Acetylcholinesterase (AChE) is a crucial enzyme in the nervous system that plays a vital role in neurotransmission by breaking down the neurotransmitter acetylcholine (ACh) at synapses. This enzyme is primarily found in neuromuscular junctions and cholinergic synapses in the central nervous system, where it rapidly hydrolyzes acetylcholine, thereby terminating synaptic transmission. The importance of AChE is underscored by its involvement in various physiological processes and its relevance in several pathological conditions, particularly neurodegenerative disorders like Alzheimer’s disease. In Alzheimer’s disease, the decrease in acetylcholine levels in the brain is partly attributed to increased AChE activity, leading to cognitive decline and other symptoms. As a result, acetylcholinesterase inhibitors (AChEIs) have been developed as a primary treatment strategy for Alzheimer’s disease, aiming to increase acetylcholine levels in the brain by inhibiting the enzyme’s activity. Understanding the structure, function, and regulation of AChE is crucial for developing effective treatments for neurodegenerative disorders and other conditions affecting the nervous system.
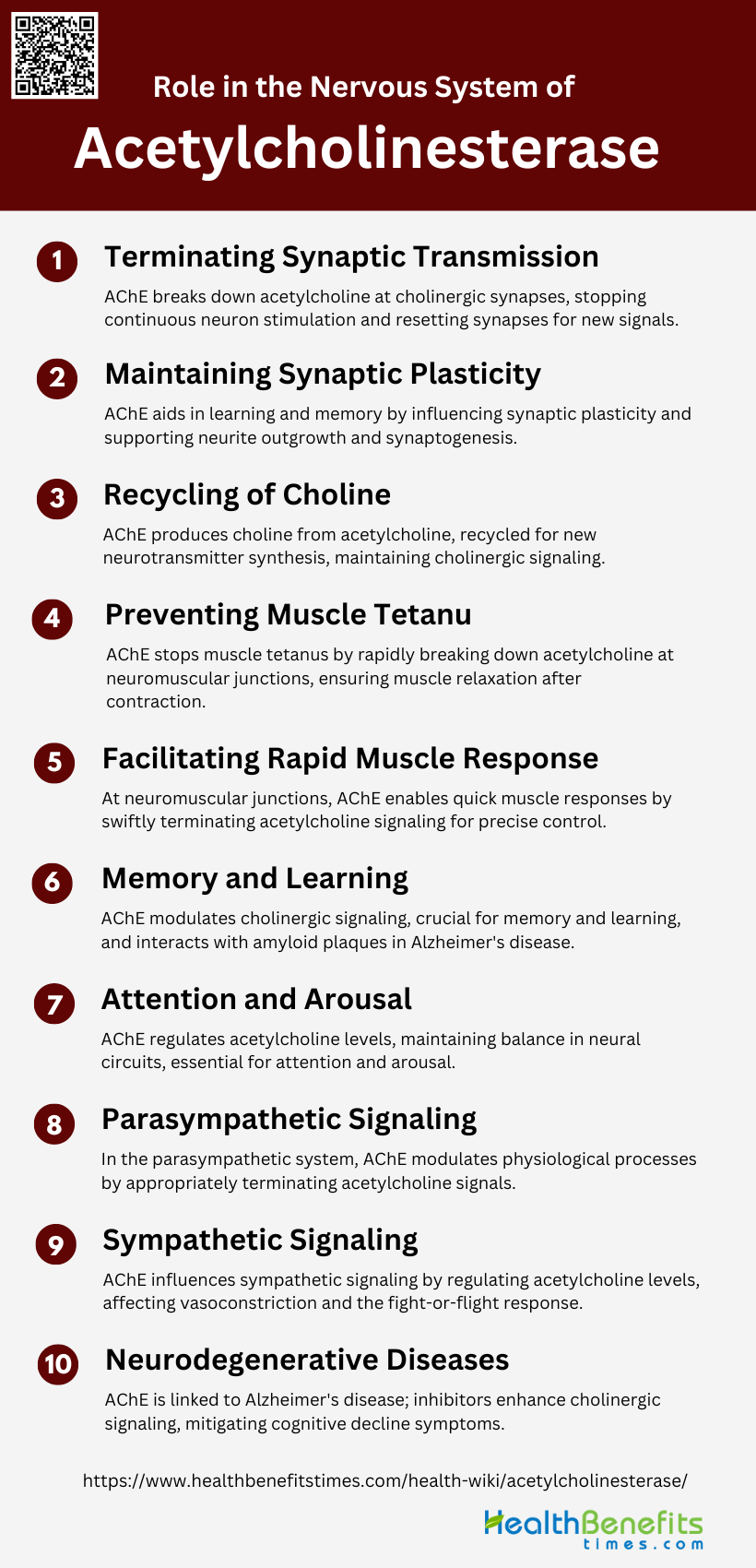
Role in the Nervous System of Acetylcholinesterase
Acetylcholinesterase (AChE) plays a crucial role in the nervous system by breaking down the neurotransmitter acetylcholine at synaptic clefts, thereby terminating synaptic transmission. This enzyme ensures that nerve impulses are not continuously sent, which is essential for proper muscle function and cognitive processes. Below are key points highlighting its significance in the nervous system:
1. Terminating Synaptic Transmission
Acetylcholinesterase (AChE) plays a crucial role in terminating synaptic transmission at cholinergic synapses by hydrolyzing the neurotransmitter acetylcholine (ACh) into acetate and choline. This rapid breakdown of ACh ensures that the neurotransmitter does not persist in the synaptic cleft, thereby preventing continuous stimulation of the postsynaptic neuron and allowing the synapse to reset for the next signal.
2. Maintaining Synaptic Plasticity
AChE is also implicated in maintaining synaptic plasticity, which is essential for learning and memory. Beyond its enzymatic role, AChE influences neurite outgrowth and synaptogenesis, contributing to the structural and functional plasticity of synapses. These non-enzymatic roles are facilitated by the diverse molecular forms of AChE, which interact with various protein partners to modulate synaptic architecture and signaling pathways.
