- It is the lack of essential nutrients in the body, leading to impaired health and functions.
- Learn evidence-based strategies to recognize early signs of nutrient deficiencies through symptoms and health indicators.
- Explore practical tips for addressing deficiencies with diet, supplements, and professional guidance.
 Nutrient deficiencies refer to the state where the body lacks one or more essential vitamins or minerals required for optimal functioning, which can have a profound impact on health and well-being (1). Understanding and addressing these deficiencies are critical, as they can lead to chronic diseases and hinder physical and cognitive development. Evidence-based strategies for identifying nutrient deficiencies include regular monitoring through biochemical assessments and dietary analysis, ensuring sufficient intake of diverse foods (2). Moreover, targeted interventions such as food fortification and supplementation can help mitigate deficiencies like iodine and vitamin D, which are common across populations (3). Emphasis on dietary diversity, especially in regions with limited access to nutrient-dense foods, is another critical approach (4). Integrating evidence-based guidelines into public health strategies can also enhance awareness and reduce the prevalence of deficiencies (5). Finally, addressing nutrient needs in specialized diets, such as ketogenic plans, requires careful consideration to avoid imbalances (6). These practical measures can serve as a foundation for addressing the growing challenge of nutrient deficiencies globally (7).
Nutrient deficiencies refer to the state where the body lacks one or more essential vitamins or minerals required for optimal functioning, which can have a profound impact on health and well-being (1). Understanding and addressing these deficiencies are critical, as they can lead to chronic diseases and hinder physical and cognitive development. Evidence-based strategies for identifying nutrient deficiencies include regular monitoring through biochemical assessments and dietary analysis, ensuring sufficient intake of diverse foods (2). Moreover, targeted interventions such as food fortification and supplementation can help mitigate deficiencies like iodine and vitamin D, which are common across populations (3). Emphasis on dietary diversity, especially in regions with limited access to nutrient-dense foods, is another critical approach (4). Integrating evidence-based guidelines into public health strategies can also enhance awareness and reduce the prevalence of deficiencies (5). Finally, addressing nutrient needs in specialized diets, such as ketogenic plans, requires careful consideration to avoid imbalances (6). These practical measures can serve as a foundation for addressing the growing challenge of nutrient deficiencies globally (7).
Understanding Nutrient Deficiencies
Nutrient deficiencies occur when the body does not receive adequate levels of essential vitamins and minerals, leading to various health complications. Common deficiencies include iron, vitamin D, iodine, and zinc, each associated with conditions such as anemia, bone disorders, and immune dysfunction (8). For example, iron deficiency is prevalent worldwide and often linked to fatigue and impaired cognitive function (9). Similarly, vitamin D insufficiency is a major concern for bone health, particularly in regions with limited sunlight (10).
The causes of nutrient deficiencies vary widely and include poor dietary habits, limited food diversity, and socioeconomic challenges. For instance, a lack of nutrient-dense foods in the diet often results from over-reliance on processed foods (11). Environmental factors, such as depleted soil quality, also contribute to reduced micronutrient content in crops (12).
Specific populations are at a heightened risk for nutrient deficiencies. These groups include pregnant women, who require higher levels of nutrients like folic acid and iron for fetal development, and the elderly, who often face challenges in nutrient absorption (13). Children in low-income settings are also particularly vulnerable due to limited access to balanced diets (14).
Evidence-Based Methods for Identifying Nutrient Deficiencies
Identifying nutrient deficiencies requires a combination of self-awareness, physical examination, and diagnostic tests. Evidence-based methods ensure accurate diagnosis, enabling targeted interventions for improved health and well-being.
