Acne is a chronic inflammatory skin condition that primarily affects the pilosebaceous unit, characterized by the formation of both inflammatory and non-inflammatory lesions such as papules, pustules, nodules, comedones, and open or closed lesions. The pathogenesis involves a combination of genetic predisposition, environmental triggers, and the crucial role of Propionibacterium acnes in inducing inflammatory responses. Acne is most prevalent among teenagers, with around 90% experiencing symptoms, and a significant portion continuing to have symptoms into adulthood. Factors contributing to acne include hormonal fluctuations, diet, stress, and genetics. While not considered a dangerous condition, acne can lead to emotional distress, physical scarring, and a negative impact on quality of life, especially when severe or persistent. Treatment strategies focus on targeting factors like increased sebum production, hyperkeratinization, P. acnes colonization, and inflammatory reactions to resolve lesions and prevent scarring, ranging from over-the-counter topical medications to prescription drugs and therapies.
Symptoms of Acnes
According to article, It is a primarily triggered by factors such as elevated sebum production, influenced by Propionibacterium acnes, and normal circulating dehydroepiandrosterone levels, particularly in adolescence. Additionally, acne fulminans, a severe variant, is characterized by painful erosions, hemorrhagic crusts, and disfiguring scars, often accompanied by systemic symptoms like fever, malaise, and polyarthralgia. Hidradenitis suppurativa (HS), another related condition, involves painful, chronic, suppurative processes affecting the skin and subcutaneous tissue, leading to physical pain, odor, chronic drainage, and disfigurement. These symptoms not only impact physical appearance but also have a significant negative effect on quality of life, potentially causing emotional distress and mental health issues such as depression and anxiety.
Types of Acne
1. Acne Vulgaris
Acne vulgaris, a common skin condition primarily affecting adolescents and young adults, is characterized by various lesions including blackheads, whiteheads, papules, pustules, nodules, and cysts. Classified into four grades based on severity, acne vulgaris appears on areas rich in sebaceous glands, such as the face, neck, chest, and upper back, as a result of clogged hair follicles due to overproduction of sebum, accumulation of dead skin cells, and the presence of Propionibacterium acnes bacteria.
2. Comedones
According to article, Comedones, a primary feature of acne vulgaris, are non-inflammatory lesions that arise from hair follicles clogged with oil, dead skin cells, and sometimes bacteria due to androgen hypersensitivity. These lesions can manifest as open comedones (blackheads) or closed comedones (whiteheads) and are a hallmark of acne pathogenesis. Various therapeutic approaches, such as chemical peels, have shown efficacy in reducing acne lesions and improving skin appearance, ultimately enhancing patient satisfaction and quality of life.
3. Blackheads
Blackheads, also known as open comedones, are a prevalent form of acne distinguished by small, dark lesions that commonly occur on the face, specifically the nose, chin, and forehead. They develop when hair follicles become obstructed with dead skin cells and excess sebum, potentially affecting facial aesthetics and mental health. Several techniques for blackhead removal have been suggested, such as using blackhead guiding essence, peel-off masks, pore-tendering essences, and a mixture of sodium bicarbonate, honey, and egg white.
4. Whiteheads
Whiteheads, also known as closed comedones, are a common type of acne that occurs when hair follicles become clogged with oil, dead skin cells, and sometimes bacteria, resulting in small, flesh-colored bumps with a white center. They are a mild form of acne that can be treated with over-the-counter topical treatments containing ingredients such as salicylic acid or benzoyl peroxide. Understanding their pathophysiology and differentiation from other types of acne is essential for dermatologists to provide targeted and successful interventions.
5. Papules
Papules acne scars are a subtype of acne scarring characterized by skin-colored, fibrotic papules that can be mistaken for active acne lesions, leading to delayed treatment. Papules, on the other hand, are small, red, tender bumps that form due to severe inflammation and clogged pores, and are treated with topical medications containing benzoyl peroxide or salicylic acid, while more severe cases may require prescription medication from a dermatologist.
6. Pustules
Pustules are a prevalent form of inflammatory acne lesion distinguished by red, inflamed bumps containing a white or yellowish pus-filled center. They are caused by a variety of factors including infections, immune-mediated responses, and the infiltration of activated neutrophils into the skin’s epithelial layers. Treatment for pustules may involve the use of topical creams, antibiotics, or other medications prescribed by a dermatologist. These treatments aim to reduce inflammation, combat bacterial infection, and prevent future breakouts, while also taking into account the potential risk of scarring resulting from the presence of pus and inflammation.
7. Nodules
Nodular acne is a severe form of acne characterized by large, hard, painful bumps beneath the skin’s surface that can persist for weeks or months and lead to significant inflammation and scarring. Due to its severity and potential for long-term skin damage, nodular acne requires prompt identification and aggressive treatment. This typically involves systemic medications such as oral antibiotics or isotretinoin under the guidance of a dermatologist to effectively manage the condition and prevent the development of atrophic scars.
8. Cysts
Cysts are a severe form of acne characterized by deep, inflamed, pus-filled lesions that can cause significant pain and carry a higher risk of scarring. Various subtypes of cysts, such as pilonidal, sebaceous, and epidermal cysts, can develop due to factors like obstruction of pilosebaceous ducts or infection, and often require professional treatment from a dermatologist. Treatment options may include oral antibiotics, hormonal therapy, isotretinoin, or surgical excision, depending on the specific type and severity of the cystic acne.
9. Mild Acne
Mild acne is a common form of the skin condition characterized by the presence of non-inflammatory lesions such as whiteheads and blackheads, which can be effectively managed with topical solutions like azelaic acid, clindamycin, benzoyl peroxide, or retinoids, as well as over-the-counter treatments, good skincare routines, and lifestyle modifications to reduce triggers such as stress and dietary factors.
10. Moderate Acne
Moderate acne, classified as acne grade II, is characterized by an increased number of inflammatory lesions such as papules and pustules, as well as comedones like blackheads and whiteheads. Treatment for moderate acne typically includes a combination of topical and oral medications, such as retinoids, antibiotics, and occasionally isotretinoin, as well as photodynamic therapy, depending on the individual case and the recommendation of the dermatologist, to effectively reduce inflammation, promote healing, and minimize the risk of scarring.
