- Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries.
- This article compares manual and digital blood pressure devices based on accuracy, ease of use, cost, and user suitability.
- Learn which device best fits your lifestyle—whether you’re a healthcare professional or someone monitoring blood pressure at home.
 Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries, a vital indicator of cardiovascular health. In clinical and home settings, the choice between manual and digital blood pressure devices has become a pivotal aspect of accurate diagnosis and ongoing health monitoring. Manual sphygmomanometers, long considered the gold standard, require training and precision in reading auscultatory sounds with a stethoscope. In contrast, digital blood pressure monitors offer user-friendly automation and quick readings, especially favored for home use and telemedicine applications. However, concerns about calibration, accuracy across different patient populations, and susceptibility to motion artifacts remain prevalent with digital options. Recent comparative studies have evaluated both types in terms of reliability and consistency, noting that while digital devices enhance accessibility and convenience, they may not always match the clinical accuracy of well-operated manual instruments.
Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries, a vital indicator of cardiovascular health. In clinical and home settings, the choice between manual and digital blood pressure devices has become a pivotal aspect of accurate diagnosis and ongoing health monitoring. Manual sphygmomanometers, long considered the gold standard, require training and precision in reading auscultatory sounds with a stethoscope. In contrast, digital blood pressure monitors offer user-friendly automation and quick readings, especially favored for home use and telemedicine applications. However, concerns about calibration, accuracy across different patient populations, and susceptibility to motion artifacts remain prevalent with digital options. Recent comparative studies have evaluated both types in terms of reliability and consistency, noting that while digital devices enhance accessibility and convenience, they may not always match the clinical accuracy of well-operated manual instruments.
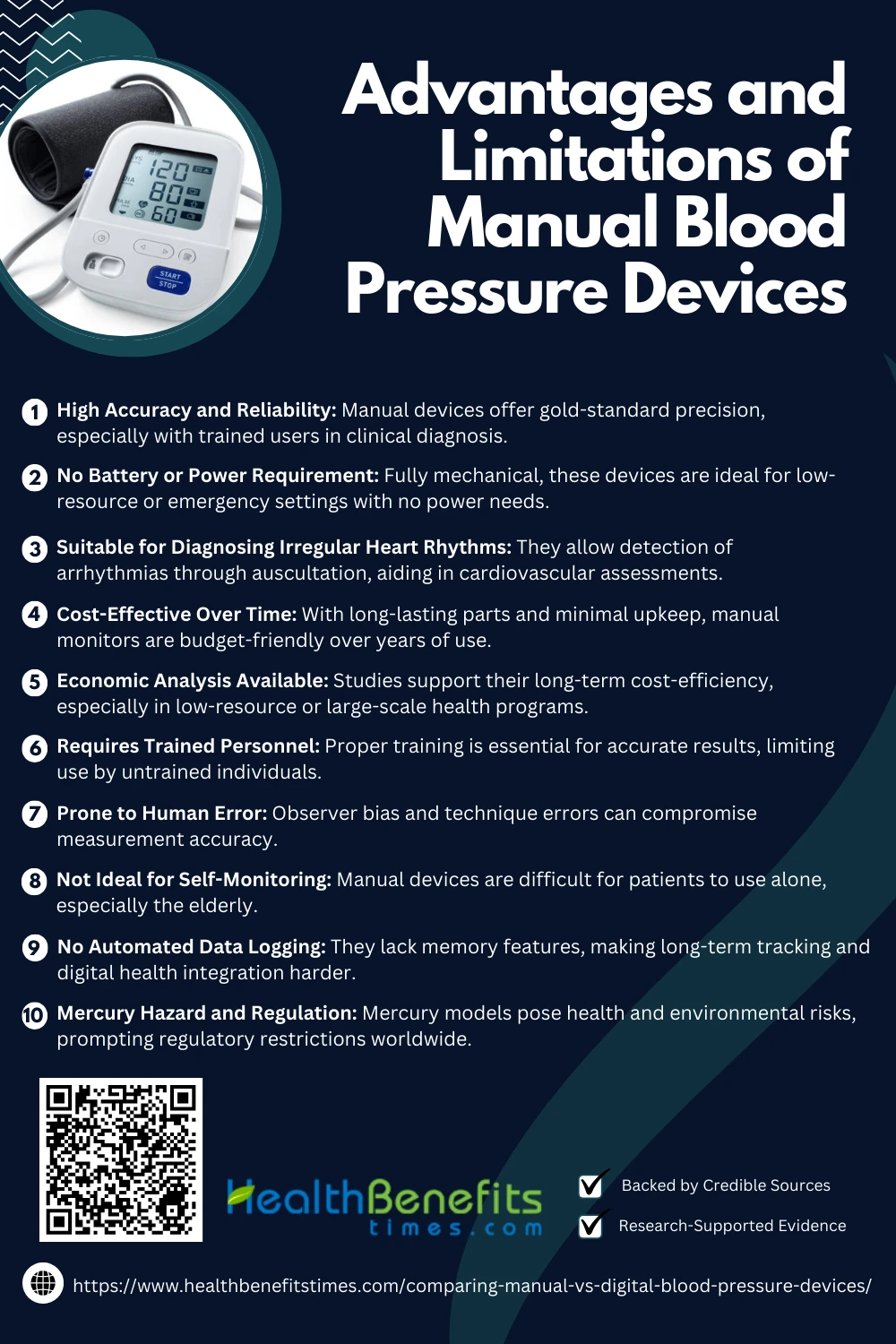
Manual Blood Pressure Devices
Manual blood pressure devices, commonly known as sphygmomanometers, are widely used for their clinical accuracy and reliability in professional settings. These devices depend on auscultation techniques and require trained personnel for accurate readings. (1) Studies confirm their superiority in detecting subtle blood pressure variations.
