The A1C test, also known as hemoglobin A1C or HbA1c, is a blood test used to diagnose and monitor diabetes. It measures the average blood sugar levels over the past 2-3 months by assessing the percentage of glycated hemoglobin in the blood. This test is particularly useful because it doesn’t require fasting and provides a longer-term view of blood glucose control compared to daily blood sugar measurements. The American Diabetes Association recommends quarterly A1C testing for patients with uncontrolled diabetes to guide clinical decisions regarding changes in patient care. The A1C test is considered a reliable indicator of diabetes risk and is used alongside other tests like fasting plasma glucose and oral glucose tolerance tests to provide a comprehensive assessment of a person’s glycemic status.
Purpose of the A1C Test
Monitoring Diabetes
The A1C test is a crucial tool for monitoring diabetes as it provides an average blood glucose level over the past two to three months. This long-term view is essential for managing diabetes effectively, as it helps in assessing how well the treatment plan is working. Regular monitoring of A1C levels can help in adjusting medications, diet, and exercise plans to maintain blood glucose levels within the target range. Studies have shown that intensive glycemic control, as indicated by lower A1C levels, minimizes the risks of microvascular complications in diabetes. Therefore, the A1C test is indispensable for ongoing diabetes management and for preventing complications.
Diagnosing Diabetes and Prediabetes
The A1C test is also used for diagnosing diabetes and prediabetes. The American Diabetes Association (ADA) recommends an A1C level of 6.5% or higher for diagnosing diabetes, while levels between 5.7% and 6.4% indicate prediabetes. This test is advantageous because it does not require fasting and can be done at any time of the day. However, its sensitivity and specificity can vary. For instance, in obese children and adolescents, an A1C of 6.5% may underestimate the prevalence of diabetes and prediabetes. Despite these limitations, the A1C test remains a practical and widely used diagnostic tool for identifying individuals at risk for diabetes and its complications.
Assessing Risk of Complications
The A1C test is valuable for assessing the risk of diabetes-related complications. Higher A1C levels are associated with an increased risk of both microvascular and macrovascular complications. For example, individuals with elevated A1C levels have a higher probability of developing cardiovascular disease (CVD) and other complications. The test can also be used preoperatively to predict perioperative complications in diabetic patients undergoing surgery. By identifying individuals with high A1C levels, healthcare providers can implement more intensive management strategies to mitigate these risks. Thus, the A1C test serves as a prognostic tool, helping to identify patients who may benefit from more aggressive treatment to prevent complications.
How the A1C Test is Conducted
The A1C test is conducted by measuring the percentage of glycated hemoglobin in the blood, which reflects the average blood glucose levels over the past 8 to 12 weeks. This test is typically performed using a blood sample taken from a vein, and it does not require fasting, making it convenient for patients. The American Diabetes Association recommends that individuals with diabetes have their A1C levels tested at least twice a year if they are meeting treatment goals and more frequently, such as quarterly, if their therapy has changed or they are not meeting glycemic goals. Understanding the results involves interpreting the A1C percentage: an A1C level below 5.7% is considered normal, 5.7% to 6.4% indicates prediabetes, and 6.5% or higher suggests diabetes. It is important to note that certain conditions, such as anemia or hemoglobinopathies, can affect the accuracy of A1C results, and alternative methods may be needed in such cases.
Interpreting A1C Test Results
Normal vs. Abnormal Levels
The A1C test, also known as the hemoglobin A1C or HbA1c test, measures the average blood glucose levels over the past two to three months. According to the International Expert Committee, an A1C level of 6.5% or higher is indicative of diabetes, while levels below this threshold are considered normal. However, the use of A1C alone for diagnosis can lead to false positives and negatives due to various factors such as hemoglobinopathies and other conditions that affect hemoglobin levels. Therefore, while A1C is a valuable tool for diagnosing diabetes, it is essential to consider other diagnostic methods and patient history to ensure accuracy.
Factors Affecting A1C Results
Several factors can influence A1C results, potentially leading to misdiagnosis or inaccurate assessments of glycemic control. Conditions such as iron deficiency anemia (IDA), variant hemoglobin, and uremia can alter A1C levels. A systematic review and meta-analysis found that while the effects of HbAS and uremia on A1C levels are within the expected individual variation, the impact of IDA/ID remains inconclusive and requires further study. Additionally, hemolytic anemia and chronic infections can lower A1C levels, while iron deficiency anemia can increase them by 1-1.5%. These factors highlight the need for careful interpretation of A1C results, especially in patients with underlying conditions.
