 Albumin is the most abundant protein in human serum, playing a crucial role in maintaining oncotic pressure and serving as a carrier for various endogenous and exogenous substances. It is synthesized in the liver and is essential for transporting hormones, fatty acids, and drugs, as well as maintaining fluid balance within the blood vessels. Albumin’s high biocompatibility and extensive distribution in blood and interstitial fluids make it a valuable component in medical treatments, including drug delivery systems and therapeutic interventions for conditions like liver cirrhosis and sepsis. Additionally, albumin levels are often used as a biomarker in various clinical settings to assess nutritional status and disease prognosis.
Albumin is the most abundant protein in human serum, playing a crucial role in maintaining oncotic pressure and serving as a carrier for various endogenous and exogenous substances. It is synthesized in the liver and is essential for transporting hormones, fatty acids, and drugs, as well as maintaining fluid balance within the blood vessels. Albumin’s high biocompatibility and extensive distribution in blood and interstitial fluids make it a valuable component in medical treatments, including drug delivery systems and therapeutic interventions for conditions like liver cirrhosis and sepsis. Additionally, albumin levels are often used as a biomarker in various clinical settings to assess nutritional status and disease prognosis.
Albumin Sources
Albumin is a protein commonly found in the blood, and it’s essential for maintaining the proper osmotic pressure in the bloodstream and for transporting various substances throughout the body. Here are some sources of albumin:
- Human Plasma: Albumin can be isolated from the plasma of human blood donors.
- Eggs: Egg whites are a rich source of albumin, particularly in the form of ovalbumin.
- Milk: Bovine serum albumin (BSA) is found in cow’s milk and is often used in medical and laboratory settings.
- Livestock: Albumin can be derived from the blood of livestock animals, such as cattle and pigs.
- Recombinant Technology: Albumin can be produced through recombinant DNA technology using yeast or bacteria.
- Plant Seeds: Certain plant seeds, like soybeans, contain albumin that can be extracted and used for various purposes.
Functions of Albumin in the Body
It is essential for various physiological processes, from sustaining blood volume to facilitating the transport of molecules. Below is a list of the key functions albumin performs in the body.
1. Maintaining Oncotic Pressure
Albumin is the primary determinant of plasma oncotic pressure, which is crucial for modulating the distribution of fluids between the vascular and interstitial compartments. This function helps maintain the balance of fluid in the blood vessels, preventing edema and ensuring proper circulation. Albumin’s role in maintaining oncotic pressure is well-documented, with approximately 75% of the total colloid osmotic pressure attributed to albumin. This pressure is essential for keeping fluids within the bloodstream and preventing leakage into surrounding tissues, thereby stabilizing blood volume and pressure.
2. Transport of Substances
It binds to both endogenous and exogenous compounds, facilitating their distribution throughout the body. This transport function is vital for the delivery of nutrients and the removal of waste products. Albumin’s ability to bind and transport various molecules also plays a significant role in pharmacokinetics, affecting the distribution and efficacy of many drugs. This multifunctional transport capability underscores albumin’s importance in maintaining physiological homeostasis.
3. Antioxidant Properties
This antioxidant function helps protect cells and tissues from oxidative damage, which is implicated in various diseases, including diabetes and cardiovascular disorders. Albumin’s ability to scavenge free radicals and reduce oxidative stress contributes to its protective role in the body, enhancing its therapeutic potential beyond its traditional functions. This property is particularly important in conditions of critical illness, where oxidative stress is prevalent.
4. Nutritional Marker
Serum albumin levels are often used as a nutritional marker, reflecting the body’s protein status and overall nutritional health. Low albumin levels can indicate malnutrition, liver disease, or chronic inflammation, making it a valuable diagnostic tool in clinical settings. Monitoring albumin levels helps healthcare providers assess the nutritional needs of patients and tailor interventions accordingly. Its role as a nutritional marker is supported by its widespread use in evaluating the health status of individuals with various medical conditions.