11. Severe Nodulocystic Acne
Severe nodulocystic acne is a severe form of acne characterized by deep, painful nodules and cysts that can result in substantial skin damage and scarring. Treatment usually involves the intervention of a dermatologist and may consist of oral antibiotics, isotretinoin, topical treatments containing acids like black peel, or a combination of these approaches. In cases where isotretinoin does not achieve complete remission of lesions, alternative options such as oral dapsone have shown potential.
12. Acne Conglobata
Acne conglobata is a severe form of acne characterized by deep, inflamed nodules, cysts, and sinus tracts that can connect beneath the skin, often resulting in significant scarring and potential systemic symptoms. Treatment for this condition usually involves a combination of systemic approaches, such as oral retinoids, antibiotics, and occasionally surgical intervention, while also taking into account the underlying microbial factors and potential associations with other systemic conditions.
13. Acne Mechanica
According to article, Acne Mechanica is a distinct form of acne that is caused by mechanical factors like friction, pressure, or occlusion on the skin. It is often observed in athletes who wear helmets and pads, as well as individuals whose clothing or accessories cause prolonged skin contact. The mechanical irritation worsens oil production and traps sweat and bacteria, resulting in the development of comedones, papules, and pustules. Treatment includes identifying and removing the triggering factors, practicing good skin hygiene, and using topical or oral medications as needed. It is also important to reduce friction and use non-comedogenic skincare products to prevent further aggravation.
What are the stages of acne?
1. Grade 1 – Mild Acne
Grade 1, or mild acne, is the initial stage of acne development characterized by the presence of relatively few open comedones (blackheads) and closed comedones (whiteheads), accounting for 60% of cases. This stage, often referred to as “physiologic acne,” is typically self-treated by patients following advice from pharmacists or personal judgment. According to article, the lesions are superficial, confined to a small area of the skin, and do not cause significant inflammation or deep cysts. In young adolescent boys, acne severity increases with advancing pubertal maturation, with comedonal acne being more frequent and severe than inflammatory lesions. Effective management of mild acne, which often responds well to over-the-counter topical treatments focusing on exfoliation and reducing oil production, is essential to prevent progression to more severe forms. Nurse prescribers play a crucial role in understanding the etiology of acne and the different stages, including mild acne, to provide appropriate treatment, support, and skincare education to patients.
2. Grade 2 – Moderate Acne
Grade 2 acne, classified as moderate acne, is characterized by an increased frequency of visible lesions, including papules, pustules, blackheads, and whiteheads, which typically appear on the face, chest, and back. Treatment for moderate acne involves a combination of topical remedies such as benzoyl peroxide, salicylic acid, and retinoids, as well as oral antibiotics like doxycycline to reduce inflammation and promote skin healing. Factors such as stress, smoking, and overproduction of oil can contribute to the severity of acne, emphasizing the importance of addressing both physiological and psychosocial aspects in the management of moderate acne, which can cause discomfort and affect an individual’s self-esteem due to its more noticeable nature.
3. Grade 3 – Severe Acne
Grade 3, or severe acne, is characterized by a high level of severity and complexity, with numerous inflamed nodules, pustules, and cystic lesions that are widespread across the face and may also affect the chest and back. These deep inflammatory nodules, cysts, abscesses, and fistulas can be quite painful and lead to significant scarring, both hypertrophic and atrophic. Treatment of severe acne typically requires systemic interventions due to its challenging nature, with options including oral antibiotics, hormonal antiandrogens for females, and oral isotretinoin, which is recommended as a second-line therapy due to its potential serious side effects. The classical three-grade acne classification system, which includes severe acne, has been found to have poor reproducibility in clinical practice, highlighting the need for more reliable and descriptive rating tools for acne severity assessment. It is crucial for individuals suffering from Grade 3 acne to seek professional dermatological treatment promptly to minimize long-term skin damage, improve the skin’s appearance, and address the condition effectively.
4. Grade 4 – Cystic Acne
Grade 4 acne, also known as cystic acne, is the most severe form of the condition. It is characterized by deep, inflamed, and painful lesions called cysts and nodules that can appear on the face, chest, back, and other areas prone to severe acne. These cysts are larger than typical pimples, located deep within the skin, and often lead to significant discomfort and a higher risk of scarring. This stage of acne is often associated with genetic influences, as seen in neonatal, nodulocystic, and conglobate acne, highlighting the role of hereditary factors in its development. Treatment options for cystic acne can vary, with research exploring the effectiveness of different approaches, such as the use of diaminodiphenylsulfone, which has been shown to impact neutrophils and inflammatory processes effectively. Due to the potential for long-term skin damage, prompt and effective treatment for cystic acne is essential and typically requires intervention from a dermatologist.