3. Recycling of Choline
The hydrolysis of ACh by AChE produces choline, which is then recycled back into the presynaptic neuron. This recycled choline is used to synthesize new ACh molecules, thus maintaining the supply of the neurotransmitter for subsequent synaptic transmission. The high-affinity choline transporter (CHT1) is responsible for the reuptake of choline, ensuring efficient recycling and sustained cholinergic signaling.
4. Preventing Muscle Tetanus
AChE prevents muscle tetanus by rapidly breaking down ACh at neuromuscular junctions (NMJs). This rapid hydrolysis ensures that muscle fibers are not continuously stimulated, which would otherwise lead to sustained, involuntary muscle contractions known as tetanus. The presence of AChE in the synaptic cleft is critical for the proper relaxation of muscles after contraction.
5. Facilitating Rapid Muscle Response
At NMJs, AChE facilitates rapid muscle response by ensuring the swift termination of ACh signaling. This allows for quick and precise control of muscle contractions, enabling rapid and coordinated movements. The collagen-tailed A12 form of AChE, concentrated in the synaptic cleft, is particularly effective in curtailing the postsynaptic response through ultrafast ACh hydrolysis.
6. Memory and Learning
AChE is involved in memory and learning through its role in modulating cholinergic signaling in the brain. The enzyme’s non-enzymatic functions, such as influencing neurite outgrowth and synaptogenesis, are crucial for the formation and maintenance of neural circuits associated with cognitive processes. Additionally, AChE’s interaction with amyloid plaques in Alzheimer’s disease highlights its significance in neurodegenerative conditions affecting memory.
7. Attention and Arousal
Cholinergic signaling, modulated by AChE, plays a vital role in attention and arousal. AChE ensures the precise regulation of ACh levels in the synaptic cleft, which is essential for maintaining the balance between excitation and inhibition in neural circuits. This balance is crucial for cognitive functions such as attention and arousal, which are mediated by cholinergic neurons in the basal forebrain.
8. Parasympathetic Signaling
In the parasympathetic nervous system, AChE regulates the activity of ACh at synapses involved in rest-and-digest functions. By hydrolyzing ACh, AChE ensures that parasympathetic signals are terminated appropriately, allowing for the modulation of physiological processes such as heart rate, digestion, and glandular secretion. This regulation is essential for maintaining homeostasis.
