Adenoids are secondary lymphoid organs located in the nasopharynx. They are part of the Waldeyer ring, along with the palatine tonsils and lingual tonsils. They are a part of the lymphatic system and play a role in the body’s immune defense, particularly in young children. Adenoids help to filter out harmful bacteria and viruses that enter the body through the nose and mouth. They are composed of lymphoid tissue, similar to the tonsils, and can become enlarged due to infections or allergies. When adenoids become chronically enlarged or infected, they may cause symptoms such as breathing difficulties, snoring, sleep apnea, chronic ear infections, or sinusitis. In some cases, surgical removal of the adenoids (adenoidectomy) may be recommended to alleviate these symptoms and improve the child’s quality of life.
What do adenoids do?
Adenoids play a vital role in the body’s immune system, especially in young children. As part of the lymphatic system, adenoids help defend the body against harmful bacteria and viruses that enter through the nose and mouth. They contain immune cells that produce antibodies and capture germs, preventing their further spread in the body. By removing these pathogens, adenoids help lower the risk of infections in the upper respiratory tract, such as colds, flu, and sinus infections. Additionally, adenoids collaborate with the tonsils to aid in the development of the immune system during early childhood. As children age, the role of adenoids in the immune system decreases, and they typically decrease in size by the age of 5 or 6. However, when adenoids become chronically enlarged or infected, they may obstruct breathing and lead to other health problems, necessitating medical attention or surgical intervention.
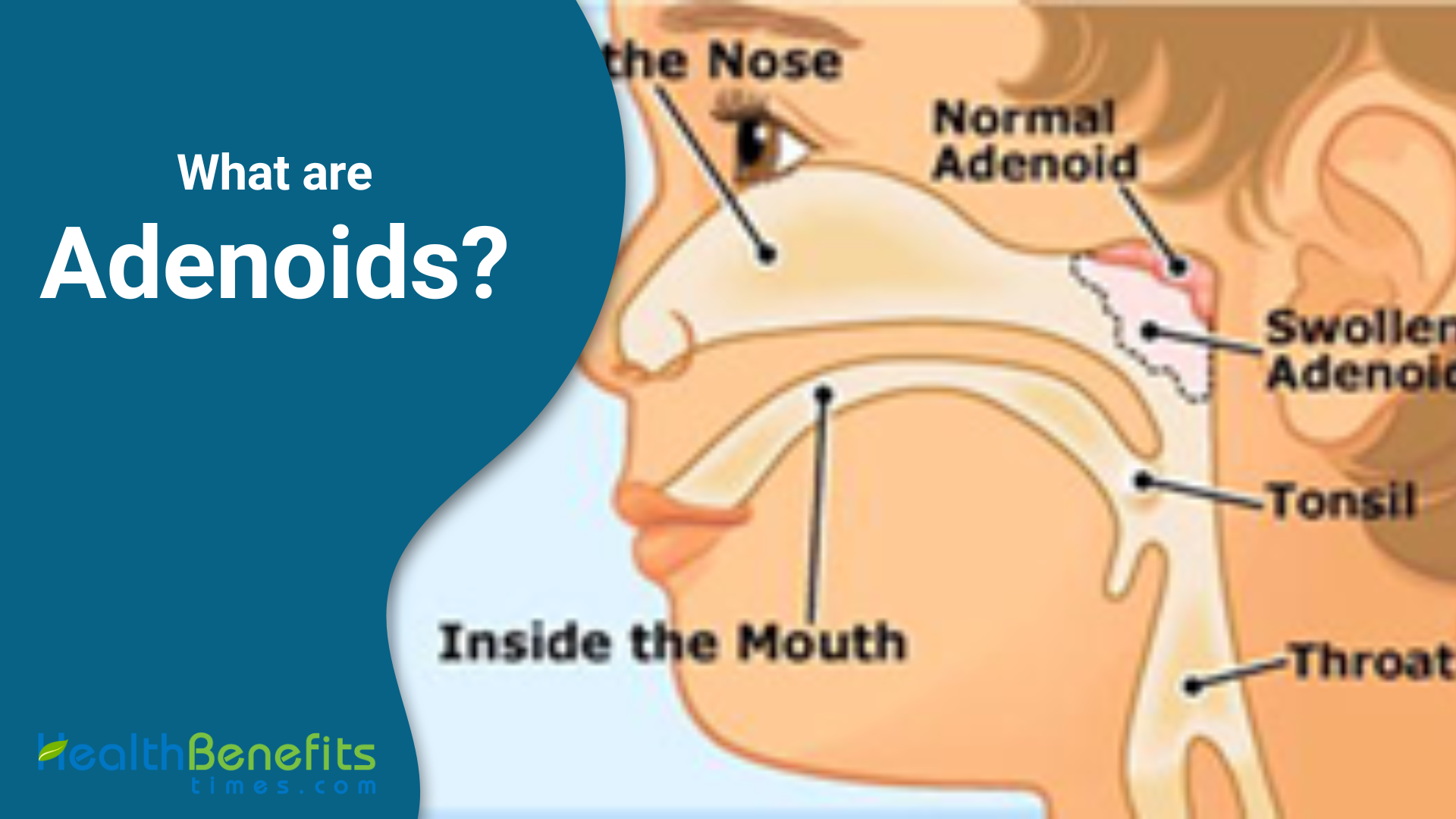
Anatomy of Adenoids
Adenoids are located in the nasopharynx, situated above the soft palate and behind the nasal cavity. They are positioned near the Eustachian tubes, which connect the middle ear to the nasopharynx. Adenoids are small, spongy, and pinkish in color, resembling soft tissue masses. They are covered by a mucous membrane similar to that found in the nasal and oral cavities. The size of adenoids varies among individuals and can change during childhood. In young children, adenoids are typically 1 to 1.5 cm in size, but can grow to the size of a ping pong ball. They usually reach their maximum size between the ages of 3 and 5 years, and then begin to shrink as the child ages. Adenoids are primarily composed of lymphoid tissue, which contains lymphocytes that help fight infections by trapping and destroying harmful bacteria and viruses that enter the body through the nose and mouth.
What are enlarged adenoids?
