An adverse drug reaction (ADR) is an unwanted or harmful reaction that occurs after administration of a drug or medication at normal therapeutic doses. It is a noxious and unintended response to a drug, distinct from intended therapeutic effects. ADRs can range from mild side effects like nausea or rash to severe reactions like organ damage or life-threatening conditions. They can be caused by the drug itself, drug interactions, or individual patient factors like genetics or underlying health conditions. Proper monitoring, reporting, and management of ADRs is crucial to enhance patient safety and optimize drug therapy.
An adverse drug reaction (ADR) is an unwanted or harmful reaction that occurs after administration of a drug or medication at normal therapeutic doses. It is a noxious and unintended response to a drug, distinct from intended therapeutic effects. ADRs can range from mild side effects like nausea or rash to severe reactions like organ damage or life-threatening conditions. They can be caused by the drug itself, drug interactions, or individual patient factors like genetics or underlying health conditions. Proper monitoring, reporting, and management of ADRs is crucial to enhance patient safety and optimize drug therapy.
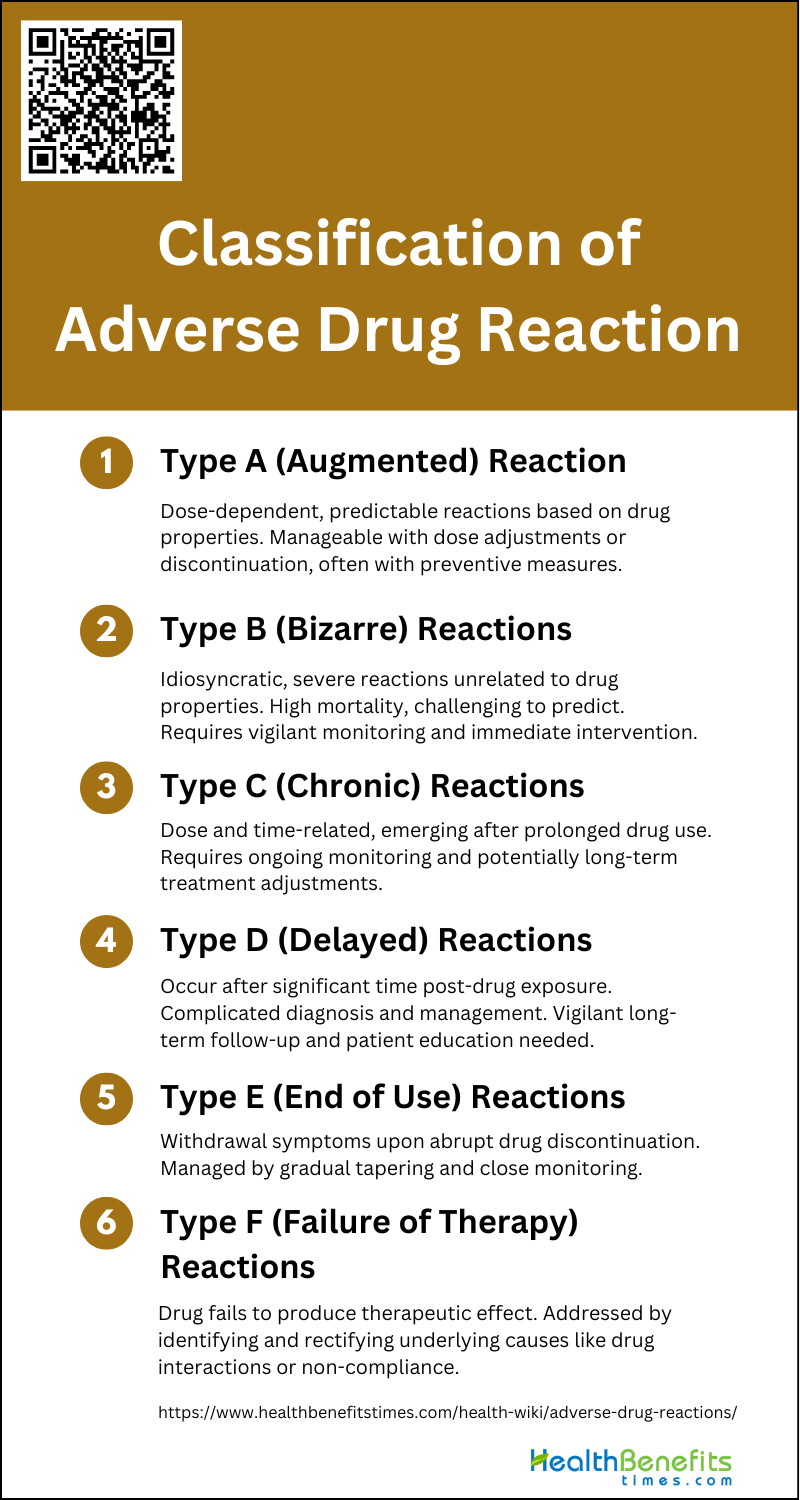
Classification of Adverse Drug Reactions
ADRs are unintended and sometimes harmful outcomes that occur following the administration of a medication. These reactions can range from mild to severe and are categorized based on their nature and causality. Below is a list detailing the various classifications of ADRs.