5. Drug Binding and Transport
Albumin’s ability to bind to a wide range of drugs significantly influences their pharmacokinetics and pharmacodynamics. By binding to drugs, albumin can affect their distribution, half-life, and clearance from the body. This binding capacity is crucial for the efficacy and safety of many medications, as it helps regulate their availability and activity within the bloodstream. Albumin’s role in drug transport is particularly important in the context of drug delivery systems, where it can enhance the therapeutic effects of medications.
6. Buffering pH
It can bind to hydrogen ions and other charged particles, thereby stabilizing the pH of the blood and preventing significant fluctuations that could disrupt cellular functions. This buffering action is essential for maintaining the optimal pH range required for various enzymatic and metabolic processes. Albumin’s role in acid-base balance underscores its importance in physiological homeostasis and its potential therapeutic applications in conditions characterized by acid-base disturbances.
7. Regulation of Capillary Permeability
Albumin plays a critical role in regulating capillary permeability, particularly in maintaining the integrity of the vascular endothelium. It helps modulate the passage of fluids and solutes across the capillary walls, preventing excessive leakage and maintaining vascular stability. This function is vital for preventing edema and ensuring proper tissue perfusion. Albumin’s regulatory effect on capillary permeability is supported by studies demonstrating its influence on endothelial cell function and microvascular integrity.
8. Stabilizing Blood Volume
It is essential for stabilizing blood volume by maintaining oncotic pressure and preventing fluid leakage from the vascular compartment. This stabilization is crucial for ensuring adequate tissue perfusion and oxygen delivery throughout the body. By retaining fluids within the bloodstream, albumin helps maintain blood pressure and supports cardiovascular function. Its role in stabilizing blood volume is particularly important in clinical settings, where albumin administration can be used to treat hypovolemia and other conditions associated with fluid imbalance.
Causes of low albumin levels
Low levels of albumin, known as hypoalbuminemia, can arise from a variety of underlying conditions and factors. Here are some of the primary causes that contribute to the reduction of albumin in the bloodstream:
1. Severe Liver Disease
Severe liver disease significantly impacts albumin levels due to the liver’s role in albumin synthesis. When liver function is compromised, the production of albumin decreases, leading to hypoalbuminemia. This condition is often observed in patients with chronic liver diseases such as cirrhosis or hepatitis. The liver’s inability to produce sufficient albumin results in a marked reduction in serum albumin levels, which can exacerbate symptoms and complications associated with liver disease.
2. Kidney Disease
Kidney disease, particularly chronic renal failure, affects albumin metabolism and synthesis. In conditions like uremia, the liver’s ability to synthesize albumin is impaired, leading to reduced serum albumin levels. Additionally, kidney disease can cause albumin to be lost in the urine, a condition known as albuminuria, further decreasing serum albumin levels. This dual impact on synthesis and loss makes kidney disease a significant contributor to hypoalbuminemia.
3. Gastrointestinal Disorders
Gastrointestinal disorders can lead to low albumin levels through malabsorption and protein loss. Conditions such as Crohn’s disease, celiac disease, and severe gastrointestinal infections can impair the absorption of nutrients, including proteins, leading to decreased albumin synthesis. Additionally, protein-losing enteropathies result in the direct loss of albumin from the gastrointestinal tract, further contributing to hypoalbuminemia.
4. Severe Burns and Trauma
Severe burns and trauma can cause a significant drop in albumin levels due to increased vascular permeability and protein loss. The body’s acute phase response to trauma or burns leads to inflammation and the release of cytokines, which can suppress albumin synthesis. Additionally, the loss of plasma proteins through damaged skin or tissues exacerbates the reduction in serum albumin levels, making it a common issue in patients with severe burns or trauma.
5. Malnutrition
Malnutrition is a primary cause of low albumin levels, particularly in populations with inadequate protein intake. Albumin synthesis requires sufficient dietary protein, and when intake is insufficient, the liver cannot produce adequate amounts of albumin. This condition is often observed in elderly populations, individuals with eating disorders, or those in regions with food scarcity. Malnutrition-related hypoalbuminemia is a significant marker of poor nutritional status and overall health.
