Acoustic neuroma, also known as vestibular schwannoma, is a benign, slow-growing tumor that develops on the vestibulocochlear nerve, which transmits sound and balance information from the inner ear to the brain. Acoustic neuromas arise from Schwann cells, which normally wrap around and insulate nerve fibers. As the tumor grows, it can compress the brainstem and other cranial nerves, resulting in symptoms such as hearing loss, tinnitus, dizziness, and balance issues. While acoustic neuromas are non-cancerous, they can lead to significant complications if not treated. Understanding the characteristics of acoustic neuromas, their symptoms, and available treatment options is essential for early detection, proper management, and improving patient outcomes.
Are acoustic neuromas dangerous?
Acoustic neuromas pose a danger based on several factors, such as the size of the tumor, its rate of growth, and the individual’s overall health. As they grow, they can exert pressure on important structures within the skull, leading to potential complications such as hearing loss, balance issues, and in rare instances, life-threatening consequences. It is essential for patients and healthcare providers to comprehend the risks linked with acoustic neuromas in order to make well-informed decisions regarding monitoring and treatment choices.
Symptoms of Acoustic neuroma
Acoustic neuroma, or vestibular schwannoma, is a benign tumor that arises on the vestibulocochlear nerve connecting the inner ear to the brain, playing a critical role in hearing and balance. Its growth can cause a range of symptoms, from unilateral hearing loss and tinnitus to balance disturbances, which may be subtle at first but can escalate to severe neurological issues, potentially becoming life-threatening if large enough to compress the brainstem. Early recognition of these symptoms is essential for prompt diagnosis and treatment, which is vital to manage the condition and preserve auditory and vestibular health effectively.
1. One-sided Hearing Loss
Acoustic neuroma, also known as vestibular schwannoma, is a noncancerous tumor that develops on the vestibulocochlear nerve and commonly leads to one-sided hearing loss, which can occur gradually or suddenly. Symptoms may include ringing in the ears, problems with balance, dizziness, and facial numbness or weakness as the tumor grows and puts pressure on nearby nerves. Some patients may experience sudden sensorineural hearing loss, which could be the first sign of the tumor and may be detected through abnormal auditory brainstem responses.
2. Ear Fullness
It can lead to a feeling of fullness in the ear, often described as pressure or congestion, and may impact the function of the Eustachian tube. This sensation is commonly accompanied by hearing loss, ringing in the ears, dizziness, and balance problems, and its severity can vary depending on the size of the tumor. While ear fullness can occur in other conditions besides acoustic neuroma, its presence, especially when combined with other ear and balance-related symptoms, should prompt medical evaluation for an accurate diagnosis. Research indicates that ear fullness is a significant symptom in approximately 34% of cases of acoustic neuroma, and healthcare providers should consider this condition when evaluating patients with these symptoms.
3. Noise in the Ear (Tinnitus)
According to article, Acoustic neuroma (AN), a benign tumor on the vestibular nerve, often manifests as tinnitus—a phantom noise in the ear, typically affecting only one side and varying in pitch and intensity. This symptom, which can present as ringing, buzzing, hissing, or whooshing, may be accompanied by hearing loss, dizziness, and a feeling of fullness in the ear. Although tinnitus is a common indicator of AN, especially when paired with hearing asymmetry and balance issues, it is not solely diagnostic, and further evaluation with hearing tests and MRI is necessary for an accurate diagnosis.
4. Balance Problems and Vertigo
According to article, it leads to balance issues and vertigo due to its interference with balance and spatial orientation. Patients commonly experience unsteadiness, difficulty walking, dizziness, and a sensation of spinning, which can be episodic or persistent as the tumor grows. These symptoms can intensify, especially in challenging environments like darkness or uneven surfaces, and may be accompanied by nausea. As the tumor enlarges, it exacerbates the disruption of inner ear equilibrium, potentially causing falls and impacting the quality of life. Nearly half of those diagnosed with acoustic neuroma report these balance disturbances, which are significant and can fluctuate in severity.
5. Other Signs of Acoustic Neuroma
Acoustic neuroma can manifest as seemingly minor health problems, extending beyond just hearing issues such as:
- Numbness in the face
- Facial twitching or weakness
- Swallowing problems
- Change in taste and tear production
- Headache and pressure
- Earache
- Visual problems
- Tiredness and lack of energy.