Enlarged adenoids, also known as adenoid hypertrophy, occur when the adenoid tissue located at the back of the nasal passage becomes swollen and increases in size. This enlargement can be caused by recurrent infections, allergies, or other factors that stimulate the immune system. When adenoids become enlarged, they can partially or completely obstruct the nasal airway, leading to various symptoms. Children with enlarged adenoids may experience difficulty breathing through the nose, mouth breathing, snoring, sleep apnea, chronic nasal congestion, and recurrent ear infections. In some cases, enlarged adenoids can also impact speech, resulting in a “nasal” or muffled voice. If left untreated, enlarged adenoids can lead to more severe complications, such as sleep disorders, facial growth abnormalities, and impaired cognitive development. Treatment for enlarged adenoids depends on the severity of the symptoms and may include medications, such as nasal corticosteroid sprays or antibiotics, to reduce inflammation and treat infections. In more severe cases, surgical removal of the adenoids (adenoidectomy) may be recommended to alleviate symptoms and improve the child’s quality of life.
Causes of enlarged adenoids?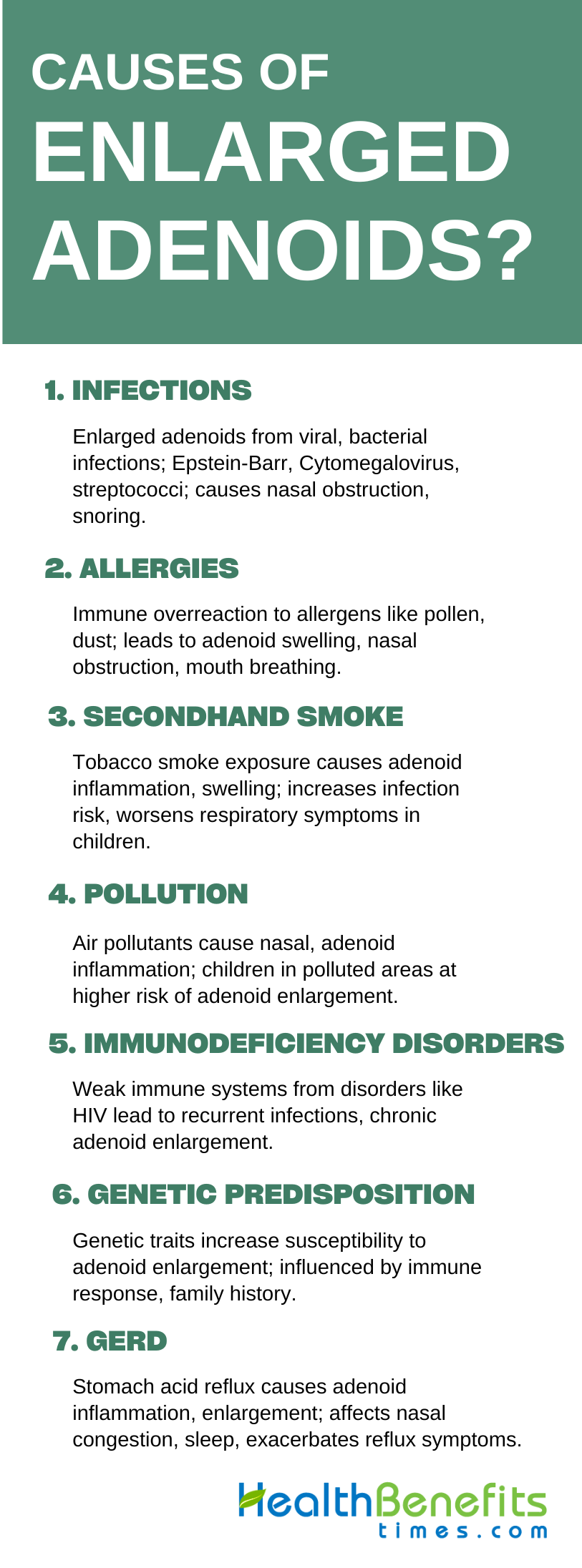
Enlarged adenoids can result from various factors, including:
1. Viral or bacterial infections:
Enlarged adenoids can be caused by viral and bacterial infections. Viruses such as Epstein-Barr virus, Cytomegalovirus, and human herpesviruses 6 (HHV6) have been detected in patients with adenoid hypertrophy. Bacterial pathogens like Haemophilus influenzae, Staphylococcus aureus, and group A beta-hemolytic streptococci can also contribute to the enlargement of adenoids. Additionally, repeated throat infections, both viral and bacterial, can lead to reactive lymphoid follicular hyperplasia and hypertrophy of the adenoids . These infections can cause nasal obstruction, mouth breathing, snoring, and otologic symptoms due to Eustachian tube blockage . Adenoids are constantly exposed to viral and bacterial agents, making them potential reservoirs for these pathogens. Therefore, viral and bacterial infections play a significant role in the development of enlarged adenoids.
2. Allergies:
Allergies are a common cause of enlarged adenoids. When a person is exposed to an allergen, such as pollen, dust mites, or pet dander, their immune system may overreact, producing antibodies known as Immunoglobulin E (IgE). These antibodies can trigger the release of histamine and other inflammatory chemicals, resulting in symptoms like sneezing, a runny nose, and congestion. The persistent inflammation caused by allergies can lead to the enlargement and swelling of the adenoids. Since the adenoids are situated in the back of the nasal passage, chronic allergic reactions can cause prolonged inflammation and enlargement of these tissues. This can obstruct the nasal airways, leading to mouth breathing, snoring, and other related symptoms. Children with allergies are particularly susceptible to developing enlarged adenoids, as their immune systems are more sensitive and reactive to environmental allergens. Identifying and managing allergies through medications, immunotherapy, or environmental modifications can help reduce inflammation and prevent the development of enlarged adenoids.
3. Secondhand smoke exposure:
Exposure to secondhand smoke is a significant risk factor for the development of enlarged adenoids. When an individual, particularly a child, is exposed to tobacco smoke from cigarettes, cigars, or pipes, the irritants and chemicals in the smoke can cause inflammation and swelling of the adenoids. The smoke can irritate the lining of the nasal passages and the adenoids, leading to chronic inflammation and enlargement. Children are especially vulnerable to the effects of secondhand smoke due to their smaller airways and developing immune systems. Exposure to secondhand smoke can also increase the risk of recurrent infections, such as sinusitis and otitis media, which can further contribute to adenoid enlargement. Additionally, children exposed to secondhand smoke may experience more frequent and severe symptoms related to enlarged adenoids, such as snoring, sleep apnea, and breathing difficulties. Preventing exposure to secondhand smoke, both at home and in public places, is crucial for reducing the risk of enlarged adenoids and other respiratory health problems in children.