6. Cancer
Cancer can lead to hypoalbuminemia through several mechanisms, including malnutrition, inflammation, and increased catabolism. Tumors can cause a hypermetabolic state, increasing the body’s protein requirements and leading to muscle wasting and reduced albumin synthesis. Additionally, cancer-related inflammation can suppress albumin production. These factors combined make hypoalbuminemia a common finding in cancer patients, often correlating with disease severity and prognosis.
7. Sepsis
Sepsis is a severe systemic infection that can drastically reduce albumin levels. The inflammatory response to sepsis increases vascular permeability, leading to the leakage of albumin into the interstitial space. Additionally, the acute phase response during sepsis suppresses albumin synthesis. This combination of increased loss and decreased production results in significant hypoalbuminemia, which is associated with worse outcomes in septic patients.
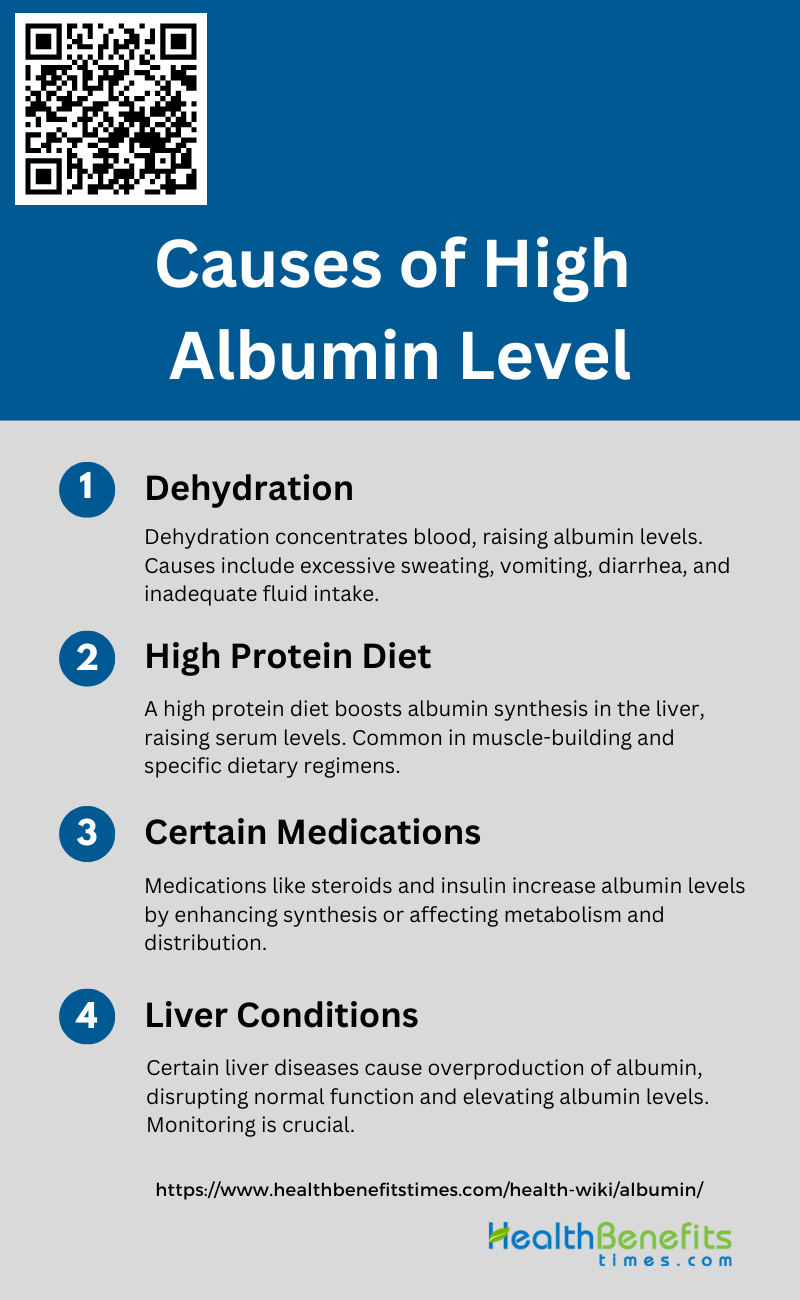
Causes of high albumin level
High albumin levels in the blood, also known as hyperalbuminemia, can be caused by several factors. Some of the common causes include:
1. Dehydration
Dehydration is a common cause of elevated albumin levels in the blood. When the body loses more fluids than it takes in, the blood becomes more concentrated, leading to higher levels of albumin. This condition can result from various factors such as excessive sweating, vomiting, diarrhea, or inadequate fluid intake. Dehydration reduces the plasma volume, thereby increasing the concentration of albumin and other proteins in the blood. Proper hydration is essential to maintain normal albumin levels and overall health.