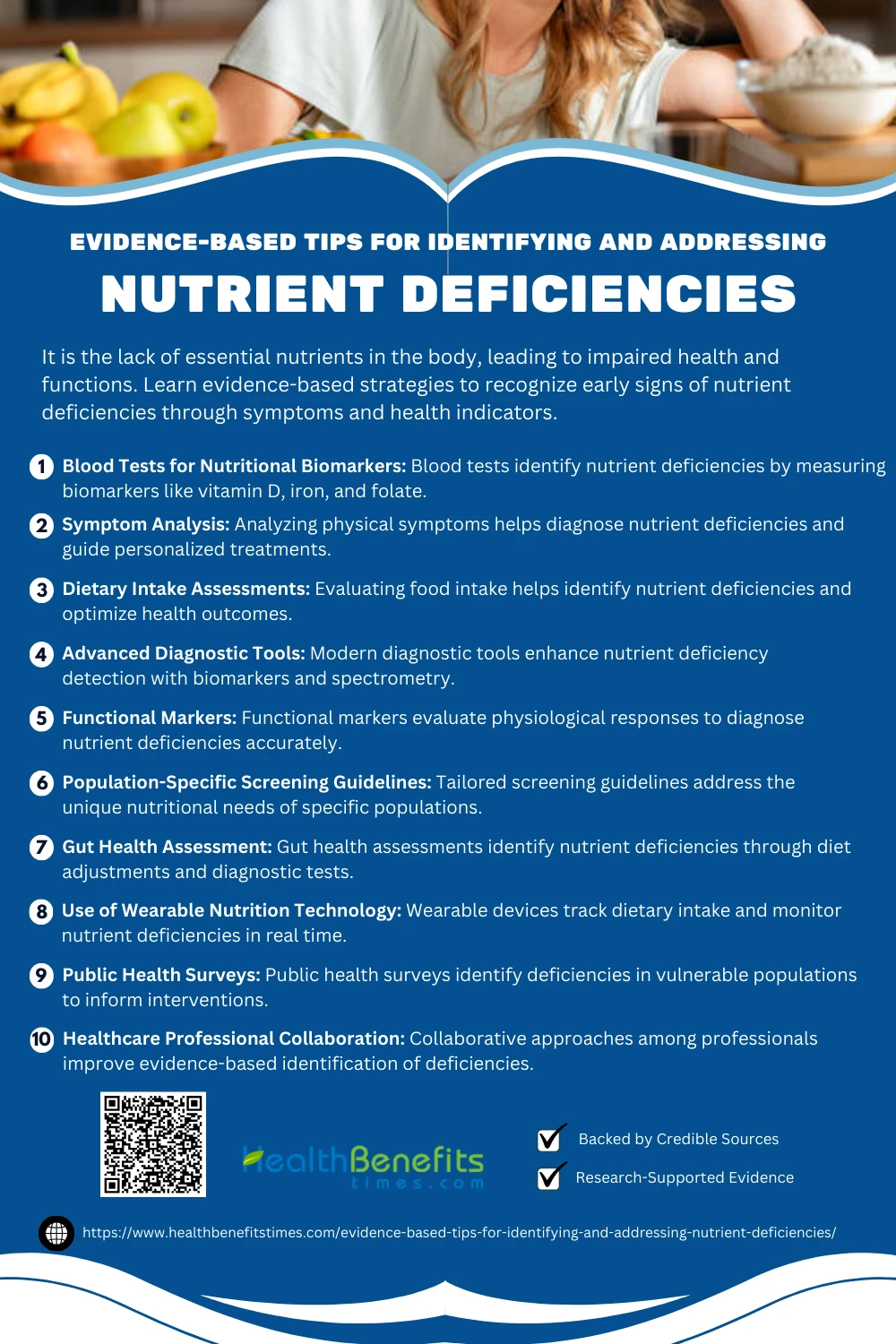 1. Blood Tests for Nutritional Biomarkers
1. Blood Tests for Nutritional Biomarkers
Blood tests are essential tools in identifying nutrient deficiencies by measuring biomarkers like vitamin D, iron, and folate. For instance, 15 are widely used to diagnose vitamin D deficiency. Iron deficiency anemia can be detected through 16. Folate levels are analyzed using 17. Additionally, 18 assess B-vitamin deficiencies, and 19 identifies zinc deficiency.
2. Symptom Analysis
Evidence-based methods for identifying nutrient deficiencies rely on symptom analysis to guide diagnosis and treatment. Analyzing symptoms like gastrointestinal issues helps clinicians employ targeted dietary interventions, such as the FODMAP approach (6). Systematic reviews emphasize the role of symptom-guided evaluation in malnutrition management. Evidence-based dietary guidelines refine nutrient assessment strategies (20). Symptom-driven methods for diagnosing micronutrient deficiencies are crucial for personalized care.
3. Dietary Intake Assessments
Dietary intake assessments are essential for identifying nutrient deficiencies and optimizing health outcomes. Methods like food frequency questionnaires help assess population-level nutrient adequacy. Assessments of nutrient insufficiencies highlight energy constraints (21). Comprehensive reviews modernize nutrient guidelines (22). Dietary strategies address chronic conditions effectively (23).
4. Advanced Diagnostic Tools
Advanced diagnostic tools enhance the detection of nutrient deficiencies through evidence-based methods. Tools like biomarkers and spectrometry effectively identify nutritional imbalances (24). Modern diagnostic pathways integrate data modeling to refine recommendations (22). Malnutrition screening tools validate deficiency detection (23). Infrared spectroscopy supports non-invasive diagnostics (25). Reliable diagnostic tests evaluate biochemical markers for clinical precision (26).
5. Functional Markers
Functional markers offer an evidence-based approach to identifying nutrient deficiencies by evaluating physiological responses. Biomarkers link nutrition to health status, enhancing diagnostic accuracy (24). Consensus-building initiatives standardize functional nutrient assessments (27). Advanced functional markers refine health claims validations (28). NFPE emphasizes functional specificity for detecting deficiencies (29).