9. Sympathetic Signaling
Although AChE is primarily associated with cholinergic synapses, it also plays a role in modulating sympathetic signaling. In certain contexts, AChE can influence the activity of sympathetic neurons by regulating ACh levels, thereby affecting processes such as vasoconstriction and the fight-or-flight response. The enzyme’s ability to modulate both parasympathetic and sympathetic signaling underscores its versatility in the nervous system.
10. Neurodegenerative Diseases
AChE is implicated in neurodegenerative diseases such as Alzheimer’s disease (AD). The enzyme’s interaction with amyloid plaques and its role in cholinergic neuron loss contribute to the cognitive decline observed in AD patients. Inhibitors of AChE are used as therapeutic agents to enhance cholinergic signaling and mitigate symptoms of AD, highlighting the enzyme’s significance in the pathology and treatment of neurodegenerative conditions.
Mechanism Action of Acetylcholinesterase
How AChE Breaks Down Acetylcholine
Acetylcholinesterase (AChE) terminates nerve impulse transmission at cholinergic synapses by rapidly hydrolyzing the neurotransmitter acetylcholine. The enzyme achieves this through a highly efficient catalytic process that involves two key sites: the acylation site (A-site) at the base of the active site gorge and the peripheral site (P-site) at the gorge entrance. The A-site is where acetylcholine is hydrolyzed, forming a short-lived acyl-enzyme intermediate. The P-site aids in substrate trapping and can modulate the catalytic efficiency by either facilitating or inhibiting substrate access to the A-site.
Chemical Reactions Involved
The hydrolysis of acetylcholine by AChE involves a two-step chemical reaction: acylation and deacylation. Initially, acetylcholine binds to the A-site, where it undergoes nucleophilic attack by the serine residue, forming an acetyl-enzyme intermediate and releasing choline. This is the acylation step. Subsequently, water molecules hydrolyze the acetyl-enzyme intermediate, releasing acetate and regenerating the free enzyme. This is the deacylation step. The entire process is facilitated by the enzyme’s active site residues, including serine, histidine, and glutamate, which form a catalytic triad essential for the reaction.
Role of Active Sites in AChE
The active sites of AChE play crucial roles in its catalytic function. The acylation site (A-site) at the base of the active site gorge is responsible for the hydrolysis of acetylcholine, forming a transient acyl-enzyme intermediate. The peripheral site (P-site) at the entrance of the gorge assists in substrate binding and can either enhance or inhibit catalysis. The P-site mediates substrate trapping and can cause steric blockade of the A-site, affecting the overall catalytic efficiency. Additionally, ligand binding to the P-site can result in allosteric activation or inhibition of the enzyme, further modulating its activity.
Types of Acetylcholinesterase Inhibitors
Acetylcholinesterase inhibitors (AChEIs) are compounds that prevent the breakdown of acetylcholine, enhancing cholinergic transmission. These inhibitors are used in various therapeutic applications, including the treatment of Alzheimer’s disease and myasthenia gravis. Below are the main types of acetylcholinesterase inhibitors:
1. Reversible Inhibitors
Reversible acetylcholinesterase inhibitors are compounds that bind non-covalently to the enzyme, leading to a temporary inhibition of its activity. These inhibitors, such as donepezil, tacrine, and edrophonium, are characterized by their ability to dissociate from the enzyme, allowing for the restoration of acetylcholinesterase activity over time. The reversible nature of these inhibitors makes them suitable for therapeutic applications where temporary inhibition is desired, such as in the treatment of Alzheimer’s disease. Studies have shown that these inhibitors can be effectively evaluated using techniques like Lineweaver-Burk plot analysis to determine their kinetic parameters and inhibitory constants. Additionally, novel reversible inhibitors have been designed to provide long-lasting protection against organophosphate poisoning, demonstrating their potential in both therapeutic and prophylactic settings.
2. Irreversible Inhibitors
Irreversible acetylcholinesterase inhibitors form covalent bonds with the enzyme, leading to permanent inactivation. These inhibitors, like organophosphates and certain carbamates, are often used in pesticides and chemical warfare agents. The irreversible binding results in a long-lasting inhibition of acetylcholinesterase, which can be detrimental in cases of poisoning. But, irreversible inhibitors also hold potential therapeutic benefits, particularly in the treatment of neurodegenerative diseases like Alzheimer’s. Research has shown that irreversible inhibitors can achieve higher levels of enzyme inhibition in the central nervous system, potentially offering improved anti-neurodegenerative benefits compared to reversible inhibitors. The development of irreversible inhibitors that specifically target the anionic binding site of acetylcholinesterase has also been explored, highlighting their potential for precise therapeutic applications.