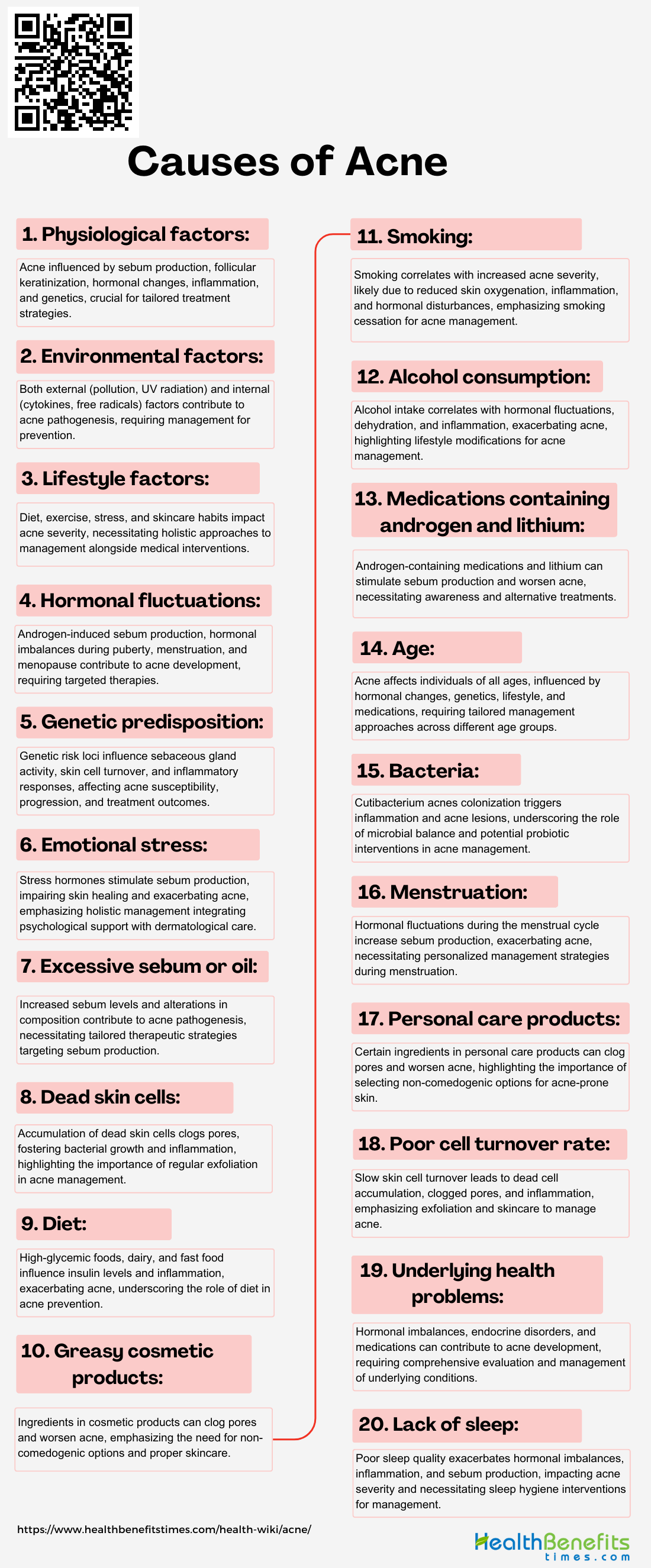
Causes of Acne
1. Physiological factors
According to article, Acne is a common skin condition that is primarily influenced by physiological factors affecting skin health and appearance. The main contributors to acne include hyperseborrhea (excessive sebum production by sebaceous glands), abnormal follicular keratinization (blockage of pores by dead skin cells), and the growth of Propionibacterium acnes bacteria in the pilosebaceous unit. Hormonal changes, particularly during puberty, pregnancy, or menstrual cycles, can exacerbate sebum production and trigger or worsen acne outbreaks. Androgens, such as testosterone, stimulate sebaceous glands, leading to increased sebum production. Inflammation also plays a key role in the development and persistence of acne, with factors like linoleic acid deficiency, inflammatory mediators, and bacterial metabolic products contributing to follicular inflammation.
2. Environmental factors
Environmental factors play a significant role in the development of acne vulgaris, a common skin condition characterized by the appearance of pimples, blackheads, and cysts. Both external factors, such as polluted air, water, high glycemic index foods, pollutants, nicotine, alcohol, drugs, and UV radiation, and internal factors, including cytokines, interleukins, free radicals, and oxidative stress, contribute to the pathogenesis of acne. According to article, these environmental exposures have been linked to various types of acne, such as dioxins-induced chloracne, coal tar acne, cigarette smoking, and UV-related acne. Studies have also highlighted the impact of in utero exposures, early-life exposures, climate, household products, and skin microbiota on the development of acne.
3. Lifestyle factors
Acne, a common skin condition, is significantly influenced by various lifestyle factors that can worsen or trigger the condition. Poor dietary choices, such as consuming high-glycemic foods, fast food, and dairy products, have been linked to increased acne severity due to their impact on insulin production and inflammation. Additionally, lifestyle choices like physical activity, bathing frequency, and the use of comedogenic skin and hair care products can affect the prevalence of acne. Stress is another important factor, as it stimulates the adrenal glands to produce more cortisol, leading to excess oil production and clogged pores. Inadequate sleep, hydration, and exposure to environmental pollutants can also contribute to the development of acne.
4. Hormonal fluctuations
Hormonal fluctuations play a significant role in the development of acne, particularly during periods such as puberty, menstruation, pregnancy, and menopause, as well as in individuals with conditions like polycystic ovarian disease and menstrual function disorders. Androgens, such as testosterone and dihydrotestosterone, are key hormones that influence sebum production and acne formation, causing sebaceous glands to produce more sebum, which can clog pores and lead to inflammation when mixed with dead skin cells and bacteria. Studies have shown that patients with acne, especially women with menstrual irregularities, often have hyperprogesteronemia, indicating a disruption in hormonal balance.
5. Genetic predisposition
Genetic predisposition plays a significant role in the development of acne vulgaris, a common chronic skin disorder characterized by the appearance of pimples, blackheads, and cysts. Studies have identified multiple genetic risk loci associated with acne, highlighting the involvement of pathways such as Wnt and MAPK, as well as genes related to lipid biosynthesis pathways. This genetic link is thought to influence factors such as the size and activity of sebaceous glands, which produce the skin’s natural oils, as well as the rate of skin cell turnover and the body’s inflammatory response.
6. Emotional Stress
According to article, Emotional stress is increasingly recognized as a significant factor in the development and exacerbation of acne. Studies have highlighted the complex relationship between stress levels and acne severity. Research has shown that acne patients have a higher presence of stressful life events, anxiety, and depression compared to controls. Factors such as anger, smoking, and dietary habits are strongly associated with the intensity of the condition. When an individual experiences stress, the body releases stress hormones, including cortisol, which can stimulate the sebaceous glands to produce more oil, leading to clogged pores and acne development.