6. Population-Specific Screening Guidelines
Population-specific screening guidelines improve nutrient deficiency detection by tailoring assessments to demographic needs. Refugee-specific guidelines address unique deficiencies (30). Consensus strategies highlight older adults’ nutritional needs (31). Frailty management guides Asian populations (32). Hemoglobinopathy screening exemplifies population-specific genetic testing (33).
7. Gut Health Assessment
Assessing gut health provides a pathway to identifying nutrient deficiencies. Evidence-based methods like the FODMAP diet 6 address functional gut symptoms. Breath tests have improved lactase deficiency diagnostics 34. Modern dietary guidelines highlight microbiota’s role in nutrient synthesis 22. Targeted strategies like gluten-free diets aid IBS patients 35, while nutrition screening tools help malnutrition 36.
8. Use of Wearable Nutrition Technology
Wearable nutrition technology enables precise identification of nutrient deficiencies. Devices like wristbands validate dietary intake 37, while advancements in low-income regions are transforming care 38. Smart systems enhance remote nutrient monitoring 39. Integrated tools like MiranaBot offer personalized nutrition insights 40. Data modeling advances wearable utility for nutrient care 22..
9. Public Health Surveys
Public health surveys play a vital role in identifying nutrient deficiencies, utilizing evidence-based methods like EURRECA guidelines 41. Tools such as DHS and MICS surveys document deficiencies in vulnerable populations 42. Vitamin deficiency interventions in public health strategies have been explored globally 43. Survey-based evidence informs maternal and child nutrition programs 44.. Additionally, data-driven interventions address deficiencies in indigenous communities 45.
10. Healthcare Professional Collaboration
Collaboration among healthcare professionals enhances evidence-based methods to identify nutrient deficiencies. EURRECA guidelines provide frameworks for micronutrient recommendations 41. Expert syntheses inform dietary interventions for improved outcomes 22. Evidence-based reviews address maternal undernutrition 44. Nutrition assessments differentiate patient needs effectively 46. Collaborative reviews foster advanced nutrition care strategies 47.
Common Signs and Symptoms of Nutrient Deficiencies
Nutrient deficiencies can manifest through various symptoms, including fatigue, brittle nails, or memory issues. Recognizing these signs early is essential for timely intervention and better health.
- Fatigue and Weakness
A lack of energy or constant tiredness is one of the most recognizable signs of nutrient deficiencies. Iron deficiency anemia impairs the oxygen-carrying capacity of red blood cells, leading to fatigue and weakness. Vitamin B12 deficiency also affects red blood cell production, causing similar symptoms. This is particularly common in individuals with poor diets, vegetarian lifestyles, or absorption issues. - Hair Loss and Brittle Nails
Deficiencies in biotin, a B-vitamin, can lead to hair thinning, brittle nails, and even skin rashes. Biotin plays a critical role in the metabolism of amino acids and fatty acids, which are essential for maintaining strong hair and nails. Symptoms may be exacerbated in individuals who consume raw egg whites or those with malabsorption issues. - Skin Problems
Nutrient deficiencies often manifest in the skin. Vitamin A deficiency may cause dry, scaly skin, while vitamin E deficiency can lead to hyperpigmentation or rough patches. Zinc deficiency may cause acne-like rashes around the mouth or face. These symptoms are more common in individuals with restrictive diets or those with conditions that impair fat absorption. - Bone Pain and Fragility:
Insufficient vitamin D levels, often due to limited sunlight exposure or poor diet, can weaken bones and lead to fractures or osteomalacia (soft bones). Calcium deficiency further exacerbates this, increasing the risk of osteoporosis and chronic bone pain, especially in older adults or postmenopausal women. - Cognitive Impairments
Memory issues, poor concentration, or brain fog can be linked to omega-3 fatty acid deficiency, as these are critical for maintaining brain function. Additionally, a lack of vitamin B1 (thiamine) can lead to nerve damage and more severe cognitive issues, such as those seen in Wernicke-Korsakoff syndrome. These issues are especially common in individuals with poor diets or chronic alcohol consumption.
Prevention of Nutrient Deficiencies
“Prevention of nutrient deficiencies is vital for optimal health. Balanced diets, proper supplementation, and awareness of essential nutrients ensure the body thrives and avoids health complications.”
 1. Dietary Diversification
1. Dietary Diversification
Dietary diversification effectively prevents nutrient deficiencies by including a variety of nutrient-rich foods from multiple groups. For example, increasing intake of diverse foods has shown potential in addressing hidden hunger and multiple micronutrient deficiencies 4. Diversification helps improve overall micronutrient intake, including iron and zinc, and mitigates antagonistic nutrient interactions 48. Furthermore, such strategies are crucial in developing regions to combat anemia among women 49. Diversification complements fortification approaches, creating sustainable nutritional outcomes 50. Lastly, interdisciplinary reviews highlight its feasibility as a sustainable approach to address deficiencies globally 51.
