Acoustic trauma is a form of hearing impairment that occurs as a result of exposure to loud noises, such as explosions, gunfire, or sustained industrial noise. This exposure can lead to temporary or permanent hearing loss by damaging the hair cells in the cochlea, which are essential for converting sound waves into neural signals. Symptoms of acoustic trauma may include sensorineural hearing loss, tinnitus, and a feeling of fullness in the ear. This condition can affect a variety of individuals, including workers, military personnel, and individuals who have been involved in acts of terrorism or accidents, potentially impacting their ability to perform tasks and find employment. Prevention is crucial in mitigating the risk of acoustic trauma, and involves the use of ear protection and adherence to safety regulations regarding noise exposure.
Acoustic trauma is classified into two types: acute and chronic. Acute acoustic trauma is the result of sudden, intense noises such as explosions or gunshots, leading to immediate hearing damage. Chronic acoustic trauma develops gradually due to prolonged exposure to high noise levels, often in industrial settings or from personal audio devices. Both types can result in hearing loss, tinnitus, and other auditory issues, with the severity depending on the intensity and duration of the noise. Preventative measures include using appropriate hearing protection and minimizing exposure to loud sounds.
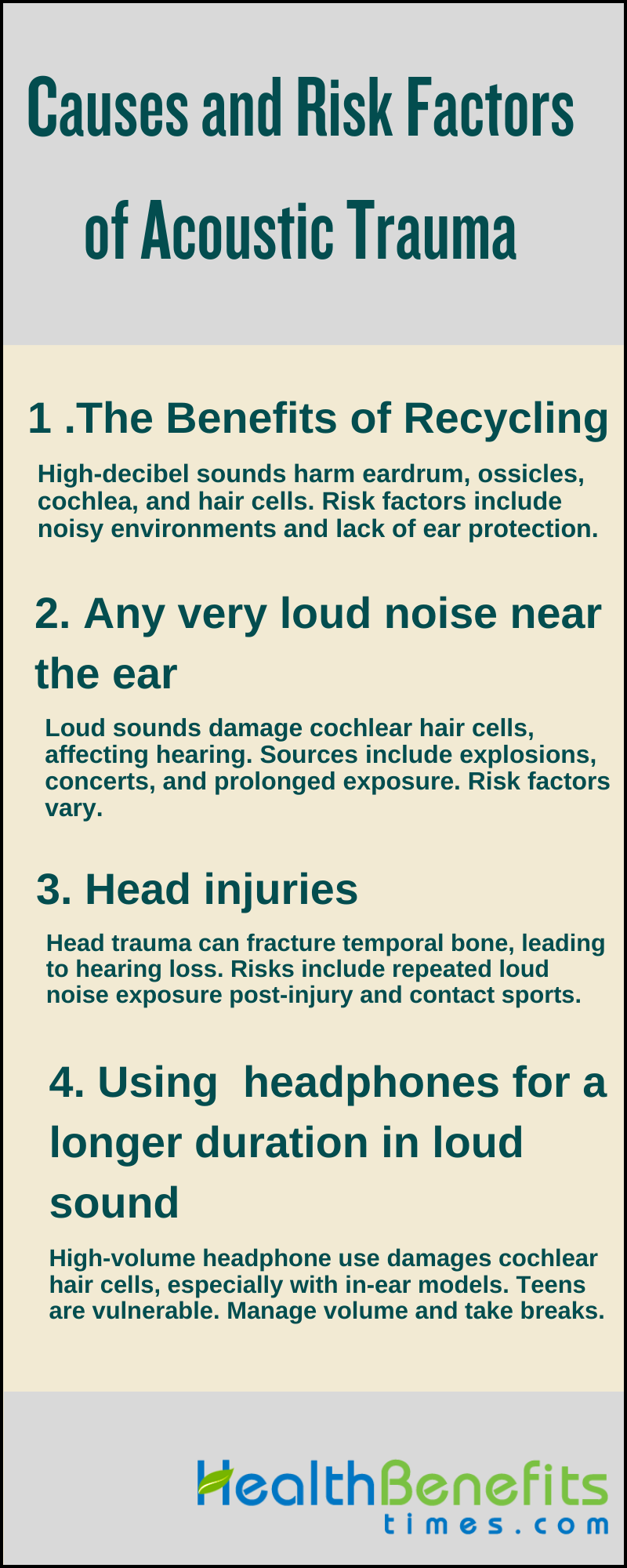
Causes of Acoustic Trauma
Various factors such as the intensity and duration of noise exposure, individual susceptibility including genetic predispositions, and pre-existing health conditions influence the risk of developing acoustic trauma. High-frequency sounds above 85 decibels are especially harmful, with even a single exposure potentially causing irreversible damage. Understanding and mitigating these risks through protective measures are essential for preserving hearing health and preventing acoustic trauma.
