Insomnia is broadly defined as a sleep disorder characterized by difficulties in falling asleep, maintaining sleep, or experiencing non-restorative sleep, which leads to significant daytime impairments such as fatigue, attention deficits, and mood instability. It can be acute, intermittent, or chronic, with chronic insomnia persisting for at least three months. Insomnia can occur as a primary disorder or as a symptom of other medical, neurological, or psychiatric conditions. The disorder is recognized in major diagnostic systems, including the DSM-5 and the International Classification of Sleep Disorders, and is associated with substantial health-care costs and risks for developing other health issues. Despite its high prevalence, the pathophysiology of insomnia is not fully understood, though hyperarousal and genetic factors are implicated. Treatment typically involves cognitive behavioral therapy and, in some cases, pharmacological interventions.
Insomnia is broadly defined as a sleep disorder characterized by difficulties in falling asleep, maintaining sleep, or experiencing non-restorative sleep, which leads to significant daytime impairments such as fatigue, attention deficits, and mood instability. It can be acute, intermittent, or chronic, with chronic insomnia persisting for at least three months. Insomnia can occur as a primary disorder or as a symptom of other medical, neurological, or psychiatric conditions. The disorder is recognized in major diagnostic systems, including the DSM-5 and the International Classification of Sleep Disorders, and is associated with substantial health-care costs and risks for developing other health issues. Despite its high prevalence, the pathophysiology of insomnia is not fully understood, though hyperarousal and genetic factors are implicated. Treatment typically involves cognitive behavioral therapy and, in some cases, pharmacological interventions.
Types of Insomnia
Insomnia, a common sleep disorder, can vary in its duration, cause, and symptoms. Understanding the different types of insomnia can help in identifying the most effective treatment options. Here’s a brief look at the primary categories of insomnia and what sets them apart:
- Acute (short-term) insomnia
- Chronic (long-term) insomnia
- Primary insomnia
- Secondary (comorbid) insomnia
- Onset insomnia
- Maintenance insomnia
- Terminal (early morning awakening) insomnia
- Mixed insomnia
- Behavioral insomnia of childhood (BIC)
- Paradoxical insomnia
Common Causes of Insomnia
Insomnia can be triggered by a variety of factors, from lifestyle choices to underlying health conditions. Identifying the root cause is essential for finding effective treatments and improving sleep quality. Here’s a look at some of the most common causes of insomnia that might be keeping you awake at night:
- Stress and anxiety
- Depression and other mental health disorders
- Irregular sleep schedule
- Poor sleep habits
- Chronic pain or discomfort
- Medical conditions (e.g., sleep apnea, restless leg syndrome, GERD)
- Medications (e.g., antidepressants, blood pressure medications)
- Caffeine, nicotine, and alcohol consumption
- Environmental factors (noise, light, temperature)
- Jet lag or shift work
- Hormonal changes (e.g., menopause, pregnancy)
- Aging
- Neurological disorders (e.g., Alzheimer’s, Parkinson’s)
- Excessive screen time before bed
- Lack of physical activity
- Overactive mind or racing thoughts
- Traumatic experiences or PTSD
- Certain foods or large meals before bedtime
- Genetics or family history of insomnia
- Chronic stress or long-term anxiety
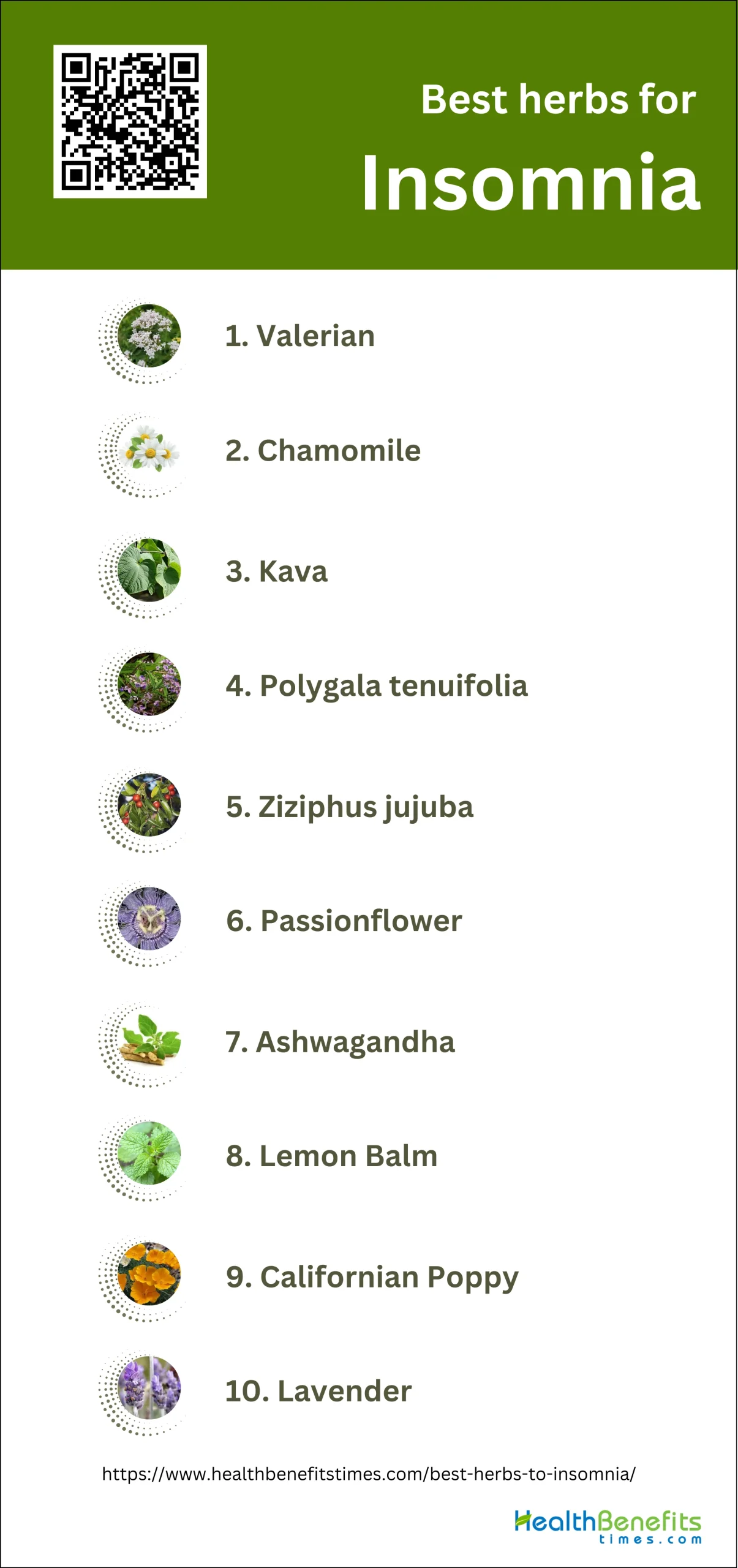
Best herbs to Insomnia
Using herbs to care for insomnia instead of conventional medication offers several advantages, primarily due to the reduced risk of adverse effects and dependency. Conventional medications, such as benzodiazepines and antihistamines, are effective for sleep induction but often lead to tolerance, dependence, and other side effects with prolonged use. In contrast, herbal remedies, which have been used for centuries, are generally associated with fewer side effects and lower risk of dependency. Herbs like valerian, chamomile, and passionflower have shown potential in improving sleep quality by interacting with neurotransmitter systems, particularly the GABAergic system, which is crucial for sleep regulation. Additionally, herbal treatments are often more cost-effective and accessible, making them a viable alternative for many individuals. While more research is needed to fully understand their mechanisms and efficacy, the current evidence supports the use of herbal medicine as a safer and effective alternative for managing insomnia.
1. Valerian
Valerian root has shown promise as a natural remedy for insomnia. Research suggests that valerian may help reduce the time it takes to fall asleep and improve overall sleep quality. The herb contains compounds that interact with GABA receptors in the brain, potentially promoting relaxation and sedation. Studies have found that taking valerian supplements, typically in doses of 300-600 mg before bedtime, may lead to faster sleep onset, better sleep quality, and increased time spent in deep sleep stages. However, it’s important to note that while many studies show positive effects, some research results are inconclusive, and larger, more rigorous studies are needed to fully establish valerian’s efficacy for insomnia. Despite this, valerian is generally considered a safer alternative to prescription sleep medications, with fewer side effects reported.