2. High Protein Diet
A high protein diet can also lead to elevated albumin levels. Consuming large amounts of protein increases the synthesis of albumin in the liver, as the body attempts to process and utilize the excess protein intake. This dietary habit is often seen in individuals aiming to build muscle mass or those following specific dietary regimens for health reasons. However, it is important to balance protein intake to avoid potential negative effects on kidney function and overall health. Studies have shown that dietary protein directly stimulates albumin synthesis, which can lead to increased serum albumin levels.
3. Certain Medications such as Steroids and Insulin
Certain medications, including steroids and insulin, can cause an increase in albumin levels. Steroids, for instance, can enhance the synthesis of albumin in the liver, leading to higher serum levels. Insulin, on the other hand, can affect albumin metabolism and distribution within the body. These medications are often prescribed for various medical conditions, and their impact on albumin levels should be monitored to ensure they do not lead to adverse effects. The use of these medications can significantly alter albumin levels, necessitating careful management and monitoring.
4. Liver Conditions
Liver conditions can also contribute to elevated albumin levels. The liver is responsible for the synthesis of albumin, and certain liver diseases can lead to an overproduction of this protein. Conditions such as hepatitis, cirrhosis, and liver tumors can disrupt normal liver function, resulting in abnormal albumin levels. Monitoring liver function and managing underlying liver conditions are crucial to maintaining normal albumin levels and overall health. Elevated serum levels of glycated albumin have been associated with liver conditions and can serve as an indicator of liver health.
Albumin Levels and Health Implications
Abnormal levels of albumin, whether high or low, can be indicative of various health conditions and warrant a closer examination of an individual’s overall health. Here is a list of health implications associated with differing albumin levels:
1. Normal Albumin Levels
Normal albumin levels, typically ranging from 3.5 to 4.5 g/dL, are crucial for maintaining various physiological functions, including maintaining oncotic pressure, transporting hormones, vitamins, and drugs, and providing antioxidant properties. In a study involving 30,732 hospitalized patients, 65% had normal albumin levels on admission, which was associated with the lowest in-hospital mortality rate of 2% and a long-term mortality rate of 29%. Normal albumin levels are indicative of good nutritional status and effective liver function, and they play a significant role in overall health and recovery from illnesses.
2. Low Albumin Levels (Hypoalbuminemia) and Its Consequences
Low Albumin Levels, defined as albumin levels below 3.5 g/dL, is associated with various adverse health outcomes. It is a potent predictor of mortality in patients with chronic diseases such as end-stage renal disease and heart failure. Hypoalbuminemia can result from malnutrition, inflammation, or increased albumin loss, as seen in conditions like nephrotic syndrome and continuous ambulatory peritoneal dialysis. It is linked to poor prognosis, increased risk of infections, prolonged hospital stays, and higher healthcare costs. In hospitalized patients, hypoalbuminemia on admission significantly increases both short- and long-term mortality rates.
