Abdominal distension is a condition characterized by a noticeable increase in the size or volume of the abdomen, often accompanied by a feeling of fullness, pressure, or discomfort. It can be caused by various factors, including gas accumulation, fluid retention, or the presence of masses within the abdominal cavity. This symptom is commonly associated with digestive issues, such as constipation, irritable bowel syndrome, or food intolerances, but it can also be a sign of more serious underlying conditions like liver disease, ovarian cancer, or intestinal obstruction. Abdominal distension may be accompanied by other symptoms such as bloating, nausea, and changes in bowel movements. In some cases, it can be a temporary and benign condition, while in others; it may require medical attention to determine the root cause and appropriate treatment.
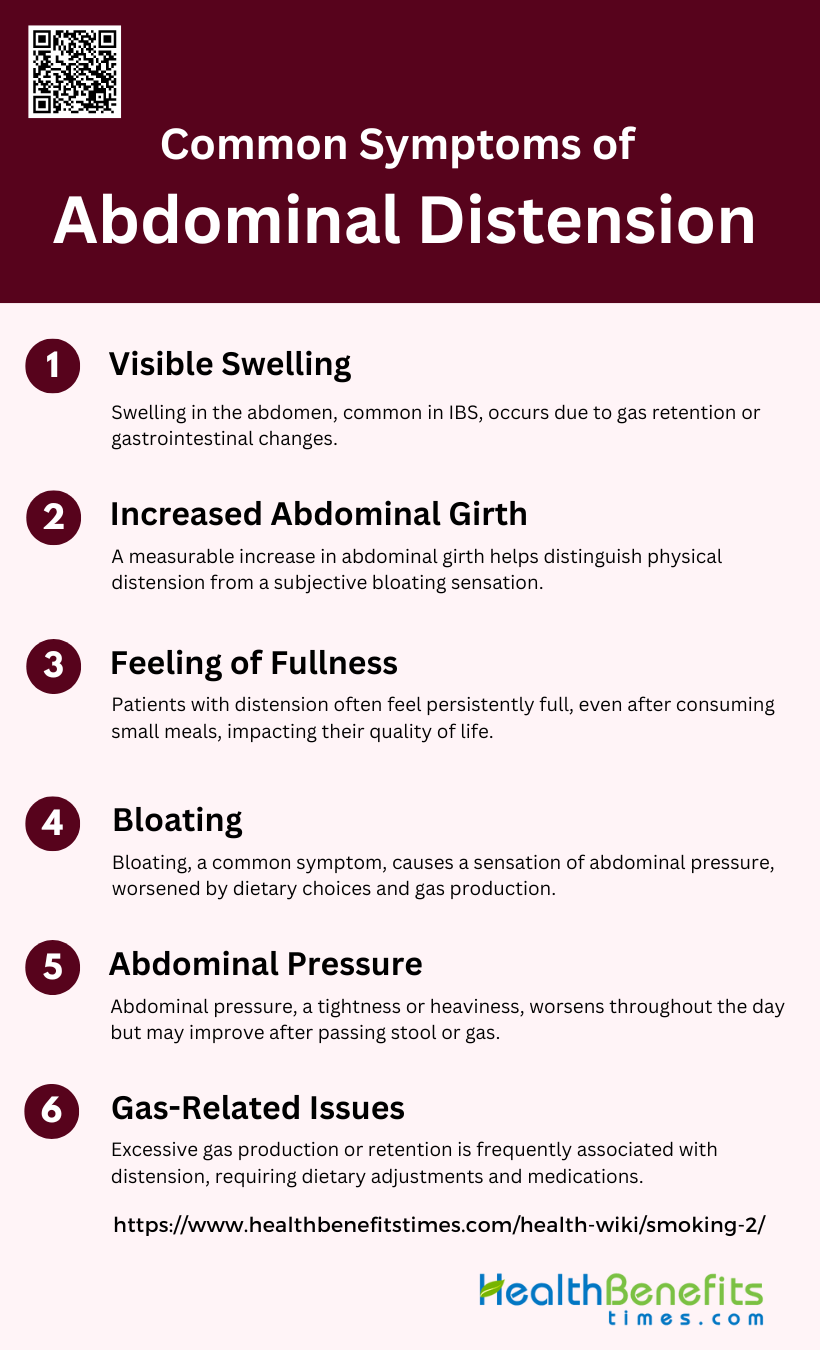
Common symptoms of Abdominal Distension
Abdominal distension can manifest with various symptoms that may vary in intensity and duration. Recognizing these signs is crucial for early detection and proper management of the condition. Some of the most common symptoms associated with abdominal distension include:
1. Visible Swelling
Visible swelling in the abdomen is a common symptom of abdominal distension, often observed in conditions like irritable bowel syndrome (IBS). This symptom is characterized by a noticeable increase in abdominal girth, which can be objectively measured using tools like a metric tape measure or abdominal inductance plethysmography. The swelling is not always correlated with the sensation of bloating, indicating that different pathophysiological mechanisms may be at play. For instance, while some patients may experience visible swelling due to gas retention or changes in gastrointestinal motility, others may not show any visible signs despite feeling bloated.