3. Quasi-Irreversible (Pseudo-Irreversible) Inhibitors
Quasi-irreversible or pseudo-irreversible inhibitors form a stable but not permanent bond with acetylcholinesterase, leading to prolonged inhibition that can eventually be reversed. These inhibitors, such as certain carbamate derivatives like physostigmine and rivastigmine, undergo a process of carbamoylation and decarbamoylation, which allows for the recovery of enzyme activity over time. Pseudo-irreversible inhibitors are particularly valuable in therapeutic contexts where extended inhibition is beneficial, but complete irreversibility is not desired. For instance, in the treatment of Alzheimer’s disease, these inhibitors can provide sustained enzyme inhibition with a lower risk of toxicity compared to fully irreversible inhibitors. Studies have demonstrated the effectiveness of pseudo-irreversible inhibitors in both in vitro and in vivo models, supporting their potential as preclinical candidates for further development.
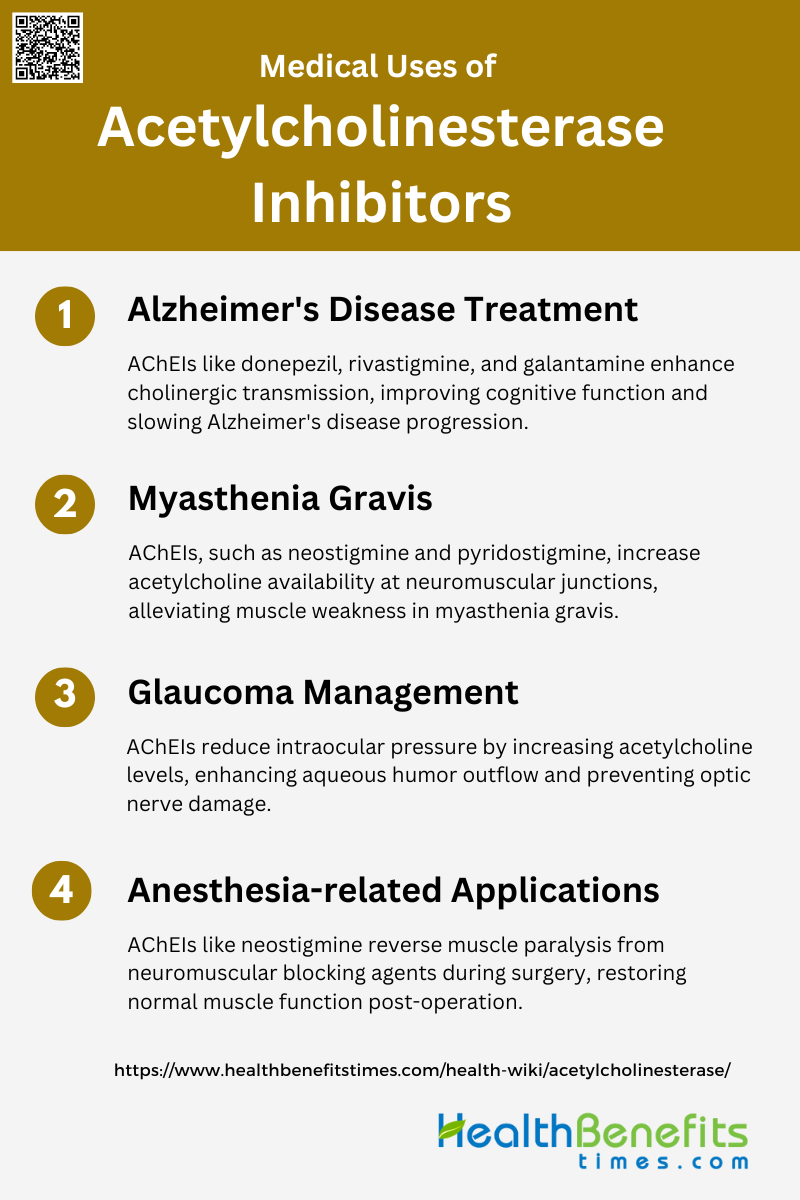
Medical uses of Acetylcholinesterase inhibitors
Acetylcholinesterase inhibitors (AChEIs) are widely used in the medical field to manage and treat several neurological and muscular disorders. By preventing the breakdown of acetylcholine, these inhibitors enhance communication between nerve cells. Below are the primary medical uses of acetylcholinesterase inhibitors:
1. Alzheimer’s Disease Treatment
Acetylcholinesterase inhibitors (AChEIs) are a cornerstone in the symptomatic treatment of Alzheimer’s disease (AD). These inhibitors work by preventing the breakdown of acetylcholine, a neurotransmitter crucial for memory and learning, thereby enhancing cholinergic transmission in the brain. Drugs such as donepezil, rivastigmine, and galantamine have been developed and approved for this purpose, showing efficacy in improving cognitive function and slowing disease progression. Recent research continues to explore new AChEIs, including naturally derived compounds and synthetic analogues, to improve efficacy and reduce side effects. The ongoing development of these inhibitors underscores their importance in managing AD symptoms.