Impact on Treatment and Lifestyle
The A1C test is crucial for managing diabetes as it provides a long-term view of blood glucose control, which is essential for adjusting treatment plans and lifestyle interventions. By translating A1C levels into estimated average glucose (eAG) values, healthcare providers can better communicate with patients and tailor their treatment strategies. Effective management of diabetes often involves a combination of medication, diet, and exercise. Understanding A1C levels helps in setting realistic goals and monitoring the effectiveness of these interventions. However, due to the potential for variability in A1C results caused by other health conditions, it is important to use A1C in conjunction with other monitoring methods to ensure comprehensive diabetes management.
Who Should Get an A1C Test?
The A1C test is an essential diagnostic tool used to measure average blood sugar levels over a period of two to three months. It is crucial for identifying individuals at risk of diabetes or those needing to manage their condition effectively. Here are the groups of people who should consider getting an A1C test:
1. Adults Age 45 and Older
Adults aged 45 and older are recommended to undergo an A1C test as part of routine diabetes screening. This age group is at a higher risk for developing type 2 diabetes, and early detection through A1C testing can help manage and mitigate complications associated with the disease. The A1C test measures average blood glucose levels over the past two to three months, providing a more comprehensive picture of an individual’s glycemic control compared to single glucose measurements. Regular screening in this demographic can lead to timely interventions, improving long-term health outcomes and reducing the risk of diabetes-related complications.
2. Adults Under 45 Who Are Overweight
For adults under 45 who are overweight, an A1C test is crucial for early detection of diabetes or prediabetes. Excess weight is a significant risk factor for insulin resistance and type 2 diabetes. The A1C test can identify individuals at risk even before symptoms appear, allowing for early lifestyle interventions and medical management to prevent the progression to full-blown diabetes. Studies have shown that overweight individuals with an A1C level of 5.7% to 6.4% are at a higher risk of developing diabetes, making regular monitoring essential for this group.
3. People Who Have Been Diagnosed with Prediabetes
Individuals diagnosed with prediabetes should regularly undergo A1C testing to monitor their condition and prevent the progression to type 2 diabetes. Prediabetes is characterized by higher-than-normal blood glucose levels that are not yet high enough to be classified as diabetes. The A1C test helps track these levels over time, providing valuable information for adjusting lifestyle and treatment plans. Regular A1C testing in prediabetic individuals can lead to early interventions, such as dietary changes and increased physical activity, which are effective in delaying or preventing the onset of diabetes.
4. People Who Have Been Diagnosed with Diabetes
For individuals diagnosed with diabetes, the A1C test is a critical tool for managing the disease. It provides a long-term view of blood glucose control, which is essential for adjusting treatment plans and preventing complications such as neuropathy, retinopathy, and cardiovascular diseases. The American Diabetes Association recommends that diabetic patients maintain an A1C level below 7% to reduce the risk of complications. Regular A1C testing allows healthcare providers to assess the effectiveness of current treatments and make necessary adjustments to improve glycemic control.
5. Pregnant Women
Pregnant women, particularly those at risk for gestational diabetes, should undergo A1C testing as part of their prenatal care. Gestational diabetes can lead to complications for both the mother and the baby, including high birth weight and preterm birth. The A1C test can help identify women with undiagnosed diabetes or those at risk of developing gestational diabetes, allowing for early intervention and management. Monitoring A1C levels during pregnancy ensures better maternal and fetal outcomes by maintaining optimal blood glucose levels throughout the pregnancy.
Why the A1C Test is Important
Benefits over Regular Blood Glucose Testing
The A1C test offers significant advantages over regular blood glucose testing by providing a more comprehensive picture of long-term glycemic control. Unlike daily blood glucose tests that reflect immediate glucose levels, the A1C test measures the average blood glucose levels over the past 2-3 months, making it a more reliable indicator of overall metabolic control. This long-term perspective helps in identifying trends and patterns that might be missed with daily testing, thereby facilitating better management of diabetes. Additionally, the A1C test is less susceptible to short-term fluctuations caused by diet, exercise, or stress, making it a more stable and objective measure.