7. Excessive sebum or oil
Excessive sebum production is a primary factor in the development of acne, a common skin condition affecting millions worldwide. Research papers highlight the crucial role of increased sebum levels and alterations in sebum composition in acne pathogenesis. Sebum, an oily substance secreted by sebaceous glands, is essential for maintaining healthy skin, but when produced in excess, it can lead to clogged pores, trapping dead skin cells and providing an ideal environment for the proliferation of the acne-causing bacteria Propionibacterium acnes. This overproduction of sebum can be influenced by various factors, including hormonal changes, stress, certain medications, and genetics. The resulting blockages manifest as blackheads, whiteheads, and inflamed pimples.
8. Dead skin cells
According to article, Acne vulgaris is a complex skin disorder caused by a combination of factors including the accumulation of dead skin cells, excessive sebum production, and bacterial growth, leading to the blockage of hair follicles. The presence of dead skin cells and sebum provides an ideal environment for the bacteria Propionibacterium acnes to thrive, resulting in inflammation and the formation of various types of acne lesions such as comedones, pimples, and blackheads. This condition typically begins in childhood, progresses to inflammatory acne in adolescents, and can persist into adulthood, with a higher prevalence among women up to 40 years old. The role of dead skin cells in the development of acne is crucial, as impaired cellular turnover and death signaling in the sebaceous follicle are believed to contribute to the progression of this chronic disease.
9. Diet
Acne vulgaris is a complex skin disorder caused by a combination of factors including the accumulation of dead skin cells, excessive sebum production, and bacterial growth, leading to the blockage of hair follicles. According to article, the presence of dead skin cells and sebum provides an ideal environment for the bacteria Propionibacterium acnes to thrive, resulting in inflammation and the formation of various types of acne lesions such as comedones, pimples, and blackheads. This condition typically begins in childhood, progresses to inflammatory acne in adolescents, and can persist into adulthood, with a higher prevalence among women up to 40 years old.
10. Greasy cosmetic products
Greasy cosmetic products can significantly contribute to the development and worsening of acne, especially in individuals with sensitive or acne-prone skin. These products often contain oils, waxes, and silicones that can form a barrier on the skin, trapping dead skin cells, bacteria, and sebum. This can lead to blocked pores and create an environment that promotes the growth of acne-causing bacteria. It is important for individuals with acne to choose their cosmetic products carefully, as certain ingredients can trigger acne or cause allergic reactions.
11. Smoking
Smoking has been identified as a potential contributing factor to the development and exacerbation of acne, particularly non-inflammatory acne such as blackheads and whiteheads. Studies have shown a positive correlation between smoking and acne severity, with smokers having a higher risk of developing acne compared to non-smokers, especially among female smokers. The relationship appears to be dose-dependent, with a higher number of cigarettes smoked daily correlating with increased acne prevalence and severity. The exact mechanisms by which smoking exacerbates acne are complex and involve decreased oxygen flow to the skin, narrowing of blood vessels, triggered inflammation, overproduction of skin oils, and potential hormonal imbalances.
12. Alcohol consumption
Alcohol consumption has been identified as a significant factor contributing to the development and exacerbation of acne. Research indicates that alcohol abuse can lead to various dermatological manifestations, including acne vulgaris, seborrhea, and dyssebacia. When alcohol is ingested, it can lead to hormonal fluctuations and an increase in androgen levels, stimulating the oil glands in the skin to produce more sebum. This can clog pores and create an environment conducive to acne-causing bacteria.
13. Medications that contain androgen and lithium
Acne, a common skin disorder, can be influenced by medications containing androgens and lithium. Androgens play a crucial role in acne pathophysiology, impacting sebum production, follicular keratinocyte proliferation, and skin inflammation, ultimately leading to acne formation. Medications containing androgens, such as those used by bodybuilders or transgender men, can exacerbate acne vulgaris by increasing the production of sebum, an oily substance that can clog pores. Similarly, lithium, commonly prescribed for bipolar mood disorders, has been associated with various dermatological side effects, including acne, with the dosage and serum levels closely tied to the frequency of cutaneous adverse effects. Although the exact mechanism by which lithium induces acne is not fully understood, it is believed to alter the function of the sebaceous glands and promote inflammation. Monitoring and recognizing these medication-induced factors are crucial in managing acne effectively, and individuals experiencing problematic acne while on such medications should consult with their healthcare provider to discuss alternative treatments or supportive skincare measures.
14. Age
According to article, Acne is a common skin condition that affects individuals of all ages, not just adolescents. It can begin as comedonal acne in young children, progress to inflammatory acne during adolescence due to hormonal changes, and persist into adulthood, impacting individuals up to 40 years old, with women being more susceptible to adult acne than men. Factors contributing to the development of acne include dead skin cells, excessive sebum production, bacterial growth, hormonal imbalances, dietary choices, smoking habits, environmental factors, genetic predispositions, stress, lifestyle choices, and certain medications. Psychological distress often accompanies acne, with patients experiencing anxiety, depression, low self-esteem, frustration, and anger, particularly due to dissatisfaction with treatment outcomes. Understanding the various causes of acne across different age groups and recognizing its complex relationship with age is essential for effective management and treatment strategies.
15. Bacteria
Acne is a complex skin condition influenced by bacterial colonization, particularly by Cutibacterium acnes (formerly known as Propionibacterium acnes) and Staphylococcus species. These bacteria contribute to acne by causing inflammation and comedone formation within clogged hair follicles, thriving in excess sebum produced by sebaceous glands. As C. acnes multiplies, it triggers an inflammatory response and prompts the immune system to react, leading to redness, swelling, and pus in acne lesions. Dysbiosis of the skin microbiota, where C. acnes plays a crucial role, is linked to acne development, highlighting the importance of microbial balance in skin health. Research suggests that probiotics may help reduce skin eruptions in acne patients by restoring microbial balance, showing the potential of therapeutic interventions targeting the skin microbiota. Understanding the role of bacteria, especially C. acnes, in acne pathogenesis is crucial for developing targeted treatments that can effectively reduce bacterial colonization and inflammation, thereby alleviating the condition.
16. Menstruation
According to article, Menstruation is closely associated with the development of acne, particularly in young women. Approximately 51% of women experience acne flare-ups during menstruation, and nearly half of women between the ages of 12 and 52 are affected by acne during the premenstrual period. Hormonal fluctuations during the menstrual cycle, specifically the rise in progesterone and decrease in estrogen levels leading up to menstruation, can stimulate the sebaceous glands to produce more sebum. This excess sebum can clog pores and create an environment conducive to the growth of acne-causing bacteria. Furthermore, the hormonal imbalance that occurs during menopause, characterized by an increase in androgens, can result in clinical hyperandrogenism, which manifests as acne, hirsutism, and androgenetic alopecia. Managing stress and adhering to a consistent skincare routine can help alleviate some of the acne symptoms associated with menstruation. Understanding the relationship between menstruation and acne is essential for developing personalized management strategies that address hormonal influences and lifestyle factors to effectively treat acne during menstruation.
17. Personal care products
Acne is a chronic inflammatory skin condition that is common among teenagers and can be influenced by personal care products. Research suggests that the use of makeup, soaps, and sunscreen can expose individuals, particularly adolescent girls, to potential endocrine disruptors such as phthalates, parabens, and other phenols. These chemicals can affect hormone levels and skin health, with daily makeup use being associated with higher urinary concentrations of compounds like monoethyl phthalate (MEP) and parabens. Personal care products often contain ingredients like oils, silicones, and emollients that can clog pores, leading to comedones, as well as comedogenic substances that can worsen skin irritation and inflammation, ultimately exacerbating acne. The presence of endocrine disruptors in personal care products has been linked to negative health effects, including early puberty in girls, underscoring the importance of being mindful of the ingredients in products like toothpaste, cosmetics, and shampoos. Therefore, it is crucial for individuals prone to acne to carefully choose non-comedogenic and oil-free personal care products, regularly cleanse the skin to remove any product residue buildup, and understand the components of personal care items in managing acne and promoting overall skin health.
18. Poor Cell Turnover Rate
Acne is a common skin condition that primarily affects adolescents but can also occur in adults. It is influenced by various factors, including poor cell turnover rates. Research suggests that acne vulgaris is caused by a combination of dead skin cells, excessive sebum production, and bacterial growth, leading to blockages in hair follicles. Studies have shown that the turnover rate of facial skin cells is faster than that of back skin cells, and differences have been observed in the movement of labeled cells into comedones. When the skin’s natural exfoliation process slows down, dead skin cells can accumulate on the surface, clogging pores and trapping oil and bacteria, which can result in inflammation, blackheads, and acne development. Age, hormonal changes, and certain skincare products can affect cell turnover rate, making it an important factor to consider in acne prevention and treatment. By understanding the complexities of acne pathogenesis, including cellular kinetics and environmental influences, a more comprehensive approach to treatment can be developed to improve skin health and address misinformation about acne, particularly online, which often includes misconceptions about its causes, such as diet and unconventional cures.
19. Underlying Health Problems
According to article, Acne is a common skin condition that primarily affects adolescents but can also occur in adults. It is caused by a combination of factors, including hormonal imbalances during puberty, pregnancy, or conditions like polycystic ovary syndrome (PCOS), endocrine disorders, certain medications, high glycemic foods, dairy products, inflammation, and stress. The development of acne is influenced by the pathology of the pilosebaceous unit, which involves androgens, sebum, bacteria like Propionibacterium acnes, immunological responses, and genetic predispositions. Psychological distress, such as anxiety, depression, and low self-esteem, often accompanies acne due to dissatisfaction with treatment outcomes. Patients’ beliefs about diet, dirt, and sunlight as acne triggers also play a role in the development and management of acne. It is important to address these factors in treatment approaches and consult with healthcare professionals to determine if there are underlying health issues contributing to the skin condition. Understanding the various health problems that contribute to acne is essential for effective management and comprehensive care.
20. Lack of sleep
Poor sleep quality has been identified as a potential factor influencing the onset and severity of acne in adults. Research suggests a bidirectional relationship between sleep and skin health. Inadequate sleep can lead to increased androgen hormone activity, triggering excessive sebum production on the face and contributing to the development of acne vulgaris. Additionally, inadequate sleep can cause the body to experience stress and release cortisol, which can stimulate oil production in the skin’s sebaceous glands. Excess oil can clog pores, creating an ideal environment for acne-causing bacteria to thrive.
How is acne treated?
Acne is most commonly seen in teenagers as a result of hormonal fluctuations during puberty, but it can also impact individuals of any age. The visible signs of acne, including pimples, blackheads, and whiteheads, are a result of blocked hair follicles and can vary in severity. Fortunately, advancements in dermatology and a deeper understanding of the root causes of acne have led to the development of numerous effective treatments to effectively manage and control this troublesome skin condition.
1. Topical acne medications
Topical acne medications are the first-line treatment for mild to moderate acne, targeting early stages of lesions with minimal systemic side effects. These medications include a variety of options such as benzoyl peroxide, salicylic acid, retinoids, Azelaic acid, Dapsone and antibiotics, which work by reducing oil production, speeding up skin cell turnover, fighting bacterial infection, and preventing new acne from forming. While some topical treatments are available over-the-counter, others require a prescription and may be used alone or in combination with other treatments for more severe cases.
2. Oral acne medications
Oral medications are essential in the management of moderate to severe acne, especially when topical treatments are not effective. Antibiotics such as tetracyclines are frequently recommended for their ability to inhibit bacterial growth and reduce inflammation. Oral contraceptives and anti-androgen agents may be used to regulate hormone levels in cases of hormonal acne. In instances of severe, cystic acne that is unresponsive to other therapies, isotretinoin, a potent retinoid, may be prescribed with close monitoring due to potential side effects. Dermatologists customize the choice of medication based on the individual’s specific type of acne, its severity, and their response to previous treatments.
- Antibiotics
- Isotretinoin (Amnesteem, Claravis and Sotret)
- Oral Contraceptives
- Hormone therapy
3. Additional acne therapies
According to article, Acne treatment involves a range of approaches beyond conventional pharmacological therapies, including emerging treatments such as clascoterone, sarecycline, and trifarotene, as well as hormonal therapies, dietary control, counseling, dermocosmetics, chemical peels, and light-based therapies. These treatments can be used alone or in combination with pharmacological therapies, and are frequently combined with traditional treatments to improve outcomes and address more severe forms of acne.
- Steroid injection
- Lasers
- Chemical peeling
- Comedone extraction
4. Nonprescription Treatment for Acne
Non-prescription acne treatments, such as over-the-counter products containing active ingredients like benzoyl peroxide, salicylic acid, and alpha hydroxy acids, as well as non-pharmacological therapies like diet control, counseling, dermocosmetics, and various physical treatments, are important in the management of acne. These treatments are available in different forms and can be used alone, in combination with other therapies, or as maintenance treatment, to help optimize the effectiveness and tolerability of prescription acne treatments.
- Soap and water
- Cleansers
- Benzoyl peroxide
- Salicylic acid
- Sulfur
- Topical retinol gel or creams
- Alcohol and acetone
- Herbal, organic, and “natural” medications

Acne home remedies
While there are many over-the-counter and prescription medications on the market, a growing number of individuals are opting for natural home remedies to address their acne concerns. These alternative treatments frequently incorporate common household ingredients, providing a cost-effective and gentle method for managing acne. This article will examine some of the most popular and effective home remedies for acne that may assist in achieving clearer, healthier skin.
1. Apply tea tree oil
Tea tree oil, recognized for its antibacterial, anti-inflammatory, and antioxidant characteristics, has demonstrated potential as a natural treatment for acne. Research indicates that tea tree oil may decrease inflammatory lesions and severity of acne by eradicating colonies of Propionibacterium acnes. To utilize tea tree oil for acne management, dilute it with a carrier oil and administer the blend to the affected region, ensuring to conduct a patch test beforehand and seek advice from a healthcare professional if you have sensitive skin.
2. Apply aloe vera
Aloe vera has been extensively researched for its efficacy in treating acne, attributed to its antibacterial properties against Propionibacterium acnes and its ability to promote wound healing. Its nutrient-rich composition makes it a valuable ingredient in cosmetic products. To use aloe vera as an acne treatment, apply a thin layer of pure aloe vera gel directly to the affected area after cleansing, up to twice daily. It is recommended to perform a patch test and seek personalized advice from a dermatologist before use.
3. Sugar or salt scrubs
Sugar and salt scrubs are popular home remedies for acne due to their exfoliating properties. Sugar scrubs are preferred for their moisturizing effects and gentle granules, making them suitable for sensitive skin. On the other hand, salt scrubs have a drying effect and antiseptic qualities that can help reduce bacterial growth. It is important to use these scrubs carefully to prevent over-exfoliation and potential skin irritation. Consulting with a dermatologist for personalized advice is recommended.
4. Use a honey mask
Honey masks are a popular and effective home remedy for treating acne vulgaris. Studies have shown that honey masks can reduce inflammation, promote skin health, and aid in the healing process of acne. The composition of honey masks can vary, incorporating ingredients such as jojoba oil, tea tree oil, bamboo charcoal, traditional Chinese medicine components, silicone, vitamin E, and hyaluronic acid, which contribute to their efficacy in moisturizing, nourishing, cleansing, whitening, and promoting collagen synthesis. To use a honey mask, apply a thin layer of raw, organic honey directly onto clean skin, focusing on affected areas, and leave it on for 10-15 minutes before rinsing off with warm water. This gentle treatment can be used several times a week to help soothe the skin, reduce redness, and prevent new breakouts.
5. Green tea
Green tea has been extensively researched for its potential in treating acne because of its antioxidant, anti-inflammatory, and antibacterial properties. The polyphenols in green tea, especially epigallocatechin gallate (EGCG), can decrease inflammation, sebum production, and bacterial growth, which are important factors in acne formation. Using green tea topically, such as by applying cooled tea as a facial rinse or placing wet tea bags on affected areas, in addition to consuming green tea, can promote overall skin health. However, it is crucial to use these treatments cautiously and in consultation with a healthcare professional for persistent or severe acne conditions.
6. Avoid touching your face
In order to effectively manage acne using home remedies, it is important to refrain from touching the face. This is because touching the face can transfer bacteria and oils from the hands to the skin, which may exacerbate acne symptoms. Although breaking this habit may be difficult, avoiding contact between the hands and face reduces the introduction of impurities, helps the skin maintain its natural balance, and prevents irritation and potential scarring. By incorporating this simple yet impactful practice into your acne treatment routine, you can promote clearer skin and improve overall hygiene.
7. Never squeeze or pick pimples
According to article, when dealing with acne, it is important to avoid squeezing or picking at pimples, as this can push bacteria and pus further into the skin, leading to increased swelling, redness, and a higher risk of scarring. Instead, consider using gentler home remedies such as applying a warm compress, utilizing natural anti-inflammatory treatments like tea tree oil, or creating a mild exfoliating paste with baking soda and water. Maintaining a consistent skincare routine that includes gentle cleansing and the use of non-comedogenic moisturizers can also promote skin health and aid in more effective healing, ultimately reducing the likelihood of long-term damage.
8. Warm compress
A warm compress can be an effective home remedy for treating acne, especially for painful, pus-filled pimples. The warmth enhances blood circulation, speeds up the healing process, and softens the skin, facilitating easier drainage of the pimple without the need for aggressive squeezing that may cause scarring or additional infection. To utilize this technique, soak a clean washcloth in warm water, squeeze out the excess water, and gently apply it to the affected area for a few minutes at a time. Repeat this process several times a day to decrease inflammation and calm the skin.
9. Ice
Ice therapy is a promising home remedy for acne treatment, providing a natural and potentially effective solution. When applied to the skin, the cold temperature of ice constricts blood vessels, reducing inflammation, redness, and swelling associated with acne lesions. To use ice as an acne treatment, wrap a few cubes in a clean cloth or use an ice pack, and gently press against the affected area for a few minutes, taking breaks to prevent skin damage. While ice can offer temporary relief and assist in the absorption of active ingredients, it should be used alongside a comprehensive skincare routine to target the root causes of acne.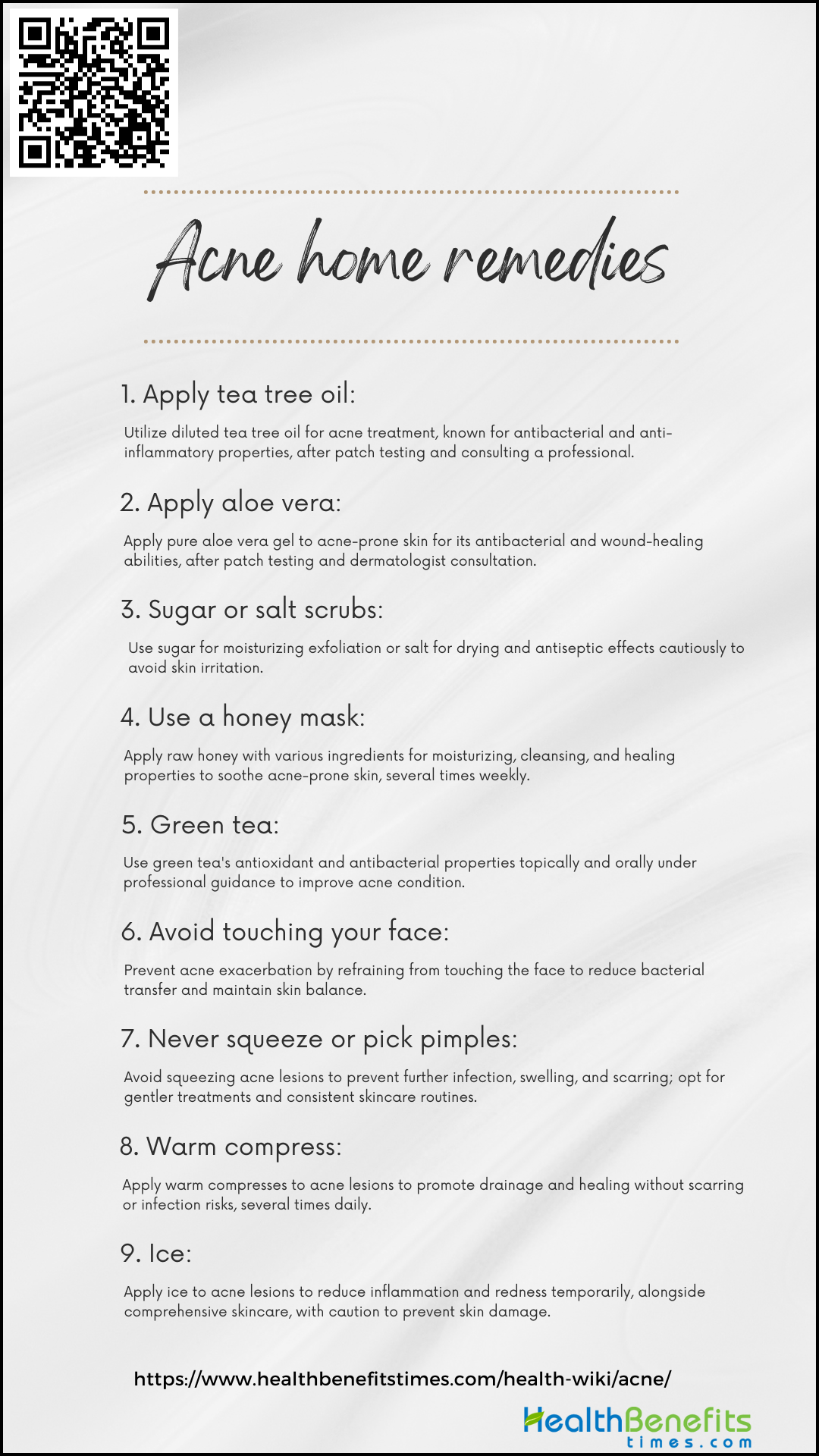
How to Prevent and manage acne?
Acne, a common skin condition that affects millions of people worldwide, can be a source of frustration, embarrassment, and even pain for those who suffer from it. Whether you’re a teenager going through puberty or an adult still dealing with breakouts, understanding how to prevent and manage acne is crucial for maintaining healthy, clear skin. While acne can be caused by a variety of factors, including genetics, hormones, and lifestyle choices, there are several effective strategies that can help minimize its impact and keep your skin looking its best. In this article, we’ll explore the causes of acne and provide practical tips for preventing and managing this pesky skin problem.
1. Don’t wear make-up every day
According to article, Preventing and managing acne requires a comprehensive approach, which includes being mindful of daily makeup usage, maintaining the skin’s natural balance with suitable skincare routines, and addressing specific challenges faced by individuals with skin of color. A regular skincare routine that incorporates cleansing, exfoliating, moisturizing, and allowing the skin to rest from makeup on certain days can effectively decrease the likelihood of breakouts and enhance the clarity and health of the skin.
2. Avoid touching your face as much
In order to prevent and manage acne effectively, it is important to minimize touching the face, as hands are exposed to various contaminants and bacteria that can clog pores and worsen acne. Following a consistent skincare regimen with suitable products and consulting a dermatologist when necessary are also crucial for optimal acne management and attaining clear, healthy skin.
3. Avoid popping spots
To prevent and manage acne effectively, it is crucial to resist the urge to pop pimples, as this can exacerbate inflammation, lead to further breakouts, or even cause scarring. Instead, maintain a consistent skincare routine that includes gentle cleansing, exfoliation, and the use of non-comedogenic moisturizers and treatments containing acne-fighting ingredients, and consult a dermatologist for persistent acne concerns.
4. Keep your skin cool
To manage and prevent acne effectively, it is important to maintain a cool skin environment by avoiding prolonged exposure to high temperatures and direct sunlight, using gentle, non-comedogenic skincare products, and cleansing promptly after sweating. Additionally, incorporating lightweight, breathable fabrics and soothing ingredients can help reduce skin irritation and the likelihood of breakouts.