What Research Says?
- Based on research carried out by Sleep Medicine, The American Journal of Medicine and Sleep Medicine, Multiple systematic reviews and meta-analyses have found the evidence for valerian’s effectiveness in treating insomnia to be inconclusive due to methodological inconsistencies and varying study designs.
- As per studies undertaken by Sleep, PLoS One and Planta Medica, Some studies suggest that valerian may offer modest improvements in subjective sleep quality and sleep latency, but these findings often lack statistical significance and are not consistently replicated across studies.
- According to studies performed by Sleep Medicine Reviews, Valerian is generally considered safe with few adverse effects reported. Most studies agree that valerian does not produce significant side effects or rebound insomnia upon discontinuation.
- Research undertaken by Journal of Traditional and Complementary Medicine reveals studies involving valerian in combination with other herbs, such as hops or Eschscholtzia californica, have shown some promise in improving sleep quality and reducing anxiety, though these findings are also modest and require further investigation.
- Findings from research done by Complementary Therapies in Medicine show polysomnographic studies and other objective measurements often do not show significant improvements in sleep parameters with valerian use, indicating that subjective improvements may not translate to measurable changes in sleep architecture.
How to Use
To use valerian for insomnia, take 300-600 mg of valerian root extract 30 minutes to two hours before bedtime. For best results, use it consistently for at least two weeks. Alternatively, steep 2-3 grams of dried valerian root in hot water for 10-15 minutes to make a tea. Start with a lower dose and gradually increase if needed. Valerian is generally considered safe, but consult your doctor before use, especially if you’re taking other medications or have ongoing sleep issues.
Potential side effects of Valerian
While generally considered safe, valerian may cause mild side effects such as headache, dizziness, stomach upset, and drowsiness. Some users report vivid dreams or mental fogginess. Rare cases of liver toxicity have been reported. Long-term use may lead to withdrawal symptoms when discontinued abruptly. It’s advisable to start with a low dose and monitor for any adverse reactions.
Who should avoid Valerian
Pregnant or breastfeeding women should avoid valerian due to insufficient safety data. Children under 3 years old should not use it. People with liver disease, epilepsy, or scheduled for surgery should consult their doctor before use. Those with depression or at risk of suicide should exercise caution, as valerian may worsen symptoms in some cases.
Interaction with medications
Valerian can interact with various medications, potentially increasing sedative effects. It may enhance the effects of sleep aids, anti-anxiety drugs, and antidepressants. Caution is advised when combining valerian with anticonvulsants, statins, or certain antifungal drugs. It may also interfere with anesthesia, so inform your healthcare provider before surgery if you’re taking valerian regularly.
2. Chamomile
Chamomile has long been recognized as a natural remedy for insomnia and sleep-related issues. This gentle herb contains apigenin, an antioxidant that binds to specific receptors in the brain, potentially inducing sleepiness and reducing anxiety. Studies have shown that chamomile can improve sleep quality, reduce the time it takes to fall asleep, and decrease nighttime awakenings. Regular consumption of chamomile tea before bedtime may help establish a relaxing pre-sleep routine, signaling to the body that it’s time to wind down. Additionally, chamomile’s mild sedative effects can help calm an overactive mind, making it easier to transition into sleep.
What Research Says?
- As research performed by Phytotherapy Research and Complementary Therapies in Medicine suggests Chamomile has been shown to significantly improve sleep quality in elderly people and in general populations, suggesting it can be a safe modality for promoting better sleep.
- Research completed by BMC Complementary Medicine and Therapies and Sleep Medicine Reviews indicates there is limited evidence to support chamomile’s effectiveness in reducing insomnia severity. One study found no significant change in insomnia severity index after chamomile treatment.
- Chamomile is generally considered safe with mild adverse events reported in a few studies. No significant adverse effects on liver enzymes, blood urea, or serum creatinine were observed.
How to Use
To use chamomile for insomnia, steep 1-2 teaspoons of dried chamomile flowers in a cup of hot water for 5-10 minutes, creating a soothing tea. Drink this 30-45 minutes before bedtime. For convenience, pre-made chamomile tea bags are widely available. Alternatively, chamomile supplements in capsule form can be taken, typically 400-1600 mg daily. Some people find chamomile essential oil beneficial when used in a diffuser or added to a warm bath before sleep. Consistency is key for best results.