Predicting Long-Term Health Risks
The A1C test is crucial for predicting long-term health risks associated with diabetes. Studies have shown that maintaining A1C levels close to the normal range significantly reduces the risk of long-term complications such as cardiovascular disease, neuropathy, and retinopathy. The Diabetes Control and Complications Trial established a clear link between lower A1C levels and reduced incidence of these complications, underscoring the test’s predictive value. Furthermore, the A1C test can identify individuals at high risk for developing diabetes, allowing for early intervention and preventive measures. This predictive capability makes the A1C test an invaluable tool in both clinical practice and public health.
Its Role in Monitoring Treatment Effectiveness
The A1C test plays a pivotal role in monitoring the effectiveness of diabetes treatment. By providing a long-term view of blood glucose levels, it helps healthcare providers assess how well a treatment plan is working and make necessary adjustments. Regular A1C testing can identify patients with poor glycemic control, prompting timely and more aggressive treatment changes. This is particularly important for noninsulin-treated type 2 diabetes patients, where structured self-monitoring of blood glucose has been shown to significantly reduce A1C levels. The test’s ability to reflect the cumulative effect of various treatment modalities makes it an essential component of diabetes management.
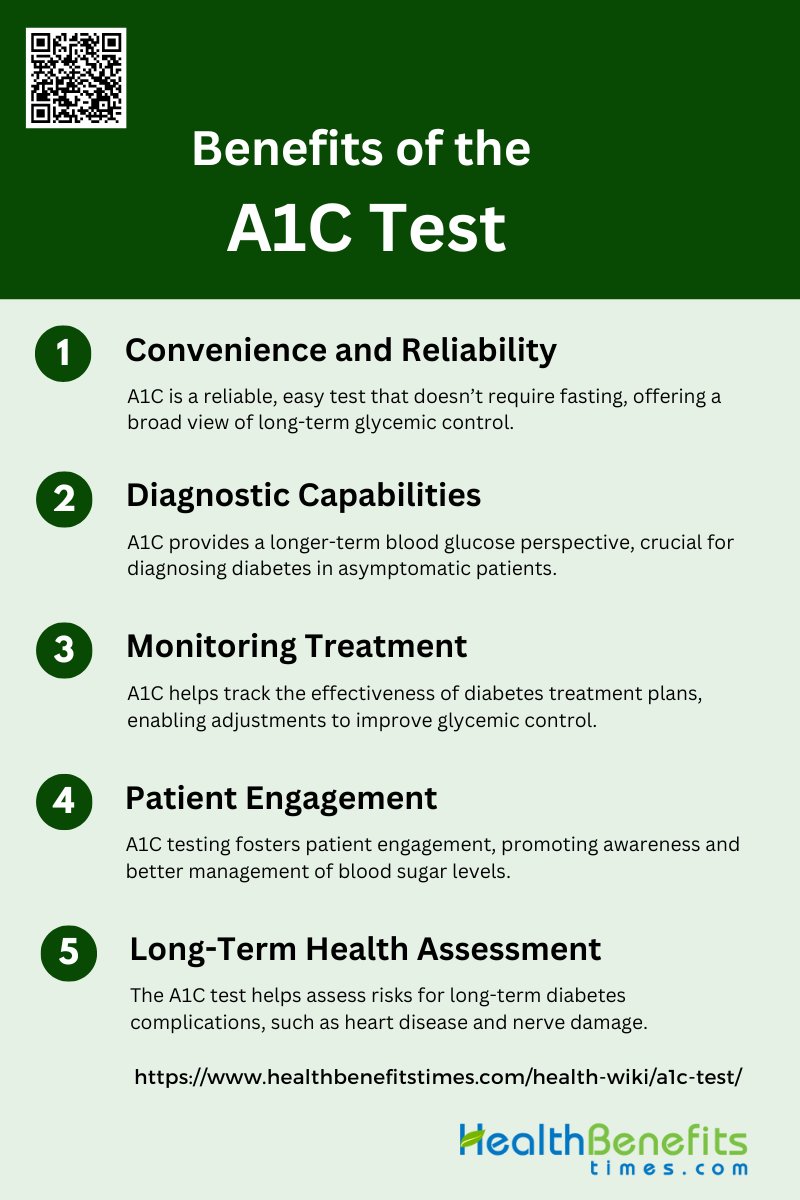
Benefits of the A1C Test
The A1C test is a crucial component in diabetes management, offering numerous advantages for both patients and healthcare providers. It provides a comprehensive view of blood sugar control over time, aiding in diagnosis, treatment, and long-term health planning. Here are the key benefits of the A1C test:
1. Convenience and Reliability
The A1C test is highly convenient and reliable for both patients and healthcare providers. It measures the average blood glucose levels over the past two to three months, providing a comprehensive picture of a patient’s glycemic control without the need for fasting or multiple daily tests. This convenience can lead to increased patient compliance and more frequent monitoring, which is crucial for effective diabetes management. Additionally, the A1C test is less affected by short-term fluctuations in blood glucose levels, making it a more stable and reliable indicator of long-term glycemic control compared to daily glucose monitoring.
