The Acetaminophen Level Test is a blood test used to measure the concentration of acetaminophen (also known as paracetamol) in a person’s bloodstream. This test is primarily used to diagnose and monitor cases of acetaminophen overdose or toxicity. Healthcare providers typically order this test when they suspect a patient has ingested excessive amounts of acetaminophen, either accidentally or intentionally. The results of the test are often plotted on the Rumack-Matthew nomogram, a tool that helps predict the likelihood of liver toxicity based on the acetaminophen concentration and the time since ingestion. The test is crucial for determining appropriate treatment, such as the administration of N-acetylcysteine, which can prevent or reduce liver damage if given within a specific timeframe after ingestion. It’s important to note that in cases of extended-release acetaminophen formulations, multiple tests may be necessary to accurately assess the risk of toxicity, as the drug’s release pattern can affect its concentration in the blood over time.
When is the Test Needed?
Determining the right time for medical testing is vital in addressing potential health crises, such as overdoses or poisoning. Tests provide essential information that guides treatment decisions and improves patient outcomes. Below are key scenarios where testing becomes imperative for effective medical intervention.
1. Suspected Overdose
When a patient is suspected of an overdose, immediate testing is crucial to identify the substance involved and guide appropriate treatment. The initial assessment often relies on clinical signs and symptoms, which can be the only clues to the diagnosis when the cause of toxicity is unknown. Quick identification of the drug or toxin through a careful history, physical examination, and laboratory tests is essential for effective management and prognosis. Comprehensive drug screening can significantly improve decision-making in emergency departments, enhancing agreement among physicians on patient management and potentially saving hospital resources.
2. Presence of Symptoms
The presence of symptoms indicative of drug intoxication necessitates testing to confirm the diagnosis and identify the specific substance involved. Symptoms can range from mild to severe and may include altered mental status, respiratory depression, and cardiovascular instability. In cases of suspected opioid intoxication, for example, the administration of naloxone and subsequent monitoring are critical steps. Drug screens can help exclude or confirm specific drugs, thereby guiding appropriate therapeutic interventions and improving diagnostic certainty.
3. Monitoring After Overdose
Monitoring patients after an overdose is essential to assess the effectiveness of treatment and detect any delayed complications. Continuous observation and repeated testing can help track the patient’s recovery and ensure that the bioavailability of the toxin is minimized. This includes considering the administration of antidotes and other measures to enhance toxin elimination. In cases of opioid overdose, for instance, follow-up questions assessing acute treatment and symptoms can provide reliable information about the incident and guide further management.
4. Risk Assessment
Risk assessment involves evaluating the potential for adverse outcomes based on the type and amount of substance ingested, the patient’s medical history, and presenting symptoms. This assessment helps determine the level of care required, such as admission to an intensive care unit or general ward. Comprehensive drug screening can aid in this process by providing detailed information about the substances involved, thereby improving the accuracy of risk stratification and guiding appropriate resource allocation.
5. Unconscious Patients
In unconscious patients, immediate testing is vital to identify the cause of altered mental status and initiate appropriate treatment. These patients may present with non-specific symptoms such as shallow breathing and pinpoint pupils, which can suggest opioid intoxication. Rapid administration of naloxone and supportive measures like intubation and mechanical ventilation may be necessary. Drug screens can help confirm the diagnosis and guide further management, ensuring that critical interventions are not delayed.
6. Emergency Situations
In emergency situations, timely testing is crucial to guide immediate therapeutic decisions and improve patient outcomes. The initial management of suspected overdose cases often relies on rapid identification of the substance involved through clinical assessment and laboratory tests. This approach helps stabilize the patient and determine the need for specific antidotes or other interventions to enhance toxin elimination. Drug screens can significantly impact diagnostic certainty and management plans, although their utility may vary depending on the clinical context.
7. Children with Suspected Overdose
In children with suspected overdose, testing is essential to identify the ingested substance and guide appropriate treatment. Pediatric patients may present with non-specific symptoms, making it challenging to diagnose the cause of toxicity. Comprehensive drug screening can provide valuable information, aiding in the accurate diagnosis and management of these cases. Additionally, the use of specific markers like procalcitonin can help guide antibiotic therapy in cases of suspected bacterial infection, reducing unnecessary antibiotic exposure and improving outcomes.
8. Monitoring Liver Function
Monitoring liver function is crucial in patients with suspected overdose, especially when hepatotoxic substances like acetaminophen are involved. Regular assessment of liver enzymes and other markers can help detect early signs of liver injury and guide appropriate interventions. This monitoring is essential for preventing severe complications and ensuring timely treatment, such as the administration of N-acetylcysteine in acetaminophen overdose cases. Comprehensive drug screening can also aid in identifying substances that may impact liver function, thereby guiding further management.