2. Increased Abdominal Girth
Increased abdominal girth is a measurable sign of abdominal distension, often used to objectively confirm the presence of this symptom. Studies have shown that patients with IBS frequently exhibit an increase in abdominal girth, which can be quantified using various methods such as tape measurements or computed tomography. This increase in girth is often more pronounced in patients with constipation-predominant IBS compared to those with diarrhea-predominant IBS. The measurement of abdominal girth provides a reliable way to distinguish between subjective sensations of bloating and actual physical distension.
3. Feeling of Fullness
The feeling of fullness is a subjective sensation often reported by patients experiencing abdominal distension. This symptom is commonly associated with functional gastrointestinal disorders like IBS and functional dyspepsia. The sensation of fullness can be due to various factors, including delayed gastric emptying, gas retention, and visceral hypersensitivity. Patients often describe this feeling as a persistent sense of having eaten too much, even when they have not consumed a large meal. This symptom can significantly impact the quality of life, making it a key focus in the management of abdominal distension.
4. Bloating
Bloating is one of the most common and bothersome symptoms associated with abdominal distension. It is often described as a subjective sensation of increased pressure within the abdomen, which may or may not be accompanied by visible swelling. Bloating is frequently reported in patients with functional gastrointestinal disorders, such as IBS, and can be exacerbated by factors like dietary choices, gas production, and visceral hypersensitivity. Despite its prevalence, the exact pathophysiology of bloating remains unclear, making it a challenging symptom to manage effectively.
5. Abdominal Pressure
Abdominal pressure is another common symptom of abdominal distension, often described as a feeling of tightness or heaviness in the abdomen. This symptom can result from various underlying mechanisms, including gas retention, fluid accumulation, and altered gastrointestinal motility. Patients with IBS and other functional gastrointestinal disorders frequently report experiencing abdominal pressure, which can worsen throughout the day and improve with the passage of stool or gas. Effective management of this symptom often involves addressing the underlying causes, such as dietary modifications and pharmacological interventions.
6. Gas-Related Issues
Gas-related issues, such as excessive gas production and retention, are frequently implicated in the development of abdominal distension and bloating. Studies have shown that patients with IBS often experience increased gas production, which can contribute to symptoms like bloating and abdominal discomfort. However, the relationship between gas production and visible abdominal distension is not always straightforward, as some patients may produce significant amounts of gas without experiencing noticeable swelling. Effective management of gas-related issues often involves dietary changes, probiotics, and medications aimed at reducing gas production and improving gastrointestinal motility.
Causes of abdominal distension
Abdominal distension can result from multiple factors, including dietary choices, medical conditions, and lifestyle habits. Identifying these causes is essential for managing symptoms effectively. Below is list of primary causes of abdominal distension:
A. Dietary Causes
Certain foods and beverages are known to cause gas and bloating, leading to abdominal distension. Foods high in poorly absorbed fermentable carbohydrates, such as beans and certain fruits, can produce gas and bloating in individuals with irritable bowel syndrome (IBS) due to colonic hypersensitivity to distension rather than excessive gas production. Additionally, carbonated drinks can introduce excess air into the digestive system, contributing to bloating and distension. Dietary modifications, such as a low-FODMAP diet, have been shown to alleviate symptoms in many patients by reducing the intake of these gas-producing foods.
B. Medical Conditions
1. Irritable Bowel Syndrome (IBS)
IBS is a common cause of abdominal distension, often linked to visceral hypersensitivity and abnormal gas production. Patients with IBS frequently report bloating and distension, which can be exacerbated by certain foods and stress.
2. Celiac Disease
Celiac disease can cause abdominal distension due to malabsorption and inflammation in the small intestine. Serologic testing and a small bowel biopsy are recommended for diagnosis, and a gluten-free diet is essential for management.
