Adhesive Otitis Media (AOM) is a complicated middle ear issue caused by adhesions from previous infections, potentially leading to hearing loss and infections that may necessitate surgical intervention such as tympanoplasty. AOM is associated with stages of tympanic membrane atelectasis, which can result in complications like cholesteatoma. Treatment strategies vary, with some opting for conservative care while others suggest early surgery to prevent further deterioration of hearing.
Adhesive Otitis Media (AOM) is a complicated middle ear issue caused by adhesions from previous infections, potentially leading to hearing loss and infections that may necessitate surgical intervention such as tympanoplasty. AOM is associated with stages of tympanic membrane atelectasis, which can result in complications like cholesteatoma. Treatment strategies vary, with some opting for conservative care while others suggest early surgery to prevent further deterioration of hearing.
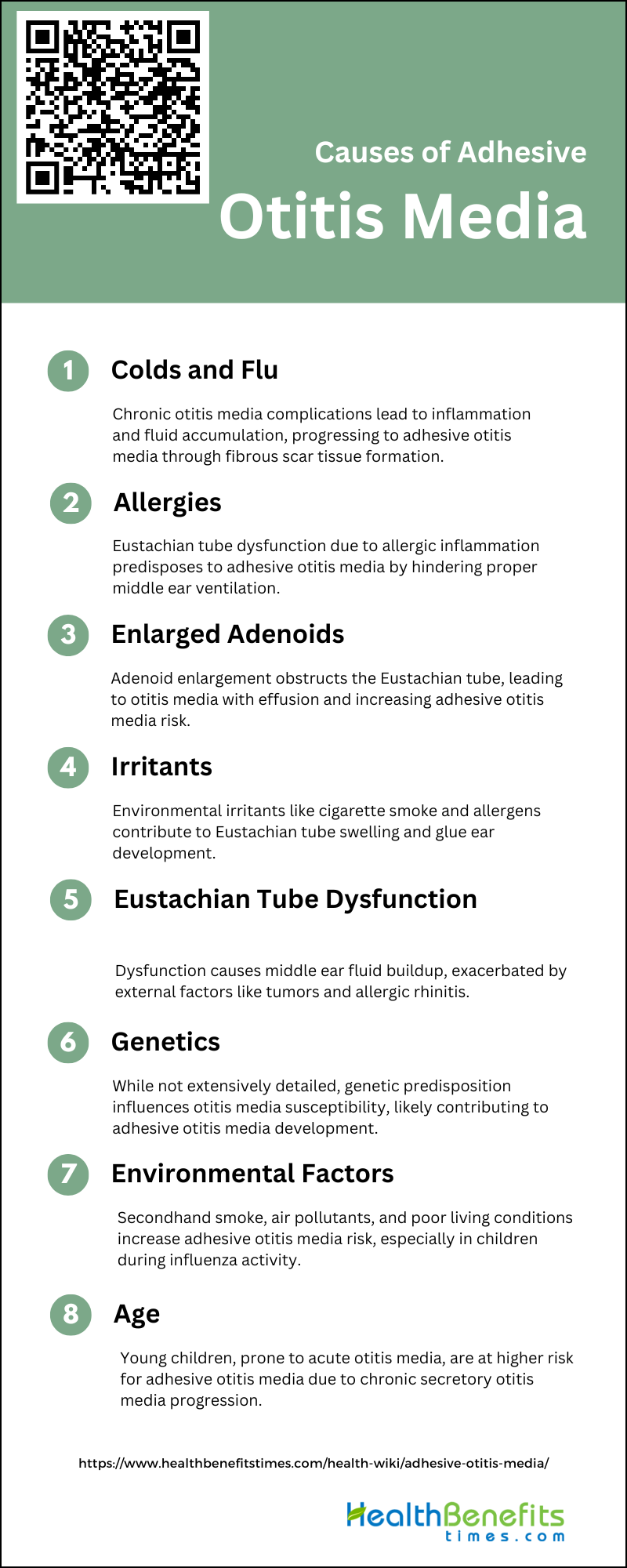
Causes of Adhesive Otitis Media
The condition often results from prolonged inflammation or infection, which causes the formation of scar tissue, restricting the movement of the ear’s ossicles and impacting auditory function. Understanding the causes of adhesive otitis media is crucial for exploring holistic health and fitness approaches to manage and alleviate its symptoms.