1. Damage to middle and inner ear structures
The exposure to to high-decibel sounds can cause damage to the eardrum and ossicles in the middle ear, as well as the cochlea and hair cells in the inner ear, which are essential for converting sound vibrations into electrical signals for the brain. Risk factors for acoustic trauma include working in noisy environments, military service, construction work, and engaging in recreational activities without using ear protection. The severity of the damage is influenced by the intensity and duration of the noise, as well as individual factors such as a history of ear infections, genetic predisposition to hearing loss, and lack of protective hearing equipment. It is crucial to be aware of harmful noise levels and take preventive measures to preserve hearing health.
2. Any very loud noise near the ear
Engaging in recreational activities without ear protection, such as motorcycling, attending auto races, concerts, and nightclubs, also poses a risk of Acoustic Trauma. The severity of acoustic trauma can be influenced by factors such as the intensity, frequency, proximity, and duration of exposure to the sound, with sounds above 85 decibels potentially causing harm and those over 140 decibels leading to immediate damage. Individuals with a history of ear infections or a genetic predisposition to hearing loss are at a higher risk, and the damage can accumulate over time, resulting in progressive hearing impairment. [
3. Head injury
According to article, Acoustic trauma resulting from head injuries can occur in various situations, including road accidents, falls, or assaults, and can cause different types of hearing loss by fracturing the temporal bone or causing concussions that affect auditory processing. The severity of the injury, angle of impact, pre-existing ear conditions, and the individual’s health and age are risk factors that can impact the likelihood of trauma. Direct impacts to the head, repeated exposure to loud noises after the injury, and participation in activities with inherent risks, such as contact sports or military service, can increase the risk of damaging the delicate structures of the inner ear, including the hair cells of the cochlea, eardrum, and ossicles. It is important to take protective measures to reduce these risks, particularly in high-risk situations like gun sports or exposure to blasts.
4. Using earphones or headphones for a longer duration in loud sound
Prolonged exposure to high-volume sound through earphones or headphones can lead to sensorineural hearing loss by damaging the delicate hair cells in the cochlea, a key part of the inner ear that transmits sound to the brain. This risk is heightened for those who use in-ear earphones, which can deliver sound more directly to the eardrum, and for individuals with pre-existing hearing conditions. Young adults and teenagers are particularly vulnerable due to their tendencies to listen at unsafe volumes for extended periods. To mitigate the risk of acoustic trauma and potential permanent hearing loss, it is essential to manage listening habits by keeping volumes at safe levels, taking regular breaks, and being mindful of the cumulative effects of noise exposure.
Symptoms of Acoustic trauma
Prolonged exposure to high-volume can lead to a range of auditory disruptions, collectively referred to as the symptoms of acoustic trauma. These symptoms are the body’s immediate or delayed response to an overwhelming acoustic event, and their manifestation can vary greatly from person to person. Recognizing these signs is crucial for timely intervention and management of the condition to prevent long-term auditory impairment.