3. Lactose Intolerance
Lactose intolerance leads to bloating and distension due to the inability to digest lactose, resulting in increased gas production and visceral hypersensitivity. Symptoms can be managed by avoiding lactose-containing foods or using lactase supplements.
4. Ascites
Ascites, the accumulation of fluid in the abdominal cavity, can cause significant abdominal distension. It is often associated with liver disease, heart failure, or malignancies and requires medical evaluation and management.
C. Lifestyle Factors
1. Sedentary Lifestyle
A sedentary lifestyle can contribute to abdominal distension by slowing down intestinal transit and reducing the efficiency of gas evacuation. Regular physical activity can help improve bowel movements and reduce bloating.
2. Stress and Anxiety
Stress and anxiety can exacerbate symptoms of bloating and distension by affecting gut motility and increasing visceral sensitivity. Psychological therapies, such as cognitive behavioral therapy and hypnotherapy, have been shown to be effective in managing these symptoms.
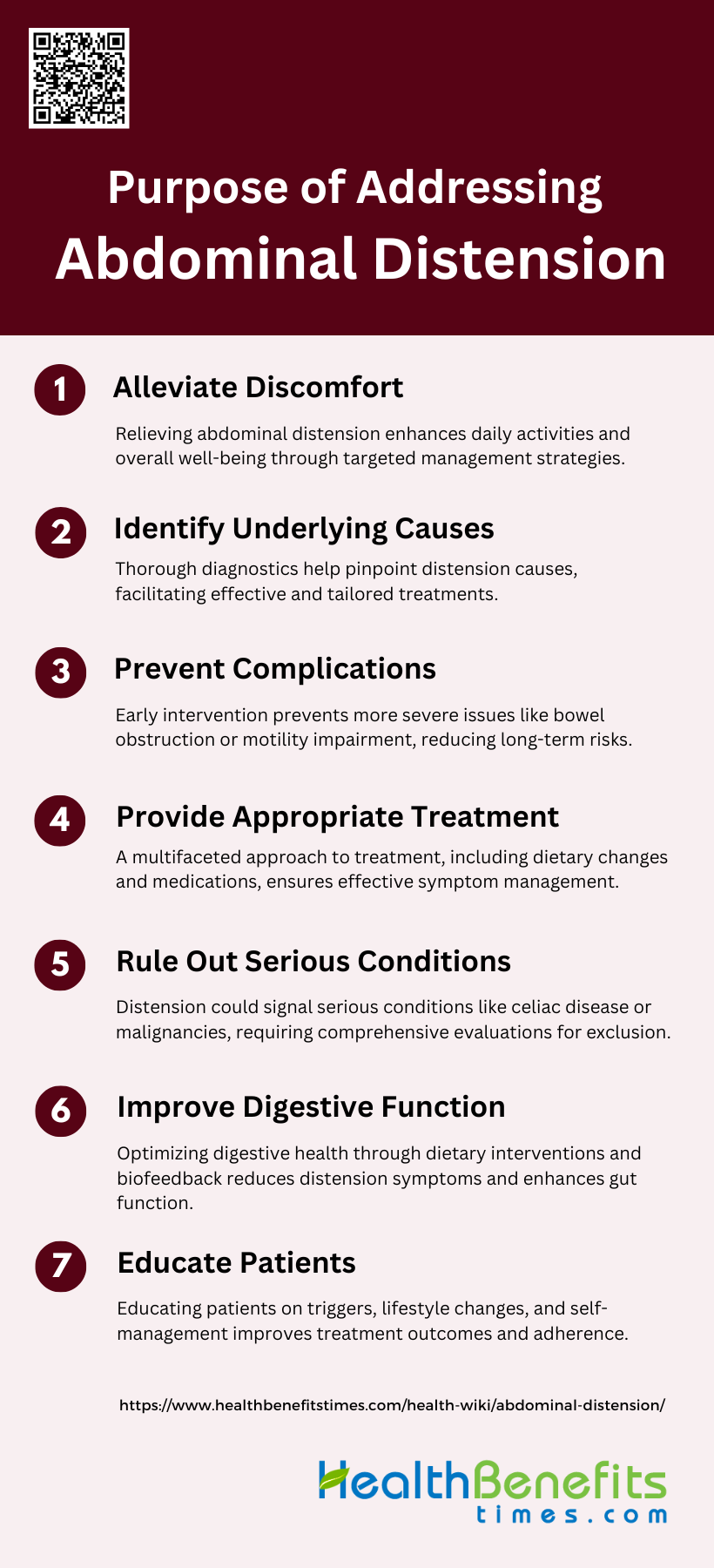
Purpose of Addressing Abdominal Distension
Addressing abdominal distension is essential for enhancing patient comfort and overall health. By focusing on the underlying causes, effective management strategies can be developed to alleviate symptoms and prevent complications. Below is a list of the key purposes for addressing abdominal distension:
1. Alleviate Discomfort and Improve Quality of Life
Addressing abdominal distension is crucial for alleviating discomfort and improving the quality of life for patients. Abdominal bloating and distension are common gastrointestinal symptoms that can significantly impact daily activities and overall well-being. These symptoms often lead to feelings of trapped gas, abdominal pressure, and fullness, which can be distressing and debilitating. Effective management strategies, such as dietary changes, probiotics, and biofeedback, have been shown to reduce symptoms and enhance patients’ quality of life by minimizing discomfort and improving digestive function. Therefore, addressing these symptoms is essential for enhancing the overall quality of life for affected individuals.
