 An agonist is a chemical substance that binds to and activates specific receptors on cells, triggering a biological response. It mimics the actions of naturally occurring molecules like hormones or neurotransmitters. Agonists can be endogenous (produced within the body) or exogenous (introduced from outside, such as drugs). For example, morphine is an exogenous agonist that binds to and activates opioid receptors, producing effects similar to the body’s endogenous opioids like endorphins. Agonists can be full agonists, producing the maximum possible response, or partial agonists, eliciting a reduced response even at full receptor occupancy.
An agonist is a chemical substance that binds to and activates specific receptors on cells, triggering a biological response. It mimics the actions of naturally occurring molecules like hormones or neurotransmitters. Agonists can be endogenous (produced within the body) or exogenous (introduced from outside, such as drugs). For example, morphine is an exogenous agonist that binds to and activates opioid receptors, producing effects similar to the body’s endogenous opioids like endorphins. Agonists can be full agonists, producing the maximum possible response, or partial agonists, eliciting a reduced response even at full receptor occupancy.
Types of Agonists
Below is a list of different types of agonists that illustrate the diversity of their action within the body.
1. Endogenous Agonists
Endogenous agonists are naturally occurring molecules within the body that bind to and activate specific receptors. These molecules are typically hormones, neurotransmitters, or other signaling compounds that play crucial roles in physiological processes. For example, endogenous opioid peptides such as endorphins and enkephalins activate the μ-opioid receptor (MOP), which is involved in pain regulation and reward mechanisms. Similarly, angiotensin II is an endogenous agonist for the angiotensin II type I receptor, which plays a significant role in blood pressure regulation. Understanding the action of endogenous agonists is essential for developing drugs that can mimic or modulate these natural processes.
2. Exogenous Agonists
Exogenous agonists are compounds that originate outside the body and can bind to and activate specific receptors, mimicking the action of endogenous agonists. These can include drugs, toxins, or other synthetic compounds. For instance, synthetic cannabinoids are exogenous agonists that target cannabinoid receptors and have been used both therapeutically and recreationally. Exogenous agonists are often used in medical treatments to replace or enhance the action of endogenous agonists, such as using synthetic opiates to manage pain.
3. Synthetic Agonists
Synthetic agonists are artificially created compounds designed to activate specific receptors. These molecules are often developed to have improved efficacy, selectivity, or safety profiles compared to natural or existing drugs. For example, synthetic cannabinoid receptor agonists (SCRAs) have been developed to explore therapeutic benefits and are now being studied for their biased signaling properties. Another example is the development of selective serotonin 5-HT1A receptor agonists for treating CNS disorders, which show promise due to their functional selectivity and reduced side effects.
4. Irreversible Agonists
Irreversible agonists bind permanently to their target receptors, leading to prolonged activation. This irreversible binding can be advantageous in certain therapeutic contexts but also poses risks of prolonged side effects. For example, some irreversible antagonists, like phenoxybenzamine, have been studied for their ability to inactivate G protein-coupled receptors (GPCRs) irreversibly, which can provide insights into receptor function and spare receptor capacity. The irreversible nature of these interactions necessitates careful consideration in drug design and therapeutic application.
5. Physiological Agonists
Physiological agonists are substances that produce the same physiological response as the endogenous ligand but may not necessarily bind to the same receptor. These agonists can be used to achieve desired therapeutic effects by mimicking the action of natural ligands. For example, in the melanocortin system, agouti-related peptide (AgRP) functions as a physiological antagonist to melanocortin receptors, influencing energy homeostasis and pigmentation. Understanding physiological agonism helps in designing drugs that can effectively mimic or modulate natural physiological processes.
6. Superagonist
Superagonists are compounds that produce a greater maximal response than the endogenous agonist when binding to the same receptor. These molecules can trigger a more substantial receptor-mediated response, which can be beneficial in certain therapeutic contexts. For instance, some ligands targeting GPCRs exhibit superagonism by generating higher receptor signaling output compared to endogenous agonists. This property can be particularly useful in situations where a more robust physiological response is desired, such as in immune modulation or metabolic regulation.
7. Biased Agonist
Biased agonists preferentially activate specific signaling pathways over others when binding to a receptor, leading to distinct physiological outcomes. This selective activation can reduce side effects and improve therapeutic efficacy. For example, biased agonism at the μ-opioid receptor by endogenous opioid peptides can lead to different signaling profiles and physiological effects compared to synthetic opiates. Similarly, biased agonists at cannabinoid receptors are being studied for their potential to maximize therapeutic benefits while minimizing adverse effects. The concept of biased agonism is transforming drug discovery by enabling the design of more targeted and effective therapies.