- Immediate symptoms can include:
- Feeling of fullness in the ear
- Burning sensations or sharp pain around or in the ear
- Numbness, tingling or soreness down the side of face, neck or shoulder
- Nausea or vomiting
- Dizziness
- Tinnitus and other head noises, such as eardrum fluttering.
- Later symptoms can include:
- headaches
- fatigue
- feeling off-balance
- hypersensitivity to noise, i.e. a sensitivity to previously
- tolerated sounds such as loud voices, television and radio
- anxiety
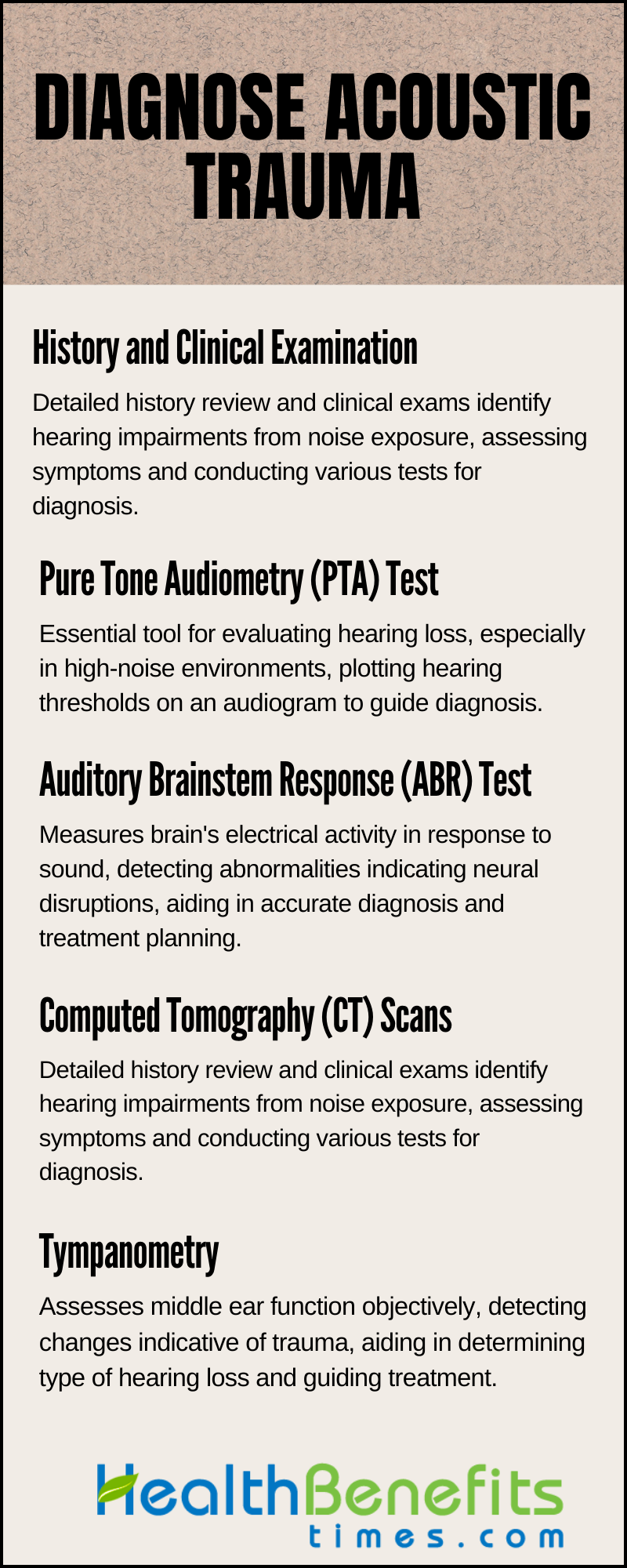
How Can We Diagnose Acoustic Trauma?
