Akathisia is a movement disorder characterized by an overwhelming urge to move and a subjective feeling of inner restlessness. It is primarily caused as a side effect of certain medications, particularly antipsychotic drugs used to treat conditions like schizophrenia and bipolar disorder. People with akathisia experience an intense feeling of restlessness and inability to remain still, often leading to repetitive movements such as rocking, pacing, shifting weight from one foot to another, or crossing and uncrossing legs. This uncontrollable urge to move can be extremely distressing and may result in poor medication adherence, exacerbation of psychiatric symptoms, and in severe cases, even suicidal thoughts or aggressive behavior.
Akathisia is a movement disorder characterized by an overwhelming urge to move and a subjective feeling of inner restlessness. It is primarily caused as a side effect of certain medications, particularly antipsychotic drugs used to treat conditions like schizophrenia and bipolar disorder. People with akathisia experience an intense feeling of restlessness and inability to remain still, often leading to repetitive movements such as rocking, pacing, shifting weight from one foot to another, or crossing and uncrossing legs. This uncontrollable urge to move can be extremely distressing and may result in poor medication adherence, exacerbation of psychiatric symptoms, and in severe cases, even suicidal thoughts or aggressive behavior.
How Common Is Akathisia?
The prevalence of akathisia varies widely depending on the type of medication and patient population. For instance, studies have reported that the prevalence of chronic akathisia in patients with schizophrenia ranges from 15% to 35%. Among patients treated with first-generation antipsychotics, the prevalence can be as high as 45%, while it is around 39% for those on clozapine. Additionally, the incidence of acute akathisia with conventional neuroleptics is estimated to be between 20% and 30%. The condition is also noted to be more common in patients on higher doses or combinations of antipsychotic medications.
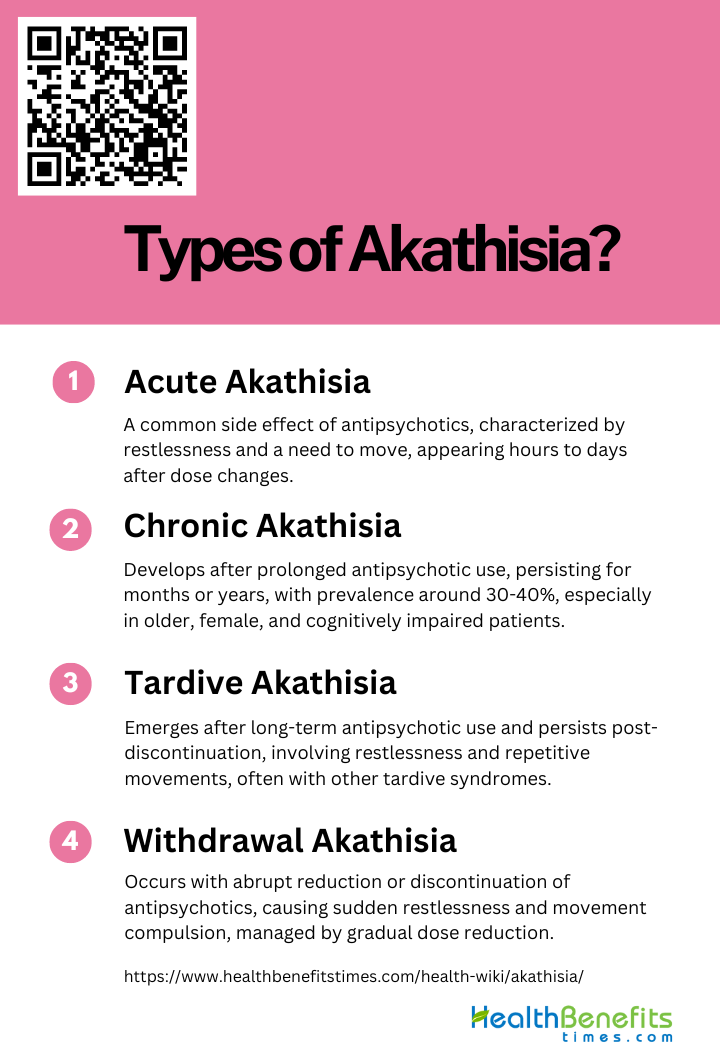
Types of Akathisia
Below are the different types of akathisia that individuals may experience.
