge, alveolectomy helps in achieving better prosthodontic and aesthetic outcomes, ultimately leading to improved patient satisfaction.
Steps involved in an Alveolectomy
The main steps involved in an alveolectomy include:
1. Pre-Surgical Assessment
The pre-surgical assessment is a critical step in the alveolectomy process. It involves a thorough evaluation of the patient’s medical history, dental condition, and specific needs. Diagnostic tools such as X-rays and CT scans are used to assess the alveolar bone structure and identify any potential complications. This step ensures that the surgical plan is tailored to the patient’s unique anatomy and health status, minimizing risks and optimizing outcomes.
2. Anesthesia
Anesthesia is administered to ensure the patient remains pain-free and comfortable during the procedure. Local anesthesia, such as Novocain nerve-block, is commonly used to numb the surgical area. In some cases, general anesthesia may be employed, especially if the patient is anxious or if the procedure is expected to be extensive. The choice of anesthesia depends on the patient’s medical history, the complexity of the surgery, and the surgeon’s preference.
3. Incision
The incision phase involves making precise cuts in the gum tissue to expose the alveolar bone. The muco-periosteum is reflected to provide clear access to the bone structure. This step requires meticulous technique to avoid damaging surrounding tissues and to ensure a clean surgical field. Proper incision techniques are crucial for minimizing postoperative inflammation and promoting faster healing.
4. Removal of Alveolar Bone
The removal of the alveolar bone is the core of the alveolectomy procedure. Techniques such as intraseptal alveolectomy or labial alveolectomy are employed depending on the specific case . The bone is carefully removed to achieve the desired contour and to facilitate subsequent dental procedures. This step must be performed with precision to avoid excessive bone loss and to maintain the structural integrity of the jaw.
5. Smoothing and Reshaping
After the removal of the alveolar bone, the remaining bone edges are smoothed and reshaped to create a uniform and stable ridge. This step is essential for ensuring that the bone heals properly and that the final dental prosthesis fits well. Smoothing and reshaping also help in reducing postoperative discomfort and preventing complications such as sharp bone edges causing irritation.
6. Irrigation
Irrigation involves thoroughly cleaning the surgical site with a sterile saline solution to remove bone debris and blood. This step helps in reducing the risk of infection and promotes a clean healing environment. Proper irrigation is crucial for minimizing postoperative complications and ensuring that the surgical area remains free from contaminants.
7. Closure
The closure phase involves suturing the gum tissue back into place over the surgical site. The sutures help in stabilizing the tissue and protecting the underlying bone as it heals. Different suturing techniques and materials may be used depending on the specific requirements of the surgery. Proper closure is vital for promoting optimal healing and reducing the risk of postoperative complications.
8. Postoperative Care
Postoperative care is essential for ensuring a smooth recovery and minimizing complications. Patients are typically advised on pain management, oral hygiene practices, and dietary restrictions to support healing. Follow-up appointments are scheduled to monitor the healing process and to address any issues that may arise. Effective postoperative care is crucial for achieving the best possible outcomes.
9. Follow-Up
Follow-up visits are scheduled to assess the healing progress and to ensure that there are no complications such as infection or excessive bone resorption. These visits allow the surgeon to make any necessary adjustments to the treatment plan and to provide additional care as needed. Regular follow-up is important for maintaining oral health and for the long-term success of the alveolectomy procedure.