2. Food Fortification
Food fortification is an effective strategy to combat nutrient deficiencies globally, enhancing the nutritional profile of staple foods and reducing the prevalence of deficiencies. Programs such as fortifying cereals and oils have demonstrated success in addressing vitamin A and iron deficiencies 52. Fortification complements dietary diversification by addressing gaps in specific micronutrient needs 53. Economic benefits from fortification programs, especially in low-resource settings, are well-documented 54. Moreover, mandatory programs, such as iodized salt initiatives, have drastically reduced global iodine deficiencies 55. Research highlights that fortification is most impactful when aligned with nutrition education 56. Integrated food fortification programs address micronutrient deficiencies sustainably 57. Addressing logistical and technical challenges further improves their success 58.
3. Bio-fortification
Bio-fortification enhances the nutrient profile of staple crops to combat micronutrient deficiencies effectively. For example, breeding zinc-rich wheat significantly reduces deficiencies in developing countries 59. Similarly, bio-fortified vegetables have improved nutrition quality globally 60. This approach also mitigates anemia and stunting caused by iron and zinc deficiencies 61. Research highlights its impact on improving global health, reducing hidden hunger effectively 62. Agronomic bio-fortification strategies in wheat further alleviate zinc deficiency in vulnerable populations 63.. Bio-fortification also enhances crop resilience against environmental challenges 64. Finally, it integrates sustainable agricultural practices with nutritional security 65.
4. Micronutrient Supplementation
Micronutrient supplementation is a vital strategy for preventing deficiencies, particularly in vulnerable populations. For instance, targeted supplementation programs in developing countries have successfully reduced deficiencies in women and children. Iron and folate supplements have effectively prevented anemia during pregnancy 66. This approach is crucial for improving growth and reducing morbidity in children 67. Moreover, supplementation remains an essential tool for addressing global micronutrient deficiencies 68.
5. Nutrition Education
Nutrition education plays a vital role in preventing nutrient deficiencies by fostering informed dietary choices. School-based interventions enhance children’s dietary knowledge and nutrient intake. Community-driven education improves maternal and child nutrition outcomes 66. Furthermore, culturally tailored approaches increase program effectiveness 67. Combining education with access to nutrient-rich foods creates long-term nutritional benefits 68.
6. Improved Agricultural Practices
Improved agricultural practices are essential for addressing nutrient deficiencies through sustainable food systems. Techniques like biofortification and crop diversification enhance nutrient content in staple foods 69. Optimizing soil management prevents deficiencies in crops, including iron and zinc 70. Integrated approaches such as agronomic interventions boost nutrient uptake in plants and promote public health 71. These methods also combat malnutrition by linking agriculture with nutrition education 72. Additionally, nutrient-efficient genotypes ensure consistent crop yields and quality 73.
7. Regular Health Screenings
Regular health screenings are crucial in identifying and preventing nutrient deficiencies, especially in at-risk populations. Screening programs have proven effective in detecting deficiencies like anemia and addressing them early 74. Initiatives for the elderly help reduce malnutrition risks 75. Neonatal screening programs have also demonstrated nutritional benefits, improving long-term health outcomes 76. Furthermore, integrating nutrition assessment into routine health check-ups enhances dietary guidance 77. Comprehensive screening guidelines, like those by WHO, emphasize their role in public health 78.
Challenges and Limitations
“Identifying and addressing nutrient deficiencies presents challenges like varying symptoms, inaccurate diagnostic tools, dietary restrictions, cultural practices, and limited access to healthcare, hindering effective prevention and treatment efforts.”
 1. Lack of Accurate Screening Tools
1. Lack of Accurate Screening Tools
The lack of accurate screening tools significantly hinders early detection of nutrient deficiencies, especially in high-risk groups. Many screening methods, like 24-hour dietary recalls, are impractical for daily use 79. Nutritional assessment tools are particularly limited for addressing individual metabolic differences and needs 80. Inadequate understanding of micronutrient biomarkers adds complexity to identifying deficiencies 81. Furthermore, existing tools lack precision in assessing coexisting deficiencies in vulnerable populations 82. Innovations are needed to create cost-effective and scalable solutions for widespread nutrient screening 83.
2. Asymptomatic Nature of Deficiencies
The asymptomatic nature of many nutrient deficiencies complicates early diagnosis and intervention, as symptoms often manifest only in advanced stages. For example, vitamin B12 deficiency can remain undetected due to nonspecific symptoms 84. Similarly, iron deficiency in children is frequently overlooked in the absence of clear clinical signs 85. Diagnostic challenges also arise with conditions like anemia, where asymptomatic cases complicate public health actions 86. Urea cycle disorders in adults often go undetected until severe complications arise 87. Additionally, the absence of overt symptoms in nutrient deficiencies can delay interventions in conditions like pancreatic insufficiency 88.