2. Diagnostic Capabilities
The A1C test has been endorsed by major health organizations, including the American Diabetes Association, as a diagnostic tool for diabetes. It offers a significant advantage over traditional fasting glucose tests by providing a longer-term view of blood glucose levels, which can help in identifying patients who might otherwise be missed. The test is particularly useful in diagnosing diabetes in nonpregnant adults and is increasingly being adopted in Western countries. However, it is important to note that certain conditions, such as hemoglobinopathies, can affect the accuracy of A1C results, necessitating the use of additional diagnostic methods in some cases.
3. Monitoring Treatment
The A1C test is invaluable for monitoring the effectiveness of diabetes treatment plans. By providing an average blood glucose level over a few months, it allows healthcare providers to make informed decisions about treatment adjustments. Regular A1C testing can identify patients with poor glycemic control and facilitate timely interventions to improve their metabolic status. Moreover, the test’s ability to reflect long-term glycemic control makes it a critical tool for assessing the risk of diabetes-related complications and ensuring that treatment goals are being met.
4. Patient Engagement
The A1C test plays a crucial role in patient engagement and education. Understanding their A1C levels helps patients grasp the importance of maintaining good glycemic control and the long-term health risks associated with poor management. Studies have shown that patients who are aware of their A1C levels are more likely to take an active role in their diabetes care, leading to better outcomes. The test also facilitates meaningful discussions between patients and healthcare providers, helping to tailor treatment plans and set realistic goals.
5. Long-Term Health Assessment
The A1C test is a powerful tool for assessing long-term health risks associated with diabetes. Maintaining A1C levels close to the normal range has been shown to significantly reduce the risk of long-term complications such as cardiovascular disease, neuropathy, and retinopathy. The test’s ability to provide a stable and reliable measure of chronic glycemia makes it essential for long-term health monitoring and risk assessment. By regularly measuring A1C, healthcare providers can better predict and prevent the onset of diabetes-related complications, ultimately improving patient outcomes.
How to Lower A1C Levels
Lowering A1C levels is crucial for managing diabetes and reducing the risk of complications. By adopting a comprehensive approach that includes lifestyle and medical strategies, individuals can effectively control their blood sugar levels. Here are some key methods to help lower A1C levels:
1. Dietary Changes
Adopting a low-carbohydrate diet can significantly lower A1C levels in individuals with type 2 diabetes mellitus (T2DM). Studies have shown that a diet with reduced carbohydrate intake leads to improvements in glycemic control and other cardiometabolic outcomes. For instance, a randomized trial demonstrated that participants on a low-carbohydrate diet had a greater decrease in A1C levels compared to those on a usual diet, with a net difference of -0.23% over six months. Additionally, dietary modifications based on postprandial glucose monitoring can further enhance glycemic control, as evidenced by a study where participants who monitored their glucose levels post-meal saw significant reductions in A1C, body weight, and lipid levels.
2. Exercise Regularly
Regular exercise is a cornerstone in managing A1C levels for individuals with T2DM. A meta-analysis revealed that exercise interventions lasting at least 12 weeks led to a significant reduction in A1C levels, with a pooled mean difference of -0.4%. The reduction in A1C was closely associated with a decrease in body fat mass, indicating that the benefits of exercise on glycemic control are partly mediated by weight loss. Another study found that supervised exercise training improved A1C levels, fitness, and body composition, highlighting the multifaceted benefits of physical activity. These findings underscore the importance of incorporating regular exercise into diabetes management plans.