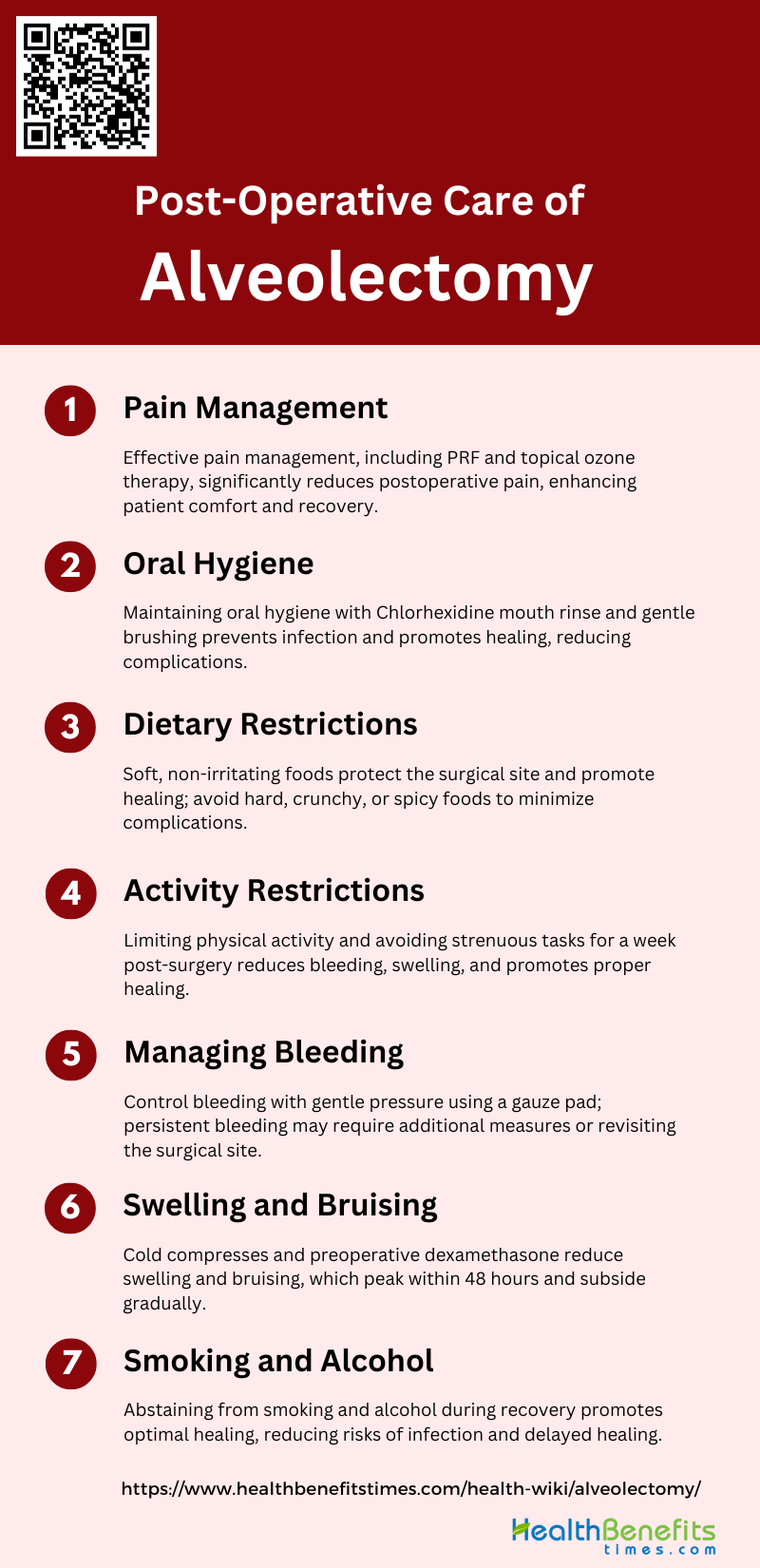
Post-Operative Care of Alveolectomy
Proper post-operative care following an alveolectomy is essential for ensuring optimal healing and minimizing complications. Adhering to the recommended guidelines can help manage discomfort, prevent infection, and promote faster recovery. Key aspects of post-operative care include:
1. Pain Management
Effective pain management is crucial following an alveolectomy to ensure patient comfort and facilitate recovery. The use of platelet-rich fibrin (PRF) has been shown to significantly reduce postoperative pain compared to controls, with notable improvements observed on the first, third, and seventh days post-surgery. Additionally, topical ozone therapy has demonstrated efficacy in reducing pain, particularly on the third postoperative day, when compared to dexamethasone. Mild analgesics are typically sufficient to manage pain, although stronger analgesics may be required depending on the severity of the pain and individual patient response.
