 An advance directive is a legal document that allows you to provide instructions about your future medical care and treatment preferences in case you become unable to make decisions for yourself. It enables you to express your wishes regarding life-sustaining treatments, appoint a healthcare representative to make decisions on your behalf, and provide other instructions related to your healthcare. Advance directives ensure that your healthcare providers and loved ones understand and respect your choices, even if you cannot communicate them directly due to incapacity.
An advance directive is a legal document that allows you to provide instructions about your future medical care and treatment preferences in case you become unable to make decisions for yourself. It enables you to express your wishes regarding life-sustaining treatments, appoint a healthcare representative to make decisions on your behalf, and provide other instructions related to your healthcare. Advance directives ensure that your healthcare providers and loved ones understand and respect your choices, even if you cannot communicate them directly due to incapacity.
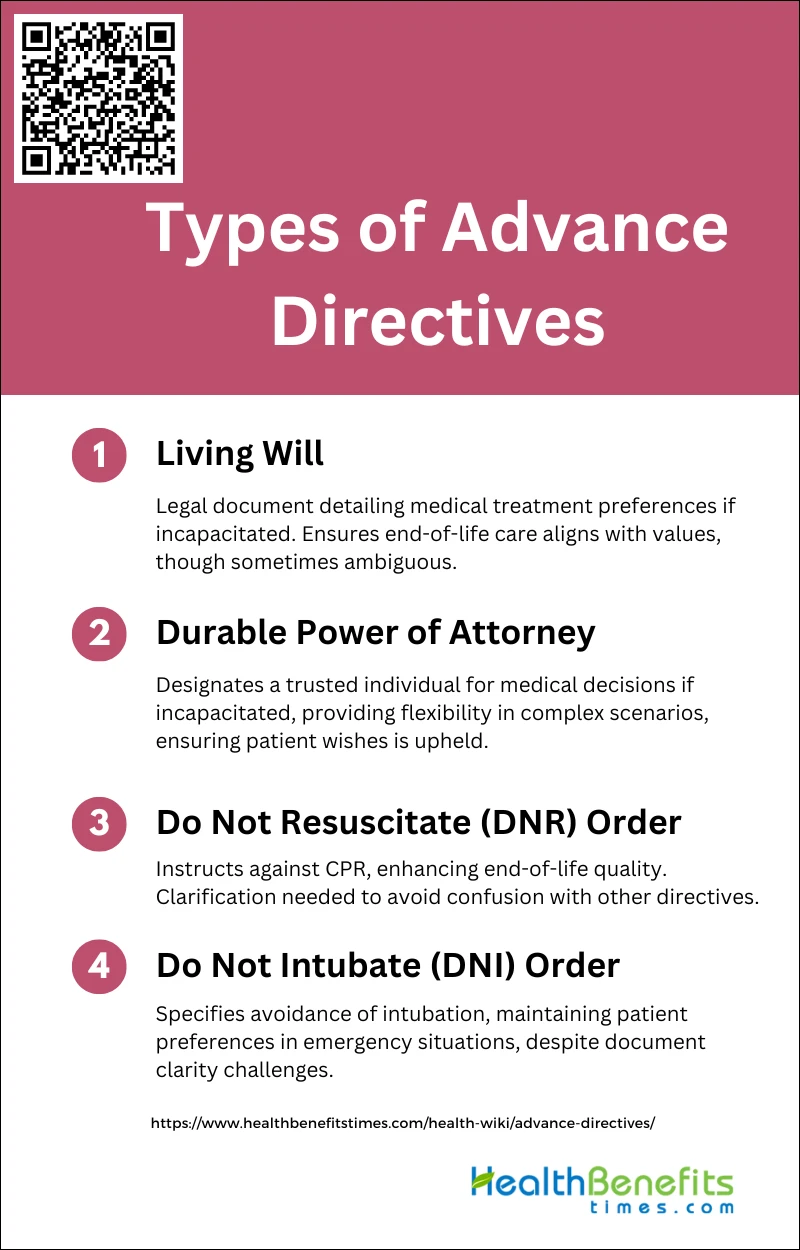
Types of Advance Directives
There are several types of advance directives that allow individuals to express their preferences for future medical care and decision-making. Below is a list of the various types of advance directives that one can consider when planning for future healthcare scenarios.