4. Pollution:
Pollution is an environmental factor that can contribute to the development of enlarged adenoids. Air pollutants, including industrial emissions, vehicle exhaust, and particulate matter, can irritate the nasal passages and cause inflammation in the adenoids. When individuals inhale these pollutants, small particles can become trapped in the mucus lining of the nasal cavity and adenoids, leading to chronic inflammation and swelling. Children living in urban areas with high levels of air pollution are particularly susceptible to developing enlarged adenoids due to prolonged exposure to these irritants. Indoor pollutants, such as volatile organic compounds (VOCs) from cleaning products, paints, and furniture, can also contribute to adenoid inflammation. The combined exposure to both outdoor and indoor pollutants can result in persistent enlargement of the adenoids, causing symptoms such as nasal congestion, mouth breathing, and sleep disturbances. To reduce the risk of enlarged adenoids and other respiratory health issues, it is recommended to minimize exposure to air pollution by using air purifiers, ventilating indoor spaces, and limiting outdoor activities during periods of high pollution.
5. Immunodeficiency disorders:
Immunodeficiency disorders are rare but potentially serious causes of enlarged adenoids. These disorders occur when the body’s immune system is unable to function properly, leaving the individual more susceptible to infections. In some cases, the adenoids may become chronically enlarged as a result of the body’s inability to effectively fight off recurrent viral or bacterial infections. Examples of immunodeficiency disorders that can lead to enlarged adenoids include human immunodeficiency virus (HIV), common variable immunodeficiency (CVID), and severe combined immunodeficiency (SCID). In these conditions, the immune system is compromised, allowing infections to persist and causing chronic inflammation in the adenoids. Children with immunodeficiency disorders may experience more frequent and severe upper respiratory tract infections, leading to prolonged adenoid enlargement. In addition to causing symptoms such as nasal obstruction, mouth breathing, and sleep disturbances, enlarged adenoids in children with immunodeficiency disorders may also be a sign of a more serious underlying health issue. Prompt diagnosis and appropriate management of the underlying immunodeficiency disorder are essential for preventing complications and improving overall health outcomes.
6. Genetic predisposition:
Genetic predisposition is a factor that can contribute to the development of enlarged adenoids. Some individuals may inherit genetic traits that make them more susceptible to adenoid enlargement, even in the absence of other risk factors such as infections or allergies. These genetic variations can influence the size and structure of the adenoids, as well as the immune system’s response to environmental triggers. For example, some studies have suggested that variations in genes related to inflammation and immune regulation, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α), may be associated with an increased risk of adenoid hypertrophy. Children with a family history of enlarged adenoids or related conditions, such as sleep apnea or chronic sinusitis, may be more likely to develop adenoid enlargement due to shared genetic factors. While genetic predisposition alone may not necessarily lead to enlarged adenoids, it can increase an individual’s risk when combined with other environmental or lifestyle factors. Understanding the role of genetic predisposition in adenoid enlargement can help healthcare providers identify children who may be at higher risk and provide appropriate preventive measures or early interventions.
7. Gastroesophageal reflux disease (GERD):
Gastroesophageal reflux disease (GERD) is a digestive disorder that can cause inflammation and enlargement of the adenoids. GERD occurs when stomach acid and other contents flow back into the esophagus, causing irritation and damage to the lining of the esophagus and other nearby tissues, including the adenoids. When stomach acid repeatedly comes into contact with the adenoids, it can lead to chronic inflammation and swelling. This is particularly problematic in children, as they have a shorter esophagus and are more prone to reflux. The acid exposure can cause the adenoids to become enlarged, leading to symptoms such as nasal congestion, post-nasal drip, cough, and sleep disturbances. In some cases, the enlarged adenoids may further exacerbate GERD symptoms by obstructing the nasal passages and increasing the likelihood of mouth breathing, which can allow more stomach acid to reflux into the esophagus and throat. Treating GERD through lifestyle modifications, medications, or surgery can help reduce inflammation in the adenoids and alleviate associated symptoms. Recognizing the connection between GERD and enlarged adenoids is crucial for providing comprehensive care and improving patient outcomes.
Common signs or symptoms of enlarged adenoids?
Common signs and symptoms of enlarged adenoids include:
1. Mouth breathing:
Mouth breathing is a common indicator of enlarged adenoids in children. When adenoids become enlarged, they can block the nasal passages, making it challenging for the child to breathe through their nose. Consequently, the child may resort to breathing through their mouth, particularly while sleeping. This can result in various symptoms, including dry mouth, halitosis, and chapped lips. Children who habitually breathe through their mouths may also develop a narrow, elongated face and a high, arched palate due to changes in tongue and jaw positioning. Mouth breathing can also impact a child’s sleep quality, leading to snoring and sleep disturbances. In some instances, chronic mouth breathing can affect cognitive development and academic performance due to disrupted sleep and decreased oxygen levels during sleep. If you observe persistent mouth breathing in your child, especially during sleep, it is crucial to seek advice from a healthcare professional to investigate the possibility of enlarged adenoids as the underlying cause.
2. Snoring:
Snoring is a common symptom of enlarged adenoids in children. When the adenoids become enlarged, they can partially or completely block the nasal passages, causing turbulent airflow during breathing. This turbulent airflow can cause the soft tissues in the throat, such as the palate and uvula, to vibrate, resulting in the characteristic snoring sound. Children with enlarged adenoids may snore loudly and frequently, often on a nightly basis. The snoring may be accompanied by other sleep-related symptoms, such as mouth breathing, restless sleep, and frequent awakenings. In some cases, the snoring may be so severe that it causes brief pauses in breathing, known as obstructive sleep apnea. This can lead to reduced oxygenation during sleep, which can have negative impacts on the child’s growth, development, and overall health. If your child is snoring loudly and frequently, it is important to bring this to the attention of a healthcare provider, as it may be a sign of enlarged adenoids or other underlying sleep-related breathing disorders.