5. Wear loose clothing
Wearing loose, breathable clothing can play a significant role in preventing and managing acne, particularly body acne caused by friction and excessive sweating. Opting for loose-fitting, absorbent fabrics like cotton allows air to circulate around the skin, reducing moisture buildup and minimizing the potential for clogged pores and irritation that can exacerbate breakouts.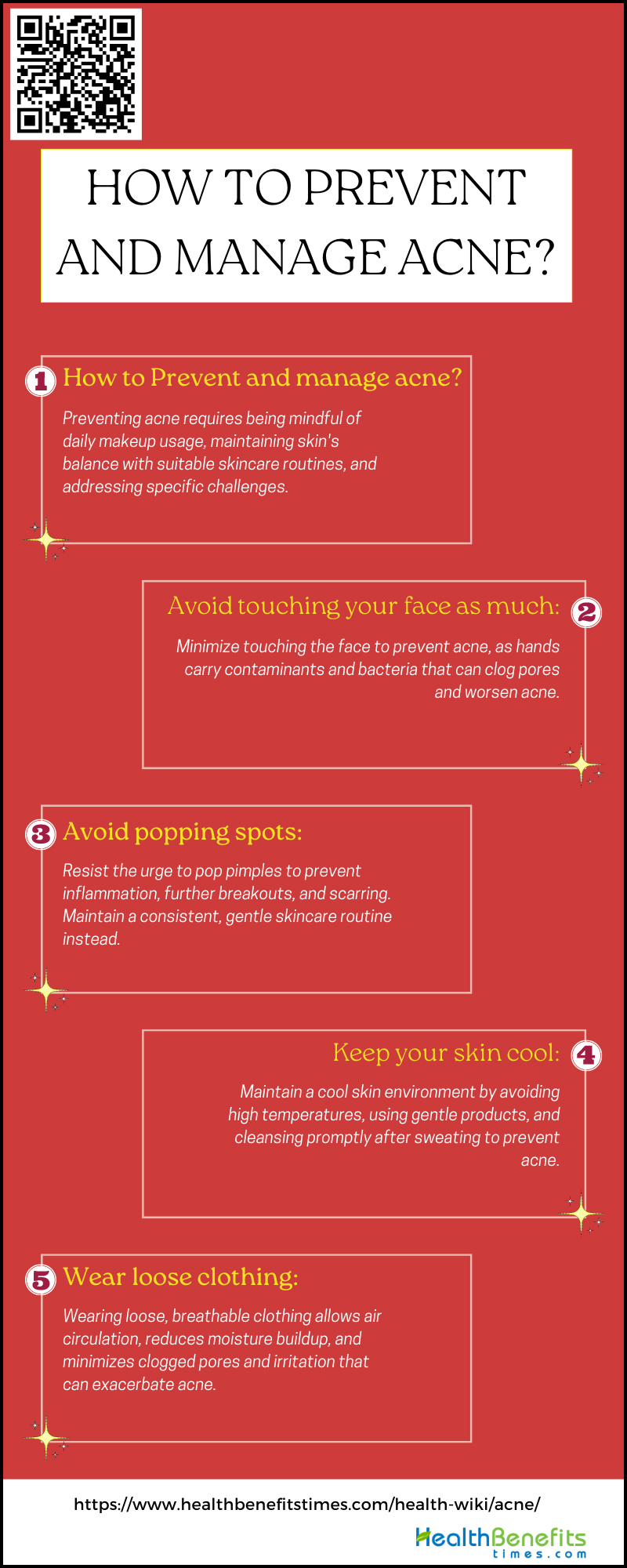
Complications of Acne
Acne, a prevalent skin condition that affects millions of individuals globally, is commonly viewed as a cosmetic concern. However, beneath the surface of this widespread ailment lies a complex network of potential complications that can significantly impact both physical and mental health. From the formation of permanent scarring to the psychological effects of diminished self-esteem, the repercussions of acne extend beyond the initial blemishes. It is essential to explore the various manifestations of acne complications and recognize the significance of timely intervention and appropriate management to minimize its lasting consequences.
1. Scarring
Acne scarring is a common complication that affects up to 95% of individuals with acne. It occurs when deep, inflamed lesions cause damage to the skin’s collagen fibers and tissue, resulting in changes in texture, indentations, and discoloration. The psychological effects of acne scars can be significant, leading to low self-esteem, social withdrawal, and an increased risk of depression. Prevention is important, but there are various treatment options available, including topical treatments and invasive procedures, that can be customized based on the type and severity of scarring to improve the skin’s appearance and smoothness.
2. Hyperpigmentation
Post-inflammatory hyperpigmentation (PIH) is a common complication of acne that affects both men and women. It occurs when healed acne lesions leave behind darkened patches due to an excess production of melanin. PIH can affect individuals of all skin tones, but it is more common and long-lasting in those with darker complexions, significantly impacting their quality of life for months to years. Treatment options include topical treatments and professional procedures, but prevention through acne management and sun protection is essential.
3. Infection
According to article, Acne-related infections, a potential complication of acne, can occur when lesions become infected with bacteria, leading to increased inflammation and potential pus formation. Gram-negative folliculitis (GNF) is a notable concern, especially in acne patients undergoing prolonged systemic antibiotic treatment, with various bacteria identified as potential causes. Maintaining a hygienic skincare routine, refraining from picking or squeezing lesions, and promptly seeking medical treatment for signs of infection are essential to prevent the advancement of infection and decrease the risk of scarring or more severe health complications.
4. Emotional distress
Acne vulgaris can significantly affect patients’ emotional well-being, as studies have shown strong associations between acne and psychological issues such as anxiety, depression, social phobia, and suicidal thoughts. The visibility and persistence of acne can cause embarrassment, low self-esteem, and social withdrawal. Therefore, it is important for healthcare providers to address both the physical and emotional aspects of acne by providing dermatological treatments and psychological support as needed.
Popular Acne Myths
- Acne is caused by having dirty skin and poor hygiene
- Squeezing blackheads, whiteheads and spots is the best way to get rid of acne
- Sexual activity can influence acne
- Sunbathing, sunbeds and sunlamps help improve the symptoms of acne
- Acne is infectious
- Using toothpaste in Acne