Types
1. Mercury Sphygmomanometer
The mercury sphygmomanometer is considered the most accurate and reliable manual blood pressure device. It features a column of mercury that rises and falls in response to blood pressure changes during measurement. The healthcare professional inflates the cuff manually and listens for Korotkoff sounds using a stethoscope. Its mechanical simplicity and direct pressure measurement make it a clinical benchmark. However, due to environmental concerns regarding mercury, its use is increasingly restricted in some regions.
2. Aneroid Sphygmomanometer
The aneroid sphygmomanometer operates without mercury and instead uses a spring-based gauge with a dial to show pressure readings. While more portable and environmentally safe than mercury devices, aneroid models are prone to mechanical wear and tear, which can lead to inaccuracies if not regularly calibrated. Proper training is essential to avoid observer errors, but when maintained well, these are effective tools for clinical and home use.
3. Hybrid Sphygmomanometer
The hybrid sphygmomanometer combines the manual inflation and auscultation method of traditional devices with a digital or electronic pressure display. This blend allows it to maintain the diagnostic accuracy of manual readings while minimizing user interpretation errors caused by dial readings. It’s especially useful in modern clinical settings aiming to phase out mercury but retain precision. Hybrid devices are often recommended for settings that require high-frequency monitoring or where multiple users are involved.
Operation Method
The operation of a manual blood pressure device involves wrapping the cuff around the upper arm, inflating it using a rubber bulb, and listening to arterial sounds (Korotkoff sounds) via a stethoscope to determine systolic and diastolic pressures. This auscultatory method is widely regarded for its clinical precision (American Heart Association). Accurate positioning and proper cuff size are essential. (2) Regular calibration ensures reliable results. (3) Training improves user proficiency (BMJ Open). Errors in technique can affect outcomes. (4)
Advantages of Manual blood pressure devices
Manual blood pressure devices offer reliable readings, especially in clinical settings. They are valued for their accuracy, durability, and independence from batteries or power, making them ideal for trained healthcare professionals.