How the Test Works
Procedure
To determine the acetaminophen concentration in a blood sample, a small volume of blood is first collected, typically through a finger-prick or venipuncture. The sample is then processed using various analytical techniques. One method involves using a disposable electrochemical test strip coated with single-walled carbon nanotubes and Nafion, which stabilizes the electrode potential and allows for selective detection of acetaminophen in the blood. The test strip can detect acetaminophen in small 40 µL samples with a detection limit of 0.8 µM and a wide linear range from 1 µM to 2 mM, making it suitable for clinical use. Another method employs aryl acylamidase to convert acetaminophen to 4-aminophenol, which is then measured amperometrically. These methods provide rapid and accurate results, essential for point-of-care testing.
Interpretation of Results
The interpretation of acetaminophen test results is crucial for determining whether the levels are within a safe range or indicate potential toxicity. Therapeutic levels of acetaminophen typically range from 10 to 30 mg/L in the blood. Levels above this range can be toxic, with concentrations exceeding 150 mg/L at 4 hours post-ingestion considered potentially harmful and indicative of overdose. Toxic levels can lead to severe liver damage and require immediate medical intervention. The rapid and accurate determination of acetaminophen levels using these advanced methods ensures timely diagnosis and treatment, reducing the risk of acute liver failure and other complications.
Why Is the Acetaminophen Level Test Needed?
Risks of Acetaminophen Overdose
Acetaminophen overdose is a significant public health concern due to its widespread use and potential for severe toxicity. Overdosing on acetaminophen can lead to dose-dependent hepatotoxicity, which is a major cause of acute liver failure and can be fatal if not treated promptly. The risk is exacerbated by the availability of acetaminophen in various over-the-counter products, leading to unintentional overdoses when multiple products are consumed simultaneously. Despite the availability of the antidote N-acetylcysteine, many cases of hepatotoxicity and deaths still occur, highlighting the need for better prevention and treatment strategies.
Symptoms of Overdose
Symptoms of acetaminophen overdose can be insidious, often starting with nonspecific signs such as nausea, vomiting, and abdominal pain. As the condition progresses, more severe symptoms such as jaundice, confusion, and hepatic encephalopathy may develop, indicating significant liver damage. The initial phase of overdose might be misleadingly mild, which can delay diagnosis and treatment. Therefore, recognizing these early symptoms is crucial for timely intervention. The Rumack-Matthew nomogram is a useful tool for assessing the risk of hepatotoxicity based on plasma acetaminophen levels, guiding the need for treatment with N-acetylcysteine.
Importance of Early Detection
Early detection of acetaminophen overdose is critical to prevent severe liver damage and improve patient outcomes. Prompt administration of N-acetylcysteine within the first 8-10 hours post-ingestion can significantly reduce the risk of hepatotoxicity and improve survival rates. The use of the Rumack-Matthew nomogram helps in early risk assessment and decision-making regarding the need for antidotal therapy. Additionally, public awareness and education about the risks of acetaminophen overdose and the importance of early medical intervention can further aid in reducing the incidence of severe outcomes.
How is the Acetaminophen Level Test Conducted?
The Acetaminophen Level Test is conducted through a series of well-defined steps to ensure accurate and reliable results. Preparation for the test typically involves the patient refraining from taking any acetaminophen-containing medications for a specified period before the test to avoid skewed results. During the testing process, a blood sample is collected from the patient, usually from a vein in the arm, using a sterile needle and syringe. The collected blood sample is then processed using various analytical methods. One such method involves the use of liquid chromatography-tandem mass spectrometry (LC-MS/MS), which provides high sensitivity and precision in quantifying acetaminophen and its metabolites in the serum. Another method employs a high-pressure liquid-chromatographic technique that uses solvent extraction and adsorption chromatography on silica to achieve excellent sensitivity and accuracy. Additionally, rapid immunoassays using membrane and gold particle-based techniques have been developed for emergency situations, offering quick results with high accuracy. Understanding the test results involves comparing the measured acetaminophen levels against established reference ranges to determine if the levels are within the therapeutic range or indicative of an overdose, which is critical for timely medical intervention.