1. Type A (Augmented) Reactions
Type A (Augmented) reactions are dose-dependent and predictable based on the known pharmacological properties of a drug. These reactions are essentially an exaggeration of the drug’s normal effects and are often related to the dosage administered. For instance, xerostomia following the use of the antimuscarinic agent atropine and prolonged bleeding due to the antiplatelet action of aspirin are classic examples of Type A reactions. These reactions are generally associated with high morbidity but low mortality, making them more manageable through dose adjustments or discontinuation of the drug. The predictability of Type A reactions allows for preventive measures and specific treatments to mitigate their impact.
2. Type B (Bizarre) Reactions
Type B (Bizarre) reactions are idiosyncratic and unpredictable, occurring independently of the drug’s known pharmacological properties. These reactions are often severe and can be life-threatening, with examples including penicillin hypersensitivity and angioedema induced by angiotensin-converting enzyme inhibitors. Unlike Type A reactions, Type B reactions are not dose-dependent and often have an immunological basis, making them difficult to predict and prevent. The incidence of Type B reactions is generally low, but their mortality rate is high, necessitating careful monitoring and immediate intervention when they occur.
3. Type C (Chronic) Reactions
Type C (Chronic) reactions are dose-related and time-related, emerging after prolonged use of a drug. These reactions are often due to the cumulative effect of the drug over time, leading to conditions like tardive dyskinesia from long-term use of antipsychotics or osteoporosis from prolonged corticosteroid therapy. The chronic nature of these reactions makes them more challenging to manage, as they require ongoing monitoring and potentially long-term treatment adjustments. Understanding the pharmacokinetics and pharmacodynamics of the drug can help in predicting and mitigating Type C reactions.
4. Type D (Delayed) Reactions
Type D (Delayed) reactions occur after a significant period following drug exposure, sometimes even after the drug has been discontinued. These reactions can include teratogenic effects, such as birth defects from thalidomide, or carcinogenic effects, like secondary cancers from chemotherapy agents. The delayed onset of these reactions complicates their diagnosis and management, as the temporal gap between drug administration and reaction can obscure the causal relationship. Vigilant long-term follow-up and patient education are crucial in managing Type D reactions.
5. Type E (End of use) Reactions
Type E (End of use) reactions, also known as withdrawal reactions, occur when a drug is abruptly discontinued. These reactions can manifest as withdrawal symptoms, such as rebound hypertension after stopping antihypertensive drugs or withdrawal seizures following the cessation of benzodiazepines. The management of Type E reactions often involves tapering the drug dose gradually to minimize withdrawal symptoms and monitoring the patient closely during the discontinuation process. Understanding the drug’s half-life and the patient’s dependency level is essential for effectively managing these reactions.
6. Type F (Failure of therapy) Reactions
Type F (Failure of therapy) reactions occur when a drug fails to produce the intended therapeutic effect. This can result from various factors, including drug interactions, incorrect dosage, or patient non-compliance. For example, the failure of antibiotics to treat an infection due to bacterial resistance or the ineffectiveness of antihypertensive drugs due to drug-drug interactions is instances of Type F reactions. Addressing Type F reactions involves identifying and rectifying the underlying cause, whether it is adjusting the dosage, switching to an alternative therapy, or improving patient adherence to the treatment regimen.