1. High Accuracy and Reliability
Manual blood pressure devices are highly regarded for their accuracy and consistency, especially in clinical diagnosis. Mercury sphygmomanometers, in particular, are considered the gold standard for blood pressure measurement. (5) Their accuracy is essential in diagnosing hypertension and cardiovascular conditions (American Heart Association). Studies have shown manual readings reduce measurement bias (BMJ). Proper training further enhances reliability, and they are often used for device calibration. (3) (4)
2. No Battery or Power Requirement
Manual blood pressure devices are entirely mechanical, making them ideal for use in any setting without reliance on electricity or batteries. (6) Their independence from power sources is especially beneficial in rural or emergency care settings. (2) Unlike digital devices, they continue to function during power outages. (7) This autonomy ensures uninterrupted patient monitoring and supports global health applications. (8)
3. Suitable for Diagnosing Irregular Heart Rhythms
Manual blood pressure devices allow healthcare providers to detect irregular heart rhythms, such as arrhythmias, through auscultation—something automated devices often miss (American Heart Association). Listening to Korotkoff sounds reveals rhythm anomalies that influence accurate systolic and diastolic readings (BMJ). This is crucial for diagnosing atrial fibrillation and similar conditions. (9) Manual measurement ensures consistency even with heart rhythm variability, making it valuable in cardiovascular assessments. (10)
4. Cost-Effective Over Time
Manual sphygmomanometers are durable and low-maintenance, making them cost-effective in long-term clinical and home settings. Unlike digital devices, they do not require battery replacements or frequent servicing. (6) Studies have shown that initial training costs are offset by years of reliable use. (11) Their longevity reduces equipment turnover in resource-limited healthcare systems (BMC Public Health). This sustainability makes them an economical choice, especially for mass hypertension screening programs. (12)
5. Economic analysis available
Economic evaluations of manual blood pressure devices consistently highlight their cost-efficiency and long-term value. Studies show that, despite requiring initial training, they incur lower operational costs compared to digital alternatives (BMC Public Health). Their longevity minimizes equipment replacement needs. (11) Manual devices also reduce dependency on consumables like batteries. (6) This makes them ideal for low-resource settings and large-scale public health programs. (12)
Limitations of Manual blood pressure devices
Manual blood pressure devices, while accurate, have limitations such as requiring training, being harder to use alone, and lacking digital features like memory storage or automatic inflation, affecting user convenience.
1. Requires Trained Personnel
Manual blood pressure measurement requires specific skills in cuff placement, inflation control, and auscultation, making training essential for accuracy. Improper technique can lead to significant errors in diagnosis. (3) Clinical guidelines emphasize the importance of standardized training to ensure consistent and reliable readings.
2. Prone to Human Error
Manual sphygmomanometers are susceptible to human errors such as incorrect cuff size, poor stethoscope positioning, and observer bias. (4) These inaccuracies can affect both systolic and diastolic readings. Distractions, fatigue, or inexperience in clinical settings further increase the likelihood of measurement variability.
3. Not Ideal for Self-Monitoring
Manual blood pressure devices require coordination, proper stethoscope use, and two-hand operation—challenges for patients, especially the elderly (American Heart Association). Without professional assistance, readings may be inaccurate or inconsistent. (9) Home-monitoring guidelines now favor automated digital devices for their ease of use and reliability. (2)
4. No Automated Data Logging
Unlike digital monitors, manual blood pressure devices cannot automatically record or store readings, limiting their utility in long-term tracking or electronic health integration. (13) This lack of data storage complicates trend analysis and remote patient monitoring. (14) Health systems increasingly prefer devices with built-in memory and digital interfaces for streamlined documentation.
5. Mercury Hazard and Regulation
Mercury sphygmomanometers pose environmental and health risks due to mercury toxicity. (15) As a result, many countries are phasing them out in favor of safer alternatives. (16) Regulatory bodies advocate for hybrid or aneroid replacements to reduce hazardous waste and promote sustainable medical practices. (17)
Digital Blood Pressure Devices
Digital blood pressure devices are automated monitors that use oscillometric technology to detect arterial pressure, displaying systolic and diastolic values on a digital screen. They are widely used for home monitoring due to ease of use and accessibility (American Heart Association) and have demonstrated clinical reliability in several studies. (7)
Types of Digital Blood Pressure Devices
Digital blood pressure devices come in various types, including upper arm monitors, wrist monitors, and fingertip models. Each type offers unique features for convenience, ease of use, and portability.
1. Upper Arm Monitors
Upper arm digital blood pressure monitors are the most accurate and widely recommended devices for both clinical and home use. They utilize oscillometric technology and require the cuff to be wrapped around the upper arm, aligning with heart level for reliable readings. Due to their consistency and validation in multiple studies, these devices are endorsed by organizations like the American Heart Association for routine monitoring and hypertension management.
