Allergies are immune system disorders characterized by an overreaction to substances known as allergens. When a person with allergies is first exposed to an allergen, their immune system produces an antibody called immunoglobulin E (IgE). Subsequent exposures lead to the production of more IgE, which binds to mast cells and basophils. These cells release histamine and other chemicals, causing allergic reactions as the body attempts to eliminate the allergen. Allergies can be triggered by various factors, including environmental elements, foods, and insect stings, and can manifest in different forms such as hay fever, food allergies, and skin reactions.
Allergies are immune system disorders characterized by an overreaction to substances known as allergens. When a person with allergies is first exposed to an allergen, their immune system produces an antibody called immunoglobulin E (IgE). Subsequent exposures lead to the production of more IgE, which binds to mast cells and basophils. These cells release histamine and other chemicals, causing allergic reactions as the body attempts to eliminate the allergen. Allergies can be triggered by various factors, including environmental elements, foods, and insect stings, and can manifest in different forms such as hay fever, food allergies, and skin reactions.
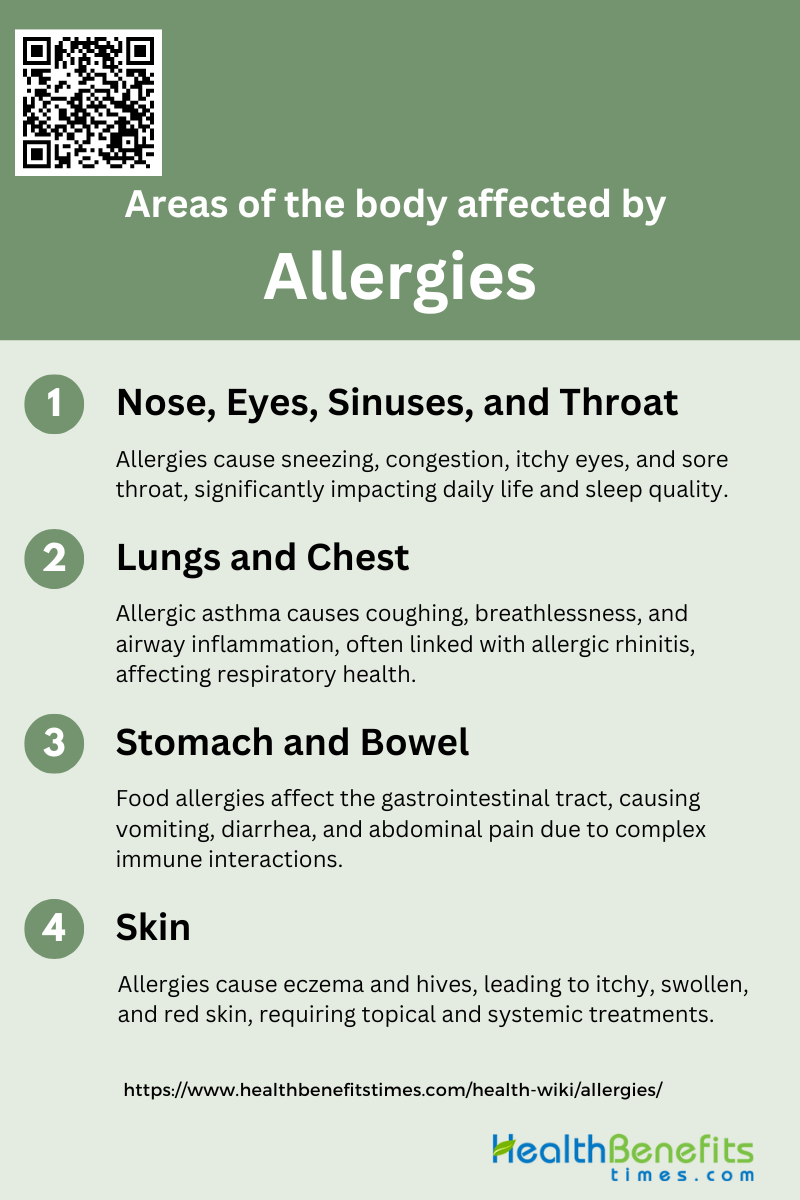
Areas of the body affected by Allergies
Understanding which areas are commonly affected can help in identifying and managing allergic reactions effectively. Here are some of the primary areas of the body that can be impacted by allergies:
1. Nose, Eyes, Sinuses, and Throat
Allergies can significantly impact the nose, eyes, sinuses, and throat, leading to a range of symptoms such as sneezing, nasal congestion, rhinorrhea, nasal itching, and sore throat. Allergic rhinitis, a common condition, is characterized by these symptoms and is often triggered by airborne allergens like pollen, dust mites, and animal dander. When the eyes are involved, the condition is referred to as allergic rhinoconjunctivitis, which includes symptoms like red, itchy, and watery eyes. The interaction between the nose and lungs in allergic diseases suggests a systemic link involving mucosal sites and inflammatory processes. These symptoms can significantly affect the quality of life, causing sleep disturbances and impairing daily activities.