3. Cultural and Dietary Habits
Cultural and dietary habits significantly influence nutrient intake, often leading to deficiencies. For instance, traditional plant-based diets in developing countries can lack critical nutrients like protein and iron 89. Religious and cultural restrictions further limit food choices, affecting nutrition 90. Socioeconomic factors exacerbate micronutrient deficiencies in regions like India, where dietary shifts create imbalanced nutrition 91. Inadequate clinical nutrition strategies often fail to address these barriers comprehensively 92. Addressing these challenges requires culturally tailored approaches to integrate traditional diets with modern nutrition science 93.
4. Economic Barriers
Economic barriers hinder efforts to address nutrient deficiencies, particularly in low- and middle-income countries. Limited financial resources constrain access to fortified foods and supplements, especially for vulnerable populations 94. Cost challenges in scaling up food fortification programs further impede progress 95. Socioeconomic disparities exacerbate malnutrition, as seen in rural Ethiopia 96. Urbanization intensifies food insecurity due to the high cost of nutritious foods 97. Addressing these barriers requires integrating nutrition into broader economic and policy frameworks 98.
5. Inconsistent Policy Implementation
Inconsistent policy implementation hinders efforts to address nutrient deficiencies effectively. Poor coordination across sectors often results in fragmented nutrition programs, as observed in Ethiopia’s multi-sectoral approaches 99. Policy gaps and lack of streamlined tools further exacerbate the issue in maternal nutrition programs 100. Urban food security policies also highlight the absence of coherence in tackling nutrition challenges comprehensively 97. In South Africa, overlapping mandates among agencies contribute to ineffective policy alignment 101. Moreover, inconsistent target population definitions undermine large-scale nutrition interventions in low-income countries 102.
6. Biological Variability
Biological variability poses significant challenges in addressing nutrient deficiencies, as individual differences in absorption and metabolism affect nutrient needs. Exploiting genetic variation in crops can mitigate these issues, enhancing nutrient quality 103. Precision nutrition strategies aim to tailor interventions based on individual biological responses 104.. Nutrigenomics explores how genetic and epigenetic variations impact nutrient metabolism and health 105. Adaptive variability in nutritional needs across populations underscores the importance of targeted interventions 106. Integrating biological data into breeding programs further aids in combating nutrient deficiencies 107.
7. Knowledge Gaps in Public Health
Knowledge gaps in public health limit efforts to address nutrient deficiencies effectively. For example, data on micronutrient malnutrition remain inconsistent, hindering evidence-based interventions 43. Reliable food composition data is often lacking, especially in developing regions 108. Urban food insecurity further exacerbates the issue due to limited understanding of socio-economic disparities 97. Gaps in research also impede the development of effective public health nutrition strategies 109. Lastly, coordination challenges between health and nutrition sectors contribute to fragmented policies 110..
8. Food Supply Chain Issues
Food supply chain issues exacerbate nutrient deficiencies through inefficiencies and losses. Poor infrastructure and storage conditions often lead to significant nutrient depletion during transit 111. Climate-related disruptions further compromise the availability of nutrient-dense foods 112. Additionally, food processing techniques frequently degrade nutrient content, impacting dietary quality 113. Smallholder value chains struggle with integrating nutrient-sensitive practices, limiting their potential to combat deficiencies 114. Addressing food loss and waste is critical for improving nutritional security 115.
9. Reliance on Single-Approach Interventions
Relying on single-approach interventions to combat nutrient deficiencies often limits effectiveness due to diverse underlying causes. Programs focusing solely on supplementation fail to address systemic dietary gaps 116. Similarly, iron supplementation during pregnancy shows inconsistent results without addressing broader dietary issues 117. Food fortification alone is insufficient for populations with limited access to diverse foods 118. Integrative approaches combining multiple interventions have shown greater success 119. Addressing deficiencies holistically requires coordinated efforts targeting production, accessibility, and education 120.
10. Stigma and Misconceptions
Stigma and misconceptions around nutrient deficiencies hinder effective interventions by perpetuating misinformation. Cultural myths about health-seeking behavior delay timely diagnosis and treatment 121. Misperceptions about conditions like obesity or tuberculosis result in social exclusion and inadequate care 122. This stigma impacts women and children disproportionately in developing countries, complicating nutrition programs 123. Public health campaigns are crucial to debunking myths and promoting awareness 124. Furthermore, addressing stigma requires culturally sensitive approaches to foster inclusivity in healthcare 125.
Conclusion
In conclusion, addressing nutrient deficiencies requires a proactive and evidence-based approach that combines regular health screenings, a well-balanced diet, and targeted supplementation when necessary. Empowering individuals with knowledge about nutrient-rich foods, recognizing early symptoms, and seeking professional guidance are key steps toward maintaining optimal health. Emphasizing the importance of personalized healthcare ensures interventions are tailored to individual needs, making them more effective. By adopting these practices and fostering awareness, we can significantly reduce the prevalence of nutrient deficiencies and their associated health risks, promoting a healthier and more resilient society.
References:
- Franz et al.