2. Oral Hygiene
Maintaining proper oral hygiene post-surgery is essential to prevent infection and promote healing. The use of a Chlorhexidine mouth rinse twice daily can help reduce the incidence of wound infection and postoperative discomfort. Patients should be instructed on gentle brushing techniques to avoid disturbing the surgical site while ensuring cleanliness. Proper oral hygiene practices can also mitigate the risk of complications such as alveolar osteitis and secondary healing issues.
3. Dietary Restrictions
Postoperative dietary restrictions are necessary to protect the surgical site and promote healing. Patients are often advised to consume soft, non-irritating foods at a moderate temperature to avoid trauma to the surgical area. It is recommended to avoid hard, crunchy, or spicy foods that could disrupt the healing process. Adhering to these dietary guidelines can help minimize discomfort and reduce the risk of complications such as bleeding and infection.
4. Activity Restrictions
Limiting physical activity post-surgery is important to prevent complications and ensure proper healing. Patients should avoid strenuous activities and heavy lifting for at least a week following the procedure. Rest and limited movement can help reduce the risk of bleeding and swelling, contributing to a smoother recovery process. The duration of activity restrictions may vary based on the individual’s healing progress and the complexity of the surgery.
5. Managing Bleeding
Postoperative bleeding is a common concern following an alveolectomy. Patients should be advised to apply gentle pressure with a gauze pad to the surgical site to control bleeding. In cases where bleeding persists, additional measures such as the use of hemostatic agents or revisiting the surgical site may be necessary. Proper management of bleeding is crucial to prevent complications and ensure a smooth recovery.
6. Swelling and Bruising
Swelling and bruising are typical postoperative responses that usually peak within the first 48 hours and gradually subside over the following days. The application of cold compresses during the initial 24 hours can help minimize swelling. Intravenous dexamethasone administered preoperatively has been shown to significantly reduce swelling and bruising in the first postoperative week. Patients should be informed that while swelling and bruising are normal, they should seek medical advice if these symptoms worsen or do not improve.
7. Smoking and Alcohol
Smoking and alcohol consumption can adversely affect the healing process following an alveolectomy. Both habits are associated with an increased risk of postoperative complications such as infection, delayed healing, and alveolar osteitis. Patients should be strongly advised to abstain from smoking and alcohol consumption during the recovery period to promote optimal healing and reduce the likelihood of complications. Educating patients on the negative impacts of these substances can support better postoperative outcomes.
Difference between Alveolectomy vs. Alveoloplasty
Alveolectomy and alveoloplasty are two distinct surgical procedures often employed in dental and maxillofacial surgery, each with specific indications and outcomes. Alveolectomy involves the removal of alveolar bone, typically to facilitate the extraction of impacted teeth, such as mandibular third molars. For instance, a study comparing distolingual and distobuccal alveolectomy techniques found that the distolingual approach was more suitable for extracting position C teeth due to shorter operation times and less facial swelling, while the distobuccal technique was preferable for position B teeth. On the other hand, alveoloplasty is a procedure aimed at reshaping and smoothing the alveolar ridge, often performed to prepare the jaw for dentures or other prosthetic devices. It can be classified into primary and secondary alveoloplasty, with primary alveoloplasty referring to the initial surgical repair of an alveolar cleft, regardless of the patient’s age, and secondary alveoloplasty addressing sequelae from previous surgeries. Additionally, a comparison of bone resorption following intraseptal alveolotomy and labial alveolectomy indicated that intraseptal alveolotomy might result in slightly less bone resorption, suggesting a potential advantage in certain clinical scenarios. Thus, while both procedures involve the alveolar bone, their purposes, techniques, and outcomes differ significantly.