3. Maintain a Healthy Weight
Maintaining a healthy weight is crucial for lowering A1C levels in individuals with T2DM. Weight loss achieved through lifestyle interventions, including diet and exercise, has been shown to significantly improve glycemic control. For example, a study on a structured lifestyle intervention program found that participants who lost weight also experienced a reduction in A1C levels by 0.3%. Additionally, a randomized clinical trial indicated that weight loss mediated a substantial portion (59%) of the reduction in A1C levels achieved through a low-carbohydrate diet. These results highlight the importance of weight management in controlling blood glucose levels.
4. Medication Management
Effective medication management is essential for lowering A1C levels in individuals with diabetes. Adjusting glucose-lowering medications to target optimal A1C levels can significantly impact patient outcomes. A study involving hemodialysis patients with diabetes found that maintaining A1C levels within a specific range (7-7.9%) was associated with lower mortality rates compared to both higher and lower A1C levels. This suggests that careful titration of diabetes medications to achieve and maintain target A1C levels is critical for improving long-term health outcomes in diabetic patients.
5. Stress Management
Managing stress is an important, yet often overlooked, aspect of controlling A1C levels. Chronic stress can negatively impact blood glucose control by increasing insulin resistance and promoting unhealthy behaviors. While specific studies on stress management and A1C levels are limited, lifestyle interventions that include stress reduction techniques, such as mindfulness and relaxation exercises, have been shown to improve overall health and well-being. For instance, a lifestyle intervention program that included motivational and educational components led to significant improvements in physical and mental health, which can indirectly contribute to better glycemic control.
6. Regular Monitoring
Regular monitoring of blood glucose levels is vital for managing A1C levels effectively. Self-monitoring of blood glucose (SMBG) allows individuals to make informed decisions about their diet, exercise, and medication, leading to better glycemic control. A study demonstrated that postprandial self-monitoring of blood glucose (pp-SMBG) resulted in further improvements in A1C levels, lipids, and body weight in individuals who had already achieved their A1C goals. This highlights the importance of regular monitoring in maintaining and improving glycemic control.
7. Lifestyle Adjustments
Comprehensive lifestyle adjustments, including diet, exercise, and regular monitoring, are essential for lowering A1C levels. Digital delivery of lifestyle interventions has been shown to be effective in decreasing A1C levels, providing a convenient and accessible option for patients. These interventions often include components such as dietary counseling, exercise programs, and self-monitoring of blood glucose, which collectively contribute to improved glycemic control. Integrating these lifestyle changes into daily routines can empower individuals to manage their diabetes more effectively and achieve better health outcomes.
Limitations of the A1C Test
While the A1C test is a valuable tool for managing diabetes, it does have certain limitations that can affect its accuracy and applicability. Understanding these limitations is crucial for both patients and healthcare providers to ensure effective diabetes management. Here are some key limitations of the A1C test:
1. Factors Affecting Accuracy
The accuracy of the A1C test can be influenced by several factors, including the presence of certain hemoglobin variants, anemia, and other hematologic conditions. For instance, conditions such as G6PD deficiency and hemoglobinopathies can lead to discrepancies between A1C levels and actual blood glucose levels. Additionally, factors like race and aging may also alter A1C interpretation, although the clinical implications of these differences remain contentious. These variations can lead to either overestimation or underestimation of glycemic control, thereby affecting the reliability of the A1C test.
2. Limitations in Specific Populations
The A1C test has shown limitations in specific populations, such as African-born individuals and obese children. In African-born blacks, the A1C test underperformed even in the absence of nutritional deficiencies, anemia, and hemoglobinopathies, missing about 60% of diabetes cases and 40% of prediabetes cases. Similarly, in obese children and adolescents, the A1C test demonstrated low sensitivity and specificity, making it a poor diagnostic tool for prediabetes and type 2 diabetes in this population. These findings suggest that alternative diagnostic methods may be necessary for accurate diabetes detection in these groups.
3. Inability to Detect Short-Term Fluctuations
One of the significant limitations of the A1C test is its inability to detect short-term fluctuations in blood glucose levels. The A1C test reflects average blood glucose levels over the past two to three months, making it unsuitable for capturing daily glycemic variability and short-term hyperglycemic excursions. Continuous glucose monitoring (CGM) systems, which provide real-time data, offer a more comprehensive picture of glycemic control and are valuable for timely intervention and individualized therapy adjustments.
