Albuminuria is a condition characterized by the presence of an abnormal amount of albumin in the urine, which is a key indicator of kidney disease and a significant risk factor for cardiovascular complications. It is commonly associated with diabetes and hypertension, and its prevalence increases with worsening glucose tolerance and higher blood pressure levels2 3. Albuminuria reflects widespread vascular damage and is linked to both renal and extrarenal complications, such as proliferative retinopathy and macroangiopathy, suggesting a common underlying cause. Genetic factors also play a role, with specific genetic loci influencing susceptibility to albuminuria, particularly in individuals with diabetes. Early detection and management of albuminuria are crucial, as it can serve as a surrogate endpoint for the progression of chronic kidney disease and guide therapeutic interventions to prevent further renal damage and cardiovascular events. Socioeconomic factors, such as poverty, have been shown to influence the prevalence of albuminuria, highlighting the need for targeted public health strategies to address these disparities.
Albuminuria is a condition characterized by the presence of an abnormal amount of albumin in the urine, which is a key indicator of kidney disease and a significant risk factor for cardiovascular complications. It is commonly associated with diabetes and hypertension, and its prevalence increases with worsening glucose tolerance and higher blood pressure levels2 3. Albuminuria reflects widespread vascular damage and is linked to both renal and extrarenal complications, such as proliferative retinopathy and macroangiopathy, suggesting a common underlying cause. Genetic factors also play a role, with specific genetic loci influencing susceptibility to albuminuria, particularly in individuals with diabetes. Early detection and management of albuminuria are crucial, as it can serve as a surrogate endpoint for the progression of chronic kidney disease and guide therapeutic interventions to prevent further renal damage and cardiovascular events. Socioeconomic factors, such as poverty, have been shown to influence the prevalence of albuminuria, highlighting the need for targeted public health strategies to address these disparities.
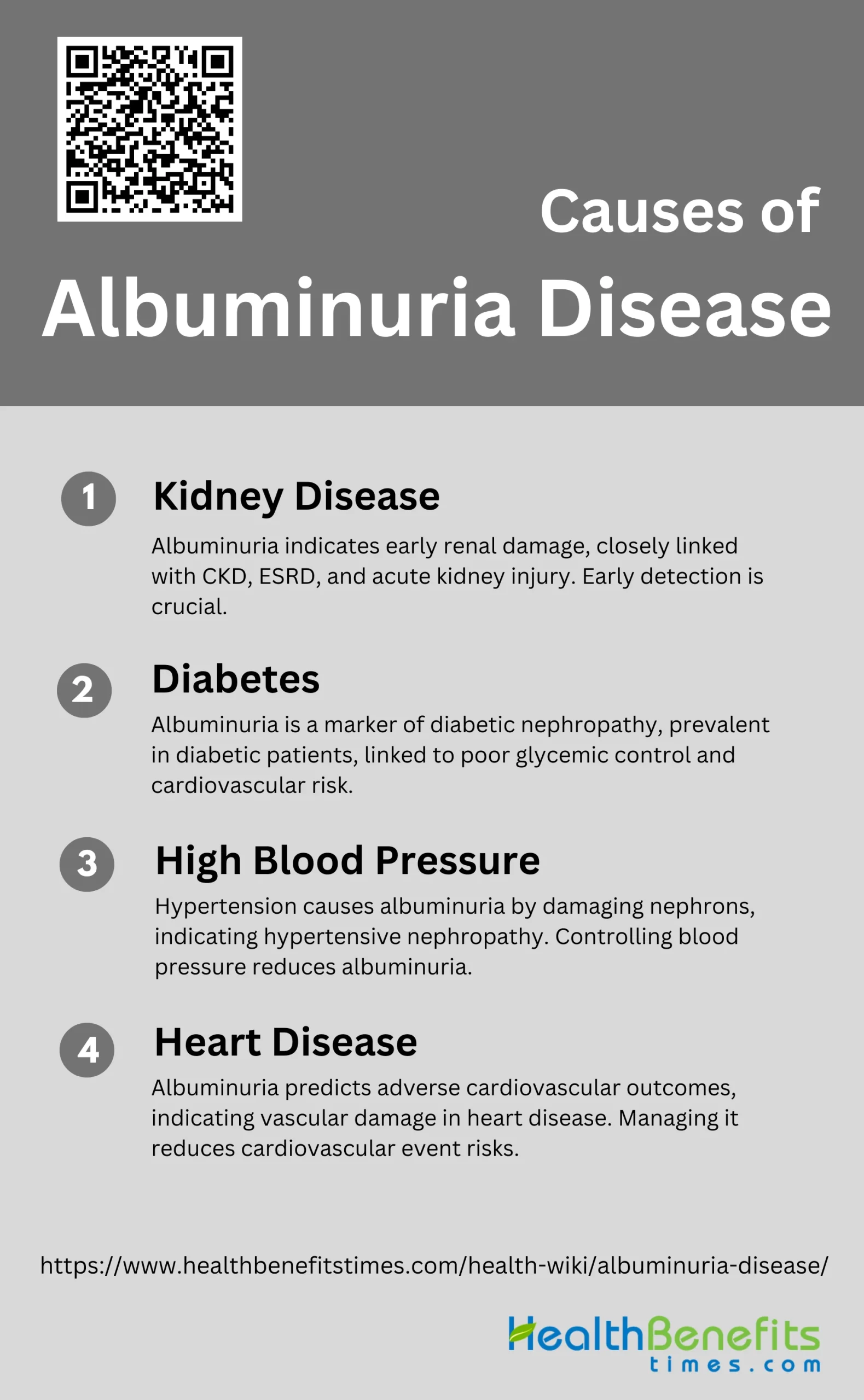
Causes of Albuminuria Disease
Below is a list of the primary causes contributing to the development of albuminuria.
1. Kidney Disease
Chronic kidney disease (CKD) and albuminuria are closely linked, with albuminuria serving as an early indicator of nephropathy. Studies have shown that albuminuria is prevalent in patients with CKD and is associated with poor renal outcomes, including end-stage renal disease (ESRD) and acute kidney injury. The presence of albumin in the urine reflects glomerular damage, which can progress to more severe kidney dysfunction if left untreated. Early detection and management of albuminuria are crucial in preventing the progression of kidney disease.