2. Identify Underlying Causes
Identifying the underlying causes of abdominal distension is a critical step in its management. Abdominal bloating and distension can result from various factors, including food intolerances, small intestinal bacterial overgrowth, constipation, and visceral hypersensitivity. A thorough diagnostic approach, which may include dietary assessments, breath tests, and imaging studies, helps pinpoint the specific etiology of the symptoms. By understanding the root causes, healthcare providers can tailor treatment plans to address the specific issues, leading to more effective and targeted interventions.
3. Prevent Complications
Preventing complications associated with abdominal distension is another important goal. Chronic distension can lead to more severe gastrointestinal issues, such as bowel obstruction or impaired motility, if left untreated. Early intervention and appropriate management strategies, such as biofeedback and dietary modifications, can help prevent these complications by addressing the symptoms before they escalate. Additionally, preventing complications can reduce the need for more invasive treatments and improve long-term health outcomes for patients.
4. Provide Appropriate Treatment
Providing appropriate treatment for abdominal distension involves a multifaceted approach tailored to the individual patient’s needs. Treatment options may include dietary changes, probiotics, antibiotics, prokinetic agents, antispasmodics, neuromodulators, and biofeedback. Personalized treatment plans that consider the patient’s specific symptoms and underlying causes are essential for effective management. For instance, a low-FODMAP diet has been shown to significantly reduce symptoms in patients with bloating and distension. By offering a range of therapeutic options, healthcare providers can ensure that patients receive the most suitable and effective treatments.
5. Rule Out Serious Conditions
Ruling out serious conditions is a vital aspect of addressing abdominal distension. Symptoms of bloating and distension can sometimes be indicative of more severe underlying conditions, such as celiac disease, gastrointestinal malignancies, or inflammatory bowel disease. Comprehensive diagnostic evaluations, including serologic testing, imaging, and endoscopy, are necessary to exclude these serious conditions. Early detection and exclusion of serious diseases ensure that patients receive timely and appropriate care, preventing potential complications and improving prognosis.
6. Improve Digestive Function
Improving digestive function is a key objective in managing abdominal distension. Effective treatment strategies can enhance gastrointestinal motility, reduce gas production, and improve overall digestive health. Techniques such as biofeedback, which helps patients control abdominal muscle activity, and dietary interventions, like reducing poorly absorbed fermentable carbohydrates, have been shown to improve digestive function and reduce symptoms. By optimizing digestive processes, patients can experience relief from distension and enjoy better gastrointestinal health.
7. Educate Patients
Educating patients about abdominal distension and its management is essential for successful treatment outcomes. Patient education involves informing individuals about potential triggers, dietary modifications, and lifestyle changes that can alleviate symptoms. Providing clear guidance on self-management techniques, such as abdominal massage and biofeedback, empowers patients to take an active role in their care. Education also helps set realistic expectations and fosters better adherence to treatment plans, ultimately leading to improved symptom control and quality of life.