Causes of Acoustic neuroma
Acoustic neuroma, a benign tumor affecting the nerve responsible for balance and hearing, poses a complex medical challenge with its exact causes still largely unknown. However, researchers have made progress in identifying genetic predispositions, such as the association with neurofibromatosis type 2 (NF2), and environmental risk factors, including exposure to high doses of radiation. Let’s explore some causes of Acoustic Neuroma:
1. Age
Acoustic neuroma is also a benign tumor that affects the vestibulocochlear nerve. The majority of cases are diagnosed in adults between the ages of 30 and 60, with a higher prevalence in the 40s and 50s. While the exact causes are unknown, age is considered a significant risk factor, suggesting that environmental factors and cellular aging may be involved. Most acoustic neuromas develop spontaneously and are not associated with specific risk factors, although some cases have been linked to high levels of radiation exposure. Ongoing research is being conducted to identify potential genetic and environmental factors that may contribute to the development of these tumors in different age groups.
2. Family History
According to article, Research consistently emphasizes the importance of family history in the risk of developing acoustic neuroma, a benign brain tumor. Genetic factors, such as pathogenic variants in genes like OTOF, have been associated with auditory neuropathy and may play a role in the development of acoustic neuroma. While many cases occur sporadically, individuals with a family history of acoustic neuroma or related genetic conditions, such as neurofibromatosis type 2 (NF2), are at an increased risk. NF2 is characterized by the growth of noncancerous tumors in the nervous system, with mutations in the NF2 gene increasing susceptibility to acoustic neuromas.
3. Radiation exposure
Exposure to ionizing radiation, particularly high doses used in therapeutic radiotherapy for head and neck cancers, has been linked to an increased risk of developing acoustic neuromas. This risk is also present with chronic low-dose exposure and is notably higher in individuals who received radiation during childhood. Although the precise causes of acoustic neuroma are not fully understood, radiation-induced DNA damage in the cells of the eighth cranial nerve is a recognized risk factor. Despite this association, acoustic neuromas remain relatively rare, even among those with significant radiation exposure, and the majority of cases are sporadic.
4. Neurofibromatosis type 2 (NF2)
According to article, Neurofibromatosis type 2 (NF2) is a genetic disorder caused by mutations in the NF2 gene located on chromosome 22. These mutations typically result in the production of the tumor suppressor protein merlin. This dysfunction leads to the development of multiple noncancerous tumors within the nervous system, including bilateral vestibular schwannomas (acoustic neuromas), meningiomas, and ependymomas. These tumors can cause symptoms such as hearing loss, dizziness, and tinnitus due to their impact on the vestibulocochlear nerve. Spinal tumors may also lead to pain, muscle weakness, or paresthesias. NF2 can be inherited in an autosomal dominant pattern or can arise from de novo mutations, with some patients displaying mosaicism.
When to see your doctor
Experiencing symptoms like unilateral hearing loss, tinnitus, ear fullness, balance difficulties, or facial numbness could indicate the presence of an acoustic neuroma, which is a benign tumor located on the nerve that connects the ear to the brain. It is important to seek advice from a healthcare professional if these symptoms are present, as early detection is crucial for effective management. Treatment options may include watchful waiting, microsurgical resection, or stereotactic radiation, depending on individual factors. Prompt medical evaluation is recommended to prevent severe complications, such as total hearing loss or increased pressure on the brain, and to preserve hearing and nerve function. Doctors may perform hearing and neurological tests and recommend imaging, such as an MRI, to diagnose and determine the most appropriate treatment approach for acoustic neuromas.
How Acoustic Neuroma is diagnosed?
The diagnosis of acoustic neuroma, a type of intracranial tumor, has been refined through the use of advanced imaging techniques such as CT and MRI, which are essential for distinguishing it from other similar intracranial masses like meningiomas, epidermoids, and metastases.
