According to article, Acromegaly is a rare hormonal disorder often caused by a benign pituitary adenoma, resulting in excessive production of growth hormone (GH) and subsequent elevation of insulin-like growth factor-1 (IGF-1). This leads to abnormal enlargement of body parts such as hands, feet, and facial bones, as well as systemic symptoms like joint pain, muscle weakness, and altered glucose metabolism. Symptoms develop slowly, making early diagnosis challenging but crucial to prevent severe complications including hypertension, heart disease, diabetes, and respiratory issues. Treatment aims to normalize GH levels through surgery, medication, or radiation therapy to reduce health risks and improve quality of life.
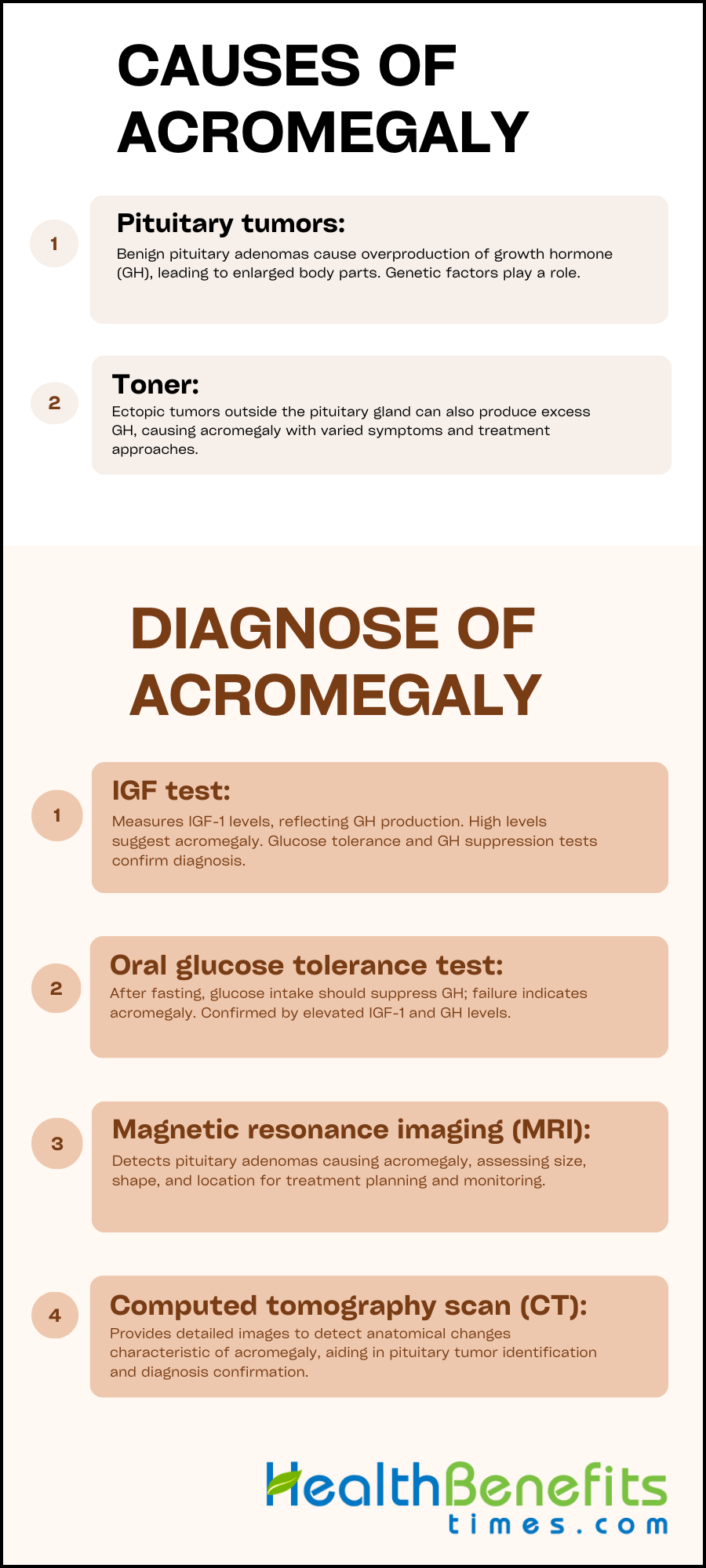
Causes of Acromegaly
Acromegaly is a hormonal disorder resulting from hormonal dysregulation, primarily due to the overproduction of growth hormone (GH), often caused by a benign pituitary adenoma. This excess GH leads to abnormal growth, such as enlarged body parts and thickened skin, alongside various health complications. While a pituitary tumor is the main etiological factor, other causes include pituitary gland hyperplasia, ectopic GH-secreting tumors, and genetic mutations impacting GH regulation. Understanding these causes is crucial for effective diagnosis and treatment, as they reveal the disorder’s pathophysiology and inform targeted therapeutic approaches. The complexity of acromegaly’s origins, including genetic and hormonal factors, underscores the importance of a comprehensive understanding to mitigate the significant impact it has on individuals’ lives.