Potential side effects of Chamomile
While generally considered safe, chamomile can cause mild side effects in some people. These may include nausea, dizziness, and allergic reactions such as skin rashes or itching. In rare cases, severe allergic reactions (anaphylaxis) have occurred. Some individuals may experience drowsiness, especially when consuming large amounts. Chamomile can also cause eye irritation if applied near the eyes.
Who should avoid Chamomile
Pregnant women should avoid chamomile due to potential risks of miscarriage or preterm labor. People with allergies to plants in the Asteraceae family (ragweed, chrysanthemums, daisies) should also avoid it due to possible cross-reactivity. Infants and young children should not consume chamomile tea due to the risk of botulism spores. Those with hormone-sensitive conditions should use caution, as chamomile may have mild estrogenic effects.
Interaction with medications
Chamomile can interact with various medications, potentially increasing their effects or altering their metabolism. It may enhance the sedative effects of medications like benzodiazepines or antihistamines. Chamomile can also interact with blood thinners like warfarin, increasing the risk of bleeding. It may interfere with the absorption of iron and other minerals. Always consult a healthcare provider before using chamomile alongside any medications.
3. Kava

Kava has shown promise as a natural remedy for insomnia, particularly for sleep disturbances associated with anxiety and stress. Research suggests that kava may help reduce the time it takes to fall asleep, improve overall sleep quality, and increase the duration of sleep. The active compounds in kava, known as kavalactones, interact with the brain’s GABAergic system, promoting relaxation and sedation without the risk of dependency associated with many pharmaceutical sleep aids. Studies have demonstrated kava’s ability to significantly reduce total stress and insomnia, with one clinical trial finding statistically significant improvements in sleep quality and recuperative effects after sleep. Additionally, kava has been found to increase delta activity during non-REM sleep, indicating a potential sleep quality-enhancement effect.
What Research Says?
- According to investigations conducted by Phytotherapy Research and Human Psychopharmacology: Clinical and Experimental, Kava has shown significant improvements in sleep parameters such as time to fall asleep, hours slept, and waking mood in patients with stress-induced insomnia.
- Research efforts by Psychopharmacology show that in sleep-disturbed rats, kava extract significantly shortened sleep latency and increased delta activity during non-REM sleep, indicating improved sleep quality.
- Research initiated by Medicine and Sleep Medicine Reviews suggests some studies found no significant difference between kava and placebo in improving insomnia symptoms, suggesting that kava may not be more effective than a placebo in some cases.
- As demonstrated by research from Journal of Psychopharmacology and Journal of Psychosocial Nursing and Mental Health Services, Kava has been associated with hepatotoxicity, leading to its ban in some countries, but it is still marketed as a safe dietary supplement in others.
How to Use
To use kava for insomnia, start with a low dose of 70-250 mg of kavalactones, taken 30-60 minutes before bedtime. Choose a high-quality, noble kava extract or tea from reputable sources. Prepare kava tea by steeping 2-4 tablespoons of kava root powder in warm water for 10-15 minutes, then strain. Alternatively, use a standardized kava extract in capsule or liquid form. Begin with the lowest effective dose and gradually increase if needed. Always consult a healthcare professional before using kava, especially if you have liver issues or take medications.
Potential side effects of Kava
Common side effects of kava include drowsiness, dizziness, headache, and gastrointestinal discomfort. More serious concerns involve potential liver toxicity, with rare cases of severe liver damage reported. Long-term use may lead to skin changes (kava dermopathy), cognitive impairments, and nutritional deficiencies. Some users experience nausea, motor reflex impairment, and visual disturbances. Excessive consumption can result in addiction and withdrawal symptoms.
Who should avoid Kava
Pregnant or breastfeeding women should avoid kava due to potential risks to the fetus or infant. Individuals with liver disease, Parkinson’s disease, or depression should not use kava as it may worsen these conditions. People with kidney problems, blood disorders, or scheduled for surgery should also avoid kava. Children and those with a history of alcohol abuse should refrain from using kava.
Interaction with medications
Kava can interact with various medications, potentially increasing sedative effects when combined with alcohol, benzodiazepines, or barbiturates. It may interfere with the effectiveness of Parkinson’s medications like levodopa. Kava can enhance the effects of antipsychotics and anticonvulsants. It may also interact with drugs metabolized by liver enzymes, potentially altering their effectiveness or increasing side effects. Always consult a healthcare provider before combining kava with any medications.