3. High Albumin Levels (Hyperalbuminemia) and Its Consequences
High Albumin Levels, defined as albumin levels above 4.5 g/dL, is relatively rare and often less studied compared to hypoalbuminemia. In the cohort study of hospitalized patients, only 6% had hyperalbuminemia on admission, which was associated with the lowest in-hospital mortality rate of 0.3% and the best short- and long-term survival rates. While hyperalbuminemia is generally considered benign, it can sometimes indicate dehydration or be a marker of other underlying conditions. However, the study suggests that patients with hyperalbuminemia tend to have better overall health outcomes compared to those with hypoalbuminemia or even normal albumin levels.
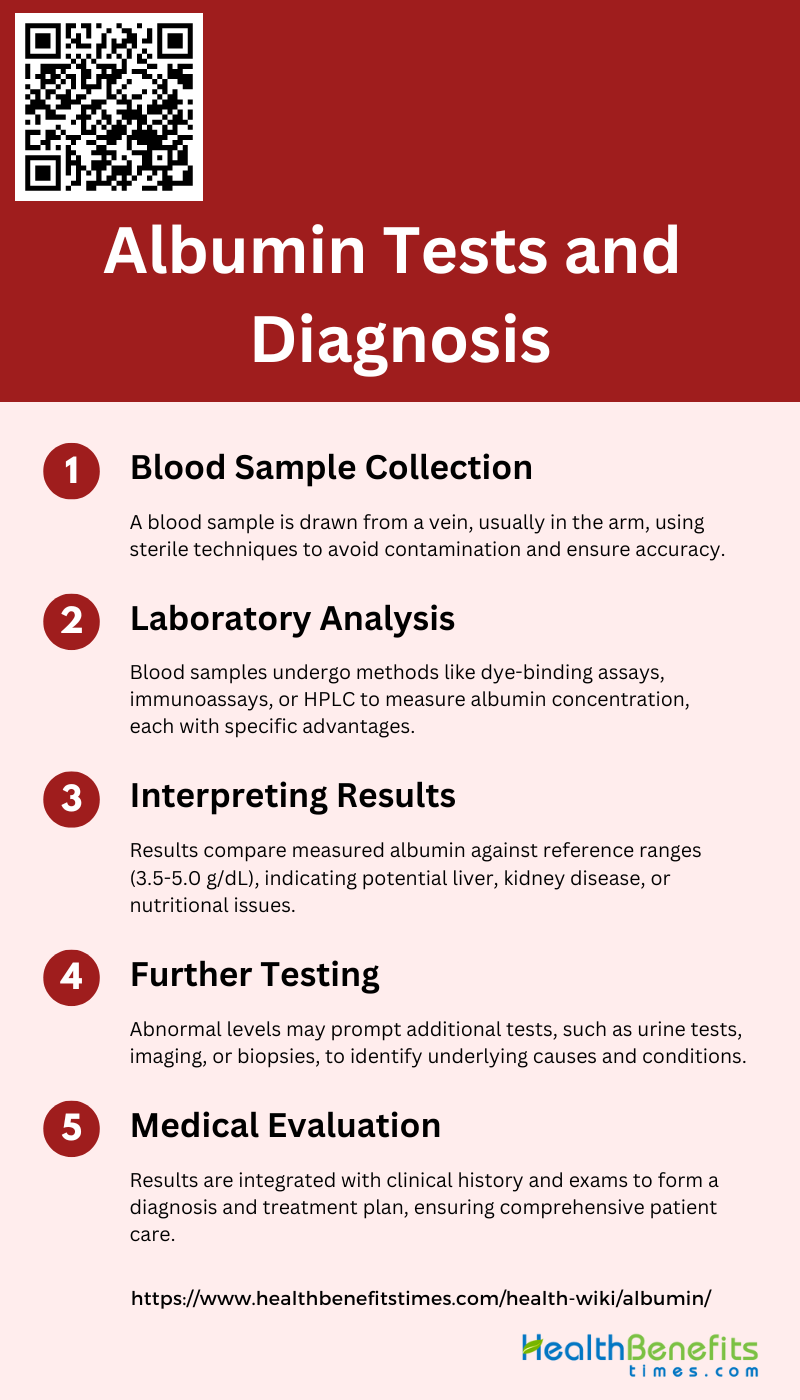
Albumin Tests and Diagnosis
Albumin tests are essential diagnostic tools used to assess the protein levels in the blood, providing valuable insights into a patient’s liver function and nutritional status. These tests are often employed when doctors suspect issues such as kidney disease, liver disease, or malnutrition. Below is a list of key points to consider regarding albumin tests and diagnosis.