3. Sleep apnea:
Sleep apnea is a serious sleep disorder that can be caused by enlarged adenoids in children. When the adenoids are significantly enlarged, they can obstruct the airway during sleep, leading to repeated pauses in breathing. These pauses, known as apneas, can last from a few seconds to minutes and may occur multiple times throughout the night. During an apnea, the child’s blood oxygen levels may drop, causing the brain to briefly wake up to resume breathing. This cycle of apneas and awakenings can severely disrupt the child’s sleep quality and lead to daytime symptoms such as fatigue, irritability, and difficulty concentrating. In severe cases, untreated sleep apnea can lead to growth delays, cardiovascular problems, and neurocognitive impairments. Children with enlarged adenoids and sleep apnea may also exhibit other symptoms, such as loud snoring, gasping or choking during sleep, and restless sleep. If you suspect that your child may have sleep apnea due to enlarged adenoids, it is crucial to consult with a pediatric sleep specialist or otolaryngologist for a comprehensive evaluation and appropriate treatment plan.
4. Nasal congestion or runny nose:
Nasal congestion and a runny nose are common symptoms of enlarged adenoids in children. When the adenoids become enlarged, they can block the nasal passages and hinder proper mucus drainage from the nose and sinuses. This can result in a buildup of mucus in the nasal cavity, leading to persistent nasal congestion or a chronically runny nose in the child. The mucus may appear clear, white, or yellow in color and may be more noticeable in the morning or after the child has been lying down for an extended period. In some cases, the nasal discharge may also be accompanied by post-nasal drip, causing the child to frequently clear their throat or cough. Chronic nasal congestion or a runny nose due to enlarged adenoids can also contribute to other symptoms, such as mouth breathing, snoring, and recurrent sinus infections. If your child is experiencing persistent nasal congestion or a runny nose that does not improve with conventional treatments, such as nasal saline rinses or over-the-counter decongestants, it may indicate enlarged adenoids, and a consultation with a healthcare provider is recommended.
5. Recurrent ear infections:
Recurrent ear infections are a common symptom of enlarged adenoids in children. The adenoids are situated near the opening of the Eustachian tubes, which connect the middle ear to the back of the throat. When the adenoids enlarge, they can obstruct the Eustachian tubes, hindering proper drainage of fluid from the middle ear. This creates a favorable environment for bacterial growth, resulting in recurrent middle ear infections, or otitis media. Children with enlarged adenoids may frequently experience ear infections, often accompanied by symptoms like ear pain, fever, irritability, and hearing loss. In some cases, these infections can become chronic, leading to persistent fluid accumulation in the middle ear, known as otitis media with effusion. This can cause long-term hearing issues and may affect the child’s speech and language development. If your child is experiencing recurrent ear infections, it is crucial to seek advice from a healthcare professional to determine if enlarged adenoids are the underlying cause. Treatment for enlarged adenoids, whether through medication or surgical removal, can often prevent future ear infections and associated complications.
6. Sinusitis:
Sinusitis is a common complication of enlarged adenoids in children. The sinuses are hollow spaces in the facial bones that are lined with mucous membranes. When the adenoids become enlarged, they can obstruct the drainage pathways of the sinuses, leading to a buildup of mucus and an increased risk of bacterial infections. Children with enlarged adenoids may develop chronic sinusitis, characterized by persistent symptoms such as nasal congestion, thick nasal discharge, facial pain or pressure, and headaches. In some cases, the child may also experience a reduced sense of smell or taste, bad breath, and a cough that worsens at night. Sinusitis can significantly impact a child’s quality of life, leading to missed school days, sleep disturbances, and general discomfort. If left untreated, chronic sinusitis can also lead to more serious complications, such as orbital cellulitis or meningitis. If your child is experiencing symptoms of chronic sinusitis, it is important to consult with a healthcare provider to determine if enlarged adenoids may be the underlying cause. Treating the enlarged adenoids, either through medication or surgical removal, can often help alleviate sinusitis symptoms and prevent future infections.
7. Difficulty swallowing:
Difficulty swallowing, also known as dysphagia, can be a symptom of enlarged adenoids in children. When the adenoids become significantly enlarged, they can cause a feeling of obstruction in the throat or may lead to frequent swallowing. This can result in challenges or discomfort when swallowing solid foods or liquids. In some instances, enlarged adenoids may also induce gagging, choking, or a sensation of food or liquid moving up the back of the nose during swallowing (nasal regurgitation). These symptoms can be distressing for the child and may result in a decreased appetite or avoidance of certain foods. Difficulty swallowing due to enlarged adenoids may also be accompanied by other symptoms, such as mouth breathing, snoring, or sleep apnea. If your child is experiencing persistent difficulty swallowing, it is crucial to seek advice from a healthcare professional to identify the underlying cause. In some cases, enlarged adenoids may be the cause and can be treated with medication or surgical removal to alleviate the swallowing difficulties and prevent potential complications, such as aspiration or malnutrition.
8. Voice changes:
Changes in voice can be a symptom of enlarged adenoids in children. When the adenoids become enlarged, they can block the nasal passages, causing the child to breathe through their mouth. This can result in a condition known as “adenoid speech” or “hyponasal speech,” which is characterized by a muffled, nasal quality in the child’s voice. Enlarged adenoids can also cause the child to sound like they are speaking through their nose, a condition known as hypernasality. In some cases, the child’s speech may be hard to understand, especially when producing certain sounds that require proper airflow through the nose, such as “m,” “n,” or “ng.” These voice changes can be frustrating for the child and may affect their social interactions and self-esteem. In addition to voice changes, enlarged adenoids can also lead to other symptoms like mouth breathing, snoring, and sleep apnea. If you notice persistent changes in your child’s voice, it is important to seek advice from a healthcare provider to determine if enlarged adenoids may be the underlying issue. Treating the enlarged adenoids, either through medication or surgical removal, can often help restore normal speech patterns and improve the child’s overall quality of life.
9. Facial changes:
Facial changes can indicate chronic enlargement of adenoids in children. When adenoids remain enlarged over time, they can result in prolonged mouth breathing, which can lead to modifications in facial growth and development. Children with enlarged adenoids may develop a condition known as “adenoid facies” or “long face syndrome,” which is characterized by specific facial features. These changes include a lengthened face, open mouth posture, narrow upper jaw, high arched palate, and prominent upper teeth. Continuous mouth breathing can cause the tongue to rest in a lower position, impacting the growth of the upper and lower jaws. Furthermore, the open mouth posture can cause dry lips, gum irritation, and an increased risk of dental issues like tooth decay and gingivitis. These facial alterations can not only affect the child’s appearance but also lead to functional problems such as difficulty biting and chewing food properly. If you observe changes in your child’s facial structure along with other symptoms of enlarged adenoids, such as mouth breathing, snoring, or recurrent ear infections, it is crucial to seek advice from a healthcare professional. Early intervention and treatment of enlarged adenoids can help prevent or alleviate long-term facial changes and related complications.