1. Acute Akathisia
Acute akathisia is a common and distressing side effect of antipsychotic medications, characterized by an intense feeling of inner restlessness and a compelling need to move. It typically manifests within hours to days of initiating or increasing the dose of antipsychotic drugs. Patients often describe an inability to sit still, accompanied by repetitive movements such as pacing or leg swinging. The condition is particularly challenging to diagnose as it can be mistaken for psychotic agitation or anxiety. Effective management often involves reducing the dose of the offending drug or switching to a different medication, along with the use of anticholinergics or beta-blockers to alleviate symptoms.
2. Chronic Akathisia
Chronic akathisia develops after prolonged exposure to antipsychotic medications and persists for months or even years. Unlike acute akathisia, which appears shortly after drug administration, chronic akathisia is more insidious and can be more challenging to treat. The prevalence of chronic akathisia among patients on long-term antipsychotic therapy is estimated to be around 30-40%. Risk factors include older age, female sex, and the presence of cognitive dysfunction or affective disorders. Treatment strategies are less well-defined compared to acute akathisia, often requiring a combination of pharmacological and non-pharmacological approaches to manage symptoms effectively.
3. Tardive Akathisia
Tardive akathisia is a subtype of akathisia that emerges after long-term use of antipsychotic drugs and persists even after the medication is discontinued. It is often associated with other tardive syndromes such as tardive dyskinesia. The condition is believed to result from neuroadaptive changes in the brain due to prolonged drug exposure. Symptoms include persistent restlessness and repetitive movements, similar to other forms of akathisia, but with a delayed onset. Management is complex and may involve the use of medications like catecholamine depleters, anticholinergics, and clozapine, although treatment outcomes are often unsatisfactory.
4. Withdrawal Akathisia
Withdrawal akathisia occurs when antipsychotic medications are abruptly reduced or discontinued. This form of akathisia is characterized by the sudden onset of restlessness and a compulsion to move, often accompanied by other withdrawal symptoms. The condition can be particularly distressing and may complicate the process of tapering off antipsychotic drugs. Gradual dose reduction is recommended to minimize the risk of withdrawal akathisia. In cases where symptoms do appear, reintroducing the medication at a lower dose and then tapering more slowly can help alleviate the symptoms.
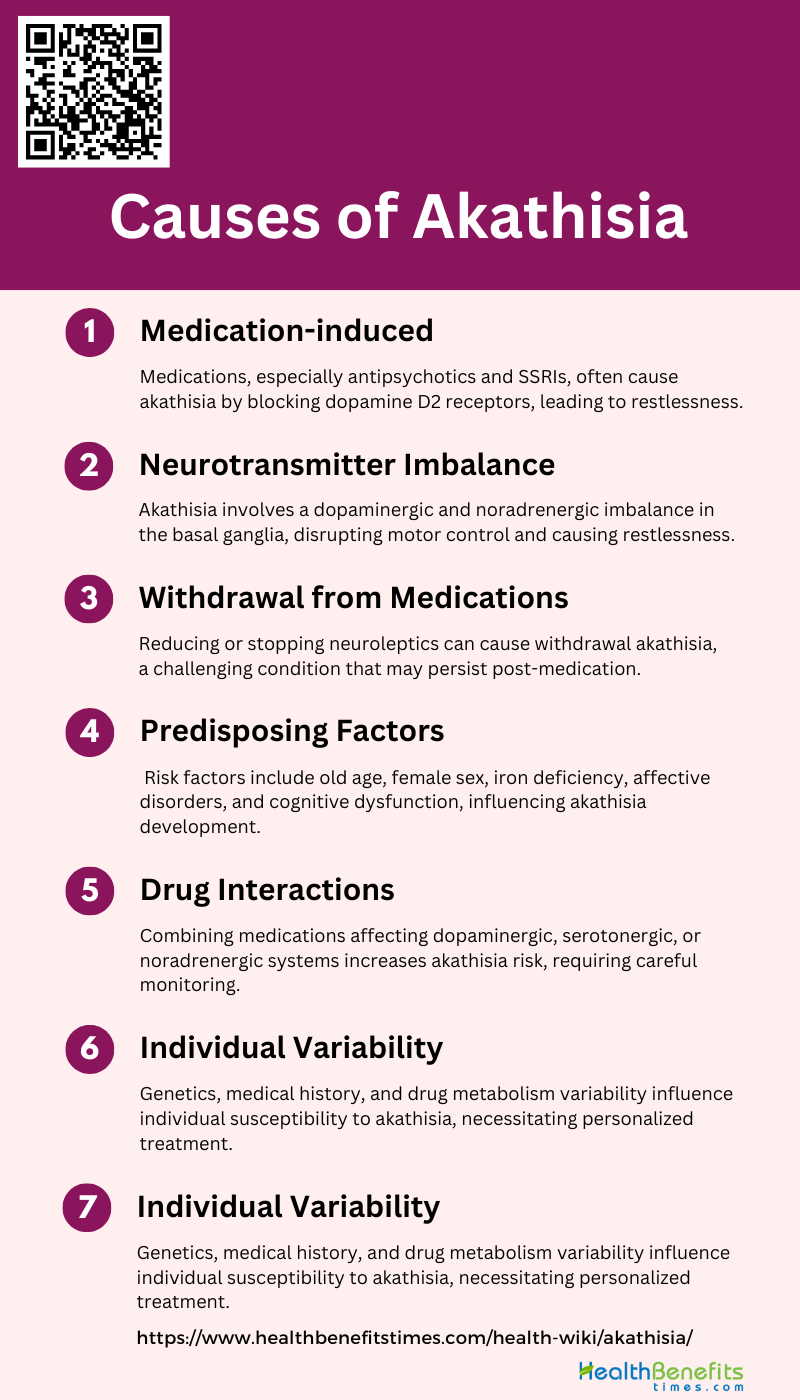
Causes of Akathisia
Below is a list of the primary factors that contribute to the development of akathisia:
1. Medication-induced
These drugs can cause an inner sense of restlessness and an intense urge to move, which are hallmark symptoms of akathisia. The condition is often associated with the blockade of dopamine D2 receptors in the brain, which disrupts normal dopaminergic activity. Studies have shown that both conventional and atypical antipsychotics can induce akathisia, although the incidence may vary. Additionally, other psychotropic medications, including fluoxetine, have been implicated in causing akathisia.
2. Neurotransmitter Imbalance
The pathophysiology of akathisia is believed to involve an imbalance between dopaminergic and noradrenergic neurotransmission in the basal ganglia. This imbalance disrupts normal motor control and leads to the characteristic symptoms of akathisia. Low activity of dopaminergic projections from the midbrain to the ventral striatum has been suggested as a contributing factor. Additionally, serotonergic inhibition of dopaminergic neurotransmission has been proposed as a mechanism, particularly in cases induced by SSRIs. The exact mechanisms remain unclear, but these neurotransmitter imbalances are central to current understanding.
3. Withdrawal from Medications
Withdrawal from medications, particularly neuroleptics, can also lead to akathisia. This form of akathisia, known as withdrawal akathisia, occurs when the causative drug is reduced in dosage or discontinued. The prevalence and risk factors for withdrawal akathisia are not well understood, but it is recognized as a significant issue in patients undergoing changes in their medication regimen. Withdrawal akathisia can be particularly challenging to manage, as it may persist even after the offending drug is stopped.
4. Predisposing Factors
Several predisposing factors may increase the risk of developing akathisia. These include old age, female sex, iron deficiency, and the presence of negative symptoms or cognitive dysfunction. Affective disorders and mental retardation have also been identified as potential risk factors. The role of iron status is particularly noteworthy, as it may interact with dopamine receptors and influence the development of akathisia. However, more research is needed to fully understand these predisposing factors and their contributions.
5. Drug Interactions
Drug interactions can exacerbate the risk of developing akathisia. Combining medications that affect dopaminergic, serotonergic, or noradrenergic systems can increase the likelihood of this condition. For instance, the concurrent use of antipsychotics and SSRIs has been shown to elevate the risk of akathisia. Understanding these interactions is crucial for clinicians to prevent and manage akathisia effectively. Careful monitoring and adjustment of medication regimens can help mitigate these risks.