2. Myasthenia Gravis
In myasthenia gravis, acetylcholinesterase inhibitors are used to alleviate muscle weakness by increasing the availability of acetylcholine at the neuromuscular junction. This compensates for the antibody-mediated blockade of acetylcholine receptors characteristic of the disease. Although these inhibitors provide temporary symptomatic relief, their long-term efficacy and optimal dosage remain subjects of debate. Despite the lack of large randomized controlled trials, observational studies have shown clear benefits, making it ethically challenging to conduct placebo-controlled trials. Commonly used AChEIs for myasthenia gravis include neostigmine and pyridostigmine, which have been shown to improve muscle strength and reduce fatigue.
3. Glaucoma Management
Acetylcholinesterase inhibitors also play a role in the management of glaucoma, a condition characterized by increased intraocular pressure that can lead to optic nerve damage. By inhibiting acetylcholinesterase, these drugs increase the levels of acetylcholine, which in turn enhances the outflow of aqueous humor through the trabecular meshwork, thereby reducing intraocular pressure. This mechanism helps to prevent further optic nerve damage and preserve vision. Although primarily used for neurological disorders, the application of AChEIs in glaucoma management highlights their versatility and potential in treating a range of conditions.
4. Anesthesia-related Applications
In the context of anesthesia, acetylcholinesterase inhibitors are used to reverse the effects of non-depolarizing neuromuscular blocking agents, which are commonly administered during surgical procedures to induce muscle relaxation. By inhibiting acetylcholinesterase, these drugs increase acetylcholine levels at the neuromuscular junction, thereby counteracting the muscle paralysis induced by the blocking agents. This facilitates the recovery of normal muscle function post-surgery. Neostigmine is one of the most commonly used AChEIs for this purpose, often administered in combination with anticholinergic agents to mitigate potential side effects such as bradycardia.
Symptoms of Acetylcholinesterase deficiency
Acetylcholinesterase deficiency can lead to a range of symptoms due to the accumulation of acetylcholine at nerve synapses. This condition affects both the nervous and muscular systems, resulting in various physiological and neurological issues. Below are the common symptoms of acetylcholinesterase deficiency:
- Generalized Weakness Increased by Exertion: Patients with acetylcholinesterase (AChE) deficiency often exhibit generalized muscle weakness that worsens with physical activity. This symptom is consistently observed across multiple studies and is a hallmark of the condition.
- Fatigue and Lack of Resistance to Fatigue: A prominent symptom of AChE deficiency is the lack of resistance to fatigue. This is particularly evident in neuromuscular functioning, where affected individuals show a significant decrease in muscle force during repetitive nerve stimulations.
- Ophthalmoplegia and Ptosis: Some patients with AChE deficiency experience ophthalmoplegia (paralysis or weakness of the eye muscles) and ptosis (drooping of the upper eyelid). These symptoms can vary in severity and are not always present in all cases.
- Decremental Electromyographic Response: A decremental response in electromyographic studies is a common finding in patients with AChE deficiency. This means that the muscle response to nerve stimulation decreases progressively, which is indicative of impaired neuromuscular transmission.