4. Polygala tenuifolia
Polygala tenuifolia has shown promising potential as a natural remedy for insomnia. Research indicates that this herb can improve sleep quality and duration through multiple mechanisms. The active component senegenin in Polygala tenuifolia has been found to increase levels of GABA and acetylcholine in brain regions associated with sleep, mimicking natural sleep patterns. Studies have demonstrated that Polygala tenuifolia can increase both non-rapid eye movement (NREM) and rapid eye movement (REM) sleep, shorten sleep induction time, and enhance the quality of sleep by increasing theta waves, delta waves, and k complex formations in EEG readings. Additionally, Polygala tenuifolia has been shown to reduce anxiety and stress, which are often underlying causes of insomnia.
What Research Says?
- According to the research carried out by Chinese Journal of Integrative Medicine, Polygala tenuifolia (PT) has shown sedative and hypnotic effects in aged insomnia rats, improving memory and prolonging sleep time induced by pentobarbital. It also increased neurotransmitter levels of 5-HT and GABA while decreasing Glu levels in the hippocampus, suggesting its role in GABAergic signaling pathways.
- Studies conducted by Biological and Pharmaceutical Bulletin and Pharmaceutical Biology indicate PT and its constituents, such as tenuifoliside B, have demonstrated cognitive improvement and cerebral protective effects, which may indirectly benefit insomnia by enhancing overall brain health and function.
- Research executed by Regulatory Toxicology and Pharmacology and Molecules reveals Historically, PT has been used to treat insomnia, amnesia, and other cognitive dysfunctions. Modern studies confirm its wide-ranging pharmacological activities, including neuroprotective, antidepressant, and hypnotic-sedative effects.
- As shown by research done by Evidence-Based Complementary and Alternative Medicine and Fitoterapia, the root extract of PT has been evaluated for genotoxicity and found to be non-genotoxic at proper doses. However, raw PT can be toxic and must be processed to reduce gastrointestinal irritation and other side effects.
How to Use
To use Polygala tenuifolia for insomnia, take 100-200 mg of a standardized extract 30-60 minutes before bedtime. Start with the lower dose and increase if needed. Alternatively, prepare a tea by steeping 3-5 grams of dried Polygala root in hot water for 10-15 minutes. For enhanced effects, some users take it sublingually. Consistency is key, so use it regularly for at least 2-3 weeks. As always, consult a healthcare professional before starting any new supplement regimen, especially if you have existing health conditions or take medications.
Potential side effects of Polygala tenuifolia
While generally considered safe, Polygala tenuifolia may cause gastrointestinal side effects in some individuals. These can include nausea, vomiting, diarrhea, and mild indigestion. Some users report experiencing headaches or dizziness. In rare cases, there have been concerns about potential liver toxicity with long-term use. As with any supplement, it’s advisable to start with a low dose and monitor for any adverse reactions.
Who should avoid Polygala tenuifolia
Pregnant or breastfeeding women should avoid Polygala tenuifolia due to insufficient safety data. Individuals with liver disease or a history of liver problems should consult a healthcare professional before use. Those with gastrointestinal sensitivities may want to exercise caution. People scheduled for surgery should discontinue use at least two weeks prior, as it may interact with anesthesia.
Interaction with medications
Polygala tenuifolia may interact with various medications, potentially altering their effectiveness or increasing side effects. It may enhance the effects of sedatives, antidepressants, and anti-anxiety medications. There’s a potential for interaction with drugs metabolized by liver enzymes. Those taking any prescription medications, especially for neurological or psychiatric conditions, should consult their healthcare provider before using Polygala tenuifolia.
5. Ziziphus jujuba

Ziziphus jujuba, commonly known as jujube or Chinese date, has shown promising potential as a natural remedy for insomnia. Research indicates that jujube contains several bioactive compounds, including flavonoids, saponins, and alkaloids, which contribute to its sedative and hypnotic effects. Studies have demonstrated that jujube extracts can reduce sleep latency, increase total sleep time, and improve overall sleep quality. The active components, such as jujuboside A and spinosin, have been found to modulate the GABAergic system, enhancing the effects of sleep-inducing neurotransmitters. Additionally, jujube has been shown to increase levels of serotonin and other neurotransmitters associated with sleep regulation. Traditional use of jujube for insomnia dates back thousands of years in Chinese medicine, and modern research is now providing scientific evidence to support these historical claims.