6. Psychiatric Disorders
Patients with psychiatric disorders, particularly those treated with antipsychotic medications, are at a higher risk of developing akathisia. The condition is commonly seen in individuals with schizophrenia, bipolar disorder, and major depression who are on long-term psychotropic treatment. Akathisia can significantly impact the quality of life and treatment adherence in these patients, making its identification and management a critical aspect of psychiatric care.
7. Individual Variability
There is considerable individual variability in the susceptibility to akathisia. Genetic factors, personal medical history, and individual differences in drug metabolism can all influence the likelihood of developing this condition. Some patients may experience severe symptoms even at low doses of medication, while others may tolerate higher doses without issues. This variability underscores the importance of personalized treatment plans and close monitoring to identify and address akathisia promptly.
Sign and Symptoms of Akathisia
A side effect of certain medications, it presents through a variety of signs and symptoms that can significantly impact an individual’s quality of life. Below is a list detailing the common manifestations of this distressing syndrome.
- Inner Restlessness and Disquiet: Patients often experience a severe feeling of inner disquiet and an inability to sit still or lie quietly.
- Compulsion to Move: There is a frequent need to move, often described as an inability to remain still.
- Motor Restlessness: Symptoms include constant pacing, purposeless movements of the feet and legs, and an intense urge to move around.
- Leg Movements: The legs are most frequently affected, showing movements such as marching in place, crossing and uncrossing, and other stereotyped movements.
- Associated Dysphoria: Patients often report marked symptoms of dysphoria, including tension, panic, irritability, and impatience.
- Suppressible Movements: Associated movements can be suppressible for brief periods.
- Anxiety and Panic: Marked anxiety is a common symptom, often accompanying the motor restlessness.
- Complex Movements: Other complex movements such as trunk rocking, respiratory grunting, moaning, and complex hand movements like face rubbing or scratching may also occur.
- Distress and Behavioral Changes: The condition causes severe distress and can lead to dramatic changes in behavior, which may be misinterpreted as a need for more medication.
- Difficulty in Diagnosis: Akathisia is often subtle and can be overlooked, especially in patients who are unable to communicate their discomfort effectively.
How Is Akathisia Diagnosed?
Doctors assess the patient’s symptoms and movements, evaluate medication use, and rule out other conditions to ensure an accurate diagnosis. Here are the key steps involved in diagnosing akathisia:
1. Clinical Observation
These include a subjective experience of mental unease and an urge to move, which manifests physically as particular patterns of restless movement. The diagnosis is often based on the patient’s description of their symptoms and the clinician’s observation of their behavior. For instance, a study on the clinical characteristics of antipsychotic-induced akathisia in Asian patients with schizophrenia highlighted the importance of clinical observation in identifying akathisia, noting that only 5% of the patients were assessed to have the condition despite the majority receiving anticholinergic agents. Another study emphasized the role of clinical assessments in diagnosing neuroleptic-induced akathisia (NIA), where patients demonstrated higher daytime motor activity, confirming clinical observations that NIA tends to disappear during sleep. Thus, clinical observation remains a fundamental approach in diagnosing akathisia.
2. Barnes Akathisia Rating Scale (BARS)
The Barnes Akathisia Rating Scale (BARS) is a widely used tool for diagnosing and assessing the severity of akathisia. Developed over 15 years ago, BARS has been validated and is extensively used in clinical studies worldwide. The scale includes items for rating observable restless movements, subjective awareness of restlessness, and any associated distress, along with a global severity rating. Studies have shown that BARS is superior to other methods, such as actometry, in screening for DSM-IV diagnosed NIA patients, providing objective validation through movement measuring. The reliability and validity of BARS have been confirmed in various settings, including its Turkish version, which demonstrated high internal consistency and inter-rater reliability. Therefore, BARS is an essential diagnostic tool that offers a structured and reliable method for assessing akathisia.