1. Colds and flu
Adhesive otitis media typically develops as a complication of chronic otitis media, characterized by inflammation and fluid accumulation in the middle ear. This condition often follows inadequately treated acute or chronic otitis media, leading to edema and exudate formation in the tympanic cavity. The exudate, rich in fibrin, may not be effectively cleared and can deposit on the middle ear structures, eventually converting into fibrous scar tissue. This process results in adhesions that impair the mobility of the auditory ossicles, crucial for sound transmission, thereby causing progressive hearing loss and other auditory issues.
2. Allergies
Allergies are a significant factor in the development of adhesive otitis media, primarily through their impact on the Eustachian tube function. Allergic reactions can cause inflammation and swelling of the mucosal linings, leading to Eustachian tube dysfunction (ETD). This dysfunction can prevent proper ventilation and drainage of the middle ear, creating an environment conducive to the accumulation of fluids and the development of adhesive otitis media. The inflammation associated with allergies can also lead to the thickening of the middle ear lining and the formation of adhesive tissues, further compromising ear function and leading to chronic conditions.
3. Enlarged adenoids
Enlarged adenoids can cause adhesive otitis media because of their location and ability to block the Eustachian tube when they are inflamed or enlarged. This blockage can result in otitis media with effusion (OME) because the dysfunction of the Eustachian tube prevents the middle ear from being properly ventilated. Research has indicated that children with enlarged adenoids are more likely to develop OME, and the severity of the blockage in the nasopharynx is related to the frequency of OME.
4. Irritants
Adhesive otitis media commonly referred to as “glue ear,” can be caused by several irritants that affect the Eustachian tube and the middle ear. Notably, cigarette smoke is a significant irritant that can lead to the development of this condition. Exposure to other environmental irritants such as air pollution and allergens can also contribute to the swelling of the Eustachian tube lining, leading to fluid accumulation in the middle ear. This fluid buildup can become thick and sticky, resembling glue, hence the name “glue ear.” Additionally, respiratory infections can exacerbate or trigger the condition by causing further inflammation and blockage of the Eustachian tube.
5. Eustachian Tube Dysfunction
Eustachian Tube Dysfunction plays a major role in adhesive otitis media, where the eardrum retracts and fluid builds up in the middle ear. Eustachian Tube Dysfunction can be caused by functional or mechanical blockages, like increased tubal compliance or problems with the opening mechanism. External factors like tumors or adenoid masses can also contribute. Allergic rhinitis can worsen the situation by causing nasal inflammation and leading to Eustachian Tube Dysfunction, which creates a negative pressure in the middle ear and affects ventilation.
6. Genetics
The specific genetic causes of adhesive otitis media are not extensively detailed in the provided sources, research in the broader field of otitis media (OM) suggests a significant genetic component in its development. Studies have identified a heritability estimate of 40%–70% for OM susceptibility, indicating that genetics play a substantial role alongside environmental factors. Although no direct references to adhesive otitis media were found in the sources, the general consensus in otitis media research underscores the importance of genetic factors in predisposing individuals to various forms of the condition.
7. Environmental Factors
Environmental factors play a big role in the development of adhesive otitis media, a condition characterized by inflammation and potential chronicity in the middle ear. Exposure to secondhand smoke is a major risk factor, with studies showing that both parents smoking and exposure to air pollutants like nitrogen dioxide and fine particles increase the chances of developing otitis media. Poor living conditions and air pollution are also linked to the condition, especially during periods of high influenza activity. Indoor factors like dampness in the home are associated with acute otitis media in subtropical areas.
8. Age
Adhesive otitis media (AOM) is when a glue-like substance is found in the middle ear, causing hearing loss and other issues. Age plays a big role in developing AOM, especially in young children who often get it after acute otitis media, the most common bacterial infection in kids. Chronic secretory otitis media, which can lead to AOM, is most common around age two and becomes less common as children get older.
Risk Factors of Adhesive Otitis Media
Adhesive otitis media, often developing after poorly treated acute or chronic otitis media, is influenced by several risk factors. The primary cause is the accumulation of inflammatory exudate in the middle ear, which includes a high concentration of fibrin. This condition typically follows unresolved inflammation, leading to the deposition of fibrin and subsequent fibrous-scar tissue formation on the middle ear structures.