What Research Says?
- Research organized by Phytomedicine and Journal of Ethnopharmacology suggests Ziziphus jujuba seeds (Semen Ziziphi Spinosae) have been shown to possess significant sedative and hypnotic effects, which are attributed to their secondary metabolites that modulate GABAergic and serotonergic systems.
- Findings from studies performed by Foods and Foods indicate the sleep-promoting effects of Ziziphus jujuba are linked to the modulation of GABA receptors. Fermented extracts of jujube seeds with high GABA content have been shown to increase non-rapid eye movement (NREM) sleep and decrease sleep latency in rodent models.
- Research performed by Processes shows the extracts also exhibit neuromodulatory effects by reducing orexin A gene expression and serotonin levels in the hypothalamus, which are crucial for wakefulness.
- According to the findings from research conducted by Processes, the extracts also exhibit neuromodulatory effects by reducing orexin A gene expression and serotonin levels in the hypothalamus, which are crucial for wakefulness.
How to Use
To use Ziziphus jujuba for insomnia, consume 250-500 mg of standardized extract 30-60 minutes before bedtime. Alternatively, prepare a tea by steeping 2-3 grams of dried jujube fruit or seeds in hot water for 10-15 minutes. For a more potent effect, some studies have used doses up to 1000 mg. Start with a lower dose and increase gradually if needed. Jujube can also be taken as a tincture or in capsule form. As with any supplement, consult a healthcare professional before use, especially if you have existing health conditions or take medications.
Potential side effects of Ziziphus jujuba
While generally considered safe, Ziziphus jujuba may cause side effects in some individuals. These can include drowsiness, dizziness, and gastrointestinal discomfort such as nausea, vomiting, and diarrhea. In rare cases, it may lead to allergic reactions. Excessive consumption can have a laxative effect. Some users report headaches or cognitive impairment, especially when taken in large doses or for prolonged periods.
Who should avoid Ziziphus jujuba
Pregnant and breastfeeding women should avoid Ziziphus jujuba due to insufficient safety data. Individuals with liver disease or a history of liver problems should consult a healthcare professional before use. People with diabetes should monitor their blood sugar levels closely, as jujube may affect blood glucose. Those scheduled for surgery should discontinue use at least two weeks prior, as it may interfere with anesthesia and blood sugar control.
Interaction with medications
Ziziphus jujuba may interact with various medications. It can enhance the effects of sedatives and anti-anxiety drugs, potentially causing excessive drowsiness. Jujube may also interact with diabetes medications, potentially leading to hypoglycemia. It may interfere with the effectiveness of anticonvulsants and certain antidepressants. Always consult a healthcare provider before combining jujube with any medications, especially those affecting the central nervous system or blood sugar levels.
6. Passionflower
Passionflower has shown promising potential as a natural remedy for insomnia. Research suggests that Passiflora incarnata, a specific species of passionflower, may help improve sleep quality and reduce sleep disturbances. The herb contains compounds that interact with GABA receptors in the brain, promoting relaxation and sedation. Studies have demonstrated that passionflower can shorten the time it takes to fall asleep, increase total sleep time, and enhance overall sleep quality. In one clinical trial, participants who consumed passionflower tea reported significantly better sleep quality compared to those who drank a placebo. The sleep-inducing effects of passionflower are attributed to its ability to increase blood melatonin levels and modulate neurotransmitters involved in sleep regulation.
What Research Says?
- Studies executed by International Clinical Psychopharmacology indicate passionflower significantly increased total sleep time (TST) in subjects with insomnia compared to placebo.
- Research work done by Planta Medica and The International Journal on Complementary and Alternative Medicine suggests Passionflower, often in combination with other herbs like valerian and hops, has been shown to improve sleep latency, reduce wake time after sleep onset, and increase total sleep time.
- As evidenced by research led by Nutrients and Journal of Psychopharmacology, Passionflower’s sedative and sleep-promoting properties may be due to its interaction with the GABAergic system, which is crucial for sleep regulation.