Treatment and Management of Akathisia
The primary strategies include adjusting the offending medication and incorporating adjunctive treatments. Below are the key treatment options:
1. Medication Adjustments
Adjusting the dosage or switching the antipsychotic medication is often the first step in managing akathisia. High-dose antipsychotic medication, antipsychotic polypharmacy, and rapid increases in dosage should be avoided to prevent akathisia. Switching to antipsychotics with a lower liability for causing akathisia, such as quetiapine or olanzapine, can be beneficial. Dose reduction of the current antipsychotic is also recommended as a primary intervention.
2. Beta Blockers
Beta-blockers, particularly propranolol, are considered a first-line treatment for antipsychotic-induced akathisia. Propranolol has shown efficacy in reducing symptoms of akathisia, although its side effects, such as orthostatic hypotension and bradycardia, may limit its use in some patients. Lipophilic beta-blockers are generally preferred due to their ability to cross the blood-brain barrier more effectively.
3. Benzodiazepines
Benzodiazepines, such as clonazepam, are often used as adjunctive treatments for akathisia. They provide symptomatic relief by reducing anxiety and restlessness associated with the condition. However, the risk of dependence and other side effects should be carefully considered. Studies have shown that benzodiazepines can be effective in reducing symptoms over a short follow-up period.
4. Anticholinergic Medications
Anticholinergic agents are another option for managing akathisia, particularly when other extrapyramidal symptoms are present. These medications work by counteracting the cholinergic activity that may contribute to akathisia. However, their use is often limited to cases where other treatments have failed due to their side effect profile.
5. Botulinum Toxin Injections
Botulinum toxin injections are not commonly used for akathisia but may be considered in refractory cases. The mechanism involves reducing muscle activity and thereby alleviating motor restlessness. However, there is limited evidence supporting its efficacy in treating akathisia specifically, and more research is needed in this area.
6. Counseling and Supportive Therapy
Counseling and supportive therapy play a crucial role in managing akathisia. These interventions help patients cope with the distress and anxiety associated with the condition. Supportive therapy can include cognitive-behavioral techniques, relaxation exercises, and psychoeducation to improve treatment adherence and overall quality of life.
7. Vitamin B6
Vitamin B6 has shown promise as a treatment for neuroleptic-induced akathisia. Studies have demonstrated that high doses of vitamin B6 can significantly improve symptoms of akathisia, possibly due to its effects on various neurotransmitter systems. In comparative studies, vitamin B6 was found to be as effective as propranolol in reducing akathisia symptoms.
8. Low-dose Mirtazapine
Low-dose mirtazapine, a 5-HT2A receptor antagonist, has been identified as a potential treatment for akathisia. It has shown efficacy in reducing symptoms at doses of 7.5 mg or 15 mg once daily. Mirtazapine’s antiserotonergic properties make it a promising option for patients who do not respond to traditional treatments.
9. Patient Education and Support
Educating patients about akathisia and its management is essential for improving treatment outcomes. Patients should be informed about the potential side effects of their medications and the importance of adhering to prescribed treatments. Providing support through regular follow-ups and addressing any concerns can help mitigate the impact of akathisia on their daily lives.
Prevention Strategies for Akathisia
Effective prevention strategies are crucial to mitigate its onset and severity. Here are some key approaches to prevent akathisia:
- Use of Novel Antipsychotics: Second-generation antipsychotics, such as quetiapine and olanzapine, have a lower liability for inducing akathisia compared to first-generation antipsychotics.
- Standardized Titration: Gradual titration of antipsychotic doses can help in minimizing the risk of developing akathisia.
- Dose Reduction: Reducing the dose of the antipsychotic medication can be an effective strategy to prevent the onset of akathisia.
- Switching Medications: Switching to antipsychotics with a lower risk of causing akathisia, such as quetiapine or olanzapine, can be beneficial.
- Adjunctive Medications: Consider prophylactic use of beta-blockers or benzodiazepines in patients with a history of akathisia or those at high risk, under careful medical supervision.
- Avoiding High-Dose and Rapid Titration: Avoiding high doses of antipsychotic medication, antipsychotic polypharmacy, and rapid increases in dosage can help prevent akathisia.
- Monitoring and Early Intervention: Regular monitoring for early signs of akathisia and prompt intervention can prevent the condition from worsening.
- Patient Education: Educating patients about the potential side effects of antipsychotic medications and encouraging them to report symptoms of restlessness early can aid in timely management.