- Tapsell et al.
- Camp et al.
- Nair et al.
- American Diabetes Association
- Gibson & Shepherd
- Ackley & Ladwig
- Beede et al.
- Roust & DiBaise
- Romera et al.
- Abbas et al.
- Yin et al.
- Reese & Miller
- Butler et al.
- “Serum 25-hydroxyvitamin D levels”
- “Serum ferritin and hemoglobin levels”
- “Red blood cell folate concentration”
- “Homocysteine tests”
- “Plasma zinc measurement”
- McKenzie, Y. A., Bowyer, R. K., & Leach, H. (2016). British Dietetic Association systematic review and evidence‐based practice guidelines.
- Maki, K. C., Slavin, J. L., & Rains, T. M. (2014). Limitations of observational evidence: implications for evidence-based dietary recommendations.
- McBurney, M. I., Blumberg, J. B., & Costello, R. B. (2021). Beyond nutrient deficiency—modernizing DRIs and supplementation recommendations.
- Ash, S., Campbell, K., & MacLaughlin, H. (2006). Evidence-based practice guidelines for the nutritional management of chronic kidney disease.
- Picó, C., Serra, F., Rodríguez, A. M., Keijer, J., & Palou, A. (2019). Biomarkers of nutrition and health: new tools for new approaches.
- Shepherd, K. D., & Walsh, M. G. (2007). Infrared spectroscopy—an evidence-based diagnostic tool.
- Matarese, L. E., & Charney, P. (2017). Capturing the elusive diagnosis of malnutrition.
- Raiten, D. J., Namasté, S., Brabin, B., & Combs Jr, G. (2011). Biomarkers of Nutrition for Development: building a consensus.
- Biesalski, H. K., Aggett, P. J., Anton, R., & Bernstein, P. S. (2011). Scientific substantiation of health claims: evidence-based nutrition.
- Bharadwaj, S., Ginoya, S., & Tandon, P. (2016). Malnutrition: laboratory markers vs nutritional assessment.
- Pottie, K., Greenaway, C., Feightner, J., & Welch, V. (2011). Evidence-based clinical guidelines for immigrants and refugees.
- Chen, L. K., Arai, H., & Assantachai, P. (2022). Roles of nutrition in muscle health of community-dwelling older adults.
- Dent, E., Lien, C., Lim, W. S., Wong, W. C., & Wong, C. H. (2017). The Asia-Pacific clinical practice guidelines for the management of frailty.
- Goonasekera, H. W., & Paththinige, C. S. (2018). Population screening for hemoglobinopathies.
- Romagnuolo J, et al. (2002). Using breath tests wisely in gastroenterology. LWW.
- McKenzie YA et al. (2016). Dietary management of IBS. Wiley.
- Correia MITD, Hegazi RA (2014). Addressing malnutrition. ScienceDirect.
- Dimitratos SM, German JB (2020). Wearable technology to quantify nutritional intake. JMIR mHealth.
- Tambo E, Ngogang JY (2018). Wearable technology revolution in low-income countries. Academic Journals.
- Coman LI et al. (2024). Smart solutions for diet-related disease management. MDPI.
- Randriambelonoro M (2022). MiranaBot: Nutrition assessment case. OAPEN.
- Dhonukshe-Rutten RAM, Bouwman J (2013). EURRECA guidelines for micronutrient recommendations. Taylor & Francis.
- Neufeld LM, Cameron BM (2012). DHS and MICS surveys for micronutrient assessment. ScienceDirect.
- Darnton-Hill I (2019). Prevention and control of vitamin deficiencies. ScienceDirect.
- Bhutta ZA et al. (2013). Maternal and child nutrition interventions. The Lancet.
- Ghosh-Jerath S et al. (2019). Food systems approach for indigenous nutrition. Springer.
- Charney P (2008). Nutrition screening vs. assessment. Wiley.
- Balk EM et al. (2007). Applying evidence-based review to nutrition. ScienceDirect.
- Gibson, R.S., & Anderson, V.P. (2009). A review of interventions based on dietary diversification or modification strategies with the potential to enhance intakes of total and absorbable zinc.
- Rao, S., Joshi, S., Bhide, P., & Puranik, B. (2014). Dietary diversification for prevention of anaemia among women of childbearing age from rural India.
- Bechoff, A., De Bruyn, J., Alpha, A., & Wieringa, F. (2023). Exploring the complementarity of fortification and dietary diversification to combat micronutrient deficiencies: A scoping review.
- Malézieux, E., Verger, E.O., Avallone, S., & Alpha, A. (2024). Biofortification versus diversification to fight micronutrient deficiencies: an interdisciplinary review.
- World Health Organization. (2006). Guidelines on food fortification with micronutrients.
- Dary, O., & Hurrell, R. (2006). Guidelines on food fortification with micronutrients.
