Akinesia is a medical condition characterized by the inability to voluntarily move one’s muscles, often resulting in a “frozen” state where the body feels rigid and immobile. It is most commonly associated with advanced Parkinson’s disease due to the degeneration of dopaminergic neurons, but it can also occur in other conditions such as hypothyroidism, medication-induced Parkinson-like symptoms, and fetal akinesia deformation sequence (FADS). Akinesia can manifest as delayed movement initiation, freezing mid-action, or complete cessation of movement, and is often accompanied by symptoms like muscle rigidity, tremors, and postural instability. Treatment typically focuses on addressing the underlying cause, such as increasing dopamine levels in Parkinson’s disease or managing thyroid hormone levels in hypothyroidism.
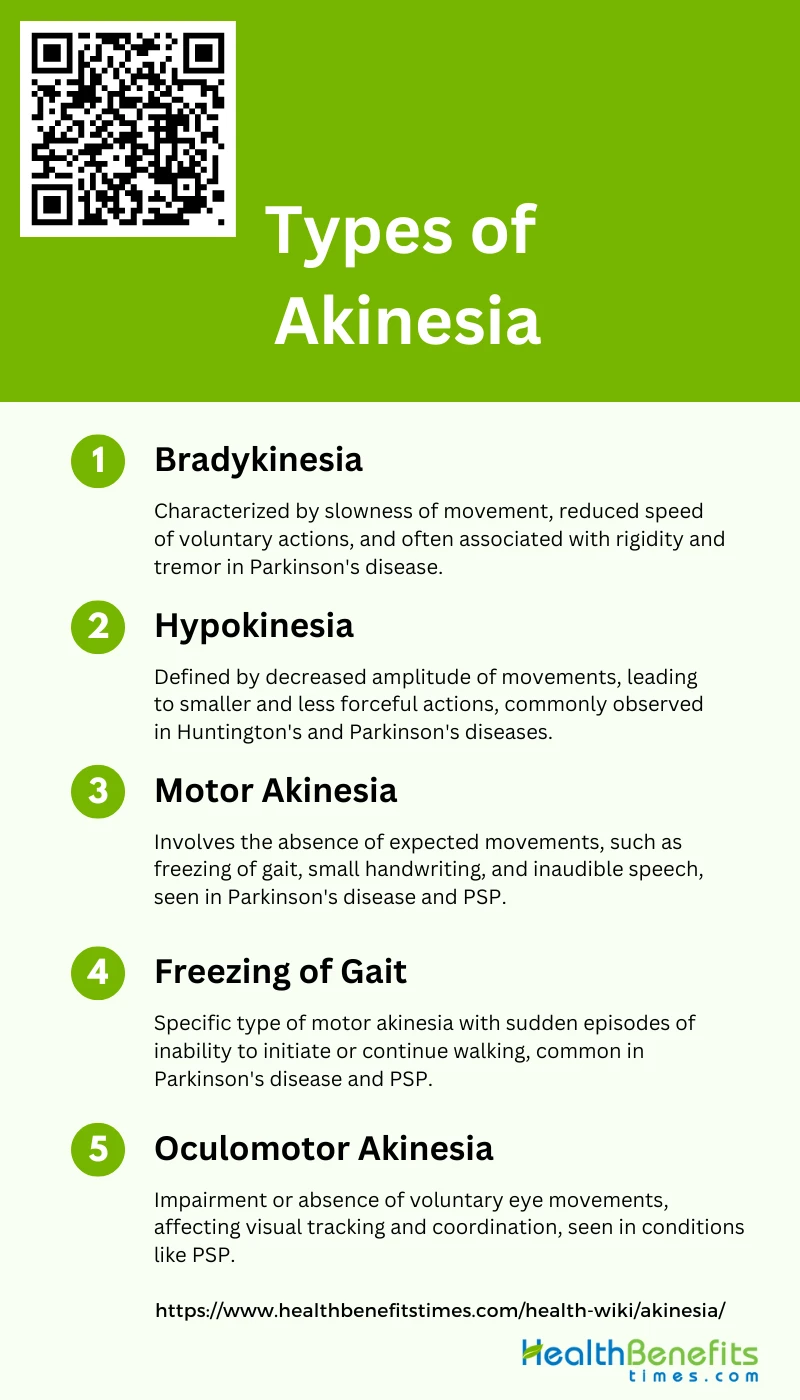
Types of Akinesia
Akinesia refers to a loss or impairment of voluntary movement. It’s often associated with various neurological disorders, particularly Parkinson’s disease. Here are some types of akinesia:
1. Bradykinesia
Bradykinesia, a hallmark of Parkinson’s disease, refers to the slowness of movement and is a complex phenomenon with multiple components. It is often accompanied by rigidity and tremor at rest, although these symptoms may not always impair movement. Bradykinesia itself is characterized by a reduction in the speed of voluntary movements, making everyday tasks challenging for patients. This condition is primarily dopamine-responsive, but some aspects may not respond to dopamine therapy. The concept of bradykinesia also includes slow reaction times, as movements do not occur when expected.