Therapeutic Applications of Agonists
Below is a list of key therapeutic applications of agonists that highlight their significance in modern healthcare.
1. Antidepressants and Anxiolytics
5-HT1A receptor agonists, such as buspirone and gepirone, have shown promise in treating depressive and anxiety disorders by enhancing serotonin activity in the brain. These agonists act on presynaptic autoreceptors to inhibit serotonin neuron firing and on postsynaptic receptors to attenuate firing activity, leading to anxiolytic and antidepressant effects. However, their clinical efficacy has been limited by pharmacokinetic issues, such as rapid elimination and suboptimal therapeutic responses at low doses. Extended-release formulations have improved compliance and efficacy by allowing once-daily dosing.
2. Migraine Treatment
δ-Opioid receptor agonists have emerged as potential treatments for migraines due to their effectiveness in managing chronic pain without inducing hyperalgesia or having high abuse potential. These agonists also possess anxiolytic and antidepressant properties, making them suitable for treating the multifaceted symptoms of migraines. Studies in mouse models have demonstrated that δ-opioid receptor agonists can inhibit migraine-related hyperalgesia, aversive states, and cortical spreading depression, suggesting their therapeutic potential in human migraine management.
3. Parkinson’s Disease
Selective 5-HT4 agonists, such as mosapride, have been investigated for their ability to improve gastric motility and reduce response fluctuations in Parkinson’s disease (PD) patients. In clinical studies, mosapride significantly shortened gastric emptying time, reduced response fluctuations, and improved motor functions without adverse reactions. These findings suggest that 5-HT4 agonists can be beneficial for PD patients experiencing gastrointestinal motility issues and motor function impairments, providing a novel therapeutic approach for managing PD symptoms.
4. Diabetes and Insulin Sensitization
Glucagon-like peptide-1 (GLP-1) receptor agonists, including exenatide, liraglutide, and dulaglutide, offer a unique approach to diabetes management by mimicking the incretin hormone GLP-1. These agonists enhance insulin secretion, reduce glucagon release, increase satiety, and slow gastric emptying, leading to improved blood glucose control. Additionally, GLP-1 receptor agonists have positive effects on weight, blood pressure, and cholesterol levels, making them effective for patients with type 2 diabetes. Common adverse effects include nausea and vomiting, but once-weekly formulations have improved patient adherence.
5. Gastrointestinal Motility Disorders
Serotonin plays a crucial role in gastrointestinal (GI) motility, with about 95% of the body’s serotonin found in the GI tract. Serotonin agonists, such as 5-HT4 agonists, have been used as prokinetic drugs to treat GI motility disorders. These agents enhance gastric motility and can be beneficial in conditions like irritable bowel syndrome (IBS). The therapeutic potential of serotonin agonists in GI disorders is supported by their direct effects on the gut, rather than central nervous system effects, offering a targeted approach to managing GI motility issues.