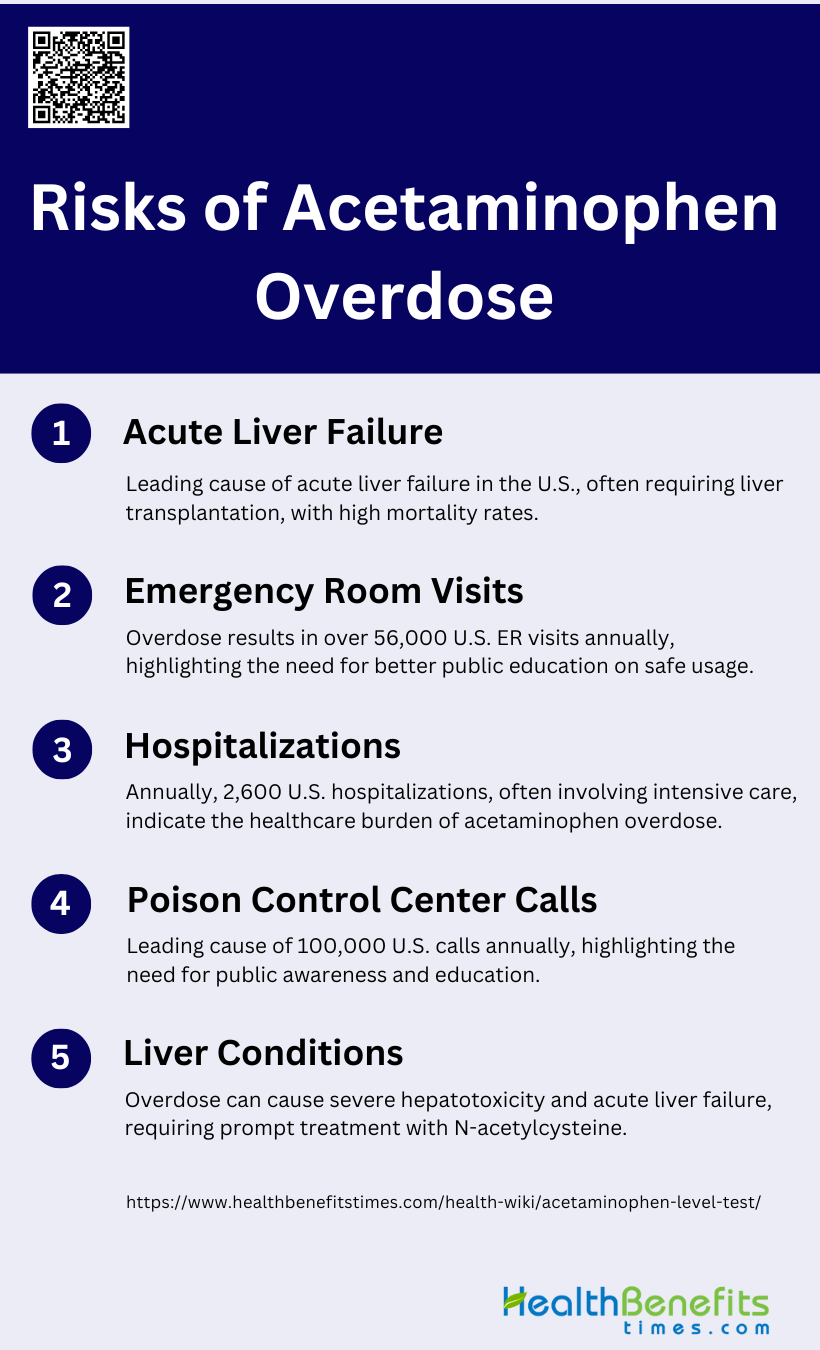
Risks of Acetaminophen Overdose
Acetaminophen, a widely used over-the-counter pain reliever and fever reducer, can pose serious health risks when taken in excessive amounts. While generally safe when used as directed, an overdose of acetaminophen can lead to severe consequences, including potentially life-threatening conditions. The following are the key risks associated with acetaminophen overdose:
1. Acute Liver Failure
Acetaminophen overdose is the leading cause of acute liver failure (ALF) in the United States and other Western countries. It accounts for nearly 50% of all ALF cases in the U.S., with a mortality rate of approximately 30%. The incidence of acetaminophen-related ALF has been increasing, with unintentional overdoses, alcohol abuse, and underlying liver disease being significant risk factors. The median dose ingested in ALF cases is around 24 grams, and the outcomes can be severe, including death or the need for liver transplantation. Despite its widespread use and perceived safety, the risk of ALF from acetaminophen remains a critical public health issue.