- Passive smoking
- Bottle feeding
- Daycare nursery
- Atopy
- Children or older adults
Symptoms of Adhesive Otitis Media
Adhesive otitis media, also known as glue ear, primarily manifests through progressive hearing loss, which is often the most troubling symptom for those affected. This condition, characterized by the adhesion of the middle ear structures due to chronic inflammation, leads to impaired sound perception at specific wavelengths and can cause persistent tinnitus (ringing in the ears). Unlike other forms of ear infections, adhesive otitis media typically does not present with pain or discharge from the ear, making it less likely for patients to seek immediate medical attention for these symptoms. Instead, the hearing impairment and tinnitus are constant issues that significantly affect the quality of life, prompting individuals to consult healthcare providers.
- Hearing loss
- Communication difficulties
- Lack of attention
- Impaired speech
- Impaired language development
- Otalgia or earache
- Aural fullness or sensation of ear popping
- Tinnitus
- A sensation of foreign body in the external auditory canal
- Upper respiratory infections
- Recurrent ear infections
- Nasal obstructions
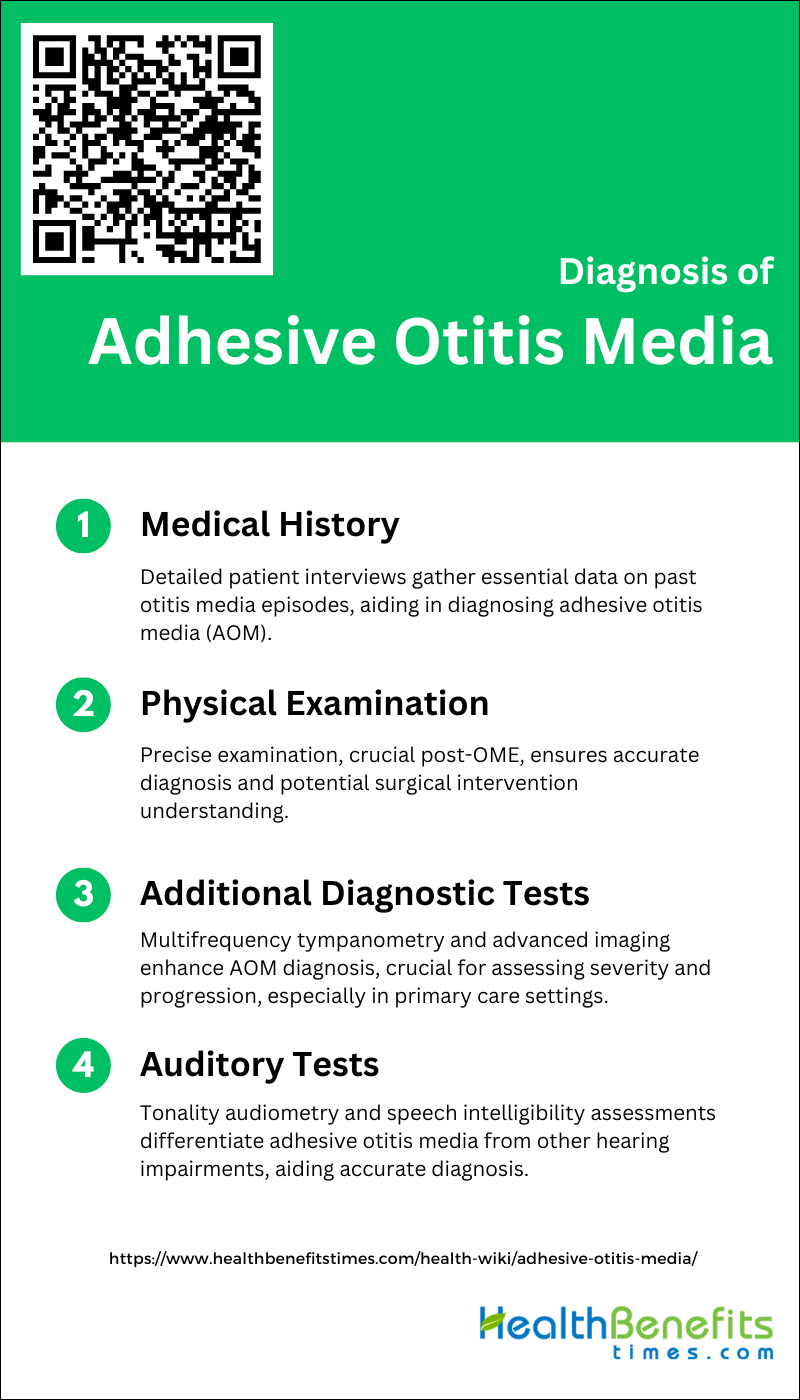
Diagnosis of Adhesive Otitis Media
Adhesive otitis media (AOM) is a chronic condition characterized by the adhesion of the tympanic membrane to the medial wall of the middle ear, often as a result of unresolved inflammation. The diagnosis of this condition involves a combination of patient history, physical examination, and specialized tests.