1. Blood Sample Collection
Blood sample collection for albumin testing involves drawing a small amount of blood from a vein, typically in the arm. This procedure is usually performed by a healthcare professional using a sterile needle and syringe or a vacuum-sealed collection tube. Proper technique and hygiene are crucial to avoid contamination and ensure accurate results. The collected blood is then labeled and sent to the laboratory for analysis. This step is essential for diagnosing various conditions, including liver disease, kidney disease, and nutritional status, as albumin levels in the blood can provide significant diagnostic information.
2. Laboratory Analysis
In the laboratory, the blood sample undergoes several processes to measure the albumin concentration. Various methods can be employed, such as dye-binding assays, immunoassays, and high-performance liquid chromatography (HPLC). Each method has its advantages and limitations. For instance, dye-binding assays are simple and cost-effective but may lack sensitivity, while immunoassays, such as enzyme-linked immunosorbent assay (ELISA) and radioimmunoassay (RIA), offer higher sensitivity and specificity. The choice of method depends on the required accuracy, available resources, and specific clinical context.
3. Interpreting Results
Interpreting albumin test results involves comparing the measured albumin concentration against standard reference ranges. Normal serum albumin levels typically range from 3.5 to 5.0 g/dL. Deviations from this range can indicate various health issues. Low albumin levels may suggest liver disease, kidney disease, malnutrition, or chronic inflammation, while high levels are less common but can occur in dehydration or high-protein diets. It is crucial to consider the patient’s overall clinical picture, including symptoms and other laboratory findings, to make an accurate diagnosis.
4. Further Testing
If abnormal albumin levels are detected, further testing may be necessary to pinpoint the underlying cause. This could include additional blood tests, urine tests, imaging studies, or biopsies. For instance, urine albumin tests, such as the albumin-to-creatinine ratio (ACR), can help assess kidney function and detect early signs of kidney disease. Advanced techniques like electron spin resonance (ESR) spectroscopy can also be used to monitor structural changes in albumin, providing insights into conditions like cancer. These follow-up tests are essential for a comprehensive evaluation and appropriate management of the patient’s condition.
5. Medical Evaluation
A thorough medical evaluation is necessary to integrate the albumin test results with the patient’s clinical history, physical examination, and other diagnostic findings. This evaluation helps in forming a differential diagnosis and developing a treatment plan. For example, in patients with diabetes or hypertension, regular monitoring of albumin levels can aid in early detection and management of kidney disease. In cases of suspected liver disease, additional liver function tests and imaging studies may be warranted. The goal is to provide a holistic approach to patient care, ensuring timely and effective interventions.