2. Diabetes
Diabetes is a major cause of albuminuria, with a significant proportion of diabetic patients exhibiting this condition. Albuminuria is an early and sensitive marker of diabetic nephropathy, a common complication of diabetes that can lead to ESRD. The prevalence of albuminuria increases with worsening glucose tolerance and poor glycemic control. Studies have shown that microalbuminuria, a subclinical form of albuminuria, is often present in the early stages of diabetes and is associated with an increased risk of cardiovascular mortality. Effective management of blood glucose levels and blood pressure can help reduce the risk of albuminuria in diabetic patients.
3. High Blood Pressure
High blood pressure (hypertension) is another significant cause of albuminuria. Hypertensive vascular damage, particularly in the juxtamedullary nephrons, leads to increased albumin excretion in the urine. Albuminuria is often an early sign of hypertensive nephropathy and is associated with poor cardiovascular outcomes. Studies have shown that controlling blood pressure can reduce the degree of albuminuria and prevent further renal damage. The relationship between high blood pressure and albuminuria underscores the importance of regular monitoring and management of hypertension to prevent kidney damage.
4. Heart Disease
Albuminuria is closely associated with cardiovascular diseases (CVDs) and is a predictor of adverse cardiovascular outcomes. The presence of albumin in the urine indicates endothelial dysfunction and vascular damage, which are common in patients with heart disease. Studies have shown that albuminuria is linked to an increased risk of coronary heart disease, stroke, and other cardiovascular events. In patients with diabetes and hypertension, albuminuria is a marker of generalized vascular disease, affecting both small and large blood vessels. Managing albuminuria through lifestyle changes and medication can help reduce the risk of cardiovascular events and improve overall heart health.
Sign and Symptoms of Albuminuria Disease
Albuminuria often presents without noticeable symptoms in its early stages. However, as the condition progresses, various signs and symptoms may become apparent:
- Foamy Urine: The presence of excess albumin in the urine can cause it to appear frothy or foamy.
- Swelling (Edema): Swelling in the hands, feet, abdomen, or face can occur due to fluid retention.
- Fatigue: Generalized tiredness and lack of energy may be experienced due to the body’s impaired ability to filter waste.
- High Blood Pressure: Elevated blood pressure may develop as a consequence of kidney damage and fluid retention.
- Frequent Urination: An increased need to urinate, especially at night, can be a sign of kidney issues.