Causes and Risk Factors of Adverse Drug Reactions
ADRs are unintended and harmful outcomes that occur during appropriate medication use. Understanding the causes and risk factors is crucial for prevention and management. Below is a list of the primary contributors to ADRs.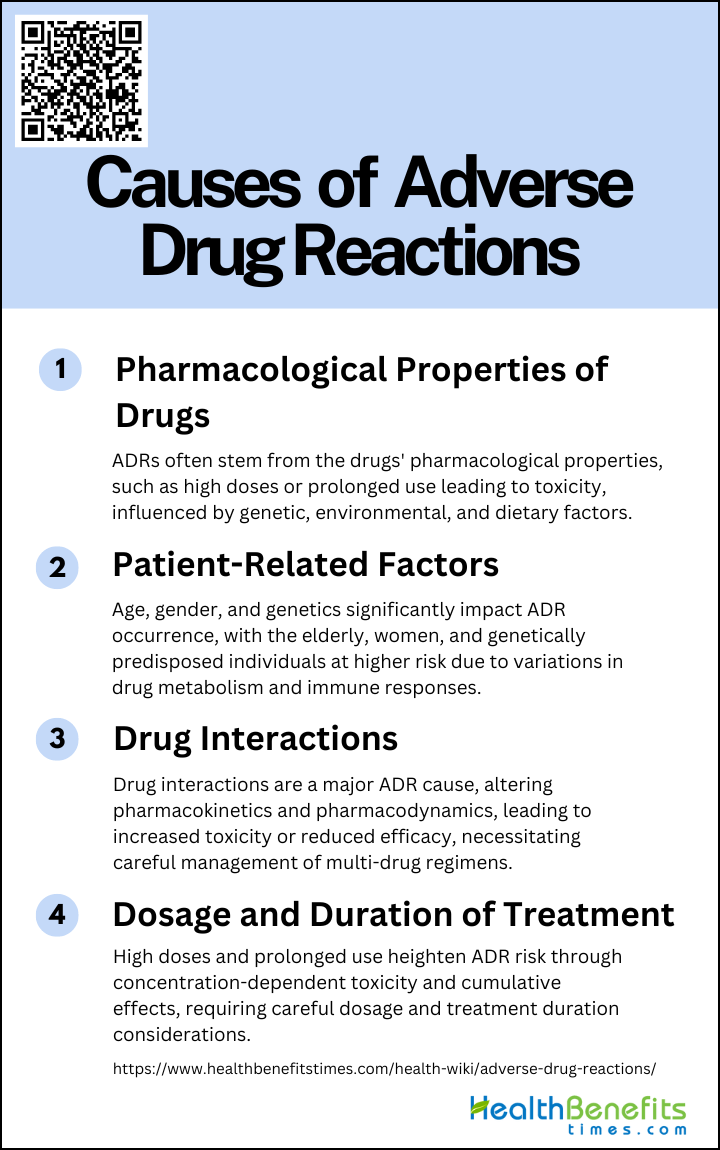
1. Pharmacological Properties of Drugs
These reactions can be concentration-dependent, where high doses or prolonged use of a drug lead to toxic effects. For instance, high plasma concentrations of a drug or its metabolites can enhance primary pharmacological activity or cause new, undesirable secondary effects. Genetic factors, such as inherited impairments in drug metabolism, can also influence these reactions. Additionally, environmental and dietary factors may affect drug metabolizing enzymes, further complicating the pharmacokinetics and pharmacodynamics of drugs.
2. Patient-Related Factors (Age, Gender, Genetics)
Patient-related factors such as age, gender, and genetics significantly influence the occurrence of ADRs. Elderly patients are particularly susceptible due to polypharmacy and age-related changes in drug metabolism. Women are at a higher risk of ADRs compared to men, possibly due to differences in body composition, hormonal factors, and drug metabolism. Genetic predispositions also play a crucial role; specific genetic polymorphisms can affect drug metabolism and immune responses, making some individuals more susceptible to ADRs. Understanding these patient-related factors is essential for personalized medicine and risk management.
3. Drug Interactions
Drug interactions are a major cause of ADRs, especially in patients taking multiple medications. These interactions can alter the pharmacokinetics and pharmacodynamics of drugs, leading to increased toxicity or reduced efficacy. For example, interactions at drug transporters and efflux pumps can affect drug absorption and elimination, resulting in unexpected neurotoxicity or hepatotoxicity. Additionally, some drugs can inhibit or induce the metabolism of other drugs, leading to altered plasma concentrations and increased risk of ADRs. Awareness and management of potential drug interactions are crucial for minimizing ADRs.
4. Dosage and Duration of Treatment
The dosage and duration of drug treatment are critical factors in the development of ADRs. High doses and prolonged use of medications increase the risk of concentration-dependent ADRs. For instance, inappropriate dose schedules can lead to high plasma concentrations of drugs, resulting in toxic effects. Conversely, low doses may lead to rapid accumulation of metabolites, causing adverse reactions. The duration of treatment also plays a role; long-term use of certain drugs can lead to cumulative toxicity. Therefore, careful consideration of dosage and treatment duration is essential to minimize the risk of ADRs.