- Muscle Atrophy and Immaturity: Muscle atrophy and immaturity of the neuromuscular junction are significant symptoms observed in models of congenital myasthenic syndrome with AChE deficiency. These conditions lead to a general atrophic phenotype and hypoplasia, particularly affecting fast muscles.
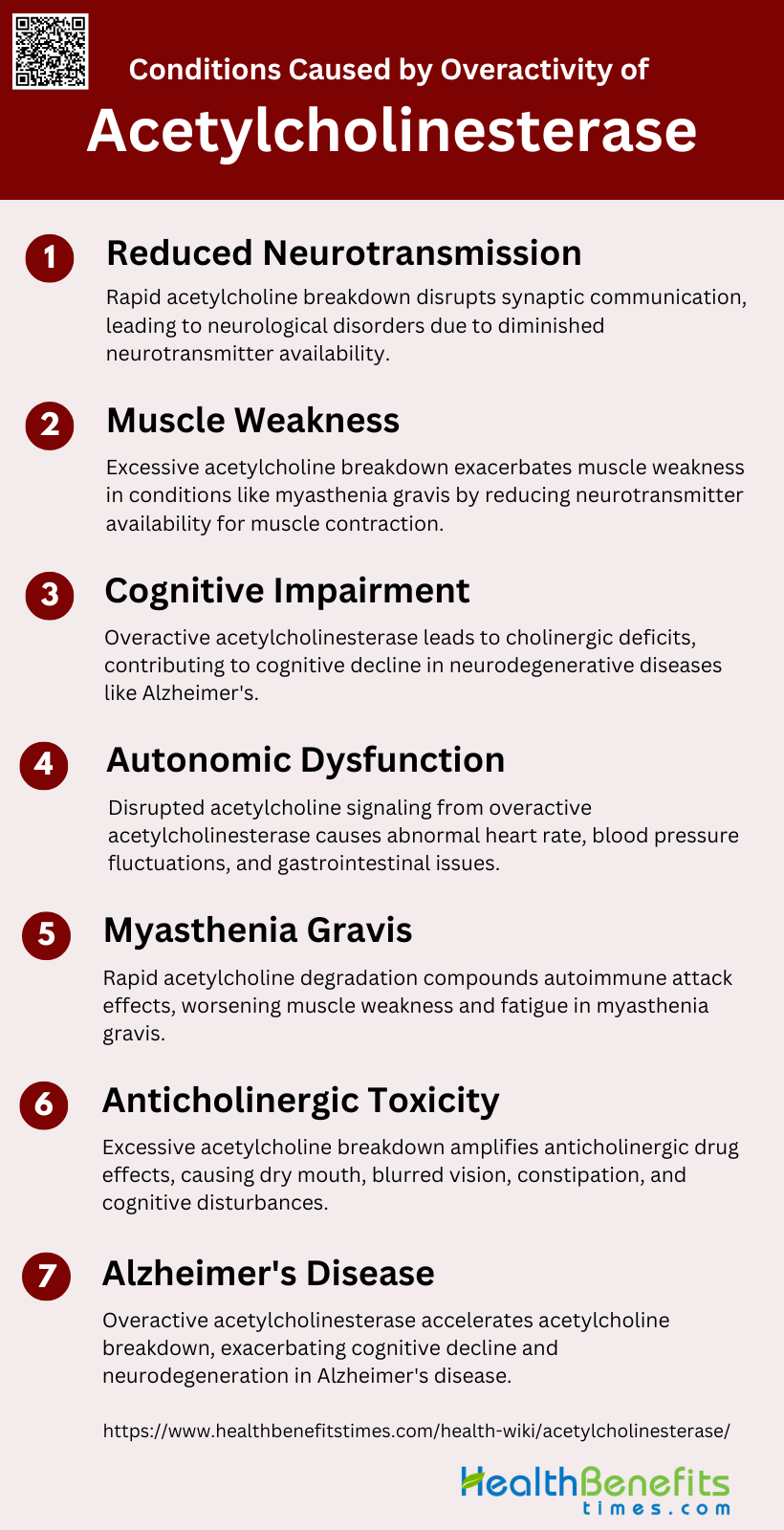
Conditions caused by overactivity of Acetylcholinesterase
Overactivity of acetylcholinesterase can lead to a rapid breakdown of acetylcholine, resulting in insufficient neurotransmission. This imbalance can cause several neurological and muscular conditions, affecting overall bodily functions. Below are the conditions caused by overactivity of acetylcholinesterase:
1. Reduced Neurotransmission
Overactivity of acetylcholinesterase (AChE) leads to the rapid hydrolysis of acetylcholine, a crucial neurotransmitter, resulting in reduced neurotransmission. This enzyme’s high efficiency in breaking down acetylcholine can disrupt normal synaptic communication, leading to impaired signal transmission across cholinergic synapses. The imbalance caused by excessive AChE activity can contribute to various neurological disorders, as the neurotransmitter’s availability is significantly diminished, affecting both central and peripheral nervous systems. This reduction in neurotransmission is a fundamental issue in conditions like Alzheimer’s disease, where cholinergic deficits are prominent.
2. Muscle Weakness
Muscle weakness is a common symptom associated with the overactivity of acetylcholinesterase, particularly in conditions like myasthenia gravis. In this autoimmune disorder, antibodies block acetylcholine receptors at the neuromuscular junction, and the excessive breakdown of acetylcholine by AChE exacerbates the problem by further reducing the availability of this neurotransmitter for muscle contraction. The temporary symptomatic relief provided by AChE inhibitors highlights the enzyme’s role in muscle function, although their long-term efficacy and side effects remain subjects of debate. The rapid hydrolysis of acetylcholine by AChE thus directly impacts muscle strength and endurance.
3. Cognitive Impairment
Cognitive impairment is significantly influenced by the overactivity of acetylcholinesterase, particularly in neurodegenerative diseases like Alzheimer’s. The excessive breakdown of acetylcholine leads to a cholinergic deficit, which is closely linked to cognitive decline. AChE inhibitors are used to mitigate these effects by increasing acetylcholine levels, thereby improving cognitive function and slowing disease progression. However, the enzyme’s overactivity can still result in substantial cognitive deficits, as seen in the reduced neurotransmission and impaired synaptic plasticity associated with Alzheimer’s disease.
4. Autonomic Dysfunction
Autonomic dysfunction can arise from the overactivity of acetylcholinesterase, affecting the autonomic nervous system’s regulation of involuntary bodily functions. The rapid degradation of acetylcholine disrupts normal autonomic signaling, leading to symptoms such as abnormal heart rate, blood pressure fluctuations, and gastrointestinal issues. This dysfunction is particularly evident in conditions where cholinergic signaling is crucial for maintaining homeostasis, and the excessive activity of AChE can severely impair these regulatory mechanisms.
5. Myasthenia Gravis
In myasthenia gravis, the overactivity of acetylcholinesterase compounds the effects of the autoimmune attack on acetylcholine receptors. The enzyme’s rapid breakdown of acetylcholine reduces the neurotransmitter’s availability at the neuromuscular junction, exacerbating muscle weakness and fatigue. AChE inhibitors are commonly used to provide symptomatic relief by increasing acetylcholine levels, although their long-term benefits and potential side effects are still under investigation. The interplay between immune-mediated receptor blockade and excessive acetylcholine degradation underscores the complexity of managing this condition.
6. Anticholinergic Toxicity
Anticholinergic toxicity can result from the overactivity of acetylcholinesterase, as the excessive breakdown of acetylcholine leads to a relative increase in the effects of anticholinergic agents. This imbalance can cause a range of symptoms, including dry mouth, blurred vision, constipation, and cognitive disturbances. The toxicity arises because the reduced availability of acetylcholine amplifies the inhibitory effects of anticholinergic drugs on cholinergic signaling, leading to significant physiological and neurological disruptions.
7. Alzheimer’s disease
Alzheimer’s disease is closely associated with the overactivity of acetylcholinesterase, which contributes to the cholinergic deficits observed in this condition. The enzyme’s excessive activity leads to the rapid breakdown of acetylcholine, exacerbating cognitive decline and neurodegeneration. AChE inhibitors are a primary treatment strategy, aiming to increase acetylcholine levels and improve cognitive function. Additionally, the interaction between AChE and amyloid-β peptides in Alzheimer’s can further enhance neurotoxicity and disease progression. The enzyme’s role in Alzheimer’s underscores the importance of targeting AChE to manage and potentially slow the disease’s progression.