- Muscle Cramps: Electrolyte imbalances due to impaired kidney function can lead to muscle cramps.
- Proteinuria: Laboratory tests reveal elevated levels of protein in the urine, a hallmark of albuminuria.
- Anemia: Reduced kidney function can lead to decreased production of erythropoietin, causing anemia and related symptoms like paleness and shortness of breath.
- Nausea and Vomiting: Accumulation of waste products in the blood can lead to gastrointestinal symptoms.
- Decreased Appetite: Loss of appetite may occur due to the buildup of toxins in the bloodstream.
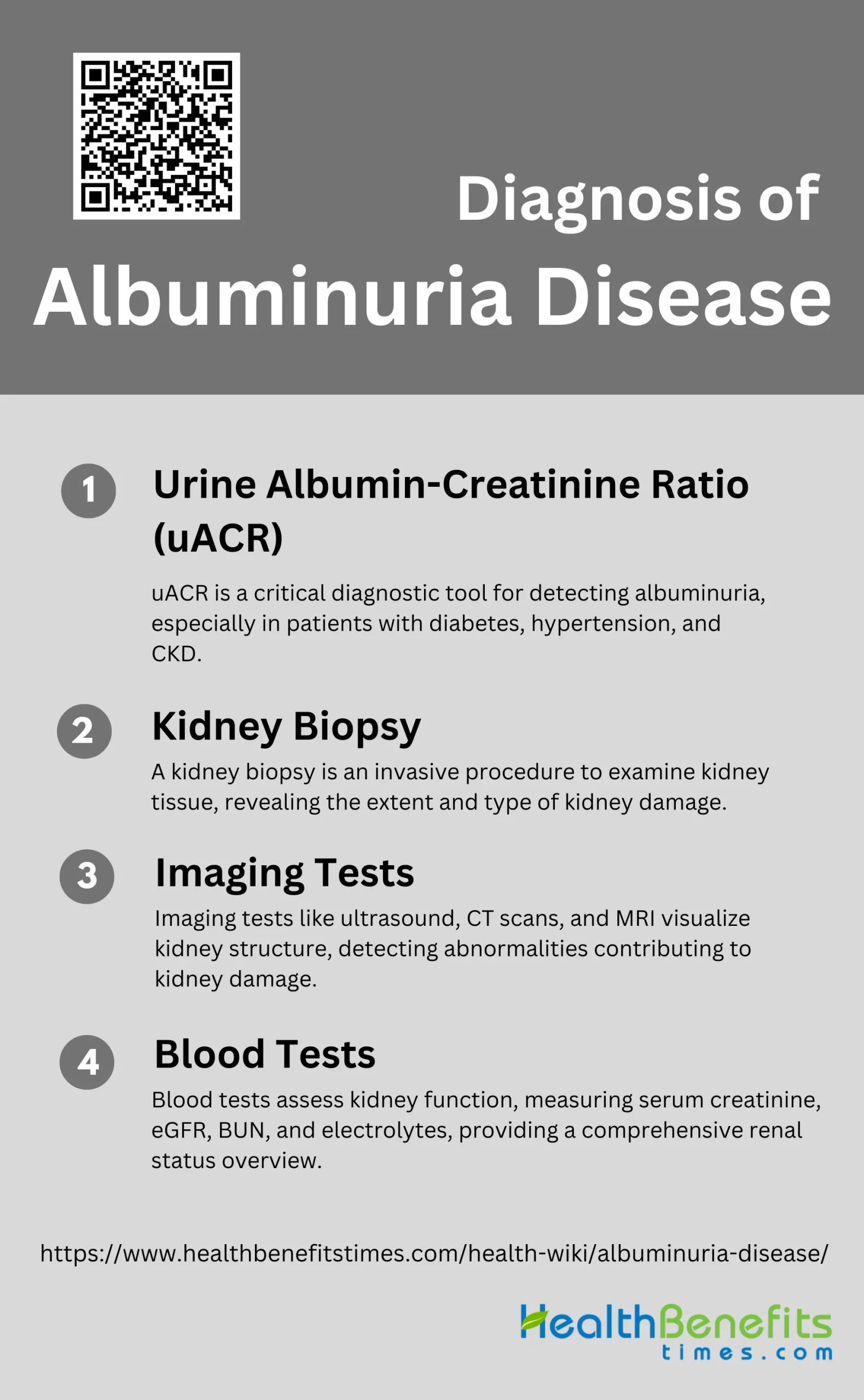
Diagnosis of Albuminuria Disease
Diagnosing albuminuria involves several tests and evaluations to determine the presence and severity of the condition. Here are the key steps in the diagnostic process:
1. Urine Albumin-Creatinine Ratio (uACR)
The urine albumin-creatinine ratio (uACR) is a critical diagnostic tool for detecting albuminuria, a key indicator of kidney disease. uACR is particularly useful for screening patients with diabetes mellitus, hypertension, and chronic kidney disease (CKD). It involves measuring the amount of albumin and creatinine in a random urine sample, providing a reliable marker for kidney damage. Studies have shown that uACR has high sensitivity and specificity for detecting microalbuminuria, making it a preferred method for early diagnosis. Point-of-care (POC) testing for uACR can further enhance diagnostic efficiency by providing immediate results, facilitating timely clinical decisions.