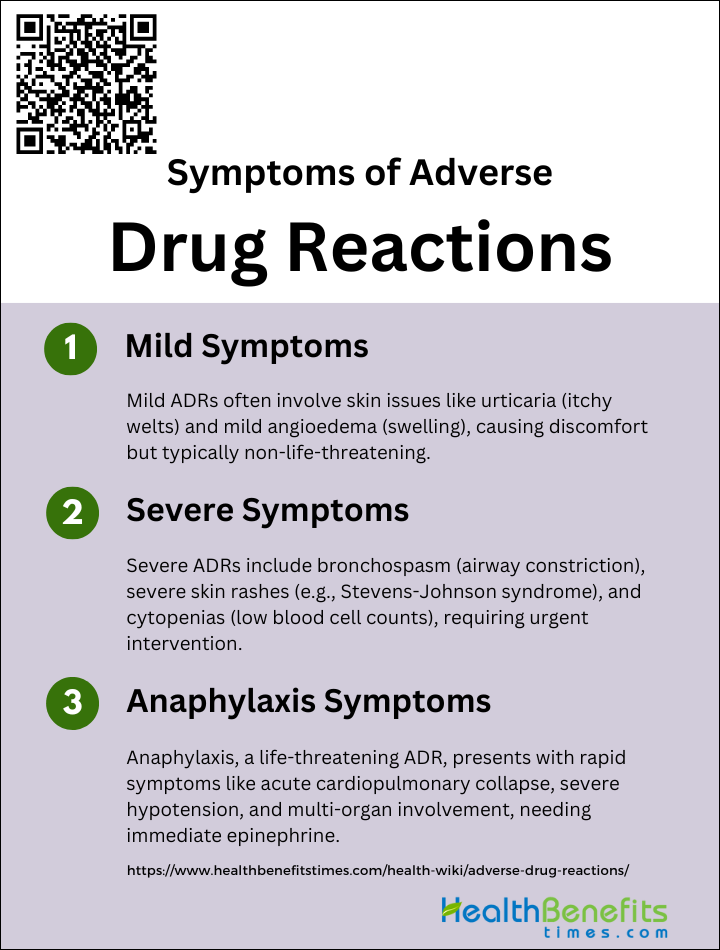
Symptoms of Adverse Drug Reactions
It can range from mild to severe and are critical to identify for patient safety. These symptoms may manifest differently in each individual, often complicating diagnosis and treatment. Below is a list of common symptoms that may indicate an adverse reaction to medication.
1. Mild Symptoms
Mild symptoms of adverse drug reactions often include skin-related manifestations such as urticaria (hives) and mild angioedema (swelling). These symptoms are generally not life-threatening but can cause significant discomfort and distress to the patient. Urticaria presents as raised, itchy welts on the skin, while angioedema involves deeper swelling, often around the eyes and lips. These reactions can occur shortly after drug intake and are commonly seen in clinical practice. Although these symptoms are usually benign, they can sometimes be a precursor to more severe reactions if not properly managed.
2. Severe Symptoms
Severe symptoms of adverse drug reactions can include more intense and potentially life-threatening conditions such as bronchospasm, severe skin rashes, and cytopenias. Bronchospasm, characterized by the constriction of airways, can lead to significant respiratory distress. Severe skin reactions may range from extensive rashes to conditions like Stevens-Johnson syndrome, which involves widespread skin detachment and mucosal involvement. Cytopenias, including hemolytic anemia and thrombocytopenia, are less common but serious conditions that can result from drug hypersensitivity and require immediate medical intervention.
3. Anaphylaxis Symptoms
Anaphylaxis is the most severe form of adverse drug reaction and can be life-threatening. It is characterized by a rapid onset of symptoms that can include acute cardiopulmonary collapse, severe hypotension, and multi-organ involvement. Common signs include difficulty breathing, swelling of the throat, a rapid drop in blood pressure, and loss of consciousness. Anaphylactic reactions can occur within minutes of drug exposure and require immediate treatment with epinephrine and supportive care to prevent fatal outcomes. Drugs commonly associated with anaphylaxis include antibiotics like penicillins and cephalosporins, NSAIDs, and radiology contrast agents.