2. Wrist Monitors
Wrist digital monitors offer portability and ease of use, especially for individuals with large arms or mobility issues. However, they are sensitive to wrist positioning and may provide inaccurate results if the arm is not held at heart level. Their accuracy is lower compared to upper arm devices, particularly in elderly patients or those with vascular conditions. (18)
3. Finger Monitors
Finger blood pressure monitors are compact and user-friendly but are generally not recommended for clinical use due to inconsistent accuracy. Factors like finger temperature and improper hand positioning significantly affect results. These devices are best reserved for occasional or informal use rather than serious medical monitoring. (19)
4. Bluetooth-Enabled or Smart Monitors
Smart digital monitors connect to mobile apps or cloud platforms via Bluetooth, allowing users to store and track their readings over time. These devices improve adherence to monitoring schedules and enable better communication between patients and healthcare providers. Research has shown their effectiveness in chronic disease management and digital health integration. (14)
5. Ambulatory Blood Pressure Monitors (ABPM)
ABPM devices are worn continuously for 24 hours to monitor blood pressure during daily activities and sleep. They are essential for diagnosing white-coat hypertension and evaluating nocturnal blood pressure patterns. Clinical studies emphasize their superior predictive value for cardiovascular outcomes compared to single-office readings. (20)
Operation Method
Digital blood pressure devices operate using oscillometric technology, which detects arterial wall vibrations during cuff inflation and deflation to determine systolic and diastolic pressures (American Heart Association). Users place the cuff on the upper arm or wrist, press a button, and view results on a digital screen. (2) Proper cuff positioning is crucial for accuracy. (7) Many models offer features like automatic inflation (BMJ) and Bluetooth syncing for data tracking. (13)
Advantages of Digital blood pressure devices
Digital blood pressure devices offer several advantages, including ease of use, quick automatic readings, memory storage, and portability. They’re ideal for home monitoring, especially for seniors and individuals with limited training.
Digital blood pressure monitors are designed for simple, user-friendly operation, making them ideal for self-monitoring, especially among the elderly and individuals with no medical training. With one-touch functionality and automated cuff inflation, they minimize the chance of user error. (2) Their intuitive design supports routine use, improving patient adherence to hypertension management. (7)
2. Quick and Automated Readings
One of the main advantages of digital blood pressure devices is their speed and automation. With automated inflation, deflation, and real-time digital display, they provide rapid, accurate readings in under a minute. (13) This efficiency supports daily monitoring routines and telehealth services. Patients benefit from immediate feedback, which enhances engagement and supports early detection of blood pressure anomalies. (14)
3. Ideal for Self-Monitoring
Digital blood pressure monitors are particularly well-suited for home and self-monitoring, allowing patients to manage their condition independently without clinical visits. Their automated function and minimal training requirement empower users, especially older adults and those managing chronic hypertension. (2) These devices support early detection and routine monitoring, leading to improved treatment adherence and better health outcomes. (3)
4. Data Storage and Tracking
Many digital blood pressure monitors feature built-in memory or Bluetooth connectivity, enabling automatic storage of readings for trend analysis over time. This function enhances clinical decision-making and supports remote patient monitoring. (13) Integration with mobile apps or cloud systems allows users and doctors to track fluctuations and adjust treatment plans accordingly, improving long-term hypertension control. (14)
5. Portable and Battery Operated
Digital blood pressure monitors are designed to be lightweight, compact, and battery-powered, making them highly portable for use at home or while traveling. (19) Their cordless operation eliminates dependence on wall power, offering flexibility in remote or rural settings. (2) This mobility supports consistent blood pressure monitoring across diverse environments, improving patient compliance and facilitating care continuity in community health programs. (7)
Limitations of Digital blood pressure devices
Digital blood pressure devices, while convenient, have limitations such as potential inaccuracies, dependence on batteries, sensitivity to movement, and higher costs. Readings may vary based on cuff position and device quality.
1. Less Accurate in Some Cases
Digital blood pressure monitors can show reduced accuracy in patients with arrhythmias, arterial stiffness, or during movement. (4) These conditions interfere with oscillometric readings, leading to inconsistent measurements. (9) Manual methods remain preferred in such clinical scenarios for their diagnostic reliability.
2. Position Sensitivity
Wrist and finger digital monitors are highly sensitive to arm positioning, requiring precise placement at heart level for accurate results. (18) Improper posture or cuff misalignment can significantly skew readings. (2) Guidelines emphasize body and cuff positioning as critical to accurate home monitoring.