In diagnosing acoustic trauma, healthcare professionals utilize a comprehensive approach that involves a variety of assessment tools and techniques to confirm the presence and severity of hearing loss or damage caused by exposure to loud noise. Diagnosis methods together offer a thorough assessment, allowing practitioners to create effective treatment plans focused on addressing potential long-term hearing loss and reducing the impact on the patient’s quality of life.
1. History and Clinical Examination
Diagnosing acoustic trauma requires a detailed history review and clinical examination to identify hearing impairments from intense noise exposure. History-taking includes the patient’s exposure to loud noises, such as bomb explosions, gunfire, and the nature of the exposure, including frequency, duration, and intensity. Clinical examination entails otoscopic evaluation for tympanic membrane damage, audiometric testing to uncover sensorineural hearing loss patterns, particularly at high frequencies, and tuning fork tests to distinguish between sensorineural and conductive hearing loss. Tympanometry assesses middle ear function, while advanced tests like otoacoustic emissions (OAEs) and auditory brainstem responses (ABR) may confirm the diagnosis and injury extent. Symptoms such as hearing loss, tinnitus, otalgia, and ear fullness are noted, and audiometry, including pure-tone and speech audiometry, evaluates hearing thresholds and speech discrimination. This comprehensive diagnostic process informs the management and treatment plan for acoustic trauma.
2. Pure Tone Audiometry (PTA) Test
Pure Tone Audiometry (PTA) is an essential diagnostic tool which measures the quietest sounds a person can hear across various frequencies, with the results plotted on an audiogram to determine hearing thresholds. A characteristic dip in the audiogram, especially in the high-frequency range, often indicates noise-induced hearing loss. PTA is also instrumental in guiding surgical decisions for chronic otitis media by correlating findings with middle ear status. While sensorineural hearing loss is common, particularly in older adults, PTA can also identify retrocochlear hearing loss with the aid of Brainstem Evoked Response Audiometry (BERA) in cases of inconsistent responses. For individuals unable to undergo PTA, such as infants or those with disabilities, Auditory Evoked Potentials (AEPs) can be used. However, PTA is not the sole test for acoustic trauma; other assessments like acoustic reflexes, otoacoustic emissions (OAEs), and auditory brainstem response (ABR) may also be utilized to confirm or refine the diagnosis.
3. Auditory Brainstem Response (ABR) Test
The Auditory Brainstem Response (ABR) measures the brain’s electrical activity through electrodes placed on the scalp and earlobes in response to sound, capturing neural activity along the auditory pathway. It can detect abnormalities such as reduced wave amplitudes, prolonged latencies, or missing peaks, particularly in the early waves associated with the auditory nerve and brainstem, indicative of disruptions in neural transmission. Optoacoustic ABR (oABR) has shown advantages in detecting tinnitus with higher wave II amplitudes and shorter transmission times. ABR is also used intraoperatively to preserve cochlear function and predict postoperative hearing impairment. By analyzing ABR waveforms, audiologists can locate lesions within the auditory system, assess the functional status of central neural structures, and identify conditions like acoustic neuroma or auditory neuropathy. Research has improved ABR’s diagnostic capabilities with signal classification tools and automatic testing methods, enhancing the efficiency and accuracy of hearing threshold detection. This objective and repeatable approach is critical for early detection, accurate diagnosis, and the development of effective treatment plans for acoustic trauma.
4. Computed Tomography (CT) Scans
Computed Tomography (CT) scans play a crucial role in diagnosing acoustic trauma by providing detailed images of the head and ear structures, specifically the bony anatomy of the temporal bone and inner ear components such as the cochlea and auditory nerve. These scans are effective in identifying fractures, disruptions in the ossicular chain, and other signs of trauma that can lead to conductive hearing loss and dizziness. While CT imaging is excellent at detecting bone abnormalities and intracranial bleeds, it is less sensitive to changes in soft tissue, often requiring additional audiometric tests and Magnetic Resonance Imaging (MRI) for a comprehensive evaluation of acoustic trauma. Radiologists use CT scans to assess for indicators of damage such as swelling, thickening, or fluid accumulation, and to rule out other causes of hearing loss such as tumors or congenital malformations. Although not always necessary for diagnosing acoustic trauma, CT scans are particularly recommended when additional pathologies are suspected or when the diagnosis is uncertain, assisting healthcare professionals in developing an effective treatment plan.