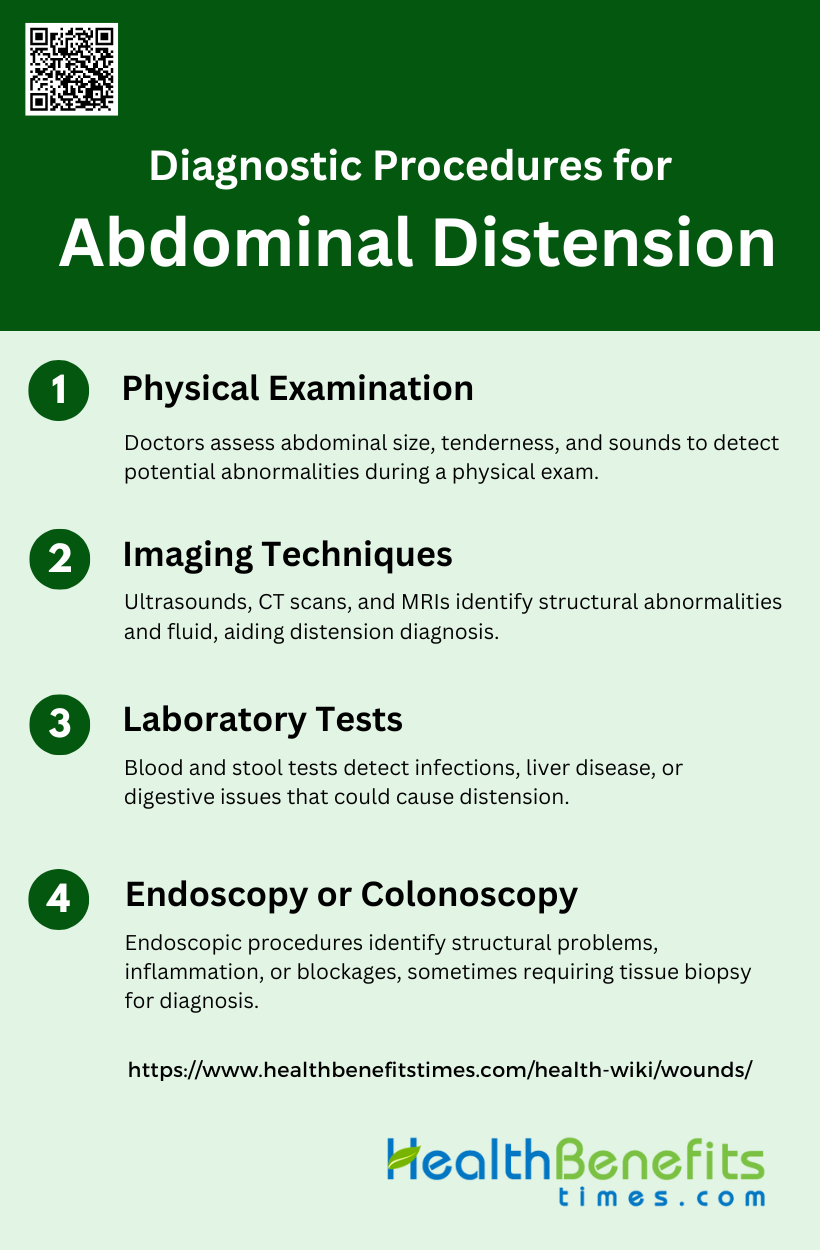
Diagnostic Procedures for Abdominal Distension
Diagnosing abdominal distension involves several procedures designed to identify its underlying causes. These diagnostic methods range from physical examinations to advanced imaging techniques and laboratory tests. Below is a list of the key diagnostic procedures used to evaluate abdominal distension:
1. Physical Examination
During a physical examination for abdominal distension, doctors carefully assess the size, shape, and symmetry of the abdomen. They palpate the area to check for tenderness, masses, or fluid accumulation. The location of any pain or discomfort is noted, as it can provide clues about the affected organs. Doctors also listen for abnormal bowel sounds and percuss the abdomen to detect any unusual dullness or tympany , which can indicate the presence of fluid or gas.
2. Imaging Techniques
Imaging plays a crucial role in diagnosing the cause of abdominal distension. Ultrasound is often the first-line imaging tool due to its accessibility and ability to visualize soft tissues and fluid collections. CT scans provide detailed cross-sectional images of the abdomen, helping to identify tumors, inflammation, or obstructions. MRI offers superior soft tissue contrast and is particularly useful for evaluating complex abdominal conditions. These imaging modalities can reveal structural abnormalities, organ enlargement, or the presence of ascites.
3. Laboratory Tests
Blood tests are essential in the diagnostic workup of abdominal distension. They can help identify infections, liver disease, or other systemic conditions that may contribute to the distension. Common tests include complete blood count, liver function tests, and markers of inflammation. Stool tests may be performed to detect digestive issues, parasites, or occult blood. These laboratory investigations provide valuable information about the patient’s overall health status and can guide further diagnostic procedures or treatment decisions.