2. Kidney Biopsy
A kidney biopsy is a more invasive diagnostic procedure used to obtain a tissue sample from the kidney for detailed examination. This method is often employed when non-invasive tests, such as uACR, indicate significant kidney damage or when the cause of kidney disease is unclear. The biopsy can reveal the extent and type of kidney damage, including glomerular, tubular, or interstitial abnormalities, and can help differentiate between various types of kidney diseases. It is particularly useful in cases where proteinuria is detected, as it can provide insights into the underlying pathology, such as glomerulonephritis or tubulointerstitial nephritis.
3. Imaging Tests
Imaging tests, such as ultrasound, CT scans, and MRI, play a supportive role in diagnosing albuminuria-related kidney disease. These tests can help visualize the kidney’s structure and detect abnormalities such as cysts, tumors, or obstructions that may contribute to kidney damage. While imaging tests do not directly measure albumin levels, they provide valuable information about the kidney’s size, shape, and any structural changes that may be associated with chronic kidney disease. Imaging is often used in conjunction with other diagnostic methods to provide a comprehensive assessment of kidney health.
4. Blood Tests
Blood tests are essential in the diagnosis and monitoring of kidney disease associated with albuminuria. Key blood tests include serum creatinine and estimated glomerular filtration rate (eGFR), which help assess kidney function. Elevated serum creatinine levels and reduced eGFR are indicative of impaired kidney function and are often correlated with increased uACR levels. Additionally, blood tests can measure other markers of kidney health, such as blood urea nitrogen (BUN) and electrolytes, providing a broader picture of the patient’s renal status. Regular blood testing is crucial for monitoring disease progression and the effectiveness of treatment strategies.
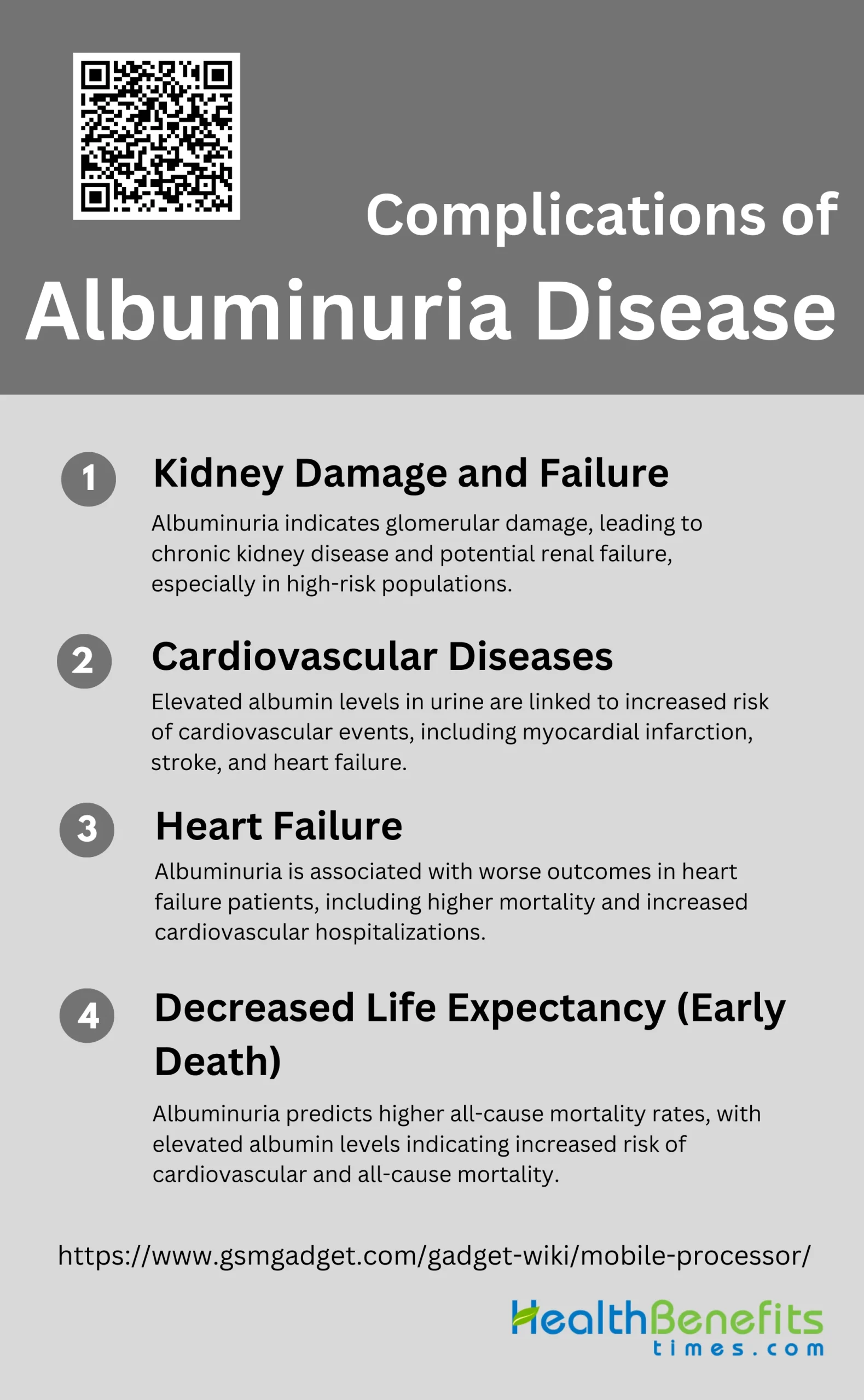
Complications of Albuminuria Disease
Albuminuria can lead to various complications if left untreated. Here are the key complications associated with the disease:
1. Kidney Damage and Failure
Albuminuria is a significant marker for kidney damage and can lead to kidney failure. Elevated levels of albumin in the urine indicate glomerular damage, which can progress to chronic kidney disease (CKD) and eventually renal failure. Studies have shown that albuminuria is prevalent in various populations, including children with sickle cell disease, where it serves as an early indicator of CKD. In kidney transplant recipients, higher urine albumin-creatinine ratios (ACR) are independently associated with increased risks of allograft failure. Monitoring and managing albuminuria can help in early detection and intervention, potentially preventing the progression to kidney failure.
2. Cardiovascular Diseases
Albuminuria is strongly associated with cardiovascular diseases (CVD). Elevated albumin levels in the urine are linked to an increased risk of cardiovascular events such as myocardial infarction, stroke, and heart failure. In patients with vascular disease, changes in albuminuria levels predict cardiovascular outcomes, with higher levels correlating with increased risks. Additionally, in hypertensive patients with left ventricular hypertrophy and diabetes, reductions in albuminuria have been shown to translate into reduced cardiovascular events. This relationship underscores the importance of albuminuria as a biomarker for cardiovascular risk assessment and management.
3. Heart Failure
Albuminuria is also associated with the severity and prognosis of heart failure. Patients with heart failure often exhibit elevated urinary albumin levels, which correlate with worse clinical outcomes. Studies have demonstrated that both microalbuminuria and macroalbuminuria are linked to increased mortality and cardiovascular hospitalizations in heart failure patients. The presence of albuminuria in these patients indicates a higher risk of adverse events, making it a critical factor in the management and treatment of heart failure. Monitoring albuminuria can thus provide valuable insights into the progression and management of heart failure.