5. Tympanometry
Tympanometry is a valuable and objective diagnostic tool used to evaluate middle ear function and diagnose acoustic trauma. It assesses the mobility of the eardrum and the compliance of the middle ear system by inducing changes in air pressure within the ear canal. A normal tympanogram typically shows a distinct peak, indicating proper eardrum mobility and middle ear pressure. However, in cases of acoustic trauma, the tympanogram may exhibit a flattened curve or a reduced compliance peak, suggesting damage to middle ear structures such as the ossicles or the tympanic membrane, as well as the presence of fluid or increased pressure in the middle ear space. These changes, in conjunction with potentially affected stapedial reflex and other audiological tests like pure tone audiometry and otoacoustic emissions, aid healthcare professionals in determining the type of hearing loss—conductive, sensorineural, or mixed—and in guiding appropriate treatment. While tympanometry alone cannot definitively diagnose acoustic trauma, it plays a crucial role in indicating the necessity for further testing to evaluate hearing function and the extent of damage resulting from exposure to loud noise.
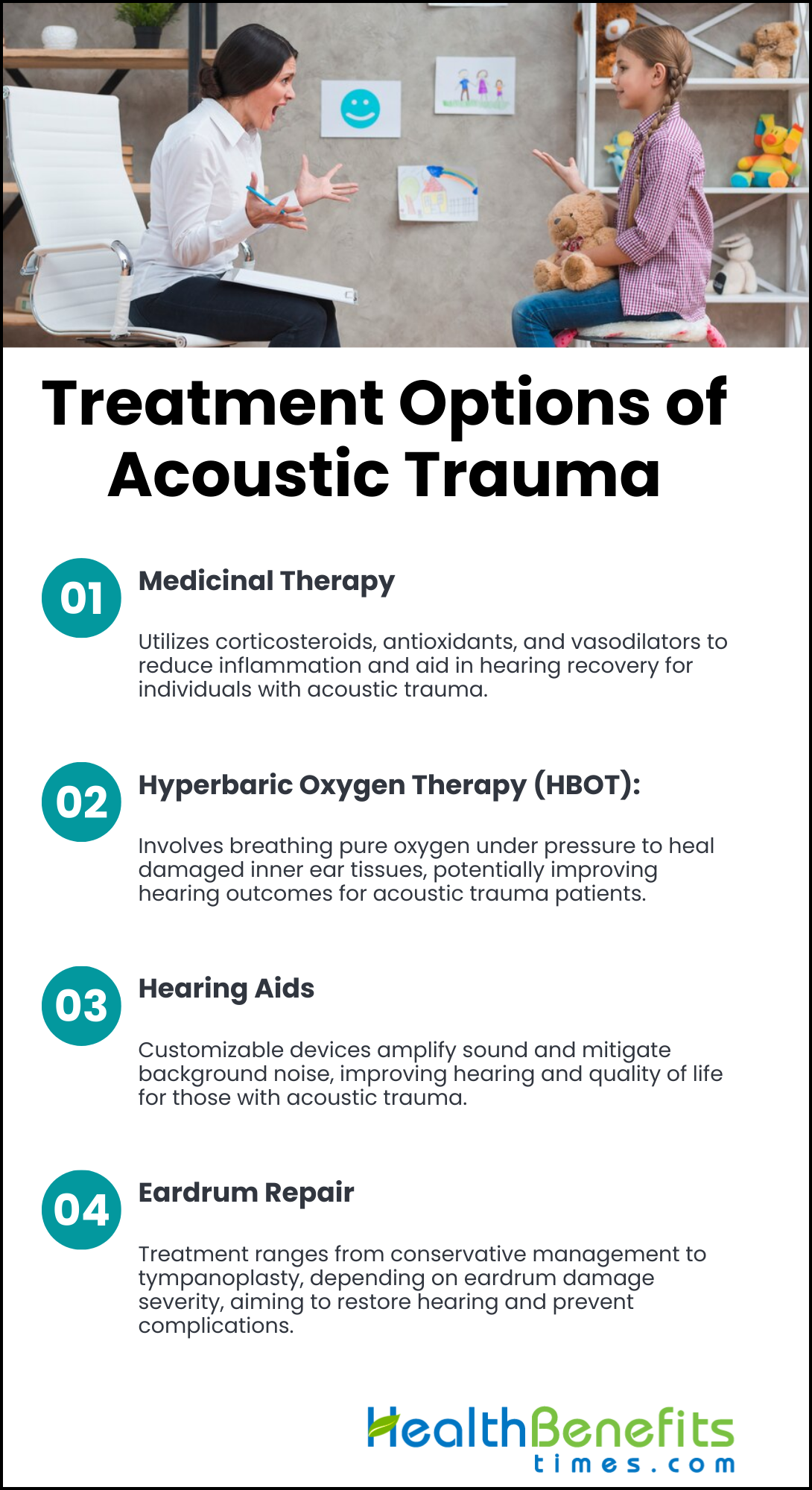
Treatment Options of Acoustic Trauma
Treatment for Acoustic trauma condition is comprehensive and tailored to the individual, including medical interventions, rehabilitative strategies, assistive devices, pharmacological management, auditory therapies, and potentially surgical procedures. These approaches aim to not only alleviate immediate symptoms but also prevent further damage to the auditory system and improve overall well-being. It is crucial for those affected, in collaboration with their healthcare providers, to explore the available treatment options to effectively manage symptoms and promote recovery, enabling informed decisions to restore auditory health.
1. Medicinal Therapy