4. Endoscopy or Colonoscopy
In cases where imaging and laboratory tests are inconclusive, endoscopic procedures may be necessary. Upper endoscopy allows visualization of the esophagus, stomach, and upper small intestine, while colonoscopy examines the large intestine. These procedures can identify structural abnormalities, inflammation, tumors, or blockages in the digestive tract that may be causing abdominal distension. Endoscopy and colonoscopy also provide the opportunity for tissue biopsy if needed, which can be crucial for definitive diagnosis.
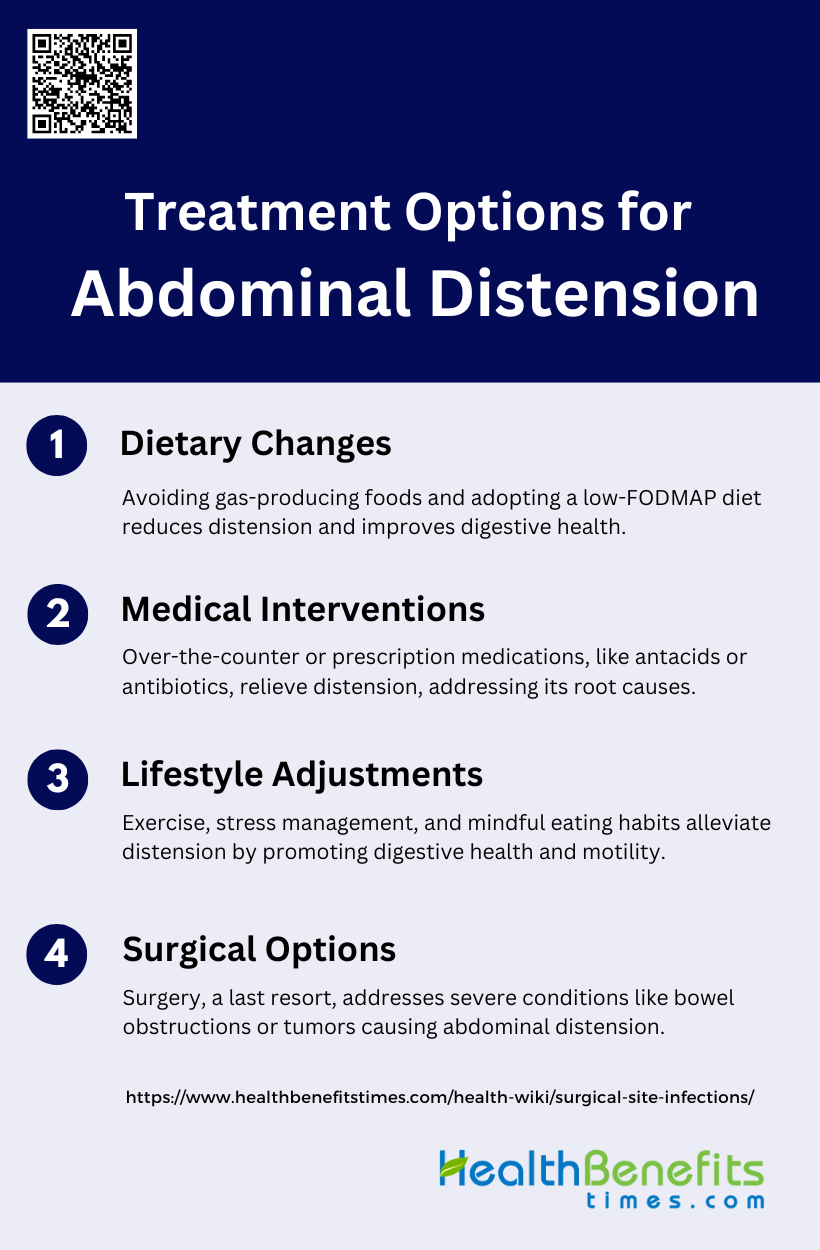
Treatment Options for Abdominal Distension
Managing abdominal distension requires a multifaceted approach that includes dietary, medical, and lifestyle interventions. These strategies are designed to alleviate symptoms and address the root causes of the condition. Below is a list of Treatment Options for Abdominal Distension:
1. Dietary Changes
Modifying one’s diet is often the first line of treatment for abdominal distension. Avoiding gas-producing foods such as beans, lentils, carbonated beverages, and certain vegetables can help reduce bloating. Incorporating fiber-rich foods gradually into the diet can improve bowel function and reduce constipation-related distension. However, it’s important to increase fiber intake slowly to avoid exacerbating symptoms. Some individuals may benefit from a low FODMAP diet, which limits certain types of carbohydrates that can cause digestive issues. Staying hydrated and eating smaller, more frequent meals can also help manage abdominal distension.