- Olson, R., Gavin-Smith, B., Ferraboschi, C., & Kraemer, K. (2021). Food Fortification: The Advantages, Disadvantages and Lessons from Sight and Life Programs.
- Darnton-Hill, I., & Nalubola, R. (2002). Fortification strategies to meet micronutrient needs: successes and failures.
- Liyanage, C., & Hettiarachchi, M. (2011). Food fortification.
- Wimalawansa, S.J. (2013). Rational food fortification programs to alleviate micronutrient deficiencies.
- Shegelman, I.R., Vasilev, A.S., & Shtykov, A.S. (2019). Food fortification-problems and solutions.
- Mulualem, T. (2015). Application of bio-fortification through plant breeding to improve the value of staple crops.
- Nagar, B.L., Thakur, S.S., & Goutam, P.K. (2024). The Role of Bio-fortification in Enhancing the Nutritional Quality of Vegetables: A Review.
- Prasad, S.V.S. (n.d.). Bio-fortification of wheat for improving nutritional security in climate change scenario.
- Ashoka, P., Spandana, B., & Saikanth, D.R.K. (2023). Bio-fortification and its impact on global health.
- Singh, S., Kaur, J., Ram, H., & Kaur, S. (2023). Agronomic bio-fortification of wheat to alleviate zinc deficiency in human beings.
- Malo, M. (n.d.). BIO-FORTIFICATION: Better Crops for Better Nutrition.
- Sandhu, R., Chaudhary, N., Shams, R., & Singh, K. (2023). A critical review on integrating bio-fortification in crops for sustainable agricultural development and nutritional security.
- Gernand, A.D., Schulze, K.J., & Stewart, C.P. (2016). Micronutrient deficiencies in pregnancy worldwide: health effects and prevention.
- Pritwani, R., & Mathur, P. (2015). Strategies to combat micronutrient deficiencies: a review.
- Bailey, R.L., West, K.P. Jr., & Black, R.E. (2015). The epidemiology of global micronutrient deficiencies.
- Welch, R.M., Graham, R.D., & Cakmak, I. (2013). Linking agricultural production practices to improving human nutrition and health.
- Zuo, Y., & Zhang, F. (2011). Soil and crop management strategies to prevent iron deficiency in crops.
- Omari, R., Quorantsen, K.E., & Omari, P.K. (2017). Nutrition knowledge and food consumption practices in rural Ghana.
- Miller, D.D., & Welch, R.M. (2013). Food system strategies for preventing micronutrient malnutrition.
- Khoshgoftarmanesh, A.H., & Schulin, R. (2010). Micronutrient-efficient genotypes for crop yield and nutritional quality.
- Sood, S.K., Srikantia, S.G., & WHO. (1989). Preventing and controlling iron deficiency anemia through primary health care.
- Posner, B.M., Jette, A.M., & Smith, K.W. (1993). Nutrition and health risks in the elderly: the nutrition screening initiative.
- Farrell, P.M., Kosorok, M.R., & Laxova, A. (1997). Nutritional benefits of neonatal screening for cystic fibrosis.
- Stang, J., & Story, M. (2005). Nutrition screening, assessment, and intervention.
- Wilson, J.M.G., & Jungner, G. (1968). Principles and practice of screening for disease.
- Reber, E., Gomes, F., Vasiloglou, M.F., & Schuetz, P. (2019). Nutritional risk screening and assessment.
- Tang, H., & Yang, M. (2023). Nutritional Assessment in Patients with Chronic Diseases: Tools, Challenges, and Future Directions.
- Stover, P.J., Garza, C., Durga, J., & Field, M.S. (2020). Emerging concepts in nutrient needs.
- Ahmed, F., Prendiville, N., & Narayan, A. (2016). Micronutrient deficiencies among children and women in Bangladesh: progress and challenges.
- Bruins, M.J., Bird, J.K., Aebischer, C.P., & Eggersdorfer, M. (2018). Considerations for secondary prevention of nutritional deficiencies in high-risk groups.
- Sobczyńska-Malefora, A., & Delvin, E. (2021). Vitamin B12 status in health and disease: a critical review.
- Suskind, D.L. (2009). Nutritional deficiencies during normal growth.
- Garcia-Casal, M.N., Dary, O., & Jefferds, M.E. (2023). Diagnosing anemia: Challenges selecting methods, addressing underlying causes, and implementing actions at the public health level.
- Stepien, K.M., & Geberhiwot, T. (2019). Challenges in diagnosing and managing adult patients with urea cycle disorders.
- Lan, X., Robin, G., Kasnik, J., Wong, G., & Abdel-Rahman, O. (2023). Challenges in diagnosis and treatment of pancreatic exocrine insufficiency.
- Solomons, N.W. (2000). Plant-based diets are traditional in developing countries: 21st century challenges for better nutrition and health.
- Poddar, A.K. (2024). Nutrition in the New Era: Bridging Cultural Traditions and Modern Health Science in Diet Choices.