According to article, Medicinal therapy for acoustic trauma involves the use of corticosteroids such as prednisone or dexamethasone to reduce inflammation and swelling in the inner ear, thereby aiding in hearing recovery. These medications can be administered orally, via injections, or as ear drops. Additionally, antioxidants like N-acetylcysteine and vitamins A, C, and E, as well as vasodilators like trimetazidine or pentoxifylline, may be utilized to improve blood flow and protect against oxidative stress in the cochlea. Aminoglycoside antibiotics may also be prescribed to protect hair cells from further damage, although caution must be exercised due to potential toxicity. It is crucial for individuals with acoustic trauma to seek guidance from an audiologist or otolaryngologist for a personalized treatment plan, which may include the use of hearing rest and protection devices. While these treatments can help manage symptoms, they cannot reverse existing damage, highlighting the importance of preventive measures such as hearing protection to prevent acoustic trauma.
2. Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric Oxygen Therapy (HBOT) is increasingly recognized as an effective treatment for Acoustic Trauma, often caused by exposure to loud noise, resulting in hearing loss and tinnitus. The therapy involves breathing 100% oxygen in a pressurized chamber, which increases the oxygen levels in the blood and aids in the healing of damaged inner ear tissues. Research suggests that early intervention, particularly within two days of the trauma and in combination with corticosteroids, significantly improves hearing outcomes. HBOT has been found to reduce inflammation, assist in the repair of cochlear cells, and enhance hearing thresholds and speech discrimination. While generally safe, it is important to address potential side effects such as middle ear barotrauma and claustrophobia through patient education and preventive measures to ensure a safe therapeutic experience. Ongoing studies are working to optimize HBOT protocols to maximize its benefits for individuals with Acoustic Trauma, underscoring its potential as a non-invasive and promising approach to auditory recovery.