10 Sleep disturbances:
Sleep disturbances are a common symptom of enlarged adenoids in children. When adenoids become enlarged, they can block the airway during sleep, resulting in various sleep-related problems. Children with enlarged adenoids may have trouble falling asleep or staying asleep throughout the night. They may wake up frequently, move around in bed, or have restless sleep patterns. These sleep disturbances may also be accompanied by other symptoms, such as loud snoring, breathing through the mouth, and even sleep apnea. Sleep apnea is a serious condition characterized by repeated pauses in breathing during sleep, which can cause low oxygen levels in the blood and strain on the cardiovascular system. Children with sleep apnea may wake up briefly, gasp for air, or feel like they are choking during the night. The disrupted sleep patterns caused by enlarged adenoids can lead to daytime symptoms like tiredness, irritability, difficulty focusing, and behavioral issues. Over time, chronic sleep disturbances can affect a child’s growth, development, and overall health. If you notice that your child is experiencing persistent sleep disturbances along with other symptoms of enlarged adenoids, it is important to seek medical advice for a comprehensive evaluation and appropriate treatment plan.
How can enlarged adenoids be diagnosed?
Enlarged adenoids can be diagnosed through a combination of physical examination, patient history, and imaging studies. The following methods are commonly used to diagnose enlarged adenoids:
1. Physical examination:
A physical examination is an essential step in diagnosing enlarged adenoids in children. During the examination, a healthcare provider will focus on the child’s nose, throat, and ears, searching for signs that may suggest the presence of enlarged adenoids. The provider may use a lighted instrument, such as an otoscope or a tongue depressor, to improve visualization of these areas. They will look for signs of nasal obstruction, such as visible narrowing of the nasal passages or the presence of mucus or other secretions. The provider will also assess for signs of mouth breathing, a common consequence of enlarged adenoids. Additionally, they may examine the child’s tonsils, as enlarged tonsils often accompany enlarged adenoids. The healthcare provider will also observe the child’s facial features, looking for characteristics such as an elongated face or open mouth posture, which can indicate chronic mouth breathing due to enlarged adenoids. By conducting a comprehensive physical examination and correlating the findings with the child’s reported symptoms, the healthcare provider can gather crucial information to support the diagnosis of enlarged adenoids.
2. Patient history:
Obtaining a thorough patient history is crucial for diagnosing enlarged adenoids in children. During the consultation, the healthcare provider will interview the parents or caregivers to gather information about the child’s symptoms and medical background. They will inquire about the presence and duration of symptoms such as snoring, mouth breathing, nasal congestion, or difficulty sleeping. The provider may also ask about the frequency and severity of these symptoms, as well as whether they have been persistent or intermittent. Additionally, the healthcare provider will inquire about the child’s history of recurrent ear infections, sinusitis, or upper respiratory tract infections, as these conditions are commonly linked to enlarged adenoids. They may also ask about the child’s overall health, growth, and development, as enlarged adenoids can sometimes result in growth delays or other health problems. The provider will also inquire about any family history of sleep disorders, allergies, or other related conditions. By collecting a comprehensive patient history, the healthcare provider can identify trends and risk factors that may contribute to the development of enlarged adenoids, enabling them to make an accurate diagnosis and create an appropriate treatment plan.
3. Nasopharyngoscopy:
Nasopharyngoscopy is a valuable diagnostic tool for directly visualizing enlarged adenoids in children. This procedure involves inserting a thin, flexible tube called an endoscope through the child’s nostril. The endoscope is equipped with a light and a tiny camera, which allows the healthcare provider to examine the nasal passages, the back of the throat, and the adenoids in real-time. During the nasopharyngoscopy, the provider can assess the size and appearance of the adenoids, as well as their impact on the airway. They can look for signs of obstruction, inflammation, or infection in the adenoid tissue. The procedure also allows the provider to evaluate the child’s nasal anatomy, including the presence of any structural abnormalities or other factors contributing to nasal obstruction. Nasopharyngoscopy is generally well-tolerated by children, and it can be performed in an outpatient setting using local anesthesia or mild sedation, depending on the child’s age and cooperation. The results of the nasopharyngoscopy, combined with the child’s symptoms and physical examination findings, can provide the healthcare provider with a comprehensive understanding of the adenoid enlargement and guide the development of an appropriate treatment plan.
4. Lateral neck X-ray:
Lateral neck X-ray is an imaging technique that can aid in the diagnosis of enlarged adenoids in children. This type of X-ray provides a lateral view of the child’s neck, allowing healthcare providers to evaluate the size and position of the adenoids in relation to the airway. During the procedure, the child is positioned laterally, and the X-ray beam is directed through the neck to produce an image on a special film or digital detector. The resulting X-ray image can display the soft tissue structures in the neck, including the adenoids, which appear as a mass or shadow in the nasopharyngeal area. Healthcare providers can measure the size of the adenoids and compare them to the size of the airway to determine if they are causing significant obstruction. It is important to note that while lateral neck X-rays can provide valuable information, they are not as precise as nasopharyngoscopy in assessing adenoid size and may not detect minor degrees of enlargement. Additionally, X-rays involve exposure to ionizing radiation, so they should only be used when necessary and in accordance with appropriate guidelines.
5. Sleep study (polysomnography):
A sleep study, also known as polysomnography, is a comprehensive diagnostic test used to evaluate sleep disorders, including obstructive sleep apnea caused by enlarged adenoids in children. This study is typically conducted in a specialized sleep laboratory or hospital setting, where the child’s sleep patterns, breathing, and other physiological parameters are monitored overnight. Various sensors and electrodes are attached to the child’s body to record brain activity (EEG), eye movements (EOG), muscle activity (EMG), heart rate (ECG), oxygen levels in the blood (pulse oximetry), and chest and abdominal movements. A small microphone is also placed near the child’s throat to record snoring sounds. Throughout the night, a trained sleep technician monitors the child’s sleep and records any disturbances or abnormalities. The data collected during the sleep study is then analyzed by a sleep specialist to determine the presence and severity of obstructive sleep apnea caused by enlarged adenoids. The sleep study can provide valuable information about the child’s sleep architecture, the number and duration of apneas or hypopneas (partial airway obstruction), and the impact of these events on oxygen levels and sleep quality. This information helps the healthcare provider make an accurate diagnosis and develop an appropriate treatment plan for managing enlarged adenoids and associated sleep disorders.