1. Pituitary tumors
Acromegaly is primarily caused by somatotroph adenomas, which are benign tumors of the pituitary gland that result in excessive production of growth hormone (GH) and insulin-like growth factor 1 (IGF-1). This leads to the gradual enlargement of body parts such as hands, feet, and facial features. These tumors account for over 95% of cases and can vary in size and location, impacting the severity of the condition. The exact cause of pituitary adenomas is not fully understood, but genetic factors and mutations in genes such as GNAS and USP8 are linked to an increased risk. Early detection and treatment are crucial due to the slow-growing nature of these tumors, which can delay the onset of symptoms. In rare cases, acromegaly can also result from non-pituitary tumors. Understanding the genetic and molecular characteristics of these adenomas is essential for developing personalized treatments and improving patient outcomes, particularly in pediatric cases where diagnosis can be more challenging.
2. Non-pituitary tumors
Acromegaly, typically caused by pituitary adenomas, can also be caused by ectopic non-pituitary tumors that are often neuroendocrine in nature and located in the pancreas, lungs, or adrenal glands. These rare tumors may produce growth hormone-releasing hormone (GHRH) or, less commonly, growth hormone (GH) itself, leading to an overproduction of growth hormone and resulting in symptoms such as enlarged hands and feet, coarsened facial features, and systemic complications, including severe hyperglycemia and, in some cases, diabetic ketoacidosis. Due to their small size and varied locations, these tumors are difficult to diagnose. Treatment may differ from pituitary-related acromegaly and can include surgical removal, radiation therapy, or medication to control hormone production, highlighting the importance of early detection and personalized management strategies.
Symptoms of Acromegaly
Acromegaly is a rare, chronic hormonal disorder characterized by excessive production of growth hormone after closure of the growth plates. This condition manifests with gradual onset of symptoms, such as enlargement of hands and feet, coarsening of facial features, deepening of voice, and increased sweating. These symptoms result from tissue and organ overstimulation, underscoring the importance of early detection and management to minimize their impact on quality of life. Understanding the various physical, metabolic, and systemic changes associated with acromegaly is essential for prompt diagnosis and treatment. The following are some of the most common symptoms associated with acromegaly:
- Body odor
- Blood in the stool
- Carpal tunnel syndrome
- Decreased muscle strength (weakness)
- Decreased peripheral vision
- Dental problems, gaps between the teeth
- Easy fatigue
- Enlarged tongue
- Excessive height (when excess GH production begins in childhood)
- Excessive sweating
- Headache
- Heart enlargement, which can cause fainting or shortness of breath
- Hoarseness
- Jaw pain
- Joint pain, limited joint movement, swelling of the bony areas around a joint
- Large bones of the face, large jaw and tongue, widely spaced teeth
- Large feet (change in shoe size)
- Large hands (change in ring or glove size)
- Large glands in the skin (sebaceous glands) causing oily skin,
- thickening of the skin, skin tags (growths)
- Sleep apnea
- Widened fingers or toes, with swelling, redness, and pain
- Colon polyps
- Excess hair growth in females (hirsutism)
- High blood pressure
- Type 2 diabetes
- Thyroid enlargement
- Weight gain
How do doctors diagnose acromegaly?