3. Hearing Aids
Hearing aids are a crucial treatment option for managing this condition, as they amplify sound and help individuals with inner ear damage hear better in various environments. These devices are highly customizable, tailored to the user’s specific hearing loss profile, and may include noise reduction features to enhance focus on important sounds while minimizing background noise. Available in different styles such as behind-the-ear (BTE), in-the-ear (ITE), and in-the-canal (ITC), hearing aids are chosen based on the severity of hearing loss, lifestyle, and ear anatomy. Audiologists play a key role in selecting the appropriate device and making necessary adjustments during follow-up appointments to ensure optimal performance and continued protection against auditory damage, ultimately improving the quality of life for individuals with acoustic trauma.
4. Eardrum Repair
According to article, Treatment options for acoustic trauma with eardrum damage vary from conservative management to surgical procedures such as tympanoplasty, depending on the severity of the injury. Tympanoplasty, which involves grafting tissue to repair the tympanic membrane, is recommended for significant perforations to restore hearing and prevent further complications. For less severe injuries, the eardrum may heal naturally, and interventions such as watchful waiting or antibiotics to prevent infection may be sufficient. Audiological evaluations are crucial in determining the degree of hearing loss and the effectiveness of the treatment. In cases of persistent hearing loss, hearing aids or cochlear implants may be recommended. Patients should minimize noise exposure during recovery to facilitate healing. Ossiculoplasty may be necessary for extensive damage affecting the middle ear bones. A personalized treatment plan that combines surgical and non-surgical approaches is essential for optimal recovery and hearing restoration following acoustic trauma.
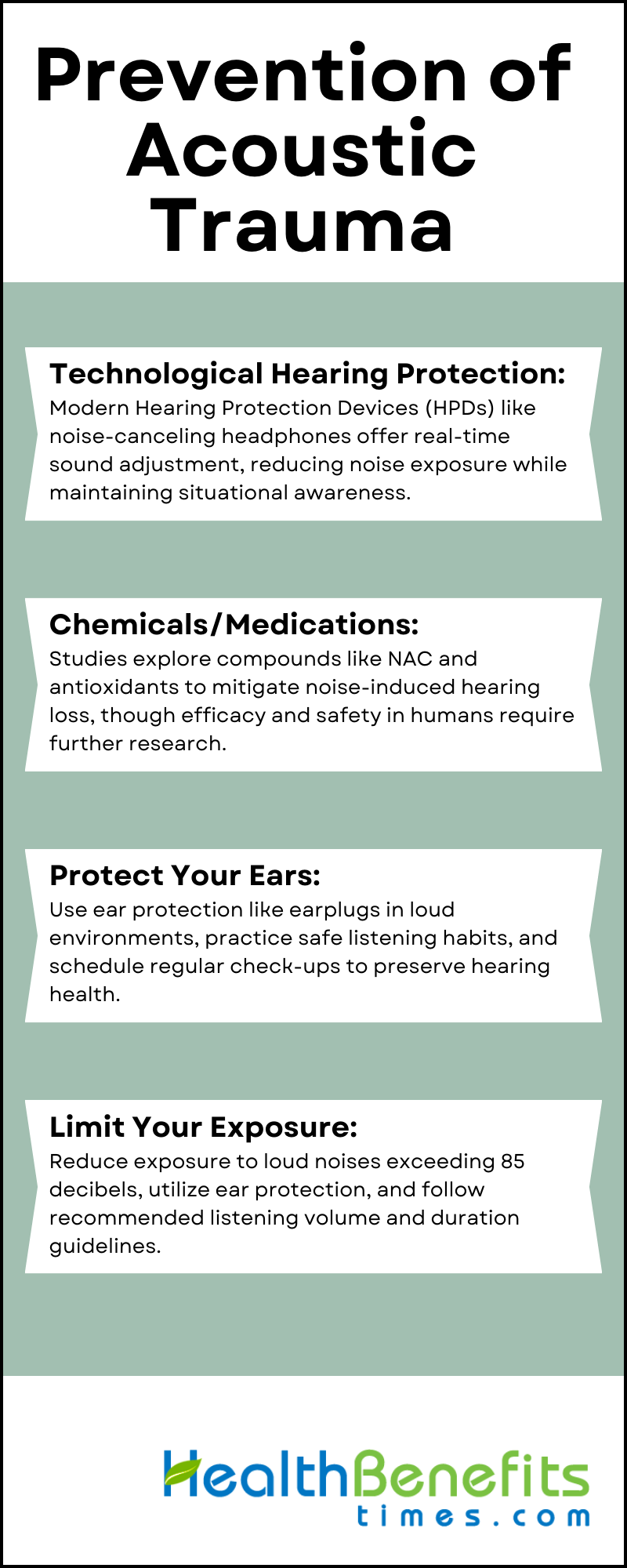
Prevention of Acoustic Trauma
In our world that is becoming increasingly noisy, it is more important than ever to protect our hearing from acoustic trauma. Fortunately, there are several effective strategies and precautions that we can take to minimize the risk of damage to our auditory system. By understanding the causes of acoustic trauma and implementing these preventive measures, we can safeguard our hearing and maintain optimal auditory health throughout our lives. Let us explore the various options available to us in preventing acoustic trauma:
1. Technological Hearing Protection
The development of Hearing Protection Devices (HPDs) is crucial for preventing acoustic trauma in high-noise environments, a major concern in occupational safety and healthcare. Modern HPDs, such as noise-canceling headphones and smart earplugs, utilize advanced technology to adjust to noise levels in real-time, providing excellent sound reduction while preserving sound quality and directionality. These devices not only decrease the intensity of sound to