- Research undertaken by Functional Foods in Health and Disease shows Molecular studies suggest that passionflower’s flavonoid glycosides may enhance the expression of clock genes, potentially influencing sleep patterns.
- According to studies led by Nutrients and Complementary Therapies in Medicine, Passionflower has been reported to be safe with no significant adverse effects, making it a viable alternative to conventional sleep medications.
How to Use
To use passionflower for insomnia, prepare a tea by steeping 1-2 teaspoons of dried passionflower in a cup of boiling water for 10-15 minutes. Drink this tea 30-60 minutes before bedtime. Alternatively, take 250-500 mg of passionflower extract in capsule form before bed. For a stronger effect, some studies have used doses up to 1000 mg. Start with a lower dose and increase gradually if needed. Passionflower can also be taken as a tincture, using 0.5-2 ml three times daily. Always consult a healthcare professional before starting any new supplement regimen.
Potential side effects of Passionflower
While generally considered safe, passionflower may cause side effects such as drowsiness, dizziness, and confusion in some individuals. Less common side effects include nausea, vomiting, and rapid heartbeat. Some users may experience altered consciousness or coordination issues. In rare cases, liver toxicity has been reported. It’s important to start with a low dose and monitor for any adverse reactions, especially when first using passionflower.
Who should avoid Passionflower
Pregnant and breastfeeding women should avoid passionflower due to potential risks to the fetus or infant. Individuals scheduled for surgery should discontinue use at least two weeks prior, as it may interact with anesthesia. Those with liver disease or a history of liver problems should consult a healthcare professional before use. People with bleeding disorders or taking blood-thinning medications should also exercise caution when using passionflower.
Interaction with medications
Passionflower can interact with various medications, potentially enhancing their effects. It may increase the sedative effects of drugs like benzodiazepines, barbiturates, and sleep aids. Passionflower can also interact with blood thinners, increasing the risk of bleeding. Those taking MAO inhibitors should avoid passionflower, as it may intensify their effects. Always consult a healthcare provider before combining passionflower with any medications, especially those affecting the central nervous system.
7. Ashwagandha

Ashwagandha has shown promising potential as a natural remedy for insomnia. Research indicates that this adaptogenic herb can improve various aspects of sleep, including sleep onset latency, sleep efficiency, total sleep time, and wake after sleep onset. A systematic review and meta-analysis of five studies found that ashwagandha supplements had a small but significant effect on improving overall sleep, with more prominent benefits observed in adults diagnosed with insomnia, at dosages of 600 mg/day or higher, and when taken for at least 8 weeks. Clinical trials have demonstrated that ashwagandha can help people fall asleep faster, enhance sleep quality, and improve mental alertness upon waking. The herb’s ability to reduce stress and anxiety, which are often underlying causes of sleep disturbances, may contribute to its sleep-promoting effects.
What Research Says?
- Research carried out by Journal of Ethnopharmacology and Cureus indicates Ashwagandha root extract significantly improves sleep onset latency, total sleep time, sleep efficiency, and reduces wake after sleep onset in both healthy individuals and those with insomnia.
- Based on research carried out by PLoS One, Studies show that Ashwagandha extract improves sleep quality and quantity, particularly in individuals diagnosed with insomnia, with effects more pronounced at higher dosages and longer treatment durations.
- As per studies undertaken by PLoS One, the sleep-promoting effects of Ashwagandha are linked to its active components, such as triethylene glycol, which induces non-rapid eye movement sleep.
- According to studies performed by Journal of Food and Drug Analysis and Journal of Education, Health and Sport, Ashwagandha’s efficacy in promoting sleep is also associated with its interaction with GABAergic and serotonin receptors, enhancing the expression of GABAA and serotonin receptors, which are crucial for sleep regulation.
- Research undertaken by CURRENT DEVELOPMENTS IN NUTRITION reveals Ashwagandha with higher concentrations of withanolides shows greater efficacy in improving sleep quality and duration compared to lower concentrations or unstandardized supplements.
- Findings from research done by AYU show Combined therapies, such as Ashwagandha root powder with Brimhana Nasya, show enhanced effectiveness in managing primary insomnia in elderly patients compared to Ashwagandha alone.