The diagnosis of acromegaly, a rare hormonal disorder characterized by excessive growth hormone production, involves a thorough and comprehensive process that incorporates clinical evaluations, laboratory tests, and imaging studies. Physicians initially assess the patient’s symptoms, which commonly involve gradual enlargement of extremities and facial features. To accurately confirm acromegaly and distinguish it from other conditions, healthcare providers measure hormone levels and may utilize imaging techniques to examine the pituitary gland, with genetic testing utilized in specific cases. This systematic diagnostic approach guarantees that each treatment plan is customized to the individual’s condition, enabling effective management of the disorder.
1. IGF test
According to article, Acromegaly is diagnosed through a combination of hormonal testing and clinical assessment. The primary test measures insulin-like growth factor-1 (IGF-1) levels in the blood, which reflect the average production of growth hormone (GH) by the pituitary gland. Elevated IGF-1 levels suggest acromegaly, indicating excess GH production. To confirm the diagnosis, doctors may perform a glucose tolerance test to check if GH levels decrease in response to glucose ingestion, as they should in healthy individuals. In acromegaly patients, GH levels typically do not fall. Additionally, a GH suppression test may be used, where medication should lower GH levels; persistent high levels despite this indicate acromegaly. It is crucial to interpret IGF-1 levels alongside other clinical and laboratory findings, including imaging studies, to ensure accurate diagnosis and to avoid misinterpretation due to factors like dietary influences, assay issues, or other medical conditions. Effective management of acromegaly requires understanding these nuances and the potential for discordant GH and IGF-1 levels, which may necessitate further monitoring.
2. Oral glucose tolerance test
The oral glucose tolerance test (OGTT) is an essential tool in diagnosing acromegaly, a condition characterized by excessive growth hormone (GH) production. During the OGTT, patients fast overnight and then consume a glucose solution. Blood samples are collected before and at regular intervals after glucose intake to measure GH and insulin-like growth factor-1 (IGF-1) levels. Normally, glucose suppresses GH secretion, but in acromegaly, GH levels remain high, failing to decrease adequately in response to glucose. A GH nadir of ≥ 0.4 µg/L during the test suggests acromegaly, especially when accompanied by elevated IGF-1 levels. However, the OGTT is just one component of a comprehensive diagnostic process that may include additional tests and imaging studies, and it requires evaluation by an endocrinologist to confirm the diagnosis and formulate a treatment plan.
3. Magnetic resonance imaging
Magnetic Resonance Imaging (MRI) is an essential tool for diagnosing acromegaly, primarily by detecting abnormal growths in the pituitary gland, such as pituitary adenomas that secrete excess growth hormone. MRI scans provide high-resolution images that reveal the size, shape, and location of these tumors, which is vital for crafting an effective treatment plan. In ectopic acromegaly, MRI is instrumental in identifying the causes and evaluating treatment response, with T2-weighted signal intensity being a significant indicator, particularly in patients treated with pasireotide. Additionally, MRI is useful for monitoring potential cardiovascular complications common in acromegaly and assessing the tumor’s impact on nearby structures, including the optic chiasm. The detailed imaging assists in determining the appropriate course of treatment, which may involve surgery, medication, or radiation, and is crucial for ongoing management, including checking for tumor recurrence.
4. Computed tomography scan
According to article, Computed Tomography (CT) scans are instrumental in diagnosing acromegaly, a condition often caused by a pituitary adenoma that secretes excessive growth hormone, leading to increased insulin-like growth factor-I and systemic complications. These scans provide detailed images that can reveal anatomical changes such as thickened skulls and enlarged extremities, characteristic of acromegaly. CT scans are particularly valuable for pinpointing the size and location of pituitary tumors, which is essential for treatment planning. Early detection is critical due to acromegaly’s slow progression and vague symptoms, which can delay diagnosis. Alongside CT imaging, hormonal blood tests are typically conducted to confirm elevated hormone levels, providing a comprehensive approach to diagnosing and managing this rare hormonal disorder.