4. Decreased Life Expectancy (Early Death)
Albuminuria is a predictor of decreased life expectancy and early death. Elevated levels of albumin in the urine are associated with higher all-cause mortality rates. In the general population, both decreased glomerular filtration rate (GFR) and increased albuminuria independently predict higher risks of cardiovascular and all-cause mortality. Similarly, in high-risk populations, lower GFR and higher albuminuria levels are multiplicatively associated with increased mortality. These findings highlight the critical role of albuminuria as a prognostic marker for early death, emphasizing the need for early detection and intervention to improve life expectancy.
Treatment and Management of Albuminuria Disease
Effectively managing albuminuria involves a combination of lifestyle changes, medications, and regular monitoring. Here are the key approaches:
1. Blood Pressure Control
Controlling blood pressure is crucial in managing albuminuria, particularly in patients with diabetic nephropathy. Antihypertensive drugs, especially those that interrupt the renin-angiotensin system (RAS) such as angiotensin II antagonists, have been shown to significantly reduce albuminuria and provide renal protection beyond their blood pressure-lowering effects. Studies indicate that a reduction in albuminuria correlates with a proportional decrease in the risk of renal end points and end-stage renal disease (ESRD). Therefore, maintaining optimal blood pressure is a key strategy in reducing albuminuria and protecting renal function.
2. Blood Sugar Control
Effective blood sugar control is essential in managing albuminuria, particularly in diabetic patients. Elevated blood glucose levels are a significant risk factor for the development and progression of albuminuria. Intensive glucose control has been shown to reduce the rate of albuminuria and slow the progression of renal disease. Moreover, the degree of albuminuria reduction achieved through glucose control is associated with long-term renal and cardiovascular protection. Therefore, maintaining optimal glycemic levels is critical in managing albuminuria and preventing further renal damage.
3. Dietary Changes
Dietary modifications, including reducing sodium intake and following a low-protein diet, can significantly impact the management of albuminuria. Sodium restriction has been shown to enhance the efficacy of RAS inhibitors in reducing albuminuria and blood pressure. Additionally, a low-protein diet can help decrease the rate of glomerular filtration rate (GFR) loss and lower albuminuria levels. These dietary changes, when combined with pharmacological interventions, can provide a comprehensive approach to managing albuminuria and protecting renal function.
4. Weight Management
Maintaining a healthy weight is important in managing albuminuria, as obesity is a known risk factor for both diabetes and hypertension, which are closely linked to albuminuria. Weight loss can improve insulin sensitivity, reduce blood pressure, and lower albuminuria levels Studies have shown that body mass index (BMI) is an independent risk factor for albuminuria, and weight management can help mitigate this risk. Therefore, incorporating weight management strategies into the treatment plan is essential for reducing albuminuria and improving overall renal health.
5. Smoking Cessation
Smoking is a significant risk factor for the progression of albuminuria and renal disease. It has been associated with increased levels of albuminuria and a higher risk of cardiovascular events. Smoking cessation can lead to a reduction in albuminuria and improve renal outcomes. Additionally, quitting smoking can enhance the effectiveness of other therapeutic interventions, such as RAS inhibitors, in reducing albuminuria. Therefore, encouraging patients to quit smoking is a critical component of managing albuminuria and protecting renal function.
6. Regular Monitoring
Regular monitoring of albuminuria levels is essential for assessing the effectiveness of treatment and making necessary adjustments. Albuminuria is a strong predictor of renal and cardiovascular outcomes, and its reduction is associated with improved long-term prognosis. Monitoring should include periodic measurements of urinary albumin excretion and other relevant biomarkers to track disease progression and treatment response. This proactive approach allows for timely interventions and adjustments to the treatment plan, ensuring optimal management of albuminuria.
7. Medication Adjustment
Adjusting medications based on the patient’s response to treatment is crucial in managing albuminuria. RAS inhibitors, such as ACE inhibitors and angiotensin II receptor blockers, are the mainstay of therapy and have been shown to significantly reduce albuminuria. However, some patients may require higher doses or combination therapy to achieve optimal results. Additionally, new therapeutic agents targeting albuminuria are being explored and may offer additional benefits. Regular assessment and adjustment of medications are necessary to ensure effective management of albuminuria.
8. Cholesterol Management
Managing cholesterol levels is important in patients with albuminuria, as dyslipidemia is a common comorbidity and risk factor for cardiovascular disease. Elevated cholesterol levels can exacerbate renal damage and increase albuminuria. Lipid-lowering medications, such as statins, can help reduce albuminuria and improve cardiovascular outcomes. Additionally, maintaining healthy cholesterol levels can enhance the overall effectiveness of the treatment plan and provide comprehensive protection against renal and cardiovascular complications. Therefore, cholesterol management should be an integral part of the treatment strategy for albuminuria.