3. Calibration and Maintenance Needs
Digital monitors require periodic calibration to maintain measurement accuracy, especially after extended use. (11) Unlike manual devices, their internal sensors can drift over time (BMJ Open). Regular professional servicing ensures reliability, particularly in clinical environments. (4)
4. Battery Dependency
Battery dependency limits digital blood pressure monitors during prolonged use or in emergencies without replacements. (19) Devices may shut down or lose accuracy as battery levels drop. (2) Rechargeable models exist but still require consistent power access for functionality.
5. Higher Initial Cost
Digital blood pressure monitors generally come with a higher upfront cost compared to manual models, especially those with advanced features like Bluetooth and memory storage. Their added convenience and automation justify the price for many users, though cost remains a barrier in low-resource settings. (11)
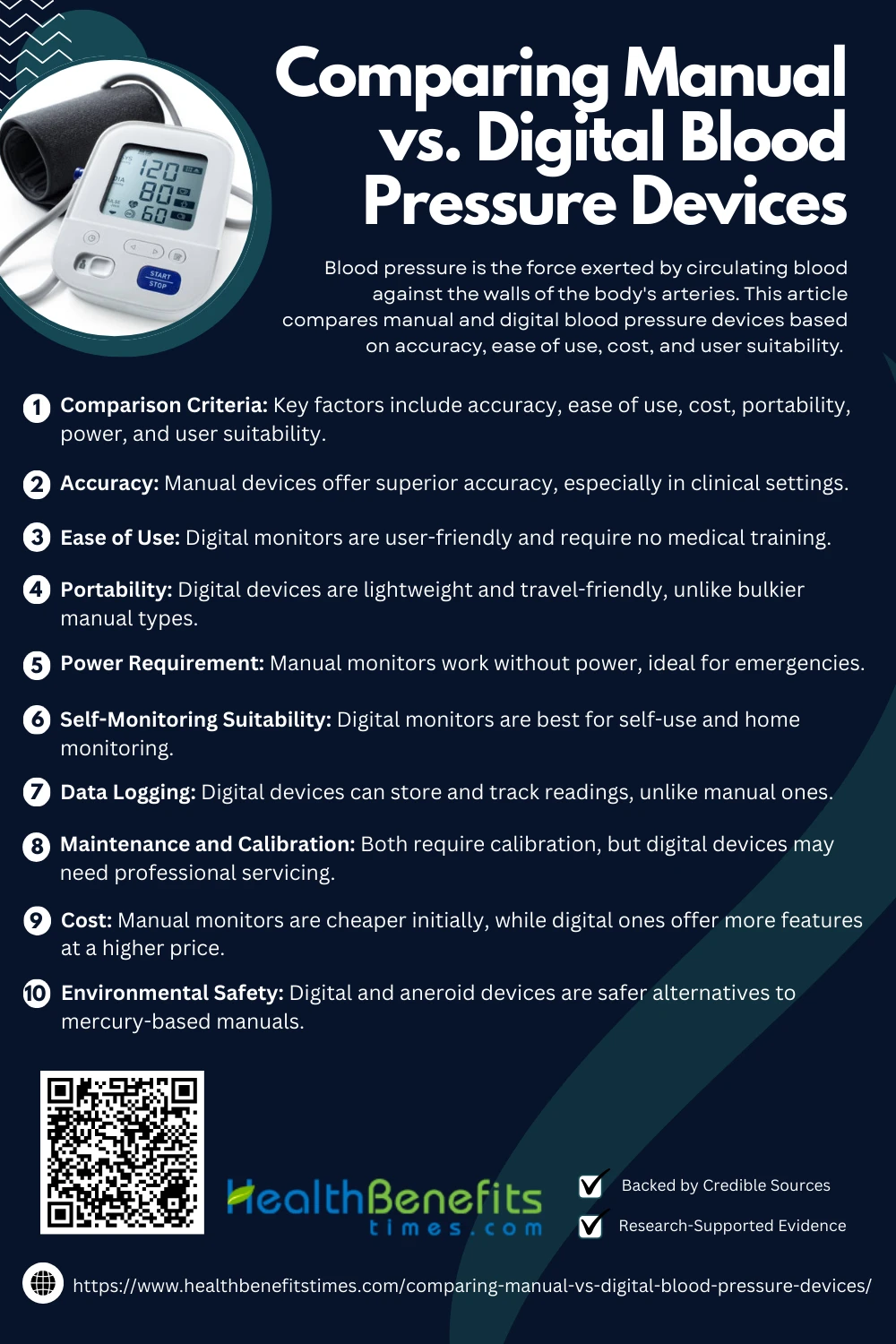
Comparison Criteria
When comparing manual and digital blood pressure devices, key criteria include accuracy, ease of use, cost, portability, maintenance, and suitability for different users in clinical or home settings.