2. Medical Interventions
Over-the-counter medications can provide relief for mild to moderate abdominal distension. Antacids may help reduce gas and bloating, while laxatives can alleviate constipation-related distension. For more severe or persistent cases, prescription medications may be necessary to address underlying conditions such as irritable bowel syndrome or inflammatory bowel disease. These might include antispasmodics, prokinetics, or specific medications targeting the root cause of the distension. In some cases, antibiotics may be prescribed if bacterial overgrowth is suspected. It’s crucial to consult a healthcare provider for proper diagnosis and treatment, as self-medication can sometimes worsen symptoms.
3. Lifestyle Adjustments
Making certain lifestyle changes can significantly improve abdominal distension. Regular exercise, particularly aerobic activities, has been shown to reduce abdominal distension and abdominal fat. Engaging in physical activity helps stimulate bowel movements and can alleviate constipation. Stress management techniques such as meditation, yoga, or deep breathing exercises can also be beneficial, as stress often exacerbates digestive symptoms. Maintaining a regular sleep schedule, avoiding late-night eating, and practicing mindful eating can further support digestive health. Additionally, quitting smoking and limiting alcohol consumption may help reduce abdominal distension in some individuals.
4. Surgical Options
Surgery is typically considered a last resort for treating abdominal distension when other treatments have failed or when there’s an underlying condition requiring surgical intervention. Surgery might be necessary in cases of severe bowel obstruction, tumors, or certain structural abnormalities. The type of surgical procedure depends on the specific cause of the distension. For instance, laparoscopic surgery may be used to remove tumors or repair hernias causing distension. In some cases, more extensive procedures such as bowel resection might be required. It’s important to note that surgery carries risks and is only recommended when the benefits outweigh the potential complications.
Preventive measures for Abdominal Distension
Preventing abdominal distension involves implementing various strategies that focus on diet, lifestyle, and overall digestive health. These measures aim to reduce the risk of bloating and discomfort by addressing potential triggers. Below is a list of key preventive measures for abdominal distension.
1. Dietary Modifications
Dietary modifications play a crucial role in managing abdominal distension. A low FODMAP diet, which restricts fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, has been shown to significantly reduce symptoms of bloating and distension, particularly in patients with irritable bowel syndrome (IBS). This diet works by minimizing the intake of poorly absorbed carbohydrates that ferment in the gut, thereby reducing gas production and abdominal discomfort. Additionally, identifying and eliminating specific food intolerances through dietary history and breath testing can help tailor dietary interventions to individual needs, further alleviating symptoms.
2. Modify Eating Habits
Modifying eating habits can also help prevent abdominal distension. Eating smaller, more frequent meals rather than large meals can reduce the burden on the digestive system and minimize bloating. Chewing food thoroughly and eating slowly can prevent the ingestion of excess air, which contributes to bloating and distension. Additionally, avoiding carbonated beverages and chewing gum can further reduce the amount of swallowed air. These simple changes in eating habits can significantly improve symptoms and enhance overall digestive comfort.
3. Lifestyle Changes
Lifestyle changes, including regular physical activity and stress management, are essential in preventing abdominal distension. Exercise promotes regular bowel movements and can help alleviate constipation, a common cause of bloating and distension. Stress management techniques such as yoga, meditation, and deep breathing exercises can reduce stress-related gastrointestinal symptoms by modulating the gut-brain axis. Additionally, abdominal massage techniques, such as the “I LOV U” method, have been shown to improve constipation and reduce abdominal circumference in elderly patients, highlighting the importance of incorporating lifestyle modifications into the management plan.
4. Digestive Support
Digestive support through the use of probiotics, enzymes, and other supplements can be beneficial in managing abdominal distension. Probiotics can help restore a healthy balance of gut microbiota, which is often disrupted in conditions like IBS, leading to reduced bloating and gas production. Enzyme supplements, such as lactase for lactose intolerance, can aid in the digestion of specific carbohydrates that may cause bloating. Additionally, biofeedback therapy has been shown to correct abnormal abdominal muscle activity and reduce distension in patients with functional gut disorders, providing another avenue for digestive support.
5. Weight Management
Maintaining a healthy weight is important in preventing abdominal distension. Excess body weight, particularly around the abdomen, can increase intra-abdominal pressure and exacerbate symptoms of bloating and distension. Weight loss through a combination of dietary changes and regular physical activity can help reduce this pressure and improve gastrointestinal function. Additionally, weight management can alleviate other related conditions, such as gastroesophageal reflux disease (GERD), which can contribute to abdominal discomfort and distension.