2. Hypokinesia
Hypokinesia is defined as a decrease in the amplitude of movement, resulting in smaller and less forceful movements. This condition is often observed in patients with Huntington’s disease and Parkinson’s disease. In Huntington’s disease, hypokinesia manifests as a reduction in stride length and joint ankle range during gait, contributing to gait disturbances. Unlike bradykinesia, which primarily affects the speed of movement, hypokinesia affects the size and extent of movements, leading to a more restricted range of motion
3. Motor Akinesia
Motor akinesia refers to the absence of expected movement and is often seen in patients with Parkinson’s disease and progressive supranuclear palsy (PSP). This condition can manifest as freezing of gait, micrographia (small handwriting), and inaudible speech. Motor akinesia is distinct from bradykinesia and hypokinesia, as it involves a complete lack of movement rather than just slowness or reduced amplitude. The underlying pathology often involves the striatal dopaminergic system, but other brain regions, such as the frontal lobe, may also be implicated.
4. Freezing of Gait
Freezing of gait (FOG) is a specific type of motor akinesia characterized by sudden, brief episodes where patients are unable to initiate or continue walking. This phenomenon is commonly associated with Parkinson’s disease and PSP. Patients with FOG often experience difficulty in starting to walk, turning, or navigating through narrow spaces. The condition is particularly debilitating as it increases the risk of falls and significantly impacts the quality of life. FOG is often resistant to conventional dopaminergic treatments, indicating a complex underlying pathology.
5. Oculomotor Akinesia
Oculomotor akinesia involves the impairment or absence of voluntary eye movements, often seen in conditions like PSP. Patients with this type of akinesia may have difficulty initiating saccades (rapid eye movements) or may exhibit a complete lack of eye movement. This condition can severely affect visual tracking and coordination, making daily activities challenging. Oculomotor akinesia is often accompanied by other motor symptoms, such as freezing of gait and speech difficulties, further complicating the clinical picture.
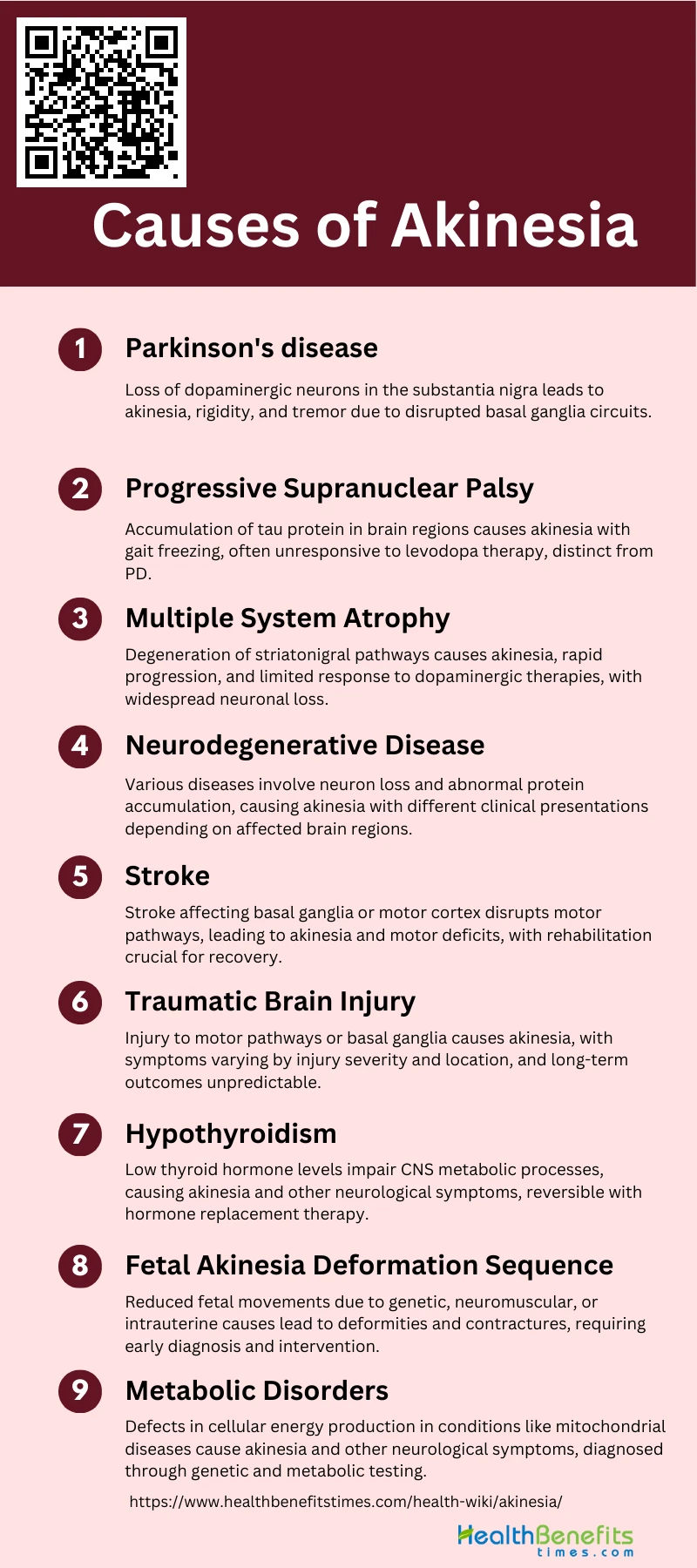
Causes of Akinesia
It is the inability to initiate voluntary movement, can be caused by various conditions affecting the central nervous system. Here are some of the main causes of akinesia:
1. Parkinson’s Disease