2. Lungs and Chest
Allergic asthma is a common manifestation where exposure to allergens triggers inflammation and narrowing of the airways, causing difficulty in breathing. The connection between allergic rhinitis and asthma is well-documented, with many patients experiencing both conditions simultaneously. The systemic nature of allergies means that inflammation in the nasal passages can exacerbate asthma symptoms, highlighting the importance of managing both conditions concurrently. Effective treatment strategies, including allergen immunotherapy, can help reduce the severity of symptoms and improve overall respiratory health.
3. Stomach and Bowel
Allergies can also impact the gastrointestinal tract, leading to symptoms such as altered gastrointestinal motility, dysphagia, and disorders of the stomach and bowel. Food allergies, in particular, can cause severe reactions including vomiting, diarrhea, and abdominal pain. The interaction between the immune system and the gut is complex, involving various inflammatory processes and neuromodulation. Understanding these mechanisms is crucial for developing effective treatments to alleviate gastrointestinal symptoms associated with allergies. The systemic nature of allergic reactions means that managing allergies holistically can help mitigate their impact on the gastrointestinal system.
4. Skin
The skin is another area commonly affected by allergies, with conditions such as eczema (atopic dermatitis) and urticaria (hives) being prevalent. Allergic reactions can cause itchy, swollen, and red skin, significantly impacting the quality of life. Eczema is characterized by itchy, bumpy rashes and thickened skin, which can appear anywhere on the body. The release of chemical mediators like histamine during allergic reactions leads to these skin symptoms. Managing skin allergies often involves avoiding known allergens, using topical treatments, and in some cases, systemic medications to control inflammation and itching. Understanding the underlying mechanisms of skin allergies can help in developing targeted therapies to reduce their impact.
Impact on health and daily life of Allergies
It can significantly affect both health and daily life, leading to a range of symptoms from mild discomfort to severe reactions. These conditions can disrupt normal activities, reduce productivity, and impact overall well-being. Here are some key ways allergies can influence daily life:
1. Physical Discomfort
Allergies often cause significant physical discomfort, including symptoms such as nasal congestion, itchy eyes, and skin rashes. These symptoms can be persistent and severe, leading to a reduced quality of life. For instance, allergic rhinitis (AR) can result in inflamed nasal mucosa and nasal congestion, which can cause nasal collapse and airway obstruction, leading to physical discomfort and sleep disturbances.
2. Sleep Disturbances
Nasal congestion from AR can lead to frequent awakenings and difficulty falling back asleep, resulting in daytime fatigue and reduced productivity. Studies have shown that individuals with perennial AR often experience sleep problems, waking multiple times per night and struggling to get back to sleep, which significantly affects their daily functioning.
3. Daily Activities
For example, adolescents with AR report that their daily activities and school performance are negatively affected by their symptoms. This can lead to absenteeism and reduced academic productivity, highlighting the far-reaching impact of allergies on daily life.
4. Dietary Restrictions
Food allergies necessitate strict dietary restrictions to avoid allergic reactions, which can be challenging to manage. Children with food allergies often have to avoid multiple foods, which can limit their dietary choices and impact their nutritional intake. This can also place a significant burden on families, as they need to be vigilant about food ingredients and preparation methods.