6. Acoustic rhinometry:
Acoustic rhinometry is a non-invasive diagnostic technique used to evaluate nasal obstruction, which may result from enlarged adenoids in children. This method utilizes sound waves to measure the cross-sectional area and volume of the nasal cavity. During the procedure, a small, handheld device is inserted into the child’s nostril entrance. The device emits sound waves that pass through the nasal cavity and reflect back upon encountering resistance, such as the adenoids or other blockages. The reflected sound waves are then analyzed by computer software to generate a detailed map of the nasal cavity, displaying the area and volume at various distances from the nostril. This information assists healthcare providers in determining the extent and location of nasal obstruction due to enlarged adenoids. Acoustic rhinometry is a rapid, painless, and child-friendly procedure that does not involve exposure to radiation. It can be conducted in a clinical setting without the need for sedation or anesthesia. The results of acoustic rhinometry, in conjunction with other diagnostic tools and the child’s symptoms, can help healthcare providers assess the impact of enlarged adenoids on nasal breathing and inform treatment decisions.
7. Allergy tests:
Allergy tests can be used to diagnose enlarged adenoids in children, as allergies are a common factor in adenoid enlargement. Chronic allergies can lead to inflammation in the nasal passages and adenoid tissue, causing the adenoids to become enlarged over time. Healthcare providers may recommend allergy tests to determine if allergies are contributing to a child’s enlarged adenoids. The two most common types of allergy tests are skin prick tests and blood tests. Skin prick tests involve placing small drops of allergen extracts on the skin and pricking it to allow the allergen to enter the surface layer. If the child is allergic to a substance, a bump or hive will appear at the test site. Blood tests, such as the radioallergosorbent test (RAST) or immunoassay capture test (ImmunoCAP), measure allergen-specific antibodies in the blood to identify specific allergens triggering the child’s allergic response and contributing to adenoid enlargement. Managing these allergies through medications, immunotherapy, or environmental modifications can help reduce inflammation in the adenoids and alleviate associated symptoms.
Once a diagnosis of enlarged adenoids is made, the healthcare provider can recommend an appropriate treatment plan based on the child’s age, severity of symptoms, and overall health.
Treatments for enlarged adenoids
There are several treatment options available for managing enlarged adenoids in children, depending on the severity of the condition and the associated symptoms. The main treatments include:
1. Watchful waiting:
Watchful waiting is a conservative approach to managing enlarged adenoids in children, particularly when the symptoms are mild and not significantly impacting the child’s quality of life. In this approach, the healthcare provider closely monitors the child’s condition over time, without immediately recommending surgical intervention or aggressive treatments. The rationale behind watchful waiting is that, in some cases, the adenoids may shrink naturally as the child grows and their immune system matures. This is because the adenoids are most active during the early years of life and tend to regress in size by the age of 5-7 years. During the watchful waiting period, the healthcare provider will regularly assess the child’s symptoms, growth, and development to ensure that the enlarged adenoids are not causing any significant complications or hindering the child’s overall well-being. If the symptoms worsen or fail to resolve over time, the healthcare provider may then recommend more active treatment options, such as medications or surgery, to address the issue. Watchful waiting allows for a more conservative and individualized approach to managing enlarged adenoids, while avoiding unnecessary interventions in cases where the condition may resolve on its own.
2. Medications:
Medications are an effective treatment option for managing symptoms associated with enlarged adenoids in children. The specific type of medication prescribed will depend on the symptoms and underlying cause of the adenoid enlargement. Nasal corticosteroid sprays, such as fluticasone or mometasone, can reduce inflammation in the nasal passages and adenoid tissue, improving breathing and reducing nasal congestion. Decongestants, such as pseudoephedrine or phenylephrine, may provide short-term relief of nasal obstruction, but should be used cautiously in young children. Antihistamines, like cetirizine or loratadine, can help control allergic responses and reduce inflammation if allergies are contributing to adenoid enlargement. In cases of bacterial infection, such as sinusitis or ear infections, antibiotics may be prescribed to eliminate the infection and prevent complications. It is important to carefully follow healthcare provider instructions when administering medications and promptly report any side effects or concerns. While medications can provide symptomatic relief and manage consequences of enlarged adenoids, they may not address the underlying cause, and surgical intervention may still be necessary in some cases.
3. Allergy management:
Managing allergies is a crucial aspect of treating enlarged adenoids in children when allergies are identified as a contributing factor. Allergic reactions can lead to chronic inflammation in the nasal passages and adenoid tissue, resulting in enlargement and related symptoms. The initial step in allergy management involves identifying the specific allergens that trigger the child’s symptoms through allergy tests, such as skin prick tests or blood tests. Once the allergens are pinpointed, healthcare providers may suggest various strategies to control the allergic response. This may involve the use of antihistamines to block the effects of histamine, a chemical released during an allergic reaction that causes inflammation and mucus production. Nasal corticosteroid sprays may also be prescribed to reduce inflammation in the nasal passages and adenoids. In certain cases, allergen immunotherapy (allergy shots) may be recommended to help desensitize the child’s immune system to specific allergens over time. This process entails administering gradually increasing doses of the allergen to build tolerance and decrease the severity of allergic reactions. Environmental modifications, such as using air purifiers, keeping windows closed during high pollen seasons, and regularly washing bedding, can also aid in minimizing exposure to allergens and reducing symptoms. By effectively managing allergies, healthcare providers can assist in reducing adenoid inflammation and alleviating associated symptoms in children with enlarged adenoids.
4. Positive airway pressure (PAP) therapy:
Positive airway pressure (PAP) therapy is a non-surgical treatment option for children with enlarged adenoids who experience obstructive sleep apnea (OSA). OSA occurs when the enlarged adenoids partially or completely block the airway during sleep, leading to pauses in breathing, reduced oxygen levels, and disrupted sleep. PAP therapy involves the use of a machine that delivers pressurized air through a mask worn over the nose or mouth during sleep. The most common type of PAP therapy used for children is continuous positive airway pressure (CPAP). The CPAP machine generates a constant stream of pressurized air, which helps keep the airway open and prevents the adenoids from obstructing breathing. This allows the child to maintain normal breathing patterns and oxygen levels throughout the night, leading to improved sleep quality and reduced daytime symptoms associated with OSA. PAP therapy is generally well-tolerated by children, and the pressure settings can be adjusted to ensure comfort and effectiveness. While PAP therapy can effectively manage OSA symptoms related to enlarged adenoids, it does not address the underlying cause of the adenoid enlargement. In some cases, the healthcare provider may recommend PAP therapy as a temporary measure while the child awaits surgical treatment or as an alternative for children who may not be suitable candidates for surgery.