1. Medical History
The diagnosis of adhesive otitis media (AOM) heavily relies on a detailed medical history, particularly noting any past episodes of acute or chronic otitis media. This history is crucial because AOM typically develops as a sequel to these earlier infections, which may have been inadequately treated or resolved. During the diagnostic process, healthcare providers conduct a thorough review of the patient’s medical records to check for previous otitis media incidents and treatments. If past medical records are not available, detailed patient interviews are used to gather this essential historical data.
2. Physical examination
The physical examination is very important in diagnosing Adhesive Otitis Media (AOM), a condition that often occurs after Otitis Media with Effusion (OME) and may need surgery. It is crucial to conduct a detailed and precise physical examination because some healthcare providers may not fully understand the criteria for diagnosis or may misinterpret the examination results.
3. Additional Diagnostic Tests
Diagnosing Adhesive Otitis Media (AOM) can be difficult due to its complex nature and potential to progress to more serious conditions like cholesteatoma. While otoscopic findings are important, additional tests are often needed to confirm the diagnosis and evaluate the severity of the condition. Multifrequency tympanometry is a highly effective method for diagnosing AOM, with a 70% diagnostic accuracy rate by detecting changes in resonant frequency. New advanced diagnostic techniques, such as short-wave infrared fluorescence chemical sensors and intelligent smartphone-based multimode imaging otoscopes, have been developed to enhance diagnostic precision and potentially enable mobile diagnosis, especially in primary care settings. These supplementary tests, along with clinical features and otoscopic findings, offer a more thorough evaluation of AOM.
4. Auditory Tests
The auditory tests typically include threshold tonal audiometry, which measures the softest sounds a person can hear at various frequencies, and assessments of ultrasound hearing sensitivity and speech intelligibility in noisy environments. These tests help differentiate adhesive otitis media from other types of hearing impairments, such as those stemming from inner ear pathologies. For instance, a characteristic finding in adhesive otitis media might be a descending audiometric curve with high hearing thresholds related to bone conduction, alongside a small bone-air gap, which are indicative of middle ear involvement rather than inner ear issues.
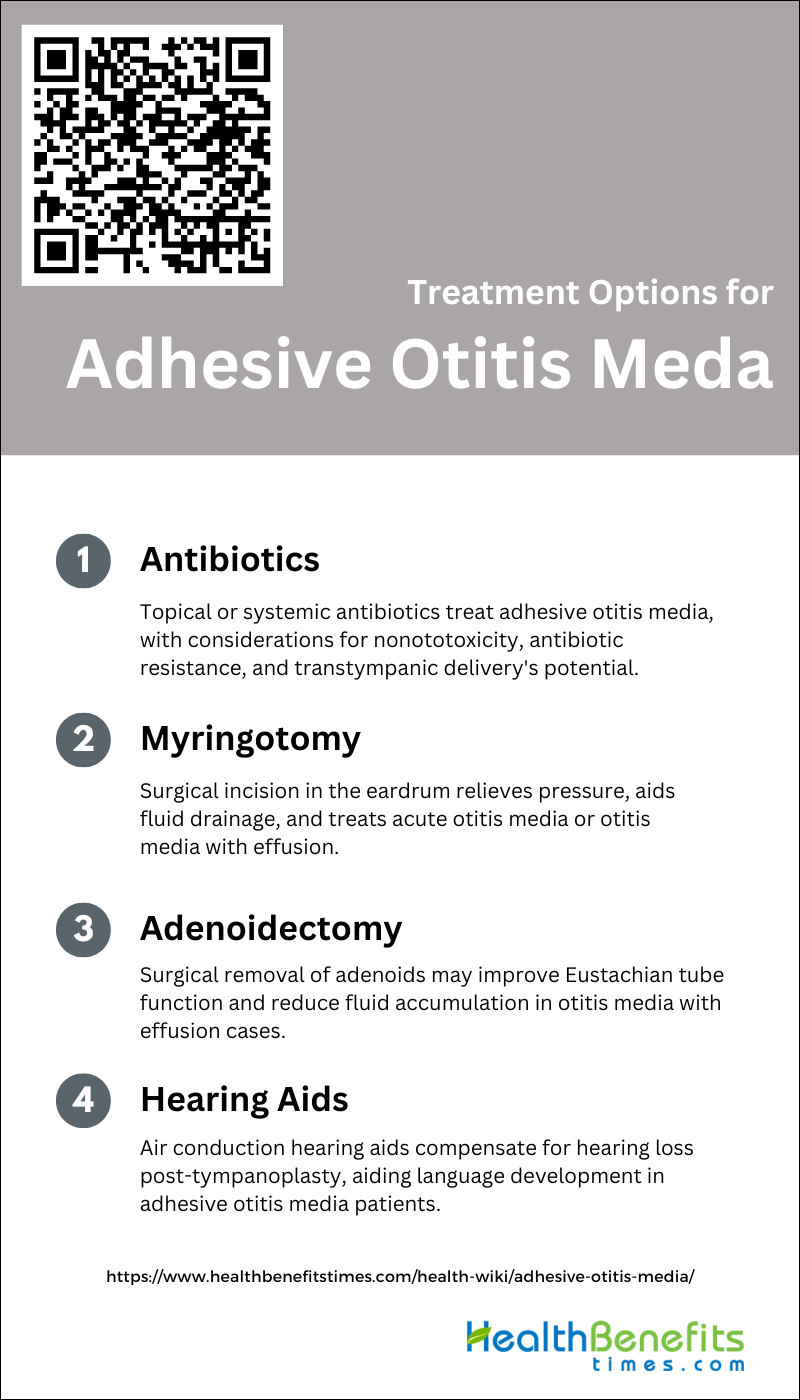
Treatment Options for Adhesive Otitis Media