- Hearing test (audiometry)
- Pure tone average (PTA)
- Speech reception threshold (SRT)
- Speech discrimination (SD)
- Imaging scans of the head
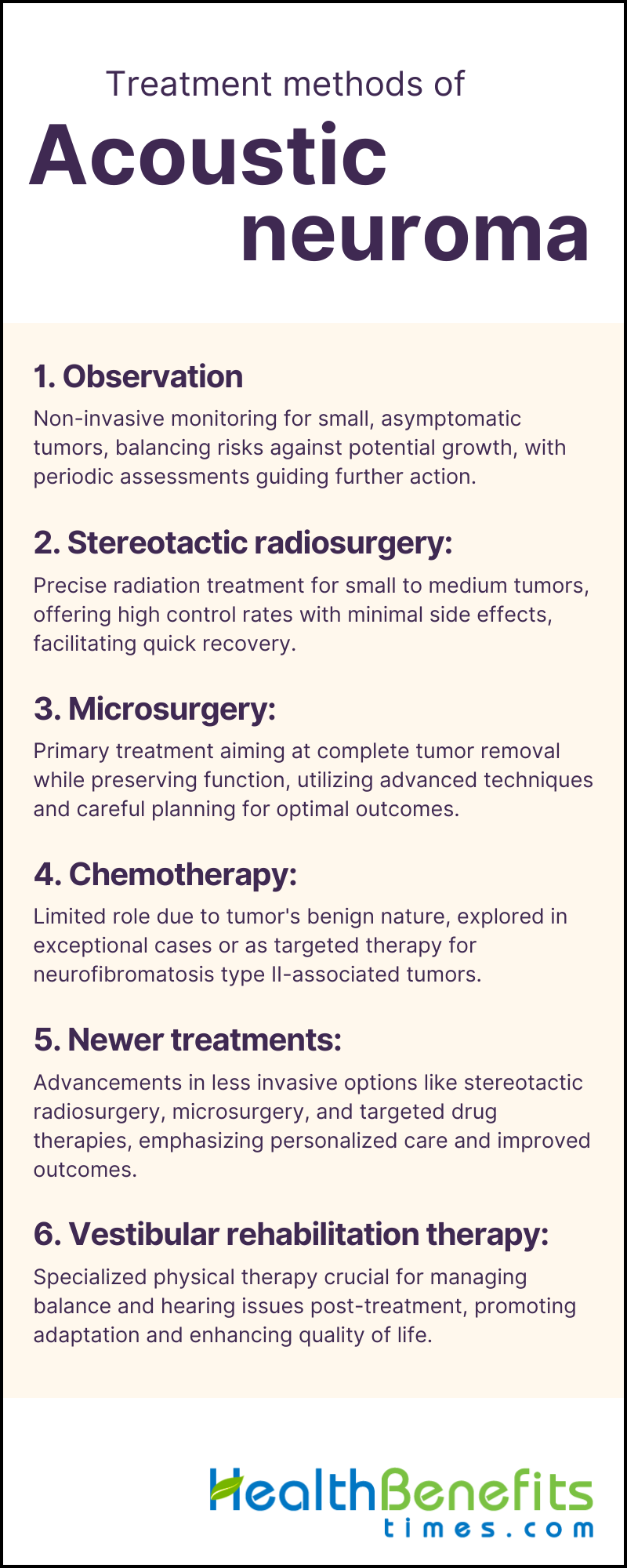
Treatment methods of Acoustic neuroma
The management and treatment of acoustic neuroma require a precise balance of expertise, as strategies can range from careful observation to advanced surgical interventions and state-of-the-art radiation therapies. As we explore the complexities of this condition, we discover the diverse approaches that represent the leading edge of neuro-otological care, each customized to the tumor’s progression and the unique needs of the patient.
1. Observation
Observation is a crucial strategy in the management of acoustic neuroma, a benign tumor that affects the nerve between the ear and brain, especially when the tumor is small and asymptomatic. This non-invasive approach involves regular MRI scans and sometimes audiometric evaluations to monitor the tumor’s size and the patient’s symptoms, with check-ups typically occurring every 6 to 12 months. Positive outcomes have been observed, with many patients able to control the tumor and maintain their hearing over long periods. The decision to observe rather than immediately intervene is influenced by factors such as tumor characteristics, patient age, overall health, and personal preference, in order to weigh the risks of surgical or radiation treatments against the potential for tumor growth. If significant growth or symptoms such as hearing loss, tinnitus, or balance issues arise, more aggressive treatments may be considered. This approach prioritizes patient safety and quality of life, while allowing for a shift to intervention if necessary.