1. Living Will
A living will is a legal document that allows individuals to outline their preferences for medical treatment in the event they become incapacitated and unable to communicate their decisions. It specifies the types of medical care they wish to receive or avoid, such as life-sustaining treatments like mechanical ventilation or feeding tubes. However, living wills can sometimes be ambiguous and may not effectively convey the patient’s wishes, leading to unintended outcomes. Despite these challenges, living wills are crucial for ensuring that patients’ end-of-life care aligns with their values and preferences, thereby enhancing their quality of life during their final days.
2. Durable Power of Attorney for Healthcare
A durable power of attorney for healthcare is a legal instrument that designates a trusted individual to make medical decisions on behalf of the patient if they become incapacitated. This type of advance directive ensures that the patient’s healthcare preferences are respected and followed, even when they cannot communicate their wishes themselves. Unlike living wills, which can be vague, a durable power of attorney provides a more flexible and dynamic approach to decision-making, allowing the appointed agent to respond to unforeseen medical situations. This form of advance directive is particularly valuable in complex medical scenarios where immediate and informed decisions are necessary.
3. Do Not Resuscitate Order (DNR)
A Do Not Resuscitate (DNR) order is a medical directive that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if the patient’s heart stops or they stop breathing. DNR orders are associated with improved quality of life in the final days, as they prevent invasive and often distressing procedures that may not align with the patient’s end-of-life preferences. However, confusion can arise when distinguishing DNR orders from other types of advance directives, potentially leading to unintended outcomes. Despite these challenges, DNR orders play a critical role in respecting patients’ wishes and ensuring a dignified end-of-life experience.
4. Do Not Intubate (DNI) Order
DNI order is a specific type of advance directive that indicates a patient’s wish to avoid intubation and mechanical ventilation in the event of respiratory failure. Similar to DNR orders, DNI orders aim to prevent invasive procedures that may not contribute to the patient’s desired quality of life. These orders are particularly important in emergency settings, where quick decisions are necessary, and they help ensure that the patient’s preferences are honored. However, the effectiveness of DNI orders can be compromised by issues such as document availability and clarity, underscoring the need for better communication and documentation practices.
Problems with Advance Directives
Misunderstandings among family members, discrepancies in legal interpretations, and issues with accessibility during medical emergencies can all undermine their effectiveness. Here are some key problems associated with advance directives:
1. Limitations
Advance directives, while crucial for ensuring patient preferences are respected, have several limitations. One significant issue is the confusion surrounding the documents themselves, including their availability and accuracy. This confusion can lead to discrepancies between the documented wishes and the actual desires of the patient and their family members at the bedside2. Additionally, even when advance directives are in place, caregivers often feel unprepared for the decision-making and caregiving responsibilities that arise, indicating that these documents alone are insufficient for comprehensive end-of-life planning. The process often falls short in providing the necessary communication, knowledge, and preparation for families, highlighting the need for more robust support systems.
2. Importance of Communication
Effective communication is paramount in the context of advance directives and end-of-life care. Despite the presence of advance directives, many caregivers report feeling unprepared for the realities of caregiving and decision-making, suggesting that the documents alone do not suffice. Communication gaps between patients, families, and healthcare providers can exacerbate these challenges, leading to conflicts and uncertainty. Addressing these gaps through improved dialogue and education can enhance the caregiving experience and ensure that patient wishes are more accurately understood and respected. Therefore, fostering open and ongoing communication is essential for the successful implementation of advance directives and for supporting families during end-of-life care.