Manual blood pressure devices—particularly mercury sphygmomanometers—are considered the gold standard for clinical accuracy due to their direct measurement and auscultatory method. In contrast, digital monitors use oscillometric techniques, which can be less precise in certain populations, such as patients with arrhythmias or vascular stiffness. (4) While newer digital models have improved, manual devices still offer greater consistency in critical care scenarios.
2. Ease of Use
Digital monitors are designed for effortless, one-touch operation, making them ideal for the general public, including elderly users. Their automated inflation and display features require no medical training. On the other hand, manual devices demand technical skill and training in auscultation to obtain accurate results, limiting their usability in non-clinical settings.
3. Portability
Digital blood pressure devices are typically lightweight and battery-powered, making them easy to carry and ideal for remote or travel use. Manual monitors, especially mercury-based ones, are bulkier and require additional components like a stethoscope, limiting their mobility and convenience. (19)
4. Power Requirement
Manual devices are completely mechanical and function without electricity or batteries, making them reliable in low-resource or emergency settings. In contrast, digital monitors rely on batteries or external power sources, making them vulnerable to interruptions when power or replacements are unavailable. (2)
5. Self-Monitoring Suitability
Digital monitors are optimized for self-use, allowing patients to take readings without assistance—an essential feature for home blood pressure management. Manual devices, however, are not practical for self-monitoring as they require two-handed coordination, auscultation skills, and proper positioning, which may be difficult for many patients. (7)
6. Data Logging
Most modern digital blood pressure monitors feature memory storage, Bluetooth connectivity, or mobile app integration. This allows for tracking of readings over time, making it easier for patients and healthcare providers to monitor trends and adjust treatments. Manual devices lack any such feature and rely on handwritten logs. (13)
7. Maintenance and Calibration
Manual devices generally require little maintenance but must be periodically calibrated and cleaned, especially in high-use environments. Digital monitors, while low-maintenance for users, may require professional recalibration and servicing over time to maintain accuracy.
8. Cost
Manual blood pressure monitors are usually more affordable upfront, making them attractive for clinics and individuals with budget constraints. However, digital monitors—especially those with advanced features—tend to have higher initial costs. Over time, the convenience and additional features may offset the price difference for some users.
9. Environmental Safety
Mercury-based manual devices pose serious environmental and health hazards due to mercury toxicity. Many countries have implemented bans or restrictions on their use. In contrast, aneroid manual and digital devices are mercury-free and considered environmentally safer alternatives. (15)
Practical Considerations for Device Selection
Choosing the right blood pressure device involves practical considerations like user skill level, budget, monitoring frequency, environment (home or clinic), and health needs to ensure accurate, convenient, and reliable readings.
The choice of device heavily depends on who will be using it. Manual blood pressure monitors require trained healthcare professionals who are proficient in using a stethoscope and identifying Korotkoff sounds. These are ideal for clinical environments where expertise is guaranteed. In contrast, digital monitors are perfect for untrained users due to their one-button functionality and automated readings, significantly reducing the chance of operator error.
2. Patient Population
Certain patient groups, such as the elderly, individuals with disabilities, or those suffering from arrhythmias, may struggle with manual devices and benefit more from digital models. Advanced digital monitors can detect irregular heartbeats and adapt to movement, offering consistent results. Manual devices, although more accurate in ideal conditions, may not perform well without patient cooperation or proper posture. (9)
3. Setting of Use
The environment where the device will be used plays a significant role in selection. Manual devices are excellent in rural or low-resource settings because they do not require electricity or batteries. On the other hand, digital devices are better suited for modern clinics, hospitals, and home environments where reliable power is available and ease of use is a priority (CDC). (2)
4. Frequency of Monitoring
If frequent or daily monitoring is required, digital monitors are far more convenient. Their quick operation and minimal skill requirement make them ideal for routine home use. Manual devices, while accurate, are more time-consuming and better suited for periodic assessments conducted by trained professionals (PubMed). (14)
5. Budget Constraints
Cost considerations are critical, especially in large-scale public health deployments or low-income households. Manual devices generally have a lower upfront cost and can last many years with basic maintenance. However, digital devices offer features like memory storage and remote data syncing, which may provide better long-term value, particularly for patients with chronic conditions.