5. Adenoidectomy:
Adenoidectomy is a surgical procedure that involves the removal of the adenoids and is typically recommended for children with severe or persistent symptoms related to enlarged adenoids. It is often considered when other conservative treatments, such as medications or watchful waiting, have not been effective in managing the child’s symptoms. During an adenoidectomy, the child is placed under general anesthesia, and the surgeon removes the adenoid tissue through the mouth using special instruments. The procedure is relatively short, usually lasting less than an hour, and does not require any external incisions. Following the surgery, children may experience some pain, swelling, and discomfort in the throat, which can be managed with pain medications and soft foods. Most children recover quickly after an adenoidectomy and can resume normal activities within a week. Adenoidectomy has been shown to be highly effective in treating the symptoms associated with enlarged adenoids, such as obstructive sleep apnea, recurrent ear infections, and chronic sinusitis. By removing the enlarged adenoid tissue, the procedure helps restore normal breathing patterns, improves sleep quality, and reduces the frequency of infections. In some cases, an adenoidectomy may be combined with a tonsillectomy (removal of the tonsils) if both the adenoids and tonsils are significantly enlarged and causing problems. The decision to proceed with an adenoidectomy will depend on the severity of the child’s condition and the potential benefits of the surgery, as determined by the healthcare provider in consultation with the family.
6. Tonsillectomy:
Tonsillectomy is a surgical procedure that involves the removal of the tonsils and is often performed in conjunction with an adenoidectomy when both the adenoids and tonsils are significantly enlarged and causing problems. The tonsils are two small glands located at the back of the throat, and like the adenoids, they can become chronically inflamed and enlarged due to recurrent infections or allergies. When enlarged tonsils and adenoids obstruct the airway, contribute to sleep apnea, or cause frequent infections, a combined adenotonsillectomy may be recommended. During this procedure, the child is placed under general anesthesia, and the surgeon removes both the adenoids and tonsils through the mouth. Recovery after an adenotonsillectomy may take a bit longer compared to an adenoidectomy alone, with most children requiring 1-2 weeks to fully recover. Pain management, soft foods, and rest are essential during the recovery period. Removing both the adenoids and tonsils can provide more comprehensive relief from symptoms such as obstructive sleep apnea, snoring, recurrent ear infections, and chronic throat infections. By addressing both sites of obstruction and infection, the combined procedure can lead to significant improvements in the child’s breathing, sleep, and overall quality of life.
7. Myofunctional therapy:
Myofunctional therapy is a non-surgical treatment approach that may be recommended for children with enlarged adenoids, particularly in cases where mouth breathing, tongue thrusting, or other orofacial muscle imbalances are present. This therapy involves teaching the child specific exercises and techniques to strengthen and retrain the muscles of the mouth, tongue, and throat. The goal of myofunctional therapy is to promote proper breathing patterns, improve nasal breathing, and correct any dysfunctional habits that may contribute to or exacerbate the symptoms associated with enlarged adenoids. During myofunctional therapy sessions, a trained therapist works with the child to perform a series of exercises that target the lips, tongue, cheeks, and soft palate. These exercises may include tongue positioning techniques, lip and cheek strengthening, and proper swallowing patterns. The child is also taught to become more aware of their breathing patterns and to consciously practice nasal breathing. By improving the strength and coordination of the orofacial muscles, myofunctional therapy can help alleviate symptoms such as mouth breathing, snoring, and sleep apnea, which are often associated with enlarged adenoids. This therapy can be used in conjunction with other treatments, such as medications or surgery, or as a standalone approach in milder cases. Myofunctional therapy requires consistent practice and patience, as progress may be gradual, but it can lead to long-lasting improvements in breathing, swallowing, and overall orofacial function in children with enlarged adenoids.
Prevention of enlarged adenoids
While it may not always be possible to prevent enlarged adenoids, there are several strategies that can help reduce the risk or minimize the severity of the condition. These prevention measures include:
1. Maintaining good hygiene:
Maintaining good hygiene is crucial in preventing the development of enlarged adenoids in children. One of the main causes of adenoid enlargement is recurrent viral or bacterial infections, which can result in chronic inflammation of the adenoid tissue. Encouraging children to practice good hand hygiene can help reduce the spread of infectious agents that contribute to this condition. This includes teaching children to wash their hands regularly with soap and water, especially before eating, after using the bathroom, and after coming into contact with shared surfaces or objects. It is also important to educate children about the importance of not touching their face, particularly their nose and mouth, with unwashed hands. In addition to hand hygiene, promoting good oral hygiene habits, such as regular tooth brushing and flossing, can help decrease the risk of oral infections that may lead to adenoid inflammation. By incorporating good hygiene practices into a child’s daily routine, parents can enhance their child’s immune system and reduce the chances of developing enlarged adenoids.
2. Avoiding irritants:
Avoiding irritants is an important strategy for preventing the development of enlarged adenoids in children. Exposure to environmental irritants, such as secondhand smoke, air pollution, and strong chemical odors, can lead to chronic inflammation in the nasal passages and adenoid tissue, resulting in enlargement over time. Parents and caregivers can reduce their child’s risk of developing this condition by minimizing exposure to these irritants. This may involve creating a smoke-free environment at home and in the car, as well as limiting outdoor activities during times of high air pollution or allergen levels. Using natural or mild cleaning products and avoiding strong perfumes or scented products can also help reduce exposure to potentially irritating chemicals. When irritants cannot be completely avoided, air purifiers with HEPA filters can help remove harmful particles and pollutants from the air, creating a cleaner and healthier environment for the child. By taking proactive steps to minimize a child’s exposure to irritants, parents can reduce inflammation in the adenoids and lower the risk of developing enlarged adenoids.