There are different treatment options for adhesive otitis media (AOM) depending on how severe and advanced the condition is. If there are repeated infections or a significant loss of hearing, surgery like tympanoplasty is often recommended. Tympanoplasty can be done along with fascia grafting catheterization, which has proven to be successful in treating AOM. This procedure can improve hearing and keep the ears dry after surgery.
1. Antibiotics
Topical antibiotics are commonly used to treat adhesive otitis media, especially in cases of chronic suppurative otitis media. The American Academy of Otolaryngology-Head and Neck Surgery recommends using nonototoxic antibiotics to prevent ear damage. Amoxicillin is the preferred drug for uncomplicated acute otitis media, but other antibiotics may be necessary for certain situations. Shorter antibiotic courses can be effective, but longer ones may be needed to prevent treatment failure. The use of systemic antibiotics is debated, with some evidence suggesting delayed treatment can be beneficial. Transtympanic delivery of antibiotics is being studied as a way to target infections in the middle ear. It’s important to weigh the benefits of antibiotics against the risks of adverse reactions and antibiotic resistance.
2. Myringotomy
Myringotomy is a surgical procedure that involves making a small incision in the eardrum to relieve pressure or drain fluid. It has been studied to see how well it treats acute otitis media (AOM) and otitis media with effusion (OME). Research shows that myringotomy can help children with AOM recover faster. One study found that 71% of children who had myringotomy were cured after two weeks, compared to only 42% of those who didn’t have the procedure. However, the benefits of myringotomy alone are not always clear. A study found that there were no significant differences in outcomes between children who had myringotomy, antibiotics, both, or neither. This suggests that treating the symptoms could be a reasonable first step[Link]. In infants, treatment with amoxicillin/clavulanate was more effective than myringotomy alone, and adding myringotomy didn’t make a big difference in how long the infection lasted or how much fluid was in the middle ear. For chronic OME, laser myringotomy was found to be safe but not as effective as ventilation tubes. Comparing myringotomy with and without tympanostomy tubes, using tubes resulted in less time with fluid in the ear and better hearing. However, there are risks like otorrhea (ear discharge) and a hole in the eardrum. Myringotomy combined with perfusion and blowing therapy has shown promise, with a lower chance of the problem coming back and better hearing. Overall, while myringotomy can help in some cases of AOM and OME, doctors should think about the patient’s individual factors and consider other treatments like antibiotics or waiting to see if the problem gets better on its own.
3. Adenoidectomy
Adenoidectomy, a surgical procedure to remove the adenoids, is often considered for treating otitis media with effusion (OME), commonly known as “glue ear,” particularly when other treatments such as tympanostomy tube placement have not been effective. The procedure aims to improve Eustachian tube function, potentially reducing the recurrence of fluid accumulation in the middle ear, which is characteristic of OME. However, the effectiveness of adenoidectomy in improving hearing or preventing the recurrence of OME is still uncertain, with some studies suggesting a modest benefit while others indicate limited or no significant improvement compared to non-surgical treatments. Additionally, adenoidectomy carries risks such as postoperative bleeding, though these complications are generally considered rare. Therefore, the decision to proceed with adenoidectomy should be carefully considered, weighing the potential benefits against the risks and the specific characteristics and medical history of the patient
4. Hearing aids
For individuals suffering from adhesive otitis media, a condition characterized by fluid accumulation in the middle ear without signs of acute infection, hearing aids represent a non-invasive treatment option, especially when hearing loss affects language development. Air conduction hearing aids are the most widely prescribed devices for treating residual hearing loss following tympanoplasty, a surgical intervention often employed in managing this condition. These devices are designed to be placed inside the ear canal, where they capture and amplify sounds entering the outer ear, thereby compensating for the hearing loss. They are particularly beneficial for patients with safe, dry ears and mild to moderate conductive hearing losses, offering excellent aural rehabilitation. However, it’s important to note that hearing thresholds may deteriorate over time, and some patients can be difficult to fit due to ongoing infection or surgical management, highlighting the need for careful consideration and customization of hearing aid solutions for each patient.
Prevention of Adhesive Otitis Media
Adhesive otitis media (AOM) is a chronic condition characterized by the adhesion of the tympanic membrane to the medial wall of the middle ear due to inflammation. Preventing this condition primarily involves addressing the factors that lead to its development.
1. Breastfeeding (chestfeeding)
Breastfeeding helps reduce the risk of ear infections in babies and young children. Studies show that exclusively breastfeeding for over six months can protect against ear infections for the first six years of life, especially during the first four months. Introducing formula before six months increases the risk of ear infections. Even breastfeeding for just three months can lower the chances of ear infections in babies. Breast milk contains substances that fight infections, reduce inflammation, and boost the immune system, which helps prevent ear infections. Long-term breastfeeding may also prevent recurrent ear infections up to three years of age. Increasing breastfeeding rates and duration could save money by reducing ear infection cases.
2. Holding your baby upright during feeding
A nursing bottle with a slanted neck has been designed to mimic the upright breastfeeding position, which is thought to be crucial in preventing ear infections. Studies have indicated that feeding infants in an upright position can decrease the occurrence of ear and respiratory problems. There is a connection between feeding babies while they are lying down and ear infections. It is advised to feed babies in an upright position to lower the chances of ear infections and to encourage breastfeeding.
3. Avoiding cigarette smoke
Avoiding cigarette smoke is crucial in the prevention of Adhesive Otitis Media (AOM), particularly in children. Exposure to tobacco smoke has been consistently linked to an increased risk of developing AOM and other middle ear infections. Studies have shown that children exposed to secondhand smoke are more likely to suffer from the accumulation of fluid in the middle ear, leading to the condition known as glue ear, which can progress to AOM if not addressed. Furthermore, environmental tobacco smoke not only contributes to the initial occurrence of AOM but also to its recurrence and the severity of the symptoms. Therefore, maintaining a smoke-free environment at home and in the car, as well as avoiding public places where smoking is allowed, can significantly reduce the risk of AOM and improve overall ear health.
4. Testing for allergies
Testing for allergies plays a crucial role in the prevention of Adhesive Otitis Media (AOM), as many common allergens are known to cause swelling of the Eustachian tubes, leading to this condition. Allergens such as pollen, dust mites, and animal fur can trigger allergic reactions that contribute to the development of AOM by causing inflammation and blockage of the Eustachian tubes. This blockage prevents proper drainage of fluid from the middle ear, creating an environment conducive to infections and the formation of adhesive tissues. Therefore, identifying and managing allergies through testing can be an effective strategy in preventing the occurrence or recurrence of Adhesive Otitis Media, ultimately protecting against the associated hearing loss and other complications.
5. Cleaning and disinfecting
Preventing adhesive otitis media, a condition characterized by the formation of scar tissue in the middle ear leading to hearing loss, involves meticulous attention to ear hygiene and avoiding self-medication. Key preventive measures include regular cleaning and disinfecting of the ear, particularly after exposure to potential contaminants or water activities, which can introduce bacteria into the ear environment. It is crucial to seek professional medical advice for ear symptoms rather than using over-the-counter or home remedies, as improper treatment can exacerbate the condition. Ensuring that the ears are kept dry and clean, using safe methods to remove earwax without damaging the ear canal, and avoiding the insertion of objects into the ear are all effective strategies to maintain ear health and prevent the onset of adhesive otitis media.