6. Need for Data Storage and Remote Sharing
In cases where tracking blood pressure trends or sharing data with healthcare providers is important, digital devices offer a distinct advantage. Many models come equipped with Bluetooth or app integrations that automatically store readings and allow for cloud-based sharing. Manual devices require users to write down results manually, which increases the chance of data loss or errors. (13)
7. Maintenance and Durability
Manual sphygmomanometers are generally more durable and require less frequent calibration, but they must be cleaned and maintained regularly to remain accurate. Digital devices are easier to use and maintain on a day-to-day basis, though they may need periodic recalibration and battery replacements, especially with heavy usage. (11)
8. Regulatory and Environmental Compliance
With increasing global efforts to eliminate mercury from medical devices, traditional mercury-based sphygmomanometers are being phased out. This has led to greater adoption of aneroid and digital devices that meet modern regulatory and environmental standards. Health systems should consider environmental impact and legal compliance when choosing equipment. (15)
Who Should Use Which?
Determining who should use manual or digital blood pressure devices depends on user expertise, health conditions, and monitoring needs, helping ensure the most accurate and convenient option is chosen.
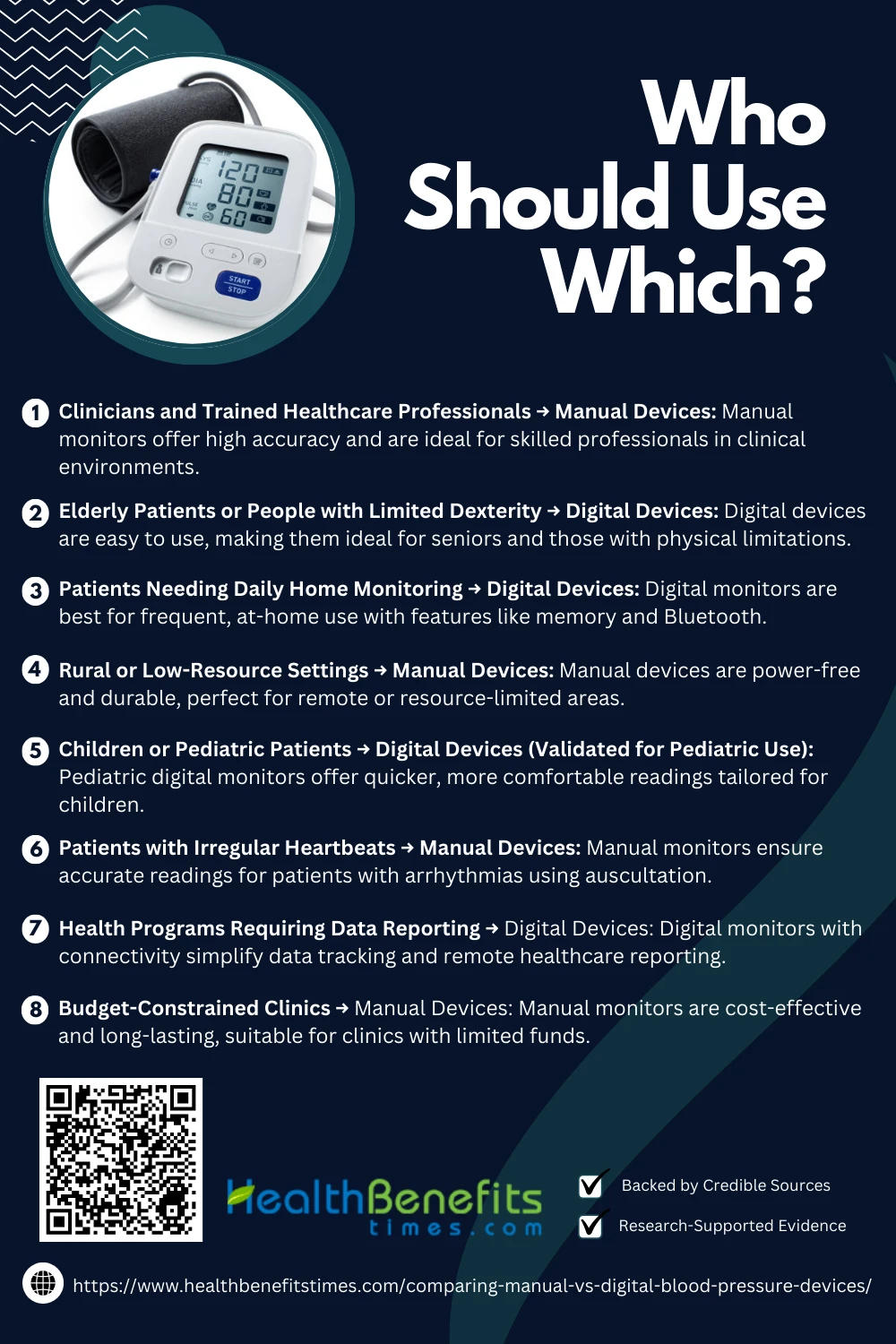 1. Clinicians and Trained Healthcare Professionals → Manual Devices
1. Clinicians and Trained Healthcare Professionals → Manual Devices
Manual blood pressure monitors, particularly mercury and aneroid types, are best suited for use by trained medical professionals. In clinical settings, they provide highly accurate readings and are preferred for diagnosing conditions like hypertension or arrhythmias. Professionals are equipped with the skills needed to interpret Korotkoff sounds, inflate the cuff manually, and ensure correct cuff placement—elements that contribute to precise measurements. (4)
2. Elderly Patients or People with Limited Dexterity → Digital Devices
Digital monitors are ideal for elderly users or those with reduced hand strength, arthritis, or cognitive impairments. These devices require minimal interaction—just the press of a button—eliminating the physical challenges associated with manual inflation and stethoscope use. Their large display screens and automated readings simplify the process, making self-monitoring more accessible.
3. Patients Needing Daily Home Monitoring → Digital Devices
For patients managing chronic hypertension or other cardiovascular conditions, digital blood pressure monitors are highly practical for regular use. They allow for quick, frequent readings and often include memory storage or Bluetooth features to track changes over time. This supports better treatment adherence and enables healthcare providers to monitor trends remotely. (2)