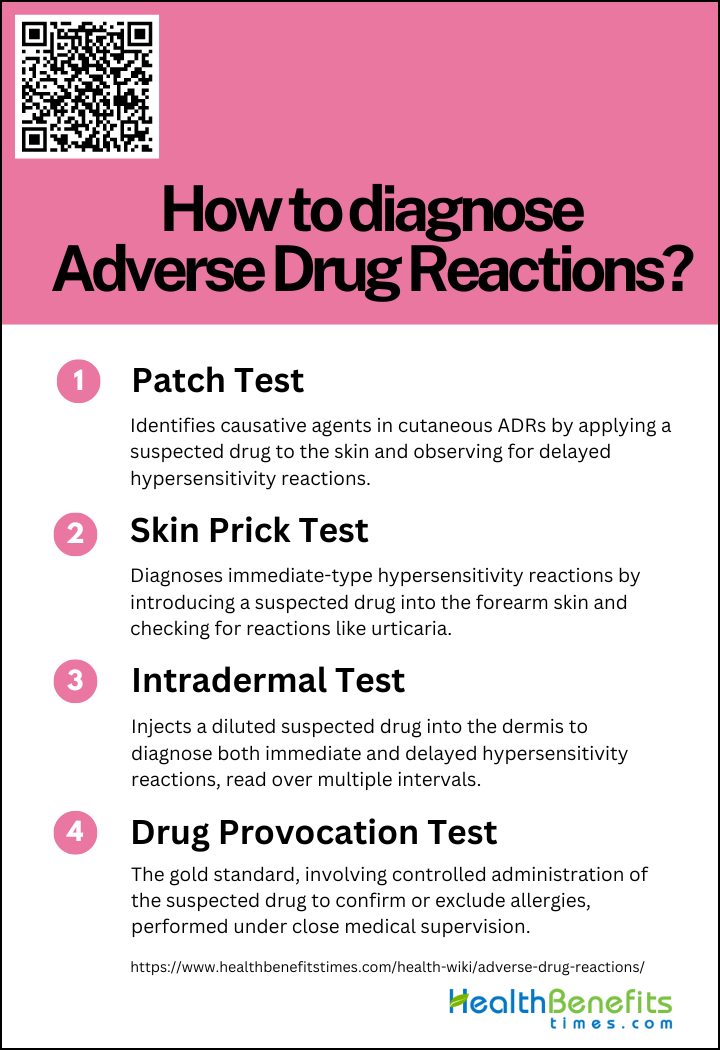
How to diagnose Adverse Drug Reactions?
Diagnosing adverse drug reactions (ADRs) is a critical step in ensuring patient safety and effective pharmacotherapy. It requires a meticulous evaluation of symptoms and a thorough investigation of the patient’s medication history. Below is a list of steps to systematically identify and assess potential ADRs.
1. A Patch Test
A patch test is a diagnostic tool used to identify the causative agent in cutaneous adverse drug reactions (CADRs). It involves applying a small amount of the suspected drug, diluted in a suitable vehicle, to the skin, typically on the back, and observing the reaction over several days. The test is particularly useful for identifying delayed hypersensitivity reactions, such as maculopapular exanthema, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms (DRESS). Patch tests are performed 6 weeks to 6 months after the complete healing of the CADR to avoid false positives due to residual inflammation. The test is considered safe and rarely causes severe adverse reactions, making it a valuable tool in the diagnostic workup of CADRs.
2. A Skin Prick Test
A skin prick test is primarily used to diagnose immediate-type hypersensitivity reactions to drugs. In this test, a small amount of the suspected drug is introduced into the skin of the forearm using a fine needle. The test is read after 20 minutes to check for an immediate allergic reaction, such as urticaria or angioedema. Skin prick tests are particularly useful for evaluating reactions to beta-lactam antibiotics and other drugs known to cause immediate hypersensitivity. However, the test has limitations, including a lower sensitivity compared to intradermal tests, and it is not suitable for all drugs, such as opiates. Despite these limitations, skin prick tests are a valuable component of the allergy workup for immediate drug reactions.
3. An Intradermal Test
An intradermal test (IDT) involves injecting a small volume (0.02-0.04 mL) of a diluted form of the suspected drug into the dermis. This test is used to diagnose both immediate and delayed hypersensitivity reactions. The test is read at multiple intervals: immediately at 20 minutes for immediate reactions, and at 24 hours, 48 hours, and sometimes up to a week for delayed reactions. IDTs are more sensitive than skin prick tests and are particularly useful when the latter are negative but clinical suspicion remains high. However, IDTs carry a higher risk of causing severe reactions, especially in patients with a history of severe CADRs, and should be performed with caution.
4. A Drug Provocation Test
A drug provocation test (DPT) is considered the gold standard for diagnosing adverse drug reactions when other tests are inconclusive. It involves administering the suspected drug to the patient under controlled conditions, starting with a very low dose and gradually increasing it while monitoring for adverse reactions. DPTs are particularly useful for confirming or excluding drug allergies, especially when multiple drugs are involved or when the history is unclear. However, DPTs carry significant risks, including the potential to precipitate severe or life-threatening reactions, and are contraindicated in patients with a history of severe reactions such as Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN). Therefore, DPTs should be performed in specialized settings with resuscitation facilities available.