5. Social Implications
Allergies can have profound social implications, including social isolation and bullying. For instance, children and teenagers with peanut allergies often face bullying and social exclusion due to their condition. This can lead to feelings of frustration, uncertainty, and stress, affecting their social interactions and overall well-being.
6. Work or School Performance
Individuals with AR and asthma often report significant impairment in work productivity and daily activities. This can lead to reduced performance and increased stress, further exacerbating the impact of allergies on their professional and academic lives.
7. Emotional Stress
Living with allergies can cause considerable emotional stress. The constant need to manage symptoms and avoid triggers can lead to anxiety and depression. For example, caregivers of children with food allergies often experience high levels of emotional stress due to the constant vigilance required to prevent allergic reactions.
8. Chronic Health Issues
Allergies can contribute to chronic health issues, such as asthma and atopic dermatitis. These conditions often coexist with allergies and can exacerbate symptoms, leading to a more significant health burden. For instance, individuals with both AR and asthma report more severe symptoms and greater impairment in daily functioning compared to those with AR alone.
9. Medication Side Effects
The medications used to manage allergies can have side effects that further impact health and daily life. For example, nasal corticosteroids used to treat nasal congestion in AR can cause side effects such as nasal irritation and dryness. These side effects can sometimes be mistaken for allergy symptoms, complicating the management of the condition.
10. Financial Burden
Managing allergies can be financially burdensome due to the cost of medications, treatments, and allergen-free foods. Families with children who have food allergies often face higher food costs and medical expenses. Additionally, the need for specialized care and frequent medical visits can add to the financial strain, impacting the overall quality of life.
Types of Allergies
Allergies can manifest in various forms, affecting different parts of the body and causing a range of symptoms. Understanding the types of allergies can help in identifying triggers and managing reactions effectively. Here are some common types of allergies:
1. Food Allergy
Food allergies occur when the immune system mistakenly identifies certain proteins in food as harmful, triggering an allergic reaction. Common symptoms include hives, swelling, digestive issues, and in severe cases, anaphylaxis. The prevalence of food allergies has been increasing, particularly among children. This rise necessitates a better understanding of the skin as a route for sensitization, as well as the biological properties of food allergens. In Iran, food allergens are among the most common, with a prevalence rate of 15.3% among patients with allergies.
2. Seasonal Allergy
Seasonal allergies, also known as hay fever or allergic rhinitis, are triggered by pollen from trees, grasses, and weeds. Symptoms include sneezing, runny nose, itchy eyes, and congestion. These allergies are most prevalent during specific times of the year when pollen counts are high. In Iran, pollen is the most common allergen, affecting 47.0% of patients with allergies, particularly in warm and dry climates. Historically, sensitization to pollens was the dominant form of allergic disease, especially before the rise in pediatric asthma.
3. Skin Allergy
Skin allergies manifest as conditions like eczema (atopic dermatitis), contact dermatitis, and hives. These reactions occur when the skin comes into contact with allergens such as certain metals, fragrances, or plants. The skin is a significant route for sensitization, particularly in the context of food allergies and atopic dermatitis. Understanding the role of skin exposure in allergic reactions is crucial for developing effective treatments and preventive measures.
4. Animal Allergy
Animal allergies are caused by proteins found in an animal’s skin cells, urine, and saliva. Common symptoms include sneezing, runny nose, and asthma-like symptoms. In Iran, animal allergens are one of the six common groups of allergens identified in patients with allergies. The rise in indoor living and close contact with pets has contributed to the increased prevalence of animal allergies, particularly among children.
5. Insect Allergy
Insect allergies are reactions to stings or bites from insects such as bees, wasps, and ants. Symptoms can range from mild local reactions to severe systemic reactions like anaphylaxis. Insect allergens are less commonly studied compared to other allergen types, but they are significant due to the potential severity of reactions. Understanding the biological properties of insect allergens and their role in allergic responses is essential for managing these allergies.