Parkinson’s Disease (PD) is a neurodegenerative disorder characterized by the loss of dopaminergic neurons in the substantia nigra. Akinesia, or the inability to initiate movement, is a hallmark symptom of PD. It is often accompanied by other motor symptoms such as rigidity and tremor. The pathophysiology of akinesia in PD is primarily linked to striatal dopamine deficiency, which disrupts the normal functioning of the basal ganglia circuits responsible for movement initiation and control.
2. Progressive Supranuclear Palsy
Progressive Supranuclear Palsy (PSP) is a rare neurodegenerative disease that often presents with akinesia. Unlike Parkinson’s Disease, PSP is characterized by the accumulation of tau protein in the brain, particularly affecting the substantia nigra, subthalamic nucleus, and globus pallidus. Patients with PSP may exhibit “pure akinesia” without rigidity or tremor, and this condition is often unresponsive to levodopa therapy. Pathological studies have confirmed that PSP can manifest as pure akinesia with gait freezing, making it a distinct clinical phenotype.
3. Multiple System Atrophy
Multiple System Atrophy (MSA) is another neurodegenerative disorder that can cause akinesia. MSA is characterized by a combination of parkinsonian, cerebellar, and autonomic symptoms. The parkinsonian features, including akinesia, are due to the degeneration of striatonigral pathways. Unlike PD, MSA often progresses more rapidly and is less responsive to dopaminergic therapies. Pathological findings in MSA include glial cytoplasmic inclusions and widespread neuronal loss in the basal ganglia, cerebellum, and brainstem.
4. Neurodegenerative Disease
N Conditions often involve the progressive loss of neurons and the accumulation of abnormal proteins such as tau or alpha-synuclein. The specific regions of the brain affected and the type of protein accumulation can vary, leading to different clinical presentations. For example, Hallervorden-Spatz disease, a form of neurodegeneration with brain iron accumulation, can present with severe akinesia.
5. Stroke
Stroke, particularly when it affects the basal ganglia or motor cortex, can lead to akinesia. The sudden loss of blood supply to these areas results in neuronal death and disruption of motor pathways. Depending on the location and extent of the stroke, patients may experience varying degrees of akinesia, often accompanied by other motor deficits such as hemiparesis or spasticity. Rehabilitation and physical therapy are crucial for recovery, although some deficits may be permanent.