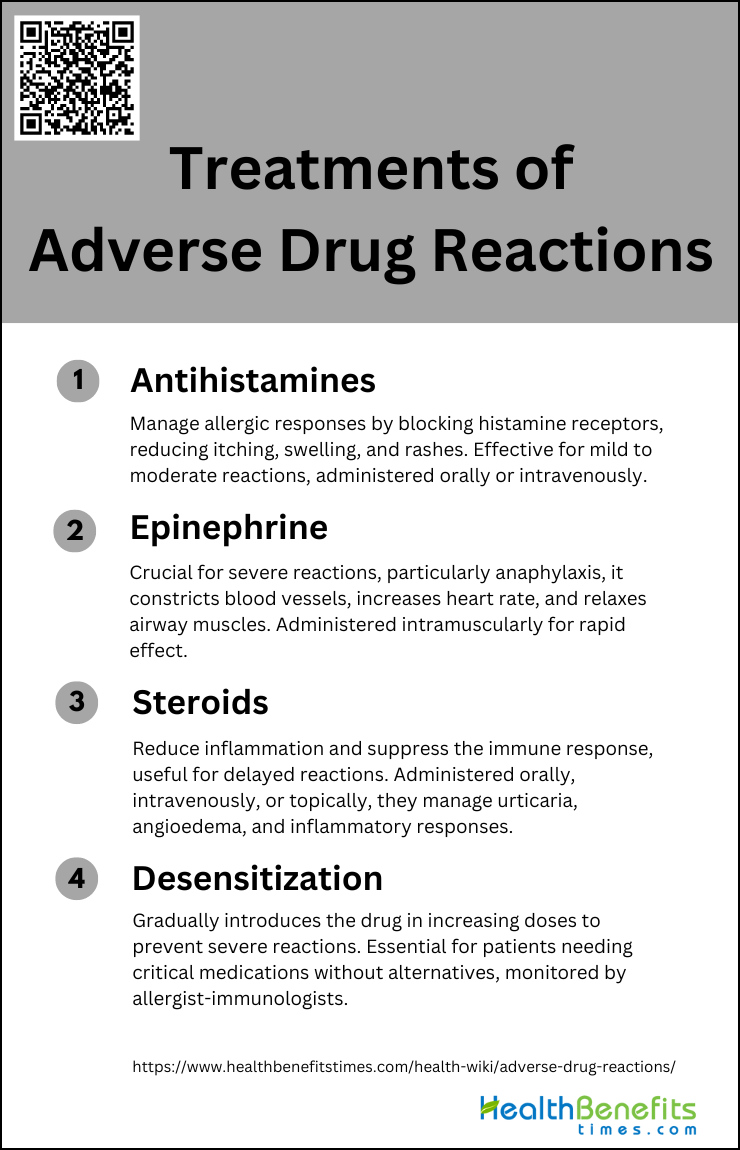
Treatments of adverse drug reaction
Treatment strategies must be tailored to the specific symptoms and severity of the reaction experienced by the patient. Below is a list of common treatments employed to address various types of ADRs.
1. Antihistamines
Antihistamines are commonly used to manage adverse drug reactions, particularly those involving allergic responses. These medications work by blocking histamine receptors, thereby reducing symptoms such as itching, swelling, and rashes. Antihistamines are effective in treating mild to moderate allergic reactions and can be administered orally or intravenously, depending on the severity of the reaction. They are often used as a first-line treatment in conjunction with other therapies to provide symptomatic relief and prevent the progression of allergic reactions1. Their role in managing adverse drug reactions is crucial, especially in cases where the reaction is not life-threatening but still requires medical intervention.
2. Epinephrine
Epinephrine is the cornerstone of treatment for severe adverse drug reactions, particularly anaphylaxis. It acts rapidly to constrict blood vessels, increase heart rate, and relax the muscles in the airways, thereby improving breathing and stabilizing blood pressure. The prompt administration of epinephrine is essential in life-threatening situations to prevent fatal outcomes. It is typically administered via intramuscular injection, and its effects are immediate, making it a critical component of emergency response protocols for severe allergic reactions. In some cases, additional doses may be required, and continuous monitoring is necessary to ensure patient stability.
3. Steroids
Steroids, or corticosteroids, are often used in the management of adverse drug reactions to reduce inflammation and suppress the immune response. They are particularly useful in treating delayed allergic reactions and preventing the recurrence of symptoms. Steroids can be administered orally, intravenously, or topically, depending on the nature and severity of the reaction. They are effective in managing conditions such as urticaria, angioedema, and other inflammatory responses associated with drug allergies. While steroids are not typically used as a first-line treatment for acute reactions, they play a significant role in the long-term management and prevention of adverse drug reactions.
4. Desensitization
Desensitization is a specialized procedure used to safely administer medications to patients who have previously experienced hypersensitivity reactions. This process involves the gradual introduction of the drug in increasing doses until the patient can tolerate the full therapeutic dose without experiencing severe adverse reactions. Rapid drug desensitization (RDD) has been shown to be highly effective, with a success rate of 99.9% in a large cohort of patients. This method is particularly valuable for patients who require essential medications for conditions such as infections, autoimmune diseases, and cancer, where no suitable alternatives exist. Desensitization protocols must be carefully designed and monitored by experienced allergist-immunologists to ensure patient safety and efficacy.
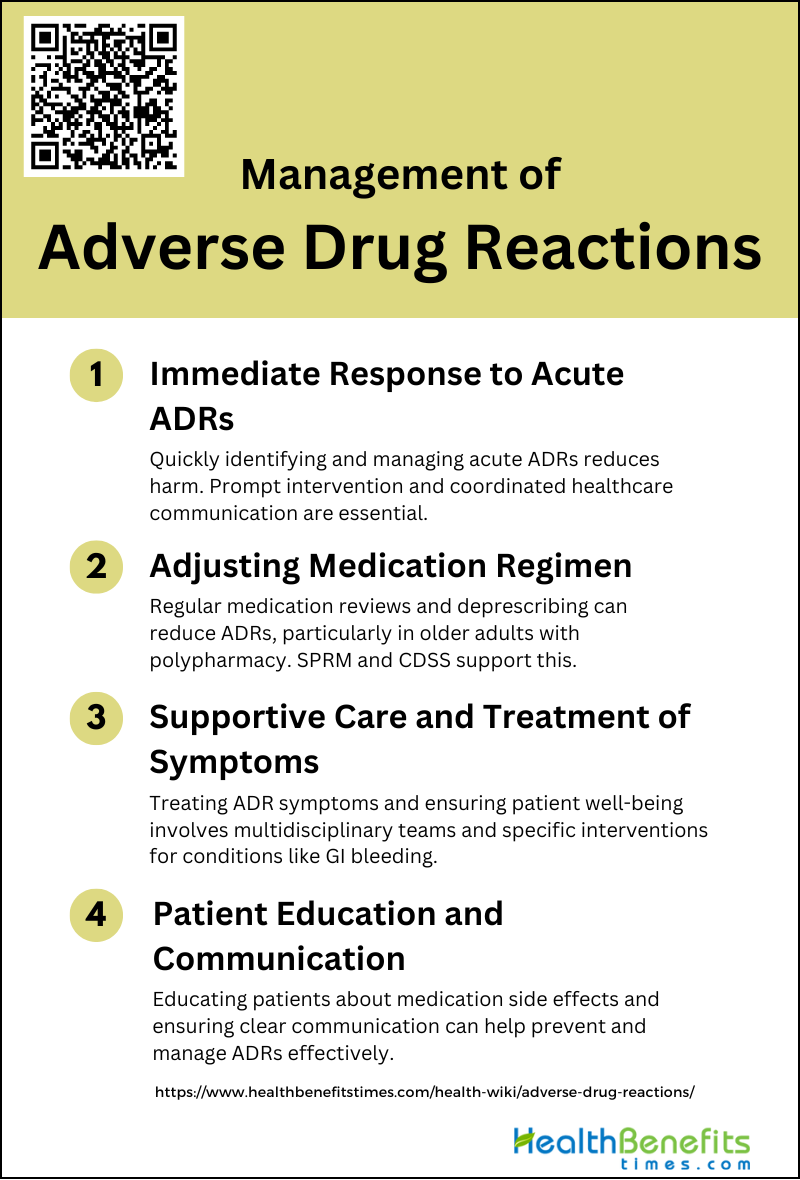
Management of Adverse Drug Reactions
The effective management of adverse drug reactions (ADRs) is crucial in ensuring patient safety and maintaining trust in healthcare systems. It involves a systematic approach to detect, assess, and respond to unintended effects of medications. Following this introduction, we will explore a list of key strategies to manage ADRs efficiently.