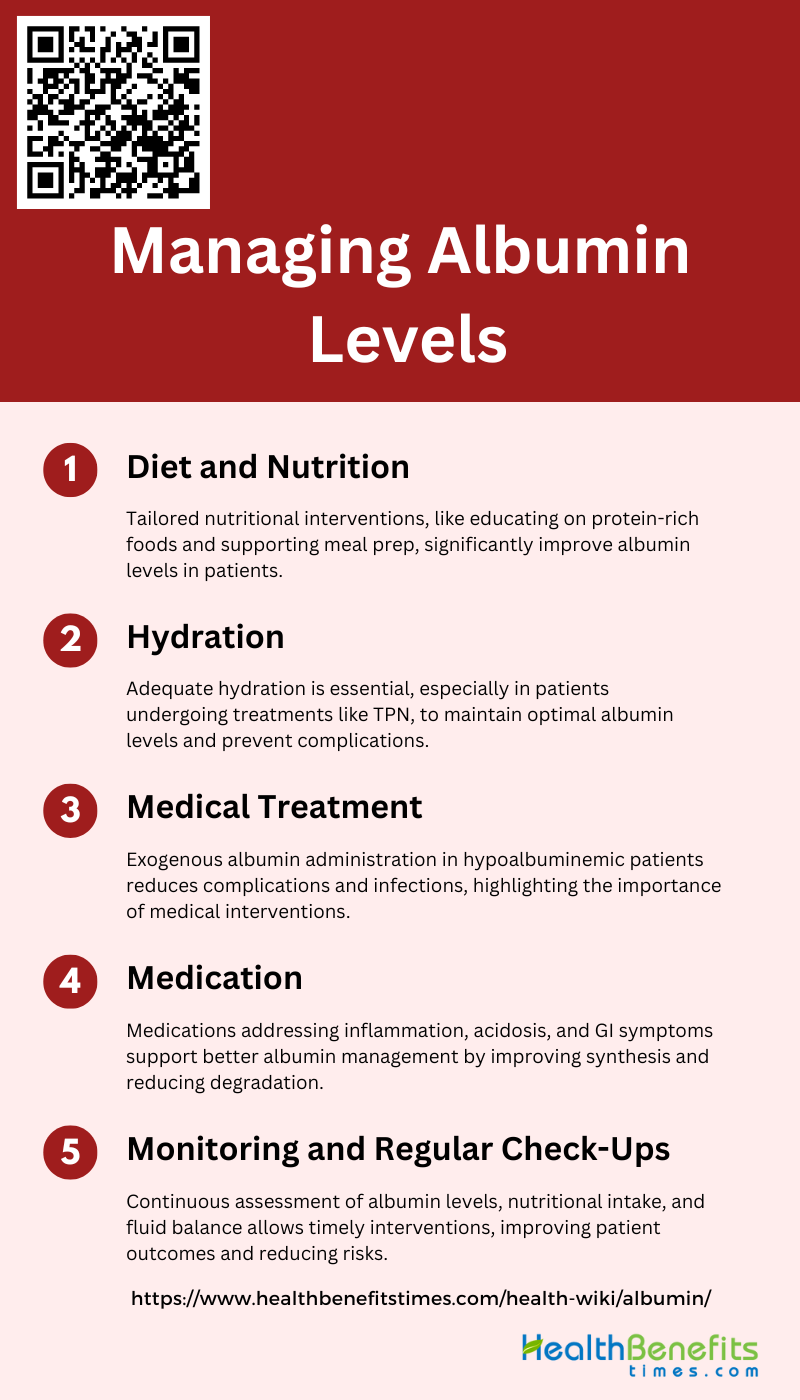
Managing Albumin Levels
Managing albumin levels involves addressing underlying health conditions and implementing lifestyle changes to maintain optimal protein balance. Key strategies include:
1. Diet and Nutrition
Diet and nutrition play a crucial role in managing albumin levels, particularly in patients undergoing treatments such as hemodialysis. Tailored nutritional interventions that address specific barriers, such as poor knowledge of protein-containing foods, poor appetite, and difficulty swallowing, have been shown to improve albumin levels significantly. For instance, a study involving hemodialysis patients demonstrated that targeted nutritional interventions led to greater increases in albumin levels and energy intake compared to usual care. These interventions often include educating patients on protein-rich foods, recommending suitable snacks, and providing support for shopping and cooking, which collectively contribute to better nutritional status and higher albumin levels.
2. Hydration
Proper hydration is essential for maintaining optimal albumin levels, especially in patients receiving treatments like total parenteral nutrition (TPN). Fluid balance is a critical factor monitored in patients undergoing TPN, as it can influence serum albumin concentrations. In cancer patients receiving TPN, maintaining an appropriate fluid balance was part of the monitoring process to assess changes in serum albumin levels. Ensuring adequate hydration helps in preventing complications such as dehydration, which can adversely affect albumin levels and overall health outcomes.