3. Managing allergies:
Managing allergies is a crucial step in preventing the development of enlarged adenoids in children. Allergic reactions can cause chronic inflammation in the nasal passages and adenoid tissue, leading to enlargement and associated symptoms. If a child has been diagnosed with allergies or is suspected to have allergies, it is important to work with a healthcare provider to identify the specific allergens triggering their symptoms and develop an appropriate management plan. This may involve the use of antihistamines or nasal corticosteroid sprays to control allergy symptoms and reduce inflammation. In some cases, allergen immunotherapy (allergy shots) may be recommended to help desensitize the child’s immune system to specific allergens over time. In addition to medical management, environmental modifications can play a significant role in reducing a child’s exposure to allergens. This may include strategies such as using allergen-proof bedding covers, regularly washing bedding in hot water, keeping windows closed during high pollen seasons, and using air purifiers with HEPA filters to remove allergens from the air. By consistently managing allergies through a combination of medical treatment and environmental control measures, parents can help reduce inflammation in their child’s adenoids and lower the risk of developing enlarged adenoids.
4. Treating infections promptly:
Prompt treatment of infections is a crucial strategy for preventing the development of enlarged adenoids in children. Recurrent viral or bacterial infections, such as upper respiratory tract infections, sinusitis, or ear infections, can result in chronic inflammation and enlargement of the adenoid tissue. Untreated or improperly managed infections can persist and cause long-term damage to the adenoids. To avoid this, parents should be vigilant in recognizing signs and symptoms of infections in their children and seek medical attention promptly. This may involve consulting a pediatrician when the child experiences persistent symptoms like nasal congestion, cough, fever, or ear pain. If a bacterial infection is suspected, the healthcare provider may prescribe antibiotics to clear the infection and prevent complications. It is essential to adhere to the prescribed treatment plan and complete the full course of antibiotics, even if the child’s symptoms improve before finishing the medication. Along with prompt medical treatment, parents can support their child’s immune system and reduce infection risk by promoting a healthy lifestyle, including a balanced diet, regular exercise, and sufficient sleep. By addressing infections promptly and effectively, parents can help prevent chronic inflammation and enlargement of their child’s adenoids.
5. Breastfeeding:
Breastfeeding plays a significant role in preventing the development of enlarged adenoids in infants and young children. Breast milk contains various immune-boosting compounds, such as antibodies, white blood cells, and other protective factors that strengthen the child’s immune system and reduce the risk of infections. Maternal antibodies provide passive immunity to the child, aiding in the fight against viruses and bacteria that can cause respiratory infections and inflammation of the adenoid tissue. Breastfeeding also promotes the proper development of oral and facial muscles, reducing the risk of mouth breathing and other orofacial issues that may contribute to adenoid enlargement. Studies have shown that breastfed infants experience fewer and less severe respiratory infections compared to formula-fed infants, potentially lowering the risk of chronic inflammation and adenoid enlargement. The World Health Organization recommends exclusive breastfeeding for the first six months of life, followed by continued breastfeeding alongside appropriate complementary foods for up to two years or longer. By providing the unique immunological and developmental benefits of breast milk, mothers can help protect their children from infections and reduce the risk of enlarged adenoids.
6. Vaccinations:
Vaccinations are essential in preventing the development of enlarged adenoids in children by protecting them from infections that can lead to adenoid inflammation and enlargement. Certain vaccines, such as the pneumococcal conjugate vaccine (PCV) and the Haemophilus influenzae type b (Hib) vaccine, help shield children from bacterial infections that can cause upper respiratory tract infections, sinusitis, and ear infections. By reducing the frequency and severity of these infections, vaccinations can help prevent the chronic inflammation that results in enlarged adenoids. Additionally, the influenza vaccine can protect children from the flu, which can also contribute to adenoid inflammation. Following the recommended childhood vaccination schedule, as outlined by health organizations like the Centers for Disease Control and Prevention (CDC) or the World Health Organization (WHO), can offer comprehensive protection against a wide range of infectious diseases. This includes timely administration of vaccines such as PCV, Hib, influenza, measles-mumps-rubella (MMR), and diphtheria-tetanus-pertussis (DTaP). By keeping up with vaccinations, parents can help boost their child’s immune system, decrease the risk of infections, and consequently, reduce the likelihood of developing enlarged adenoids. Regular check-ups with a pediatrician can ensure that a child receives all necessary vaccinations at the appropriate times.
7. Healthy lifestyle:
Maintaining a healthy lifestyle is an important strategy for preventing the development of enlarged adenoids in children. A balanced diet, regular exercise, and adequate sleep can all contribute to a strong immune system, which helps protect against infections and reduces the risk of chronic inflammation in the adenoid tissue. Parents should encourage their children to eat a variety of nutrient-dense foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats, to provide the necessary vitamins, minerals, and antioxidants for optimal immune function. Regular physical activity, such as playing outdoors, participating in sports, or engaging in other age-appropriate exercises, can also help boost the immune system and promote overall health. Additionally, ensuring that children get enough quality sleep each night is crucial for maintaining a healthy immune system. The American Academy of Sleep Medicine recommends that children aged 6-12 years old get 9-12 hours of sleep per night, while teenagers aged 13-18 years old should aim for 8-10 hours. Creating a consistent bedtime routine and promoting good sleep hygiene habits can help children get the restful sleep they need to support their immune health. By fostering a healthy lifestyle through proper nutrition, regular exercise, and adequate sleep, parents can help strengthen their child’s immune system and reduce the risk of developing enlarged adenoids.
8. Addressing mouth breathing:
Addressing mouth breathing is a crucial strategy for preventing the enlargement of adenoids in children. Chronic mouth breathing can result in various health issues, including an increased susceptibility to respiratory infections, which can lead to inflammation and enlargement of the adenoids. When a child breathes through their mouth, the air entering the lungs is not as effectively filtered, humidified, or warmed compared to breathing through the nose. This can cause dryness and irritation in the oral cavity and respiratory tract, making the child more prone to infections. Furthermore, mouth breathing can impact facial structure and dental development, exacerbating the issue. To address mouth breathing, parents should collaborate with a healthcare provider to identify and treat any underlying causes, such as allergies, a deviated septum, or enlarged tonsils. Managing these conditions can promote nasal breathing and reduce the risk of respiratory infections. In some cases, myofunctional therapy may be recommended to retrain the child’s oral and facial muscles and encourage proper breathing patterns. Parents can also promote nasal breathing by reminding the child to keep their lips closed and breathe through their nose, especially during activities like reading or watching television. By addressing mouth breathing and encouraging healthy nasal breathing habits, parents can help lower the risk of respiratory infections and prevent the enlargement of adenoids in their children.
It is important to note that some children may be more susceptible to developing enlarged adenoids due to factors such as genetics, facial structure, or underlying health conditions. Regular check-ups with a pediatrician can help monitor a child’s adenoid health and address any concerns promptly.