2. Emergency Room Visits
Acetaminophen overdose leads to a significant number of emergency room visits annually. In the United States alone, it accounts for more than 56,000 emergency room visits each year. These visits are often due to both intentional and unintentional overdoses, with patients presenting with symptoms ranging from mild gastrointestinal distress to severe hepatotoxicity and encephalopathy. The high volume of emergency room visits underscores the need for better public education on the safe use of acetaminophen and the importance of early intervention in overdose cases.
3. Hospitalizations
Annually, acetaminophen overdose results in approximately 2,600 hospitalizations in the United States. Hospitalized patients often require intensive care, including the administration of N-acetylcysteine (NAC) to mitigate liver damage and, in severe cases, liver transplantation. The risk factors for hospitalization include unintentional overdoses, alcohol abuse, and pre-existing liver conditions, which can exacerbate the hepatotoxic effects of acetaminophen. Despite the availability of effective treatments, the burden on healthcare systems remains substantial due to the high number of hospitalizations.
4. Poison Control Center Calls
Acetaminophen overdose is the leading cause of calls to Poison Control Centers in the United States, with more than 100,000 calls reported annually. These calls often involve cases of both intentional and unintentional overdoses, highlighting the widespread nature of the issue. Poison Control Centers play a crucial role in providing immediate guidance on the management of acetaminophen toxicity, including the use of activated charcoal and NAC. The high volume of calls indicates a need for increased public awareness and education on the proper use of acetaminophen to prevent overdoses.
5. Liver Conditions
Acetaminophen overdose can lead to severe liver conditions, including hepatotoxicity and acute liver failure. The risk of developing hepatotoxicity is higher in individuals with underlying liver disease, alcohol abuse, or those who have taken unintentional overdoses. Hepatotoxicity can manifest as elevated liver enzymes, jaundice, and coagulopathy, and in severe cases, it can progress to liver failure requiring transplantation. The management of acetaminophen-induced liver conditions involves the prompt administration of NAC and supportive care, but the outcomes can be poor, especially in patients with advanced liver disease or delayed presentation.
What happens if Levels are Too High
Treatment Options
When acetaminophen levels are too high, immediate treatment is crucial to prevent liver damage. Activated charcoal can be administered to reduce the absorption of acetaminophen if the patient presents within a few hours of ingestion. N-acetylcysteine (NAC) is the standard treatment for preventing hepatotoxicity and is most effective when given within 8 hours of overdose. NAC works by replenishing glutathione stores, detoxifying the harmful metabolites of acetaminophen. In cases of massive overdose, extended or alternative NAC regimens may be necessary to manage persistently high acetaminophen levels and prevent liver injury.
Medical Follow-up
Ongoing monitoring and medical care are essential in cases of acetaminophen overdose to ensure patient safety and recovery. Regular assessment of liver function tests, acetaminophen plasma levels, and clinical symptoms is necessary to guide treatment decisions. Patients may require extended NAC therapy if acetaminophen levels remain elevated or if there are signs of hepatic injury. Additionally, consultation with a clinical toxicologist can provide specialized guidance for complex cases. Continuous monitoring helps in early detection of complications such as hepatic failure, allowing timely interventions to improve patient outcomes.
Preventing Acetaminophen Overdose
Acetaminophen overdose is a serious concern, but it can be prevented through proper education and careful use of medications. By understanding the risks and following recommended guidelines, individuals can safely use acetaminophen while minimizing the potential for harm. Here are essential steps to prevent acetaminophen overdose:
1. Follow dosage instructions carefully
Following dosage instructions for acetaminophen is crucial to prevent overdose and subsequent liver damage. Acetaminophen is a widely used analgesic and antipyretic, but its safety is dose-dependent. Overdosing can lead to severe hepatotoxicity and acute liver failure, which are significant health concerns in many countries. The Rumack-Matthew nomogram is a useful tool for assessing the risk of toxicity in cases of acute overdose and guiding treatment with N-acetylcysteine (NAC). Adhering to prescribed dosages and understanding the maximum allowable daily intake can significantly reduce the risk of accidental overdose and its severe consequences.
2. Avoid multiple acetaminophen-containing products
Simultaneous ingestion of multiple acetaminophen-containing products is a common cause of overdose. Many over-the-counter and prescription medications contain acetaminophen, and unintentional overdoses often occur when individuals are unaware of this overlap. This can lead to excessive cumulative doses, increasing the risk of hepatotoxicity. It is essential to read labels carefully and consult healthcare providers to avoid combining products that contain acetaminophen. Education on the potential risks of using multiple acetaminophen-containing medications can help prevent accidental overdoses and the associated health risks.