6. Medical Considerations
Medical considerations are essential in the comprehensive management of abdominal distension. Identifying and treating underlying conditions such as small intestinal bacterial overgrowth (SIBO), celiac disease, and functional gastrointestinal disorders is crucial. Diagnostic strategies may include breath testing, serologic testing, and imaging studies to rule out organic causes of bloating and distension. Treatment options may involve the use of antibiotics, prokinetic agents, and neuromodulators to address specific etiologies. A multidisciplinary approach, including consultation with gastroenterologists and dietitians, can ensure optimal management and improve patient outcomes.
When to See a Doctor for Abdominal Distension
Red Flags for Seeking Medical Attention
Abdominal distension can be a symptom of various underlying conditions, some of which may require immediate medical attention. Persistent pain, significant weight loss, and the presence of blood in the stool are critical red flags that should prompt a visit to a healthcare provider. Chronic and highly distressing pain, as well as symptoms that significantly impact daily life, should not be ignored. Additionally, if abdominal distension is accompanied by other alarming symptoms such as fever, vomiting, or changes in bowel habits, it is essential to seek medical advice promptly. These symptoms could indicate serious conditions like gastrointestinal infections, inflammatory bowel disease, or even malignancies.
How to Prepare for a Doctor’s Visit
Preparing for a doctor’s visit regarding abdominal distension involves several steps to ensure a comprehensive evaluation. Patients should keep a detailed diary of their symptoms, including the frequency, duration, and severity of the distension, as well as any associated symptoms like pain or changes in bowel habits. Documenting dietary habits and any potential food intolerances can also provide valuable insights. It is helpful to note any over-the-counter medications or supplements being taken. Bringing a list of questions and concerns can facilitate a more productive consultation. Additionally, patients should be prepared to discuss their medical history, including any previous gastrointestinal issues or surgeries, as this information can aid in diagnosing the underlying cause of the distension.
FAQs
1. Can abdominal distension be caused by hormonal changes?
Yes, hormonal fluctuations, particularly in women, can contribute to abdominal distension. Conditions like PMS (premenstrual syndrome), pregnancy, or menopause can lead to fluid retention and bloating, causing temporary abdominal distension.
2. How is abdominal distension different from bloating?
Abdominal distension refers to a visible enlargement of the abdomen, which can be measured objectively, while bloating is the subjective feeling of fullness or pressure in the abdomen, even if there’s no physical swelling. They can occur together, but they are distinct symptoms.
3. Can abdominal distension be related to posture or muscle tension?
Yes, poor posture or excessive muscle tension in the abdominal area can contribute to or exacerbate abdominal distension. Engaging the core muscles and maintaining proper posture may help alleviate symptoms in some cases.
4. Is abdominal distension common after surgery?
Post-surgical abdominal distension can occur due to the effects of anesthesia, immobility, or the body’s response to surgical stress. Gas retention and slowed bowel movements are common after abdominal or gastrointestinal surgeries and usually resolve as normal function returns.
5. Can abdominal distension cause breathing difficulties?
Severe abdominal distension may exert pressure on the diaphragm, potentially causing shortness of breath or discomfort while breathing. This symptom warrants medical attention, especially if breathing becomes labored.
6. Is abdominal distension related to food allergies?
Yes, food allergies, particularly to common allergens like wheat, soy, or nuts, can trigger abdominal distension as part of a broader immune response. If you suspect a food allergy is causing distension, seek medical advice for testing and management.
7. Can dehydration cause abdominal distension?
Yes, dehydration can lead to constipation, which can cause abdominal distension. Drinking sufficient water and maintaining hydration can help prevent this type of distension.
8. Are there any home remedies to relieve abdominal distension?
Home remedies such as drinking peppermint tea, applying heat to the abdomen, engaging in gentle exercise, or practicing abdominal massage techniques can provide temporary relief from abdominal distension.
9. Can abdominal distension be a side effect of medication?
Yes, certain medications, including antidepressants, antacids, and some pain relievers, can cause abdominal distension as a side effect. If you notice distension after starting a new medication, consult your doctor.
10. Can abdominal distension affect children, and are the causes the same as in adults?
Children can also experience abdominal distension, though the causes may vary. In children, common causes include food intolerances, constipation, and gastrointestinal infections. It’s important to monitor symptoms in children closely and consult a pediatrician if distension is persistent.