Treatment Options for Acromegaly
In the management of acromegaly, a condition characterized by excessive production of growth hormone, treatment should be tailored to the severity of the disease, the patient’s health status, and potential complications. A comprehensive approach includes surgical removal of the pituitary adenoma, pharmacological treatments such as somatostatin analogs, growth hormone receptor antagonists, and dopamine agonists to regulate hormone levels, as well as radiotherapy as a supplementary or alternative option. These strategies aim to control the disease and improve quality of life, underscoring the importance of understanding the various treatment options to develop an individualized and effective management plan for acromegaly.
1. Surgery for acromegaly
According to article, Transsphenoidal surgery is the primary treatment for acromegaly, aiming to remove the pituitary adenoma and achieve surgical remission while normalizing growth hormone levels. The success of this minimally invasive procedure, performed through the nasal cavity, depends on tumor characteristics such as size and invasiveness, as well as the skill of the neurosurgeon. While success rates can be as high as 80% for smaller tumors, larger or more invasive adenomas may require additional treatments after surgery, such as medication or radiotherapy, especially if complete tumor removal is not possible. Preoperative use of somatostatin receptor ligands (SRLs) is sometimes employed to improve surgical outcomes, although its efficacy is debated. Postoperative care involves monitoring hormone levels and imaging to detect any tumor regrowth, with additional therapies like SRLs, cabergoline, and pegvisomant introduced if surgical remission is not achieved.
2. Medications for acromegaly
Treatment options for acromegaly focus on medications that regulate the excessive production of growth hormone (GH) and alleviate symptoms. Somatostatin analogs like octreotide and lanreotide are commonly used as initial pharmacological interventions, as they can reduce GH production and potentially lead to tumor shrinkage. GH receptor antagonists, such as pegvisomant, work by blocking GH effects and normalizing insulin-like growth factor 1 (IGF-1) levels. Dopamine agonists, like cabergoline, may also be prescribed to lower GH secretion. The treatment plan is individualized, taking into account patient responses, any existing health conditions, and is overseen by an endocrinologist. Medication therapy is typically long-term, with regular monitoring of hormone levels and tumor size to ensure efficacy and safety, especially for patients with persistent disease after surgery or those who are not candidates for surgery.
3. Radiation therapy
Radiation therapy is essential for the management of acromegaly, especially in cases where surgery is not feasible or when there is residual tumor. This treatment includes various techniques, such as stereotactic radiosurgery (SRS) and external beam radiation therapy (EBRT), which are used to target the pituitary adenoma and reduce the production of excess growth hormone. SRS, which includes Gamma Knife and CyberKnife, provides a precise, high-dose treatment that minimizes damage to surrounding tissues. Studies have shown that SRS has a success rate of 75% in achieving remission or controlling the disease within 10 years, often leading to quicker normalization of hormone levels and fewer side effects such as pituitary insufficiency compared to EBRT. However, both methods may take years to reach their full effectiveness and can have long-term effects like hypopituitarism, which may require the use of medication for immediate hormone level management. Patients should work closely with their healthcare team to develop a personalized treatment plan, taking into consideration potential side effects such as fatigue, skin irritation, and the need for hormone replacement therapy.
Complications of Acromegaly
Acromegaly is a rare endocrine disorder characterized by the excessive secretion of growth hormone, resulting in abnormal growth and a range of serious complications affecting multiple body systems, including cardiovascular and metabolic disruptions. These complications can greatly impact a patient’s health and quality of life, and in certain instances, may pose a risk to life. A thorough comprehension of these complications is crucial for early detection, highlighting the significance of prompt diagnosis and efficient management to alleviate the varied and severe consequences of this condition.
- High blood pressure (hypertension)
- High cholesterol
- Heart problems, particularly enlargement of the heart (cardiomyopathy)
- Osteoarthritis
- Type 2 diabetes
- Enlargement of the thyroid gland (goiter)
- Precancerous growths (polyps) on the lining of your colon
- Sleep apnea, a condition in which breathing repeatedly stops and starts during sleep
- Carpal tunnel syndrome
- Increased risk of cancerous tumors
- Spinal cord compression or fractures
- Vision changes or vision loss