2. Stereotactic radiosurgery
Stereotactic radiosurgery (SRS) is a non-invasive and precise treatment for acoustic neuromas that delivers high doses of radiation to the tumor while sparing surrounding healthy tissue. Techniques such as Gamma Knife and LINAC-based radiosurgery have shown similar quality of life outcomes and low toxicity, making SRS a safe option with high tumor control rates. SRS is beneficial for patients with small to medium-sized tumors or those at higher risk from traditional surgery. Typically performed in a single session, SRS allows patients to quickly resume normal activities. It effectively halts tumor growth, preserves hearing, and maintains facial nerve function, with long-term control rates exceeding 90% and minimal side effects. Regular imaging follow-ups are essential to monitor treatment response and potential recurrences.
3. Microsurgery
Microsurgery is the primary treatment for acoustic neuromas, which are benign tumors on the vestibular nerve that affect hearing and balance. The goal of this treatment is to completely remove the tumor while preserving neurological function. Surgical approaches, such as translabyrinthine, retrosigmoid, and middle fossa, are selected based on the characteristics of the tumor and the patient’s health. Intraoperative nerve monitoring is used to protect the integrity of the facial nerve and, when possible, hearing. This specialized procedure typically involves a neurosurgeon and otolaryngologist and requires precision and careful planning with the help of MRI imaging. Postoperative care is crucial for monitoring hearing, facial strength, and balance, and may include rehabilitation. Despite the potential risks of hearing loss, facial nerve damage, and balance issues, advancements in surgical techniques have led to improved outcomes, making microsurgery a collaborative effort among multiple disciplines to ensure optimal patient recovery.
4. Chemotherapy
Acoustic neuroma, a benign tumor affecting the nerve between the ear and the brain, is typically managed through observation, surgical removal, or radiation therapy rather than chemotherapy, due to its slow growth and non-malignant nature. Chemotherapy is not a standard treatment but may be considered in exceptional circumstances, such as with Neurofibromatosis Type II or when other treatments are not viable options. The potential of chemotherapy, including targeted therapies like bevacizumab, is still being investigated, particularly for complex or recurrent cases. However, its effectiveness remains uncertain, and it is generally reserved for cases where standard treatments have failed. Patients should consult with their healthcare team to assess the benefits and risks of available treatments for their specific situation.
5. Newer treatments
According to article, Stereotactic radiosurgery, such as Gamma Knife and CyberKnife, delivers targeted radiation treatment, reducing damage to surrounding tissues and preserving neurological functions. Surgical advancements, including intraoperative monitoring and minimally invasive techniques, have improved the safety and effectiveness of tumor removal. The use of targeted drug therapies like bevacizumab, which inhibits tumor blood supply, and the exploration of chemotherapy, particularly for neurofibromatosis type 2-associated tumors, show promise. These treatments, combined with improvements in microsurgical techniques and stereotactic laser ablation, demonstrate a shift towards personalized care that takes into account the tumor’s characteristics, the patient’s overall health, and their treatment preferences, with the goal of optimizing outcomes and minimizing the impact on patients’ lives.
6. Vestibular rehabilitation therapy
Vestibular rehabilitation therapy (VRT), a specialized form of physical therapy, targets symptoms such as dizziness and balance problems through exercises that facilitate compensation by the central nervous system and enhance vestibular function. Customized to meet individual needs, VRT includes habituation, gaze stabilization, and balance training exercises to promote adaptation and reduce the risk of falls. Following treatment, VRT is vital for recovery, aiding patients in restoring stability and enhancing their quality of life. According to article, The efficacy of this therapy depends on tailoring it to the specific characteristics of the tumor and the patient’s response, with regular adjustments made by a trained therapist to achieve optimal results.
Surgery for Acoustic Neuroma
When an acoustic neuroma, a noncancerous tumor on the nerve responsible for hearing and balance, disrupts this harmony, surgery becomes a necessary intervention. This procedure, a reflection of the advancements in modern medicine, provides an opportunity to remove the unwanted growth and restore the equilibrium disturbed by this intruder. As patients consider undergoing surgery, they experience a mix of hope and uncertainty, embarking on a journey that combines state-of-the-art technology with the timeless pursuit of health and well-being. Understanding the intricacies of acoustic neuroma surgery is essential for individuals facing the decision-making process, as the chosen path can significantly impact their quality of life and overall well-being. Some Surgical procedures to treat Acoustic Neuroma are as follows:


