Acid reflux, also known as heartburn, is a condition characterized by a burning sensation in the chest or throat that frequently occurs after meals. It’s caused by the backflow of stomach contents, including acidic gastric juices, into the esophagus, a tube connecting the throat to the stomach. This reflux of acidic content can lead to symptoms like chest pain, a burning feeling in the chest, and acid regurgitation. While occasional episodes are common and can occur in nearly every person at some point, persistent acid reflux, experienced more than twice a week over several weeks, may indicate the development of Gastroesophageal Reflux Disease (GERD). GERD is a chronic digestive disorder that results from the reflux of stomach acids into the distal esophagus, causing irritation and inflammation of the esophageal lining. This condition is not only uncomfortable however can lead to more serious health issues if left untreated, which includes esophageal damage.
Causes of Acid Reflux
Acid reflux, a situation characterized by the uncomfortable ascent of stomach acid into the esophagus, can disrupt daily life with its bothersome symptoms. While occasional episodes are common, persistent acid reflux can indicate gastroesophageal reflux disease (GERD). The underlying causes of acid reflux are multifaceted, involving anatomical, lifestyle, and dietary factors that compromise the function of the lower esophageal sphincter or increases gastric pressure, leading to the backflow of acid. Understanding these contributing elements is necessary for effective management and treatment. Below is a list of common causes that can trigger acid reflux:
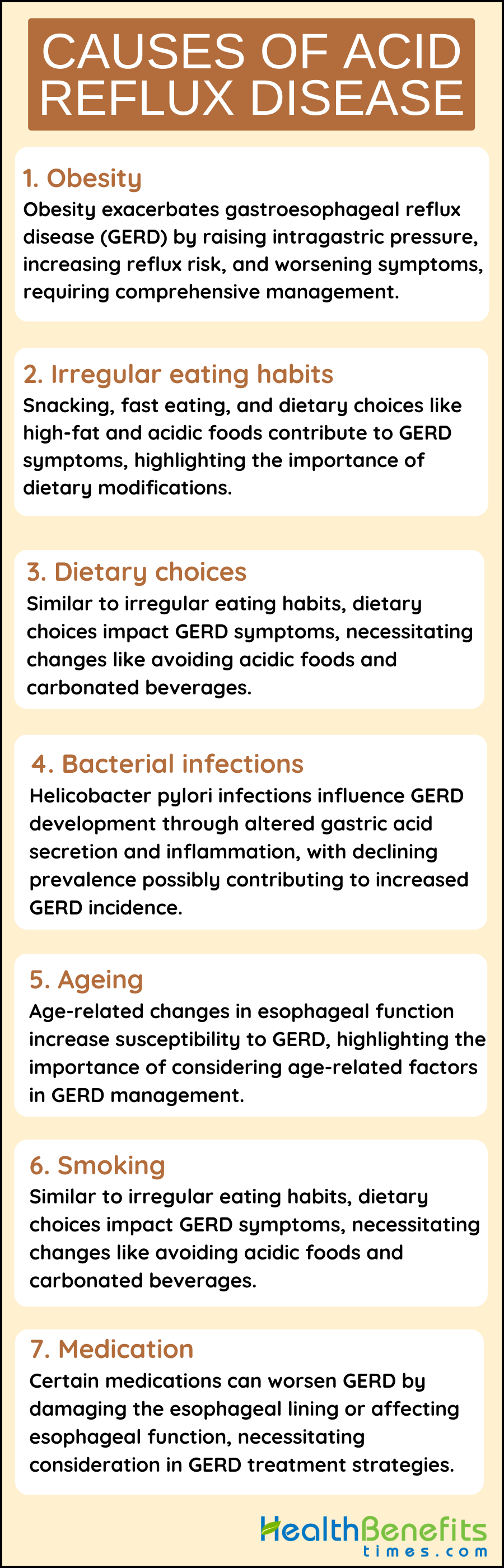
1. Obesity
Obesity is an important contributor to the growth of gastroesophageal reflux disease (GERD), a condition characterized by the backflow of stomach contents into the esophagus, leading to symptoms like heartburn and acid regurgitations. The relationship between obesity and GERD is well-established, with obesity increasing the risk of GERD along numerous mechanisms. One primary way in which obesity worsens GERD is by raising intragastric pressure, which weakens the esophagogastric junction and facilitates the reflux of gastric contents into the esophagus. Additionally, obesity, particularly visceral fat obesity, is linked to a higher occurrence of transient lower esophageal sphincter relaxations and abnormal peristalsis, further promoting reflux.
2. Irregular eating habits
Irregular eating habits play a significant role in the development and worsening of acid reflux disease, also known as gastroesophageal reflux disease (GERD), through various mechanisms. The practice of snacking and consuming soft drinks between main meals, which is common in Western lifestyles, leads to increased gastric acid secretion and temporary relaxation of the lower esophageal sphincter (TLESRs), resulting in higher levels of acid in the esophagus and persistent GERD symptoms. Fast eating and overeating are recognized as major risk factors for GERD, as they can overwhelm the digestive system and raise intra-abdominal pressure, causing stomach contents to reflux into the esophagus. Additionally, dietary choices such as high-fat diets and the consumption of spicy and acidic foods have been linked to worsening GERD symptoms by relaxing the lower esophageal sphincter and delaying stomach emptying, increasing the likelihood of acid reflux. The consumption of carbonated beverages has also been associated with an increased risk of developing GERD, likely due to their role in causing gastric distension and TLESRs. Furthermore, lifestyle factors like eating close to bedtime or wearing tight clothing can worsen GERD symptoms by raising abdominal pressure and promoting gastric reflux. The complex relationship between these irregular eating habits and lifestyle factors emphasizes the importance of making dietary and behavioral changes in the management and prevention of GERD, highlighting the necessity of a comprehensive treatment approach that addresses these modifiable risk factors.
3. Dietary choices
Irregular eating habits play a significant role in the development and worsening of acid reflux disease, also known as gastroesophageal reflux disease (GERD), through various mechanisms. The practice of snacking and consuming soft drinks between main meals, which is common in Western lifestyles, leads to increased gastric acid secretion and temporary relaxation of the lower esophageal sphincter (TLESRs), resulting in higher levels of acid in the esophagus and persistent GERD symptoms. Fast eating and overeating are recognized as major risk factors for GERD, as they can overwhelm the digestive system and raise intra-abdominal pressure, causing stomach contents to reflux into the esophagus. Additionally, dietary choices such as high-fat diets and the consumption of spicy and acidic foods have been linked to worsening GERD symptoms by relaxing the lower esophageal sphincter and delaying stomach emptying, increasing the likelihood of acid reflux. The consumption of carbonated beverages has also been associated with an increased risk of developing GERD, likely due to their role in causing gastric distension and TLESRs.
4. Bacterial infections
Bacterial infections, especially Helicobacter pylori (H. pylori), are known to play a major role in the pathogenesis of gastroesophageal reflux disease (GERD) by affecting gastric acid secretion and the inflammatory response in the gastrointestinal tract. H. pylori infection can result in changes in acid secretion, with the location of the infection within the stomach determining its impact on the development of GERD. It is noteworthy that the prevalence of H. pylori infection has been declining, particularly in Western populations, which may be contributing to the increasing incidence of GERD, Barrett’s esophagus, and esophageal adenocarcinoma seen in recent years. Additionally, research has indicated that eradicating H. pylori may reveal underlying GERD symptoms by reducing inflammation, underscoring the intricate relationship between bacterial infections and acid reflux disease.
5. Ageing
Aging is a significant factor contributing to the development of Gastroesophageal Reflux Disease (GERD) due to various physiological changes in the gastrointestinal tract. As individuals age, alterations in esophageal motility and sensory functions occur, potentially increasing the susceptibility to complications like GERD. While it was previously believed that gastric acid secretion decreased with age, recent research indicates that this decline may be linked to Helicobacter pylori infection and atrophic gastritis, conditions that have become less prevalent in recent decades. Additionally, age-related changes can lead to a reduction in esophageal sphincter tone and clearance mechanisms, making the esophageal mucosa more vulnerable to reflux and subsequent inflammation, which are key components of GERD development. These age-related physiological changes, combined with factors like comorbidities and medication use, contribute to the increased risk of GERD in older individuals.
6. Smoking
Smoking is a significant contributor to acid reflux disease. It is considered an etiological factor of Gastroesophageal Reflux Disease (GERD), as it decreases lower esophageal sphincter pressure and saliva production, both of which are essential for clearing acid in the esophagus. Research has shown that heavy smokers are more likely to experience symptoms of GERD, and there is a noticeable link between smoking and Body Mass Index (BMI) in patients with GERD. Furthermore, smoking can induce reflux episodes by reducing lower esophageal sphincter pressure, allowing gastric contents to flow back into the esophagus. The harmful effects of smoking on the esophageal lining make individuals more susceptible to acid-related damage, worsening GERD symptoms. Therefore, quitting smoking is recommended to lower the risk of developing or exacerbating acid reflux symptoms, underscoring the importance of lifestyle changes in managing GERD.
7. Medication
Medications can have a significant impact on the development and worsening of Gastroesophageal Reflux Disease (GERD). Certain drugs can directly cause damage to the mucosa, decrease pressure in the lower esophageal sphincter (LESP), or affect the movement of food from the esophagus to the stomach, all of which can lead to the emergence or exacerbation of GERD symptoms. For example, anti-inflammatory drugs, non-steroidal medications like aspirin, estrogenic drugs, progesterones, hormone replacement therapy, diphosphonates, calcium channel blockers, nitrates, antidepressants, benzodiazepines, sleep aids, drugs that block acetylcholine, theophylline, and medications for asthma have been linked to GERD. It is important to consider the potential impact of these medications on the gastrointestinal system when treating patients with GERD, as they can contribute to the underlying causes of the disease and affect the effectiveness of treatment.
Symptoms of Acid Reflux Disease
Symptoms of acid reflux disease, also known as gastroesophageal reflux disease (GERD), encompass a range of manifestations affecting various body systems. Common symptoms include heartburn, regurgitation, chest pain, and epigastric pain, with some patients experiencing these symptoms primarily after eating. In addition, atypical symptoms such as cough, laryngitis, asthma, and dental erosions may also be present, indicating manifestations of the disease beyond the esophagus. Refractory GERD, characterized by symptoms that persist despite twice-daily proton pump inhibitor (PPI) therapy, can lead to complications such as chronic cough, chronic laryngitis, and dental erosions. Patients with confirmed reflux micro-aspiration often exhibit symptoms such as regurgitation, cough, heartburn, throat clearing, and dysphonia, demonstrating the varied clinical presentation of reflux-related issues. The presence of GERD-related symptoms alongside upper abdominal symptoms can have a significant impact on daily life and quality of life, underscoring the importance of comprehensive symptom management in GERD patients.
- Heartburn
- Acid regurgitation
- Chest pain
- Cough
- Sleep pattern disturbance
- Nausea
- Vomiting
- Mouth ulcers
- Toothache
- Loose teeth
- Bleeding gums
- Periodontitis
- Regurgitation
- Cough
- Throat clearing
- Dysphonia
- Bloat
- Constipation
- Epigastric pain
- Asthma
- Chronic cough
- Pharyngitis
- Laryngitis
- Sleep disturbances
How Is Acid Reflux Disease Diagnosed?
Acid reflux disease, or gastroesophageal reflux disease (GERD), is diagnosed through a combination of clinical evaluation and specialized tests. Physicians typically start with a thorough medical history and a physical examination, focusing on symptoms and dietary habits. When symptoms are not entirely indicative of GERD or when treatment does not alleviate the discomfort, more definitive diagnostic procedures may be employed. These methods not only confirm the presence of acid reflux but also assess the severity of the condition and check for potential complications. Below is a list of diagnostic methods used to identify acid reflux diseases?
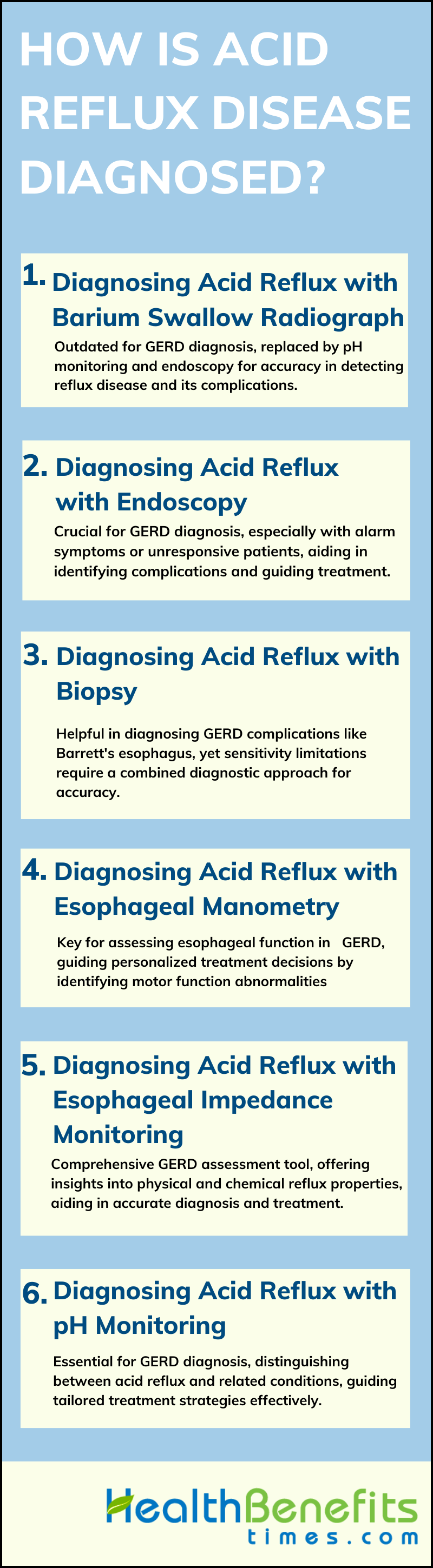
1. Diagnosing Acid Reflux with a Barium Swallow Radiograph
The use of a barium swallow radiograph for diagnosing acid reflux disease, also known as gastroesophageal reflux disease (GERD), is not recommended according to recent guidelines. While this radiographic technique can detect anatomical abnormalities that may present symptoms similar to GERD, its sensitivity and specificity are lower compared to pH monitoring, which is considered the gold standard for GERD diagnosis. This diagnostic test, which involves visualizing the esophagus after ingesting a barium sulfate solution, tracks the movement of the barium through the esophagus and into the stomach. It allows a radiologist to assess the structure and function of the esophagus, identify any abnormalities such as strictures or hiatal hernias, and observe if there is any backflow of barium, indicating reflux. Despite its non-invasive nature and provision of valuable information for the diagnosis and management of acid reflux, the test’s lower sensitivity and specificity make it less preferred for GERD diagnosis according to current guidelines.
2. Diagnosing Acid Reflux with Endoscopy or EGD
According to the article, Acid reflux disease can be diagnosed using various methods. Endoscopy, or esophagogastroduodenoscopy (EGD), is recommended for patients with alarm symptoms or those who do not respond well to proton-pump inhibitors. This procedure helps identify complications of GERD, detect potential alternative diagnoses, and assess the esophagogastric junction for anatomical or physiological abnormalities. Additionally, pH-impedance monitoring and esophageal manometry are useful tools for characterizing the amount of reflux, determining symptom patterns, and identifying esophageal motility issues. These tests help establish the link between abnormal reflux and symptoms, guide treatment decisions, and identify patients who may benefit from anti-reflux surgery. In cases where symptoms persist despite proton pump inhibitor therapy, functional esophageal tests are important for defining the specific characteristics of GERD based on reflux exposure, motility issues, and symptom severity. This information can help tailor effective treatment strategies.
3. Diagnosing Acid Reflux with a Biopsy
Diagnosing acid reflux disease, particularly non-erosive reflux disease (NERD), with a biopsy involves evaluating esophageal mucosal samples for histological abnormalities. Although traditional methods such as upper endoscopy with biopsies have been commonly used for diagnosing gastroesophageal reflux disease (GERD), they may have limitations in sensitivity. However, biopsies taken within 3 cm of the lower esophageal sphincter (LES) have shown improved sensitivity when specific histologic features such as eosinophils and dilated intraepithelial spaces are taken into consideration. In cases where patients do not respond to proton pump inhibitor therapy, endoscopy with biopsies becomes essential for diagnosing conditions such as Barrett esophagus, dysplasia, and adenocarcinoma. Overall, while biopsies play a role in diagnosing acid reflux disease, a comprehensive approach that combines various diagnostic methods like pH monitoring and impedance testing is often necessary for accurate diagnosis and management.
4. Diagnosing Acid Reflux with Esophageal Manometry
According to article, Esophageal manometry, particularly high-resolution manometry, is an important diagnostic tool for assessing esophageal motor function in patients with gastroesophageal reflux disease (GERD). It is recommended for cases of difficulty swallowing and when standard treatments do not rule out other conditions or before anti-reflux surgery. Esophageal manometry helps identify problems with the barrier function at the junction between the esophagus and stomach, as well as issues with esophageal muscle function, which are key factors in GERD. Recent international guidelines stress the significance of high-resolution manometry in the diagnostic process for GERD to determine the specific type of GERD for personalized treatment. By using the Chicago classification version 4.0 and including new measures for evaluating GERD, esophageal manometry assists in accurately identifying and measuring esophageal abnormalities, guiding treatment decisions for patients with acid reflux disease.
5. Diagnosing Acid Reflux with Esophageal Impedance Monitoring
Diagnosing acid reflux disease, particularly with esophageal impedance monitoring, involves various techniques outlined in the literature. The use of hypopharyngeal multichannel intraluminal impedance-pH (HMII-pH) technology has been developed to detect pharyngeal reflux, with a high rate of validation for candidate pharyngeal acid reflux episodes and good interobserver reproducibility. Combined impedance-pH monitoring (MII-pH) is recommended for a comprehensive assessment of both physical and chemical properties of the refluxate to achieve a conclusive diagnosis of gastro-esophageal reflux disease (GERD), especially in cases of diagnostic uncertainty. Additionally, prolonged reflux monitoring, extending up to 96 hours, has shown increased diagnostic yield due to day-to-day variability in acid exposure levels, emphasizing the importance of patient activities during monitoring to reduce variation in esophageal acid exposure levels.
6. Diagnosing Acid Reflux with pH Monitoring
Diagnosing acid reflux often involves pH monitoring to assess the presence and severity of acid reflux. This procedure involves placing a small sensor in the esophagus to measure the acidity levels over a 24 to 48-hour period. The sensor transmits data to a portable recorder worn by the patient, tracking acid levels during normal eating, sleeping, and activities. This method provides a direct and objective measurement of acid exposure in the esophagus, which is particularly useful for patients whose symptoms are not clearly indicative of acid reflux, or for those who do not respond to treatment. The results help physicians to confirm a diagnosis of GERD, tailor treatment plans, and assess the effectiveness of medications or surgical interventions. pH monitoring can also differentiate between GERD and laryngopharyngeal reflux (LPR) in patients with swallowing disorders, providing essential information on the characteristics of reflux events. It can distinguish between liquid acid esophageal events typical in GERD and gaseous weakly acid or nonacid pharyngeal reflux events often seen in LPR.
Treatment of Acid Reflux?
The treatment of acid reflux, or gastroesophageal reflux disease (GERD), involves a multifaceted approach aimed at relieving symptoms and preventing complications. Strategies range from lifestyle modifications to medication and, in severe cases, surgical interventions. The goal is to reduce the frequency and severity of reflux episodes, heal any esophageal damage, and manage or eliminate the discomfort associated with the condition. Below is a list of common treatment methods for acid reflux:
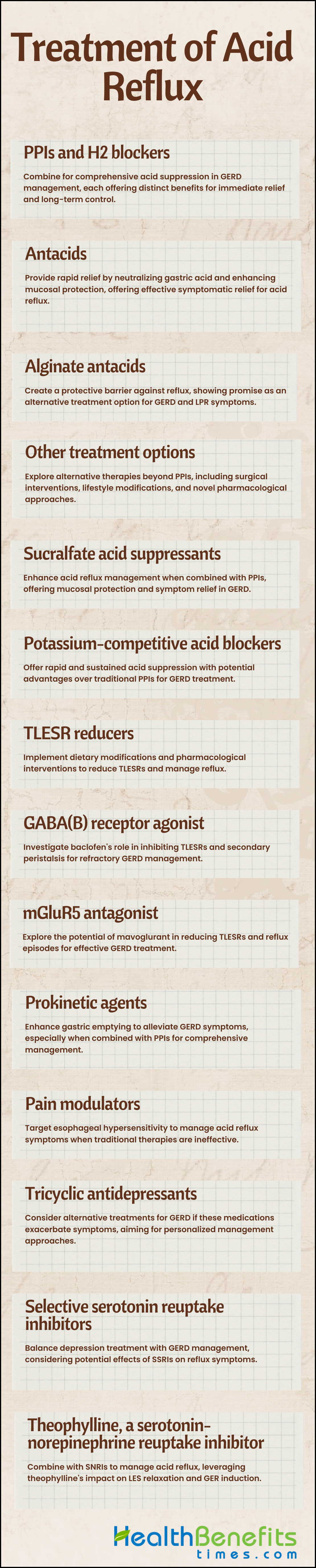
1. PPIs and H2 blockers
According to article, to effectively manage acid reflux, a combination of Proton Pump Inhibitors (PPIs) and Histamine H2 receptor antagonists (H2 blockers) can be used. PPIs, like omeprazole and lansoprazole, are commonly prescribed for acid-related disorders like gastroesophageal reflux disease (GERD) and peptic ulcer disease (PUD) because they inhibit gastric acid production by blocking the H+/K+ ATPase pump. However, PPIs have limitations such as slow onset of action and meal-associated dosing. On the other hand, H2 blockers like ranitidine and famotidine suppress gastric acid production by blocking H2 receptors in parietal cells. Combining PPIs for long-term acid suppression with H2 blockers for immediate symptom relief can provide a comprehensive approach to managing acid reflux effectively.
2. Antacids
According to article, to effectively alleviate symptoms of acid reflux, antacids play a crucial role by directly neutralizing gastric acid, increasing gastric pH, and providing relief from associated conditions. Antacids containing aluminum hydroxide and magnesium hydroxide demonstrate superior therapeutic efficacy with fewer side effects, sustained elevation of gastric pH, and rapid pain relief. Additionally, antacids have cytoprotective and gastroprotective effects by stimulating the synthesis of bicarbonate and prostaglandins, enhancing mucosal protection, and promoting local reparative processes. These medications also have enveloping and adsorbing actions, binding aggressive substances in the gastrointestinal tract, and regulating motility in the stomach and duodenum. By using antacids with high neutralizing capacities, such as Digene, individuals can achieve rapid symptomatic relief from acid reflux. Therefore, incorporating antacids as the first-line treatment for heartburn can greatly improve the quality of life for individuals experiencing symptoms of acid reflux.
3. Alginate antacids
According to article, In order to effectively address acid reflux using alginate antacids, it is crucial to understand their mechanism of action and comparative efficacy. Alginate antacids, such as Gastrotuss®, create a non-systemic barrier against acid reflux by forming a neutral ‘raft’ that displaces the postprandial acid pocket, providing protection to the esophageal mucosa during reflux episodes. Studies have demonstrated that alginate suspensions are comparable to proton pump inhibitors (PPIs) in reducing laryngopharyngeal reflux (LPR) symptoms and signs, making them a viable alternative treatment option with minimal adverse effects. While PPIs are generally more effective in controlling symptoms of gastroesophageal reflux disease (GERD) compared to alginate antacids, the latter have shown promise, particularly in patients with non-erosive reflux disease (NERD). The combination of mucosal adhesion and reflux action of alginate antacids presents an appealing opportunity for developing topical therapies against reflux and as potential drug delivery vehicles for conditions such as eosinophilic esophagitis.
4. Other treatment options
To address acid reflux beyond traditional proton pump inhibitors (PPIs), there are various alternative treatment options available. These include histamine-2 receptor antagonists (H2RAs), alginates, antacids, mucosal protective agents, potassium competitive acid blockers (PCABs), prokinetics, gamma aminobutyric acid-B (GABA-B) receptor agonists, metabotropic glutamate receptor-5 (mGluR5) antagonists, and pain modulators, as outlined in the study by Rettura et al. Surgical interventions such as laparoscopic antireflux surgery (LARS), endoscopic transoral incisionless fundoplication (TIF), magnetic sphincter augmentation (LINX), and radiofrequency therapy (Stretta) are also viable options for refractory cases, as discussed by Clarke and d8yjowi816. Lifestyle modifications, acid suppression, and strengthening the esophagogastric junction are key strategies, with surgical management becoming increasingly popular for those unresponsive to medical therapy, as highlighted by Melvin and Dumitru et al.
5. Sucralfate acid suppressants
To effectively manage acid reflux, a combination of treatments can be considered. Acid suppressive therapy (AST), particularly proton pump inhibitors (PPIs), is commonly used for symptomatic relief in gastroesophageal reflux disease (GERD). Additionally, drugs like sucralfate, a mucosal protective coating agent, have shown efficacy in alleviating chronic heartburn, especially in patients with mild reflux symptoms. Studies have compared sucralfate with H2-receptor antagonists for treating reflux esophagitis, with results indicating that sucralfate can be an effective alternative treatment for reflux disease
6. Potassium-competitive acid blockers
In order to effectively address acid reflux, particularly using potassium-competitive acid blockers (PCABs), it is important to understand their distinct advantages over traditional treatments such as proton pump inhibitors (PPIs). PCABs, including vonoprazan and tegoprazan, offer rapid onset of action, sustained acid suppression, and independence from meal timing. These novel acid suppressants demonstrate superior efficacy in healing erosive esophagitis, gastric ulcers, and eradicating Helicobacter pylori, highlighting their potential in managing acid-related disorders. PCABs provide complete acid suppression after a single dose, exhibit less variability with CYP2C19 polymorphisms, and have extended half-lives, making them valuable additions to clinical practice for treating gastroesophageal reflux disease and other acid peptic disorders.
7. Transient lower esophageal sphincter relaxation (TLESR) reducers
To reduce acid reflux associated with transient lower esophageal sphincter relaxations (TLESRs), dietary modifications can play a crucial role. Research has shown that meals containing wheat noodles, which are part of a high FODMAP diet, can increase the frequency of TLESRs and worsen symptoms of gastroesophageal reflux disease (GERD) compared to meals containing rice noodles, which are part of a low FODMAP diet. Additionally, studies have examined the effects of pharmacological interventions on TLESRs, with results indicating that ONO-8539, an EP1 receptor antagonist, can modestly reduce TLESRs in humans.
8. GABA (B) receptor agonist
To address acid reflux, especially in cases of refractory gastroesophageal reflux disease (GERD), the use of GABA (B) receptor agonists such as baclofen has been investigated. Baclofen, a gamma-aminobutyric acid agonist, has demonstrated potential in inhibiting secondary peristalsis induced by esophageal acid infusion, thereby reducing symptoms associated with acid reflux. Additionally, GABA (B) receptor agonists have been shown to decrease transient lower esophageal sphincter relaxations (TLESRs), which play a crucial role in gastroesophageal reflux events, suggesting a potential therapeutic approach for managing GERD-related symptoms. While the effectiveness of baclofen as an adjunct therapy to proton pump inhibitors (PPIs) for refractory GERD is still under debate, its ability to modulate acid-induced esophageal perception and secondary peristalsis underscores its potential in alleviating acid reflux symptoms.
9. mGluR5 antagonist
To effectively address acid reflux using mGluR5 antagonists, such as mavoglurant and AZD2066, research suggests promising outcomes in inhibiting transient lower esophageal sphincter relaxations (TLESRs) and reducing reflux episodes in patients with gastroesophageal reflux disease (GERD) who have persistent symptoms despite proton pump inhibitor (PPI) treatment. Studies have shown that mGluR5 antagonists like mavoglurant can significantly decrease the number of TLESRs and reflux episodes, leading to a potential clinical benefit in managing GERD. In addition, the mGluR5 antagonist ADX10059 has demonstrated a reduction in acid reflux and improvement in clinical symptoms in GERD patients, indicating a potential role in the clinical management of the condition. These findings highlight the promising role of mGluR5 antagonists in addressing acid reflux by targeting the underlying mechanisms involved in GERD.
10. Prokinetic agents
To effectively manage acid reflux, especially in cases where proton pump inhibitors (PPIs) are not effective, adding prokinetic agents to the treatment plan has shown promise. Prokinetics are important for improving the emptying of the stomach, which can help reduce symptoms of gastroesophageal reflux disease (GERD) and other upper gastrointestinal issues. Research has shown that combining prokinetics with PPIs can significantly improve overall symptom relief in patients with GERD. While PPIs are still the main treatment for GERD, adding prokinetics has been shown to enhance symptom response and improve quality of life for patients. Prokinetics like itopride hydrochloride have been proven effective in treating motility disorders that contribute to the development of GERD, making them a valuable addition to the treatment options available.
11. Pain modulators
To address acid reflux, especially in cases where proton pump inhibitors (PPIs) are ineffective, pain modulators can be a beneficial treatment option. Pain modulators, traditionally used for functional esophageal disorders, have shown promise in managing conditions such as non-erosive reflux disease and hypersensitive esophagus that do not respond to PPI therapy. These medications, which include tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and others, can help alleviate symptoms by modulating esophageal pain. In cases where patients have weakly acidic or weakly alkaline reflux as the underlying cause of their symptoms, pain modulators are recommended as part of the personalized treatment plan. By targeting esophageal hypersensitivity and other contributing factors, pain modulators offer a valuable approach to managing acid reflux when traditional therapies are not effective.
12. Tricyclic antidepressants
To address acid reflux associated with tricyclic antidepressants, it is important to consider the potential worsening of gastroesophageal reflux disease (GERD) by these medications. Tricyclic antidepressants have been linked to an increased risk of GERD, while selective serotonin reuptake inhibitors (SSRIs) do not have the same association. If patients on tricyclic antidepressants continue to experience persistent GERD symptoms, alternative treatment strategies may be required. Proton pump inhibitors (PPIs) are commonly used as the first-line treatment for GERD, but approximately 20-30% of patients may need different medications due to inadequate response. For patients with non-erosive reflux disease (NERD) who do not respond to standard PPI therapy, options such as prokinetics, reflux inhibitors, or even tricyclic antidepressants may be considered to effectively manage symptoms. Therefore, a comprehensive approach involving a combination of medications tailored to individual patient needs is crucial in addressing acid reflux related to tricyclic antidepressants.
13. Selective serotonin reuptake inhibitors (SSRIs)
To alleviate symptoms of acid reflux in patients with gastroesophageal reflux disease (GERD), the use of selective serotonin reuptake inhibitors (SSRIs) like citalopram has been investigated. Studies have demonstrated that combining citalopram with traditional GERD treatments like esomeprazole and sodium alginate can affect reflux symptoms in patients with moderate to severe depression and/or anxiety. Research suggests that while SSRIs like citalopram are commonly used as first-line treatments for depression, they may have negative effects on the gastrointestinal system, potentially impacting the function of the lower esophageal sphincter and worsening GERD symptoms. Therefore, when managing acid reflux in patients with GERD who also have depression or anxiety, healthcare providers should consider the potential effects of SSRIs on reflux symptoms and adjust treatment strategies accordingly.
14. Theophylline, a serotonin-norepinephrine reuptake inhibitor
To address acid reflux, the combination of theophylline and serotonin-norepinephrine reuptake inhibitors (SNRIs) may be beneficial. Theophylline has been shown to decrease lower esophageal sphincter pressure (LESP) and induce gastroesophageal reflux (GER) in healthy adults. Conversely, SNRIs are commonly used as first-line treatment for depression but may also lead to the development of GERD symptoms. By combining theophylline and SNRIs, it is possible to effectively manage acid reflux. This approach takes advantage of the impact of theophylline on LESP relaxation and GER induction, while also considering the potential development of GERD associated with SNRIs. Therefore, a comprehensive treatment strategy involving theophylline and SNRIs can be a valuable approach in addressing symptoms of acid reflux.
Holistic Treatment methods of Acid Reflux
Holistic treatment methods for acid reflux focus on a comprehensive approach that considers the whole person—body, mind, and spirit—to achieve optimal health and wellness. Rather than solely targeting the symptoms, holistic therapies aim to identify and address the root causes of acid reflux. These methods often involve natural remedies, dietary adjustments, lifestyle changes, and stress-reducing techniques that work in harmony to restore the body’s balance and alleviate the discomfort associated with acid reflux. Below is a list of holistic treatment methods for acid reflux:
1. Eat sparingly and slowly
Slowing down the pace of eating has consistently been associated with reduced food intake and potential benefits for weight management, as indicated by multiple studies. Research suggests that eating slowly allows for better recognition of satiety, potentially preventing overeating. In addition, mindfulness and techniques for slow eating have been recommended in weight loss programs, showing trends towards decreased energy intake and prevention of increased intake compared to normal eating behaviors. Time-restricted feeding (TRF), a type of intermittent fasting that involves eating within specific time windows, has shown promise in reducing calorie intake and improving hypertension through mechanisms involving changes in immune cell populations and inflammatory cytokines. These findings collectively emphasize the importance of eating slowly and sparingly as effective strategies for managing food intake, promoting satiety, and potentially aiding in weight and blood pressure control.
2. Avoid certain foods
Various methods for avoiding specific foods are essential for individuals with particular dietary requirements or health concerns. Computerized systems have been created to identify unsafe items on menus for individuals with food restrictions by analyzing ingredient information and potential cross-contamination risks. In the management of childhood eczema, a common approach involves identifying and avoiding underlying allergens, despite the presence of myths and misconceptions regarding the role of food in the disease’s pathophysiology. Additionally, to prevent urinary tract infections, it is recommended to consume cranberry juice and avoid certain products such as salt, coffee, and meat. When it comes to outdoor risks, it is advisable to refrain from consuming wild mushrooms and educate children to do the same, as distinguishing between safe and poisonous varieties can be difficult. These various methods highlight the importance of personalized approaches to food avoidance based on individual needs and health conditions.
3. Don’t drink carbonated beverages
Consuming carbonated beverages, especially in excess, can have negative effects on health. Research has shown that excessive consumption of carbonated beverages, both carbonated and non-carbonated, can increase the risk of diabetes by impacting C-peptide levels, which are important for insulin secretion. Additionally, carbonated soft drinks have been found to contain harmful substances that can lead to long-term health issues, underscoring the importance of reducing intake. It is crucial to explore alternative beverages and methods to stay hydrated and maintain overall health. Non-carbonated soft drinks, which are processed with strict standards and typically pasteurized for safety, can be a healthier choice compared to carbonated options. By choosing non-carbonated beverages and decreasing the consumption of carbonated drinks, individuals may be able to reduce the risks associated with excessive intake of sugary and artificially flavored beverages.
4. Stay up after eating
According to article, various methods have been explored in different contexts, including staying awake after eating. While traditional methods such as acupuncture, moxibustion, laser acupuncture, and herbal treatments have been commonly used to address chronic conditions, new approaches focusing on the energy bases of therapy have emerged to improve the effectiveness of these treatments. In the realm of technology, combining server-side and client-side approaches has been suggested to enhance functionality and address issues when using email applications. Additionally, research has highlighted the challenges faced by Hispanic students in developing proficient writing skills, which may be related to cultural and linguistic differences. These diverse methods and strategies demonstrate the ongoing evolution and adaptation in various fields to address complex issues and improve outcomes.
5. Don’t move too fast
According to article, Rapid movement and the integration of multiple methods can negatively impact efficiency and performance, as supported by research. A study on software method usage demonstrates that familiarity with multiple methods for a task can lead to increased errors and longer planning times, ultimately impeding user efficiency. Similarly, in the realm of business development, entering the market hastily without a solid plan and sufficient resources often results in failure, highlighting the importance of balancing speed with thorough preparation. Additionally, time constraints in healthcare settings present challenges that underscore the adverse effects of haste, such as disregarding patient preferences and making suboptimal decisions. Therefore, the warning against excessive speed and the potential drawbacks of incorporating additional methods offer valuable insights across various fields, underscoring the importance of deliberate planning and strategic decision-making.
6. Sleep on an incline
Sleeping on an incline has shown promising results in various health conditions. Research by Danoff-Burg et al. demonstrated that using an adjustable bed base to sleep with the upper body inclined at 12 degrees led to a reduction in snoring duration and improved sleep quality, with fewer awakenings and increased time spent in deep sleep. Additionally, Iwanaga highlighted the potential benefits of incline sleeping for individuals with hypertension or hypotension, suggesting that specific incline positions could help alleviate these conditions within a few days. Moreover, Minson’s invention of an inflatable, wedge-shaped incline mattress aimed at relieving Gastric Esophageal Reflux Disease (GERD) further supports the positive impact of sleeping on an incline for health purposes. These studies collectively indicate that incline sleeping may offer noninvasive and effective methods to address various health concerns and improve overall sleep quality.
7. Lose weight if it’s advised
Additional methods for weight loss include a psychological approach focusing on self-control skill learning through a psychological contract for compliance with a rational diet. Another method involves a complex food formulation designed for weight reduction by 4-6 kg per month, emphasizing low glycemic index, low fat, and low salt percentage foods, along with specific meal plans and fasting days. Furthermore, internet-based behavioral interventions with regular face-to-face or remote support have shown effectiveness in primary care settings for weight management, resulting in significant weight reduction and maintenance of valuable weight loss over time. These diverse methods offer individuals various strategies to effectively lose weight when advised to do so, catering to different preferences and needs for successful weight management.
8. Quit Smoking
Various additional methods have been explored for smoking cessation, as supported by research findings. The Population Assessment of Tobacco and Health (PATH) Study identified e-cigarettes as a commonly used method for quitting smoking, demonstrating higher success rates compared to attempts without assistance. A study on adult cigarette smokers in the US found that substituting some cigarettes with e-cigarettes was more common than traditional nicotine replacement therapies, indicating the need for further research on the effectiveness of e-cigarettes as a cessation aid. Physicians in Iran preferred combination methods and Nicotine Replacement Therapy (NRT) as effective strategies for quitting smoking, with e-cigarettes receiving lower effectiveness ratings. A review of smoking cessation methods highlighted the support for NRT and Champix, suggesting a combination of these methods with educational interventions for successful outcomes. Aversion therapy using onion-powdered cigarettes was also studied, showing promising results as an adjunct to behavioral therapy in smoking cessation programs.