4. Limited Utility in Some Situations
The A1C test has limited utility in certain clinical situations, such as during periods of acute stress or illness, where stress hyperglycemia can occur. For example, in tuberculosis patients, the A1C test performed better than fasting plasma glucose (FPG) but still had limitations in accurately diagnosing newly diagnosed diabetes (NDD). Additionally, the A1C test may not be suitable for populations where the test is either unavailable or too expensive, necessitating the use of alternative glucose tests and criteria.
5. Standardization Issues
Despite significant efforts to standardize the A1C test, inconsistencies still exist. The National Glycohemoglobin Standardization Program (NGSP) has made substantial progress in improving the accuracy of A1C measurements, but some factors that previously influenced results, such as carbamylation and common hemoglobin variants, have not been entirely eliminated. Moreover, the lack of standardization for clinically useful cut-offs or guidelines for alternative glycemic markers further complicates the landscape of diabetes diagnosis and management. These standardization issues highlight the need for ongoing improvements and consensus in the field.
FAQs
1. Can lifestyle changes alone lower A1C levels, or is medication always necessary?
Lifestyle changes, such as improved diet, regular exercise, and weight loss, can significantly lower A1C levels, especially for individuals with prediabetes or early-stage type 2 diabetes. However, for some people, medication may be necessary in conjunction with lifestyle changes to maintain healthy A1C levels. It’s important to consult with a healthcare provider to determine the best course of action.
2. How frequently should someone without diabetes get an A1C test?
For individuals without diabetes, the A1C test is typically recommended as part of routine screening starting at age 45, or earlier if there are risk factors like obesity or a family history of diabetes. For those with normal A1C levels, testing every 3 years is usually sufficient, unless new risk factors emerge.
3. Can non-diabetic conditions cause elevated A1C levels?
Yes, certain conditions, such as kidney disease, anemia, or certain genetic hemoglobin disorders, can lead to elevated A1C levels even in individuals who do not have diabetes. This is why additional tests or assessments may be needed to accurately diagnose diabetes.
4. Can an A1C test be used to detect gestational diabetes?
The A1C test is not typically used to diagnose gestational diabetes, as it reflects average blood sugar levels over a period of 2-3 months and may not capture the rapid changes in glucose levels that occur during pregnancy. Oral glucose tolerance tests (OGTT) are more commonly used for diagnosing gestational diabetes.
5. Can stress or illness affect my A1C test results?
While short-term stress or illness can cause temporary spikes in blood glucose levels, the A1C test measures long-term glucose control over 2-3 months. Therefore, temporary stress or illness is less likely to have a significant impact on A1C levels, but chronic stress may lead to prolonged elevations in blood glucose, affecting the result.
6. What alternative tests are available if the A1C test is inaccurate for me?
In cases where the A1C test may not provide accurate results (e.g., due to hemoglobin variants, anemia, or certain genetic conditions), alternative tests like the fasting plasma glucose (FPG) test, oral glucose tolerance test (OGTT), or continuous glucose monitoring (CGM) may be used to assess blood sugar levels.
7. How does A1C relate to the risk of cardiovascular diseases?
Higher A1C levels are associated with an increased risk of cardiovascular diseases, such as heart attacks and strokes, particularly in individuals with diabetes. Maintaining lower A1C levels helps reduce the risk of these complications by improving overall blood sugar control.
8. Can weight loss lower A1C levels, and if so, how much weight loss is needed?
Weight loss, especially in people with type 2 diabetes or prediabetes, can significantly lower A1C levels. Even a modest weight loss of 5-10% of body weight has been shown to improve blood sugar control and reduce A1C levels.
9. What happens if my A1C levels remain high despite following treatment plans?
If A1C levels remain high despite medication, diet, and exercise, it may indicate that your current treatment plan is not effective. In such cases, your healthcare provider might adjust your medications, recommend more frequent monitoring, or explore other factors such as medication adherence or underlying conditions affecting blood sugar control.
10. Does the A1C test provide any information on hypoglycemia (low blood sugar)?
The A1C test measures average blood glucose levels and does not provide specific information about episodes of hypoglycemia. Continuous glucose monitoring (CGM) or self-monitoring with blood glucose meters are better tools for identifying patterns of low blood sugar.