protect the inner ear but also enable communication and awareness of surroundings, which is essential in industries like manufacturing and the military. With features like Bluetooth connectivity and built-in monitoring systems, users are alerted to dangerous noise levels, allowing for immediate action to protect their hearing. The incorporation of these innovative solutions, backed by standardized performance testing, represents a significant advancement in reducing the risks of noise-induced hearing damage and promoting auditory health.
2. Chemicals/Medications
Research on the prevention of acoustic trauma has identified several chemical and medicinal interventions that have the potential to protect against noise-induced hearing loss. N-acetylcysteine (NAC), as well as antioxidants such as vitamins A, C, and E, and minerals like magnesium, have shown protective effects in animal studies by reducing damage from reactive oxygen species and improving blood flow in the inner ear. However, the safety and effectiveness of these treatments in humans are still being investigated. Therefore, individuals are encouraged to use proven preventive measures like earplugs and earmuffs, and to follow safe listening practices while further research works towards incorporating these new strategies into standard care for hearing protection.
3. Protect Your Ears
According to article, In order to maintain good hearing health and prevent acoustic trauma, it is crucial to proactively protect your ears from high noise levels. This can be accomplished by using ear protection such as earplugs or earmuffs during activities with high decibel levels, such as concerts, construction sites, or when operating loud machinery. It is also important to practice safe listening habits by keeping the volume low on personal audio devices and taking regular breaks from noise exposure. Regular hearing check-ups are recommended to detect any early signs of hearing loss. By being mindful of noise levels, using specialized ear protection, and limiting exposure to loud environments, individuals can significantly reduce the risk of hearing damage and preserve their auditory health in the long term.
4. Limit Your Exposure
Acoustic trauma, which can result in permanent hearing loss, is often caused by exposure to high-intensity noise from sources such as explosions, sirens, and machinery. To reduce this risk, particularly in noisy work environments, it is crucial to limit exposure to sounds exceeding 85 decibels, as recommended by the Occupational Safety and Health Administration (OSHA). Protective measures include using earplugs or noise-canceling headphones and following the 60/60 rule, which advises listening to audio at a maximum of 60% volume for no more than 60 minutes. Additionally, decreasing exposure time to 100 dB to 15 minutes per day and taking breaks in quieter environments can help maintain hearing health. By implementing these strategies, individuals can safeguard themselves from the harmful effects of loud noises and preserve good auditory health.