3. Use proper measuring devices
Using proper measuring devices is vital when administering liquid acetaminophen, especially in pediatric cases. Inaccurate dosing can result from using household spoons, which vary in size and can lead to either underdosing or overdosing. Proper dosing devices, such as oral syringes or dosing cups, ensure accurate measurement and administration of the correct dose. This practice is particularly important for children, who are more susceptible to the toxic effects of acetaminophen due to their smaller body size. Ensuring accurate dosing helps maintain therapeutic efficacy while minimizing the risk of overdose.
4. Be cautious with alcohol
Alcohol consumption can exacerbate the hepatotoxic effects of acetaminophen. Chronic alcohol use induces cytochrome P450 enzymes, increasing the production of toxic metabolites from acetaminophen and thereby heightening the risk of liver damage. Individuals who consume alcohol regularly should be particularly cautious with acetaminophen use and may need to limit their intake to lower doses. Healthcare providers should advise patients on the risks associated with concurrent alcohol and acetaminophen use to prevent potential liver injury.
5. Store safely
Safe storage of acetaminophen is essential to prevent accidental ingestion, particularly by children. Unsupervised ingestions by children under six years old account for a significant number of emergency department visits for acetaminophen overdose. Medications should be stored in child-resistant containers and kept out of reach and sight of children. Educating caregivers on the importance of safe storage practices can reduce the incidence of accidental poisonings and ensure that acetaminophen is used safely within the household.
6. Educate caregivers
Educating caregivers about the safe use of acetaminophen is crucial in preventing overdose. Caregivers should be informed about the correct dosages, the importance of using proper measuring devices, and the risks of combining multiple acetaminophen-containing products. They should also be aware of the signs of overdose and the need for prompt medical attention if an overdose is suspected. Providing clear and accessible information can empower caregivers to use acetaminophen safely and effectively, reducing the risk of accidental overdoses.
7. Read labels carefully
Reading labels carefully is a fundamental step in preventing acetaminophen overdose. Labels provide critical information about the active ingredients, dosage instructions, and potential interactions with other medications. Consumers should be vigilant in checking labels to avoid exceeding the recommended dose and to ensure they are not inadvertently taking multiple products containing acetaminophen. Understanding and following label instructions can help prevent accidental overdoses and ensure the safe use of acetaminophen.
FAQs
1. What are the symptoms that might prompt an Acetaminophen Level Test?
Symptoms like nausea, vomiting, stomach pain, or confusion after consuming acetaminophen may prompt a healthcare provider to order the test to assess potential toxicity.
2. How long after taking acetaminophen should I wait before getting tested?
The test is usually most accurate if conducted at least 4 hours after ingestion, as this is when the levels in the blood are most reflective of toxicity risk. However, testing may still be done earlier or later, depending on the specific situation.
3. Can I have a normal Acetaminophen Level Test result but still experience liver damage later?
Yes, in rare cases, delayed liver damage can occur even with initially normal test results, especially in cases of extended-release acetaminophen formulations or if other liver-damaging factors are present.
4. Do I need to fast before an Acetaminophen Level Test?
Generally, fasting is not required for this test. However, follow your healthcare provider’s instructions about preparation.
5. Can other medications or substances affect my Acetaminophen Level Test?
Yes, certain medications, alcohol consumption, and pre-existing liver conditions can impact both the test results and your body’s response to acetaminophen. Make sure to inform your doctor of any other substances you’ve taken.
6. How is the test different for children?
The test may be ordered for children if they are suspected to have ingested acetaminophen. Pediatric guidelines for blood acetaminophen levels and treatment thresholds may differ from adults due to differences in metabolism.
7. Can I monitor acetaminophen levels at home?
Currently, there are no home test kits for acetaminophen levels. Testing must be conducted in a medical setting with laboratory analysis.
8. What should I do if I accidentally take more than the recommended dose of acetaminophen but have no symptoms?
Even without symptoms, you should seek medical advice. A doctor may recommend an Acetaminophen Level Test to determine if treatment is necessary, as symptoms of overdose can be delayed.
9. Can I refuse the Acetaminophen Level Test if I think I’ve taken too much acetaminophen?
While you have the right to refuse any test, this test is crucial in determining potential liver damage and guiding treatment. Refusing it could delay critical medical intervention.
10. What are the long-term effects if I don’t seek treatment after a high acetaminophen level is detected?
Failure to seek treatment for high acetaminophen levels can lead to severe liver damage, liver failure, and even death. Prompt treatment, such as with N-acetylcysteine, is crucial in preventing these outcomes.