- Chowdhury, S.R., & Ray, S. (2024). Micronutrient Deficiency in Indian Diet.
- Almteiri, F. (2024). Clinical Nutrition and Diet Practice in Developing Countries.
- Tontisirin, K., Nantel, G., & Bhattacharjee, L. (2002). Food-based strategies to meet the challenges of micronutrient malnutrition in the developing world.
- Darnton-Hill, I., & Samman, S. (2015). Challenges and opportunities in scaling-up nutrition in healthcare.
- Osendarp, S.J.M., Martinez, H., & Garrett, G.S. (2018). Large-scale food fortification and biofortification in low-and middle-income countries.
- Bezabih, A.M., Wereta, M.H., Kahsay, Z.H., & Getahun, Z. (2018). Demand and supply side barriers limiting the uptake of nutrition services among pregnant women in Ethiopia.
- Ruel, M.T., Garrett, J.L., Morris, S.S., Maxwell, D.G., & Oshaug, A. (1998). Urban challenges to food and nutrition security.
- Tirado, M.C., Cohen, M.J., Aberman, N., & Meerman, J. (2010). Addressing the challenges of climate change and biofuel production for food and nutrition security.
- Ayele, S., Zegeye, E.A., & Nisbett, N. (2020). Multi-sectoral nutrition policy and programme design, coordination, and implementation in Ethiopia.
- Sanghvi, T., Nguyen, P.H., & Tharaney, M. (2022). Gaps in the implementation and uptake of maternal nutrition interventions.
- Delport, C. (2019). Food and nutrition policy in South Africa: the national vision, policy space, and policy alignment.
- Billings, L., Pradeilles, R., & Gillespie, S. (2021). Coherence for nutrition: insights from nutrition-relevant policies and programmes.
- Genc, Y., Humphries, J.M., & Lyons, G.H. (2005). Exploiting genotypic variation in plant nutrient accumulation to alleviate micronutrient deficiency.
- Raiten, D.J., Combs Jr., G.F., Steiber, A.L., & Bremer, A.A. (2021). Nutritional status as a biological variable: integrating nutrition science.
- Reddy, V.S., Palika, R., & Ismail, A. (2018). Nutrigenomics: Opportunities & challenges for public health nutrition.
- Chen, J., Fewtrell, M., Kennedy, G., & Naska, A. (2016). Nutrition challenges ahead.
- Graham, R.D., Welch, R.M., & Bouis, H.E. (2001). Addressing micronutrient malnutrition through enhancing nutritional quality of staple foods.
- Ene-Obong, H., Schönfeldt, H.C., & Campaore, E. (2019). Reliable food composition data generation by nutrition professionals.
- Berti, C., Faber, M., & Smuts, C.M. (2014). Prevention and control of micronutrient deficiencies in developing countries.
- Fanzo, J., Shawar, Y.R., Shyam, T., & Das, S. (2021). Challenges to establish effective public-private partnerships to address malnutrition.
- Allen, S., & De Brauw, A. (2018). Nutrition sensitive value chains: Theory, progress, and open questions.
- Tirado, M.C., Cohen, M.J., Aberman, N., & Meerman, J. (2010). Addressing the challenges of climate change and biofuel production for food and nutrition security.
- Michel, M., Eldridge, A.L., Hartmann, C., & Klassen, P. (2024). Benefits and challenges of food processing in the context of food systems.
- Fanzo, J.C., Downs, S., Marshall, Q.E., & De Pee, S. (2017). Value chain focus on food and nutrition security.
- Heydari, M. (2024). Cultivating sustainable global food supply chains.
- Latham, M.C., Ash, D., Ndossi, G., & Mehansho, H. (2001). Micronutrient dietary supplements: A new fourth approach.
- Beard, J.L. (2000). Effectiveness and strategies of iron supplementation during pregnancy.
- Horwitz, A., Kennedy, E.T., & Howson, C.P. (1998). Prevention of micronutrient deficiencies.
- Alt, M., Bruns, H., & DellaValle, N. (2024). Synergies of interventions to promote pro-environmental behaviors.
- Rao, D., Higgins, C., Margot, H., & Lyle, T. (2016). Micronutrient deficiencies in the developing world.
- Qureshi, N., & Shaikh, B.T. (2006). Myths, fallacies and misconceptions: applying social marketing for promoting appropriate health-seeking behavior.
- Westbury, S., Oyebode, O., & Barber, T.M. (2023). Obesity stigma: causes, consequences, and potential solutions.
- Nayar, U.S., Stangl, A.L., & De Zalduondo, B. (2014). Reducing stigma and discrimination to improve child health and survival.
- Ramírez Ramos, L.M. (2024). Health challenges in African countries: a focus on physical, mental, and emotional well-being.
- Cremers, A.L., de Laat, M.M., Kapata, N., & Gerrets, R. (2015). Assessing the consequences of stigma for tuberculosis patients in urban Zambia.