3. Medical Treatment
Medical treatments, including the administration of exogenous albumin, can significantly impact albumin levels in patients. Studies have shown that hypoalbuminemic patients receiving central TPN with normal serum albumin supplementation experienced fewer hospital complications and infections compared to those who did not receive albumin supplementation. Similarly, cancer patients receiving at least 25 grams of exogenous albumin during TPN showed a significant elevation in serum albumin levels, highlighting the importance of medical interventions in managing albumin levels effectively.
4. Medication
Medications can also play a role in managing albumin levels, particularly in addressing underlying conditions that contribute to hypoalbuminemia. For example, addressing inflammation and other medical conditions that affect albumin synthesis and degradation can help improve albumin levels. Although the relationship between inflammatory markers and albumin levels was not significant in some studies, managing conditions like acidosis and gastrointestinal symptoms through appropriate medications can support better albumin management. Tailoring medication regimens to address these underlying issues is crucial for maintaining optimal albumin levels.
5. Monitoring and Regular Check-Ups
Regular monitoring and check-ups are vital for managing albumin levels effectively. Continuous assessment of serum albumin concentrations, nutritional intake, and fluid balance allows for timely interventions and adjustments in treatment plans. For instance, in studies involving hemodialysis and TPN patients, regular monitoring of albumin levels and other health parameters was essential for evaluating the effectiveness of interventions and making necessary adjustments. Regular check-ups ensure that any deviations in albumin levels are promptly addressed, thereby reducing the risk of complications and improving patient outcomes.
Albumin Supplements and Therapies
Albumin supplements and therapies are used to manage low albumin levels, addressing various health conditions and improving patient outcomes. Key aspects include:
1. Intravenous Albumin
Intravenous albumin therapy has shown promise in the treatment of various conditions, including Alzheimer’s disease (AD). The AMBAR (Alzheimer Management By Albumin Replacement) study explores the use of Albutein(therapeutic albumin) in combination with intravenous immunoglobulin (IVIG) to reduce beta-amyloid peptide (Aβ) burden in the brain. Preliminary research indicates that Albutein has Aβ binding capacity and can mobilize Aβ, leading to cognitive improvements in AD patients. The study confirms that therapeutic apheresis to replace endogenous albumin with Albutein® 5% is both feasible and safe, offering a new therapeutic perspective for AD treatment.
2. Nutritional Support
Albumin is a critical protein in the human body, playing a significant role in maintaining oncotic pressure and serving as a carrier for various substances. Nutritional support involving albumin supplementation can be crucial for patients with hypoalbuminemia, often seen in chronic illnesses and malnutrition. By providing albumin through dietary means or supplements, patients can experience improved nutritional status, better wound healing, and enhanced overall recovery. This approach is particularly beneficial in clinical settings where maintaining adequate protein levels is essential for patient outcomes.
3. Monitoring and Adjustment
Effective use of albumin supplements and therapies requires careful monitoring and adjustment to ensure optimal outcomes. Regular assessment of albumin levels in the blood can help healthcare providers tailor the dosage and frequency of albumin administration to meet individual patient needs. This is especially important in conditions like AD, where the therapeutic goal is to reduce Aβ burden while avoiding potential side effects. Monitoring also allows for timely adjustments in therapy, ensuring that patients receive the maximum benefit from albumin supplementation.
4. Combination Therapies
Combination therapies involving albumin have shown potential in enhancing treatment efficacy for various diseases. The AMBAR study, for instance, combines therapeutic apheresis with Albutein and IVIG to treat AD. This approach leverages the Aβ binding capacity of Albutein and the immunomodulatory effects of IVIG, resulting in cognitive, functional, and behavioral improvements in patients. Such combination therapies can offer synergistic benefits, making them a promising avenue for future research and clinical application.
5. Parenteral Nutrition
Parenteral nutrition, which involves the intravenous administration of nutrients, can be vital for patients who cannot obtain adequate nutrition through oral or enteral routes. Albumin is often included in parenteral nutrition formulations to help maintain plasma volume and oncotic pressure. This is particularly important in critically ill patients or those with severe malnutrition. By incorporating albumin into parenteral nutrition, healthcare providers can ensure that patients receive the necessary protein support to aid in recovery and improve clinical outcomes.