6. Dust Allergy
Dust allergies are primarily caused by house dust mites, which thrive in warm and humid environments. Symptoms include sneezing, runny nose, and asthma. In Iran, sensitization to house dust mites is predominant in northern and southern coastal areas, with a prevalence rate of 35.2% among patients with allergies. The rise in pediatric asthma has been linked to increased sensitization to indoor allergens like dust mites, driven by indoor living and reduced physical activity.
7. Drug Allergy
Drug allergies occur when the immune system reacts to medications, leading to symptoms such as hives, rash, and anaphylaxis. These reactions can be triggered by various drugs, including antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs). Understanding the immunological mechanisms behind drug allergies and identifying the specific allergens involved are crucial for preventing and managing these reactions. The prevalence and specific types of drug allergies can vary widely based on regional and demographic factors.
Common Symptoms of Allergies
Recognizing these symptoms is crucial for managing and treating allergic reactions effectively. Here are some common symptoms of allergies:
1. Nasal Congestion: Blocked or stuffy nose often due to inflammation of the nasal passages.
2. Itchy Eyes: Persistent itching, redness, and watering of the eyes caused by allergens.
3. Sneezing: Frequent sneezing as the body tries to expel allergens from the nasal passages.
4. Skin Rashes: Red, itchy, or swollen patches on the skin, often resulting from contact with allergens.
5. Shortness of Breath: Difficulty breathing, wheezing, or tightness in the chest, particularly in cases of asthma triggered by allergies.
6. Hives: Raised, red, itchy welts on the skin, typically appearing suddenly as a reaction to allergens.
Common Causes of Allergies
Allergies are caused by a variety of factors that can trigger an immune response in sensitive individuals. Understanding these common causes can help in managing and preventing allergic reactions. Here are some of the most prevalent causes of allergies:
1. Genetics
Genetic factors play a significant role in the development of allergic diseases. Studies have shown that atopic allergic conditions, such as asthma, rhinitis, and eczema, tend to cluster within families, indicating a strong genetic predisposition. Specific genes, such as those related to the immune system’s response to allergens, have been identified through Single Nucleotide Polymorphism (SNP) studies. For instance, genes like CD14 and Toll-like receptors (TLR4 and TLR2) are crucial in determining susceptibility to asthma and allergies. The genetic basis of these conditions is complex and involves multiple genes interacting with environmental factors.
2. Environment
Environmental factors are equally crucial in the development and exacerbation of allergic diseases. The “hygiene hypothesis” suggests that reduced microbial exposure during childhood, due to Westernized lifestyles, leads to an increased prevalence of allergic disorders. Airborne environmental antigens, such as pollen, are major triggers for conditions like asthma and allergic rhinitis. Additionally, environmental pollutants, dietary changes, and modern chemicals in detergents can alter the microbiome and epithelial surfaces, contributing to allergic responses. The interplay between genetic predisposition and environmental exposures is essential in understanding the pathogenesis of allergies.
3. Immune System Response
The immune system’s response to allergens is a critical factor in the development of allergic diseases. Allergies are often the result of an exaggerated type 2 T helper (Th2) cell-mediated immune response to otherwise harmless antigens. This response involves the production of IgE antibodies, which trigger inflammatory reactions upon allergen exposure. The failure to develop allergen-specific T-memory cells that suppress Th2 responses can lead to the proliferation of Th2 cells and subsequent allergic reactions. Additionally, epithelial barrier dysfunction and loss of immune tolerance are significant contributors to the altered immune responses seen in allergic diseases. Understanding these mechanisms is vital for developing effective prevention and treatment strategies.
When to See a Doctor for Allergies
If you experience persistent allergy symptoms that significantly impact your daily life, it may be time to see a doctor. Symptoms such as chronic nasal congestion, frequent sinus infections, difficulty breathing, or severe reactions like swelling, hives, or anaphylaxis warrant professional medical attention. Additionally, if over-the-counter medications fail to provide relief or if you suspect you have developed new allergies, consulting with a healthcare provider can help identify triggers and develop an effective treatment plan. Early intervention can prevent complications and improve your quality of life.