4. Rural or Low-Resource Settings → Manual Devices
Manual blood pressure devices are ideal for rural health clinics and field settings where electricity or battery supply may be unreliable. They require no power source and are durable, making them perfect for consistent use in remote or emergency environments. Their long lifespan and independence from consumables like batteries make them cost-effective and sustainable. (6)
5. Children or Pediatric Patients → Digital Devices (Validated for Pediatric Use)
Digital monitors designed specifically for children are more comfortable and less intimidating than manual setups. They deliver faster readings, which reduces the time a child has to stay still—an important factor in pediatric care. Pediatric digital devices come with appropriately sized cuffs, making them both effective and user-friendly for caregivers and clinicians. (7)
6. Patients with Irregular Heartbeats → Manual Devices
In cases of arrhythmia or other irregular heart rhythms, digital devices often produce inaccurate or inconsistent readings because their oscillometric algorithm can misinterpret abnormal pulsations. Manual devices, which use auscultation, allow a trained professional to accurately detect and assess these variations, ensuring better diagnostic reliability in such cases. (9)
7. Health Programs Requiring Data Reporting → Digital Devices
For telemedicine, community health initiatives, or clinical trials that involve tracking and sharing patient data, digital monitors with data storage and connectivity features are ideal. These devices streamline the reporting process, reduce human error in record-keeping, and allow for real-time transmission of readings to centralized health systems. (13)
8. Budget-Constrained Clinics → Manual Devices
Manual blood pressure monitors are typically more affordable and durable than digital options, making them a good fit for budget-limited clinics. Though they require trained staff, their long-term cost efficiency, lack of dependency on batteries, and minimal need for technological support make them a practical investment in many healthcare environments.
Conclusion
In conclusion, both manual and digital blood pressure devices have their own strengths and limitations. Manual monitors are known for their accuracy and are ideal for trained professionals in clinical settings. On the other hand, digital devices offer greater convenience, ease of use, and helpful features like automatic readings and memory storage, making them suitable for home monitoring and everyday users. The best choice depends on individual needs, lifestyle, and level of comfort with technology. By understanding the differences and evaluating key factors like accuracy, cost, and usability, you can make an informed decision that supports better heart health.