6. Traumatic Brain Injury
Traumatic Brain Injury (TBI) can cause akinesia if the injury affects the motor pathways or basal ganglia. The mechanism involves direct damage to neurons, axonal injury, and secondary inflammatory responses that disrupt normal brain function. Patients with TBI may exhibit a range of motor symptoms, including akinesia, depending on the severity and location of the injury. Long-term outcomes vary, and some patients may experience persistent motor deficits.
7. Hypothyroidism
Hypothyroidism, a condition characterized by low levels of thyroid hormone, can lead to a range of neurological symptoms, including akinesia. The exact mechanism is not well understood, but it is believed that thyroid hormone deficiency affects the central nervous system’s metabolic processes, leading to slowed neural conduction and impaired motor function. Treatment with thyroid hormone replacement can often reverse these symptoms.
8. Fetal Akinesia Deformation Sequence
Fetal Akinesia Deformation Sequence (FADS) is a condition that occurs in utero and is characterized by reduced fetal movements, leading to a range of deformities and contractures. The causes of FADS are varied and can include genetic mutations, neuromuscular disorders, and intrauterine constraints. The lack of movement in the fetus can result in joint contractures, facial anomalies, and pulmonary hypoplasia. Early diagnosis and intervention are crucial for managing the condition.
9. Metabolic Disorders
Metabolic disorders, such as mitochondrial diseases and certain inborn errors of metabolism, can lead to akinesia. These conditions often involve defects in cellular energy production, leading to impaired function of neurons and muscle cells. The resulting energy deficit can cause a range of neurological symptoms, including akinesia. Diagnosis often involves genetic testing and metabolic screening, and treatment may include dietary modifications and supportive therapies.
Sign and Symptoms of Akinesia
Here are some common signs and symptoms of akinesia:
1. Delayed Response
Delayed response in akinesia is characterized by a significant lag in initiating voluntary movements. This delay is often due to the failure of the motor cortex to activate promptly, which can be studied through reaction time evaluations. Patients with Parkinson’s disease, for instance, exhibit prolonged simple reaction times while their choice reaction times remain normal, indicating that the delay is not due to cognitive slowness but rather the time required to execute a motor program. This phenomenon is also observed in patients with rest tremor, who must wait for a tremor beat in the agonist muscle to initiate movement.
2. Freezing of Muscles
Freezing of muscles, particularly during repetitive voluntary movements, is a hallmark of akinesia. This symptom is often unresponsive to L-dopa therapy and is characterized by a sudden inability to move, commonly seen in gait, handwriting, and speech. The freezing phenomenon can be triggered by the hastening of repetitive movements, leading to a breakdown in motor function. This symptom is particularly prevalent in conditions like progressive supranuclear palsy (PSP), where it is associated with a specific pattern of striatal dopamine transporter loss.
3. Inability to Execute Multiple Actions at Once
Patients with akinesia often struggle to perform multiple actions simultaneously due to the impaired coordination of motor programs. This difficulty is linked to basal ganglia lesions, which disrupt the execution of learned automatic series of movements. The inability to multitask is exacerbated by the slowness and awkwardness of coordinated movements, making it challenging for patients to engage in complex motor activities. This symptom is also evident in the reduced ability to perform repetitive gestures smoothly, further complicating multitasking.
4. Complete Abolition of Movement
Complete abolition of movement, or severe akinesia, is observed in advanced stages of Parkinson’s disease and other neurodegenerative disorders. This condition is marked by an absolute inability to initiate any voluntary movement, often due to extensive striatal dopamine deficiency. In some cases, this severe form of akinesia is unresponsive to conventional treatments like L-dopa, indicating a different underlying pathology from typical Parkinson’s disease. The complete lack of movement can also be seen in patients with PSP, where it is associated with significant tau pathology.
5. Reduced Facial Expressions
Reduced facial expressions, or hypomimia, is a common symptom of akinesia, particularly in Parkinson’s disease. This symptom results from the slowness and poverty of facial muscle movements, leading to a mask-like appearance. The lack of spontaneous facial movements, such as blinking and smiling, is due to the impaired motor control of the facial muscles, which is often linked to basal ganglia dysfunction. This reduction in facial expressiveness can significantly impact social interactions and the overall quality of life for patients.
6. Slowness of Voluntary Movements
Slowness of voluntary movements, or bradykinesia, is a defining feature of akinesia. This symptom involves a marked reduction in the speed and amplitude of voluntary movements, making everyday tasks laborious and time-consuming. The slowness is attributed to the failure to energize muscles adequately, resulting in prolonged movement execution times. Bradykinesia is often accompanied by other motor symptoms such as rigidity and tremor, further complicating the patient’s motor abilities.
7. Postural Instability
Postural instability in akinesia is characterized by an impaired ability to maintain balance and respond to shifts in the center of gravity. This instability often leads to unsteadiness and falls, particularly during walking or standing. The disturbance in postural reactions is linked to basal ganglia lesions, which affect the body’s ability to anticipate and adjust to postural changes. This symptom is also prevalent in PSP, where it is associated with a specific pattern of neuronal loss in the substantia nigra and globus pallidus.
8. Freezing Episodes, Especially During Walking
Freezing episodes, especially during walking, are a common and debilitating symptom of akinesia. These episodes involve sudden, transient inability to move, often triggered by changes in walking pace or direction. Freezing of gait is particularly challenging as it increases the risk of falls and significantly impairs mobility. This symptom is often unresponsive to L-dopa therapy and is associated with specific neurodegenerative conditions like PSP, where it reflects a distinct pattern of striatal dopamine transporter loss.
Complications of Akinesia
The complications of akinesia can be severe and varied, depending on the underlying cause and the patient’s condition. Here are some of the key complications:
- Having blurred vision
- Loss of vision
- Unable to move eyes quickly
- Unable to look up and down easily
- Unable to keep eye contact for very long
- Difficulty in swallowing
- Symptoms of depression-like mood swings
Treatment and Management of Akinesia
Effective treatment and management are pivotal to improving patient quality of life. Below is a list of strategies and therapies currently employed to combat this condition:
1. Medications
Medications play a crucial role in managing akinesia, particularly in Parkinson’s disease (PD) and related disorders. Levodopa is commonly used, although its effectiveness can vary. For instance, in cases of pure akinesia, levodopa may not be effective, and alternative medications like L-threo-3,4-dihydroxy-phenylserine (L-DOPS) have shown some promise. Dopamine receptor agonists such as lergotrile and bromocriptine have also been used successfully in certain cases, particularly when akinesia is related to hypothalamic damage. However, the response to these medications can be inconsistent, and careful monitoring is required to manage side effects and optimize treatment efficacy.
2. Surgical Treatment
Surgical interventions can be considered for patients with akinesia who do not respond adequately to medication. Motor cortex stimulation (MCS) has shown promising results in patients with levodopa-resistant akinesia, leading to significant improvements in motor function and gait. Additionally, procedures like posterior ventral pallidotomy have been attempted, although their success can be variable. These surgical treatments aim to modulate neural circuits involved in motor control, offering an alternative for patients with severe, medication-resistant akinesia.
3. Physiotherapy
Physiotherapy is an essential component of managing akinesia, focusing on improving mobility, strength, and coordination. Techniques such as gait training, balance exercises, and repetitive movement therapy can help mitigate the effects of akinesia. For example, the use of a specially designed walking stick has been shown to improve gait in patients with pure akinesia, enhancing their daily functioning. Physiotherapy can also include the use of assistive devices and tailored exercise programs to address specific motor deficits and improve overall quality of life.
4. Lifestyle Adjustments
Lifestyle adjustments are crucial for managing akinesia, particularly in maintaining independence and reducing the risk of complications. Patients are encouraged to engage in regular physical activity, adopt a balanced diet, and ensure adequate hydration. Environmental modifications, such as removing tripping hazards and installing grab bars, can help prevent falls and injuries. Additionally, establishing routine and using visual or auditory cues can assist in overcoming freezing episodes and improving movement initiation. These adjustments, combined with medical and therapeutic interventions, can significantly enhance the quality of life for individuals with akinesia.
5. Supportive Therapies
Supportive therapies, including occupational therapy, speech therapy, and psychological support, play a vital role in the comprehensive management of akinesia. Occupational therapy focuses on improving daily living skills and adapting tasks to the patient’s abilities. Speech therapy can address communication difficulties and swallowing issues that may arise in akinesia. Psychological support, including counseling and support groups, helps patients and their families cope with the emotional and social challenges associated with the condition. These therapies provide a holistic approach to managing akinesia, addressing both physical and emotional well-being.