Potential Risks and Complications
While an alveolectomy is generally a safe procedure, it is not without potential risks and complications. Understanding these risks can help patients make informed decisions and prepare for any possible outcomes. The primary risks and complications associated with alveolectomy include:
1. Infection
Infection is a common complication following alveolectomy, often due to the presence of oral bacteria in the surgical site. Postoperative infections can lead to increased pain, swelling, and delayed healing. The use of antibiotics and maintaining good oral hygiene are critical in preventing infections. Studies have shown that the incidence of postoperative infections can be influenced by factors such as the duration of surgery and the patient’s medical history. Additionally, the application of platelet-rich fibrin (PRF) has been found to reduce the incidence of postoperative infections by promoting better soft tissue healing.
2. Pain and Swelling
Pain and swelling are typical postoperative responses following alveolectomy. These symptoms are usually temporary but can significantly affect the patient’s quality of life. The use of analgesics such as paracetamol and ibuprofen has been shown to be effective in managing postoperative pain. Moreover, platelet-rich fibrin (PRF) has been demonstrated to reduce pain and swelling by accelerating the healing process. Corticosteroids may also be used in selected cases to minimize inflammation and discomfort.
3. Bleeding
Postoperative bleeding is a potential risk associated with alveolectomy. It can be immediate or delayed and may result from trauma to the blood vessels during surgery. Proper surgical techniques and the use of hemostatic agents are essential to control bleeding. Studies have indicated that factors such as the type of surgical flap and the duration of the procedure can influence the risk of bleeding. Ensuring adequate hemostasis before concluding the surgery is crucial to prevent complications.
4. Nerve Damage
Nerve damage, particularly to the inferior alveolar and lingual nerves, is a significant concern in alveolectomy. This can result in temporary or permanent paresthesia, affecting the patient’s sensory functions. The risk of nerve injury is higher in cases where the surgical site is in close proximity to the nerves. Techniques such as coronectomy , which involves removing only the crown of the tooth, have been suggested to minimize the risk of nerve damage. Studies have reported varying incidences of nerve injuries, with some cases resolving within weeks.
5. Dry Socket
Dry socket, or alveolar osteitis, is a painful condition that can occur after tooth extraction, including alveolectomy. It is characterized by the dislodgement of the blood clot from the socket, leading to exposed bone and severe pain. The use of PRF has been shown to significantly reduce the incidence of dry socket by promoting better clot stability and healing. Additionally, maintaining good oral hygiene and avoiding smoking can help prevent this complication.
6. Jaw Fracture
Jaw fractures are a rare but serious complication of alveolectomy, particularly in patients with weakened bone structures due to conditions such as osteoporosis or previous radiation therapy. The risk of fracture increases with the complexity of the surgery and the amount of bone removal required. Preventive measures include careful surgical planning and the use of less invasive techniques when possible. Studies have highlighted the importance of evaluating the patient’s bone health before proceeding with the surgery.
7. Improper Healing
Improper healing can result from various factors, including infection, poor surgical technique, and patient non-compliance with postoperative care instructions. This can lead to complications such as delayed wound closure, formation of scar tissue, and chronic pain. The use of PRF has been shown to enhance the healing process by promoting tissue regeneration and reducing inflammation. Ensuring that patients follow postoperative care guidelines is crucial for optimal healing outcomes.
8. Allergic Reactions
Allergic reactions to medications or materials used during alveolectomy, such as local anesthetics or sutures, can occur. These reactions can range from mild skin rashes to severe anaphylaxis. It is essential to take a thorough medical history to identify any known allergies and to monitor the patient closely during and after the procedure. In cases where allergic reactions are suspected, alternative medications or materials should be used. Proper patient education and communication are key to preventing and managing allergic reactions effectively.