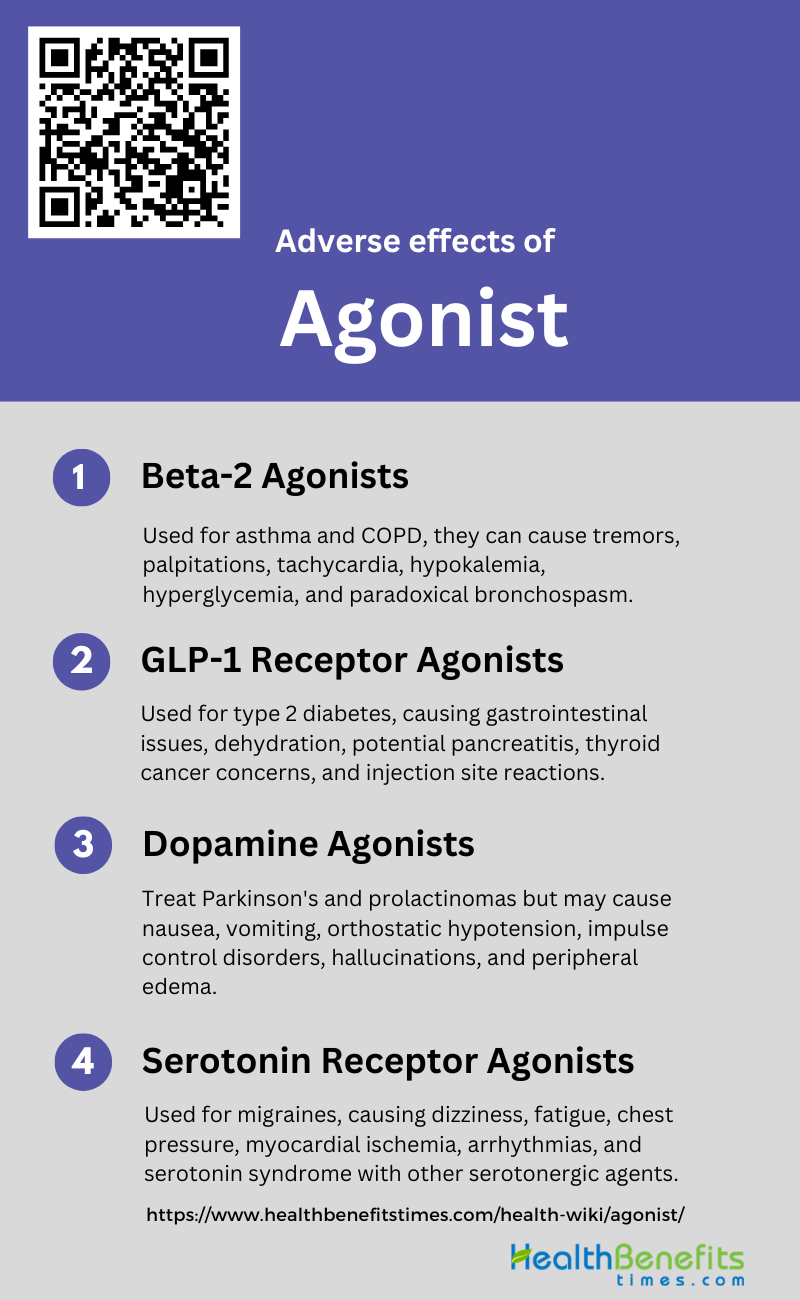
Adverse effects and considerations of agonist
While agonists can be beneficial in therapeutic settings by activating receptors to produce desired effects, it is crucial to consider their potential adverse impacts. These effects can range from mild to severe and may influence treatment outcomes. Below is a list of key considerations and adverse effects associated with the use of agonists.
1. Beta-2 Agonists
Beta-2 agonists are commonly used in the management of asthma and chronic obstructive pulmonary disease (COPD) due to their bronchodilatory effects. However, their use is associated with several adverse effects. These include tremors, palpitations, and tachycardia, which result from the stimulation of beta-2 receptors in skeletal muscles and the cardiovascular system. Additionally, prolonged use can lead to hypokalemia and hyperglycemia, posing risks for patients with diabetes or cardiovascular conditions. There is also a risk of paradoxical bronchospasm, which can exacerbate respiratory symptoms. Careful monitoring and appropriate dosing are essential to minimize these adverse effects.
2. GLP-1 Receptor Agonists
GLP-1 receptor agonists are injectable drugs used to improve glycemic control in patients with type 2 diabetes. While they offer benefits such as weight loss and cardiovascular protection, they are not without adverse effects. Common side effects include gastrointestinal symptoms like nausea, vomiting, and diarrhea, which can lead to dehydration and acute kidney injury. There are also concerns about their potential association with pancreatitis and thyroid cancer, although meta-analyses have not confirmed a direct cause-effect relationship. Injection site reactions, headache, and nasopharyngitis are other reported adverse effects. Despite these issues, GLP-1 receptor agonists generally have a favorable safety profile.
3. Dopamine Agonists
Dopamine agonists are used in the treatment of Parkinson’s disease and prolactinomas. However, their use can lead to several adverse effects. These include nausea, vomiting, and orthostatic hypotension, which are common during the initial stages of treatment. Long-term use has been associated with impulse control disorders such as pathological gambling, hypersexuality, and compulsive shopping. Additionally, patients may experience hallucinations and psychosis, particularly at higher doses. Peripheral edema and erythromelalgia are other less common side effects. Monitoring and dose adjustments are crucial to manage these adverse effects effectively.
4. Serotonin Receptor Agonists
Serotonin receptor agonists, particularly those targeting the 5-HT1 receptor, are used in the treatment of migraines. While effective, they can cause several adverse effects. Common side effects include dizziness, fatigue, and a sensation of tightness or pressure in the chest and throat. More serious but rare adverse effects include myocardial ischemia and arrhythmias, particularly in patients with underlying cardiovascular conditions. Serotonin syndrome, characterized by agitation, confusion, rapid heart rate, and high blood pressure, can occur if these drugs are combined with other serotonergic agents. Careful patient selection and monitoring are essential to mitigate these risks.