1. Immediate Response to Acute ADRs
Immediate response to acute adverse drug reactions (ADRs) is crucial to mitigate potential harm to patients. Prompt identification and management of ADRs can significantly reduce morbidity and mortality rates. Health professionals should be trained to recognize the clinical features of ADRs, which can range from mild symptoms like pruritus and rash to severe reactions such as systemic anaphylaxis and cardiovascular emergencies. Quick intervention often involves discontinuing the offending drug, administering appropriate antidotes or supportive treatments, and monitoring the patient closely for any progression of symptoms. Effective communication among healthcare providers is essential to ensure a coordinated and timely response to acute ADRs.
2. Adjusting Medication Regimen
Adjusting the medication regimen is a key strategy in managing ADRs, particularly in older adults who are often on multiple drug therapies. Polypharmacy and inappropriate prescribing are significant risk factors for ADRs in this population. A structured pharmacist review of medication (SPRM) supported by clinical decision support software (CDSS) has been shown to reduce inappropriate prescribing and ADR incidence in hospitalized older patients. Regular medication reviews, deprescribing unnecessary medications, and substituting safer alternatives can help minimize the risk of ADRs. Comprehensive geriatric assessments can also aid in tailoring medication regimens to the individual needs of older patients.
3. Supportive Care and Treatment of Symptoms
Supportive care and symptom management are essential components of ADR management. This involves treating the symptoms caused by the ADR while ensuring the patient’s overall well-being. For instance, gastrointestinal bleeding, a common ADR, requires specific interventions such as proton pump inhibitors and blood transfusions if necessary. In cases of drug-induced renal failure or delirium, appropriate supportive measures like hydration, electrolyte management, and cognitive support are critical. Multidisciplinary teams, including pharmacists, nurses, and physicians, play a vital role in providing comprehensive care to manage and alleviate the symptoms of ADRs.
4. Patient Education and Communication
Patient education and effective communication are fundamental in preventing and managing ADRs. Educating patients about the potential side effects of their medications, the importance of adherence to prescribed regimens, and the need to report any unusual symptoms promptly can help in early detection and management of ADRs. Clear communication between healthcare providers and patients, especially during transitions of care, such as hospital discharge, is crucial to ensure continuity of care and prevent ADRs. Utilizing tools like the PADR-EC ADR score to assess and communicate the risk of ADRs can further enhance patient safety and engagement in their own care.
Prevention of Adverse Drug Reactions
Proactive measures to prevent ADRs are essential in enhancing patient outcomes and optimizing medication efficacy. Below is a list of strategies aimed at minimizing the occurrence of these unwanted drug events.
1. Rational Prescribing and Deprescribing Practices
Rational prescribing and deprescribing are essential to prevent adverse drug reactions (ADRs), especially in older adults who are more susceptible due to polypharmacy and multimorbidity. Rational prescribing involves integrating the physiological changes of aging with pharmacological knowledge to minimize inappropriate drug use and polypharmacy. Deprescribing should be considered when medications are no longer beneficial or when safer alternatives exist. This approach helps in reducing the prescribing cascade, where new medications are prescribed to counteract the side effects of other drugs, often leading to further complications. Comprehensive geriatric assessments and explicit prescribing criteria can aid in making informed decisions about medication use.
2. Medication Review and Reconciliation
Medication review and reconciliation are critical processes in preventing ADRs. These involve creating the most accurate list of medications a patient is taking and comparing it against the medications prescribed during different transitions of care. Regular medication reviews help in identifying and rectifying discrepancies, thus reducing the risk of ADRs. In South Africa, a study showed that medication reconciliation significantly reduced medication discrepancies and improved patient care by ensuring continuity of care throughout the patient’s hospital stay. Pharmacists play a crucial role in this process by conducting comprehensive drug reviews and aiding in drug/dosage selection.
3. Patient Monitoring and Follow-up
Continuous patient monitoring and follow-up are vital to detect and manage ADRs promptly. Inadequate monitoring of drug therapy is a common cause of preventable ADRs, leading to hospital admissions and increased healthcare costs. Regular follow-ups allow healthcare providers to assess the efficacy of prescribed medications and adjust dosages as needed to prevent toxicity and other adverse effects 6. Multidisciplinary approaches, including the use of computerized alerts and decision support systems, can enhance monitoring efforts and reduce the incidence of ADRs.
4. Education and Training for Healthcare Providers
Education and training for healthcare providers are fundamental in preventing ADRs. Medical students and physicians should be well-versed in geriatric medicine principles and appropriate prescribing practices for older adults. Continuous professional development and training programs can help healthcare providers stay updated on the latest guidelines and best practices for medication management. Additionally, involving pharmacists in the education process can provide valuable insights into drug interactions and optimal therapeutic strategies. Effective education and training can empower healthcare providers to make informed decisions, ultimately reducing the risk of ADRs.