Prevention Strategies for Albuminuria Disease
Preventing albuminuria involves adopting healthy lifestyle habits and managing underlying health conditions. Here are key prevention strategies:
1. Control Blood Sugar
Maintaining optimal blood sugar levels is crucial in preventing albuminuria, especially in diabetic patients. Intensive diabetes treatment has been shown to significantly reduce the risk of developing albuminuria. For instance, the Diabetes Control and Complications Trial (DCCT) demonstrated that intensive diabetes management led to a 45% reduction in the risk of microalbuminuria and a 61% reduction in the risk of macroalbuminuria over an 18-year follow-up period. Effective blood sugar control helps mitigate the progression of diabetic nephropathy, thereby reducing the incidence of albuminuria.
2. Manage Blood Pressure
Managing blood pressure is another critical strategy in preventing albuminuria. Antihypertensive drugs, particularly those that inhibit the renin-angiotensin-aldosterone system (RAAS), have been shown to reduce urinary albumin excretion and provide renal protection. Studies have demonstrated that RAAS inhibitors, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), significantly lower albuminuria levels and are associated with long-term renal and cardiovascular protection. These medications help reduce glomerular pressure and proteinuria, thereby protecting kidney function.
3. Healthy Diet
A healthy diet plays a vital role in preventing albuminuria. Dietary interventions, such as reducing salt intake and following a low-protein diet, can help manage blood pressure and reduce the burden on the kidneys. Additionally, a balanced diet rich in fruits, vegetables, and whole grains can help control blood sugar levels and reduce the risk of developing diabetes-related complications. Studies have shown that dietary modifications, along with pharmacological interventions, can significantly reduce albuminuria and slow the progression of chronic kidney disease (CKD).
4. Regular Exercise
Regular physical activity is essential for maintaining overall health and preventing albuminuria. Exercise helps control blood sugar levels, manage blood pressure, and maintain a healthy weight, all of which are important factors in preventing kidney damage. Studies have shown that regular exercise can improve insulin sensitivity, reduce inflammation, and enhance cardiovascular health, thereby reducing the risk of albuminuria and its associated complications. Incorporating moderate-intensity aerobic exercise and strength training into daily routines can provide significant health benefits.
5. Avoid NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) can have detrimental effects on kidney function and should be avoided, especially in individuals at risk for albuminuria. NSAIDs can cause renal vasoconstriction, reduce glomerular filtration rate, and increase the risk of acute kidney injury. Long-term use of NSAIDs has been associated with the development and progression of CKD. Therefore, it is important to use alternative pain management strategies and consult healthcare providers before using NSAIDs, particularly in individuals with diabetes or hypertension.
6. No Smoking
Smoking is a significant risk factor for the development and progression of albuminuria. It contributes to endothelial dysfunction, increases oxidative stress, and promotes inflammation, all of which can damage the kidneys. Studies have shown that smoking cessation can significantly reduce the risk of albuminuria and slow the progression of CKD. Quitting smoking not only benefits kidney health but also improves overall cardiovascular health, reducing the risk of heart disease and stroke.
7. Regular Check-ups
Regular medical check-ups are essential for early detection and management of albuminuria. Routine screening for albuminuria, especially in individuals with diabetes, hypertension, or a family history of kidney disease, can help identify the condition at an early stage. Early intervention with appropriate medications and lifestyle modifications can prevent the progression of albuminuria and reduce the risk of CKD and its complications. Regular monitoring of kidney function, blood pressure, and blood sugar levels is crucial for effective management.
8. Medications
Medications play a crucial role in the prevention and management of albuminuria. RAAS inhibitors, such as ACE inhibitors and ARBs, are the cornerstone of pharmacological treatment for reducing albuminuria and protecting kidney function. These medications help lower blood pressure, reduce proteinuria, and provide long-term renal and cardiovascular protection. Additionally, other medications, such as anti-inflammatory agents and glucose-lowering drugs, may also be used to manage albuminuria and its underlying causes. It is important to follow healthcare providers’ recommendations and adhere to prescribed medications for optimal outcomes.