How to use
To use ashwagandha for insomnia, take 300-600 mg of a standardized root extract 1-2 hours before bedtime. Start with a lower dose and gradually increase if needed. Alternatively, consume 1-2 teaspoons of ashwagandha powder mixed in warm milk or water before bed. For optimal results, use consistently for at least 8-10 weeks. Some studies suggest taking it earlier in the evening may be more beneficial. As always, consult with a healthcare professional before starting any new supplement regimen, especially if you have existing health conditions or take medications.
Potential side effects of Ashwagandha
Common side effects of ashwagandha are generally mild and may include stomach upset, loose stools, nausea, and drowsiness. In rare cases, more serious side effects such as liver dysfunction have been reported. Some users may experience headaches, dizziness, or skin rashes. Long-term safety data is limited, so it’s important to monitor for any adverse reactions, especially with prolonged use.
Who should avoid Ashwagandha
Pregnant women should avoid ashwagandha due to potential risks of miscarriage. Breastfeeding mothers, individuals with hormone-sensitive prostate cancer, and those with autoimmune diseases like lupus or rheumatoid arthritis should also avoid it. People with thyroid disorders or liver problems should consult a healthcare provider before use. Those scheduled for surgery should discontinue ashwagandha at least two weeks prior.
Interaction with medications
Ashwagandha may interact with various medications, including thyroid hormone medications, potentially altering their effectiveness. It may enhance the effects of sedatives, antidiabetic drugs, and blood pressure medications. Caution is advised when combining ashwagandha with immunosuppressants or benzodiazepines. Those taking any prescription medications, especially for thyroid issues, diabetes, or anxiety, should consult their healthcare provider before using ashwagandha.
8. Lemon Balm
Lemon balm (Melissa officinalis) has shown promising potential as a natural remedy for insomnia. Research suggests that this herb can help improve sleep quality and reduce sleep disturbances. The active compounds in lemon balm, particularly rosmarinic acid, interact with GABA receptors in the brain, promoting relaxation and sedation. Studies have demonstrated that lemon balm can shorten the time it takes to fall asleep, increase total sleep time, and enhance overall sleep quality. A clinical trial found that participants who consumed lemon balm tea reported significantly better sleep quality compared to those who drank a placebo. Additionally, lemon balm’s ability to reduce anxiety and stress, which are often underlying causes of insomnia, may contribute to its sleep-promoting effects. When combined with other herbs like valerian, lemon balm has been shown to be particularly effective in improving sleep patterns and reducing restlessness.
What Research Says?
- As research performed by European Psychiatry suggests Lemon balm significantly improved sleep quality in menopausal women compared to a placebo, as measured by the Pittsburgh Sleep Quality Index (PSQI).
- Research completed by Complementary Therapies in Medicine indicates a combination of melatonin, vitamin B6, and lemon balm extract showed significant improvements in sleep quality, sleep onset latency, and total sleep duration in individuals with mild-to-moderate insomnia.
- According to investigations conducted by Cogent Medicine, An herbal supplement containing lemon balm, along with other ingredients like lavender essential oil, showed significant improvements in subjective sleep quality in participants with mild to moderate insomnia.
- Research efforts by show that Nutrients, Lemon balm’s sedative and sleep-promoting properties are believed to be due to its interaction with the GABAergic system, which is crucial for sleep regulation.
- As demonstrated by research from Phytomedicine and Phytomedicine, A combination of valerian root and lemon balm was effective in reducing restlessness and dyssomnia in children, indicating potential benefits for sleep disorders.
- Research initiated by Phytotherapy Research and Pharmaceuticals and drug technology suggests Lemon balm has been shown to significantly improve anxiety and depression scores, which are often comorbid with insomnia, suggesting an indirect benefit for sleep through mood improvement.
How to Use
To use lemon balm for insomnia, prepare a tea by steeping 1-2 teaspoons of dried lemon balm leaves in a cup of hot water for 5-10 minutes. Drink this tea 30-60 minutes before bedtime. Alternatively, take 300-600 mg of lemon balm extract in capsule form before bed. For a stronger effect, some studies have used doses up to 1200 mg. Lemon balm can also be used as a tincture, taking 2-3 ml before bedtime. Always start with a lower dose and consult a healthcare professional before use.
Potential side effects of Lemon Balm
While generally considered safe, lemon balm may cause side effects in some individuals. These can include nausea, vomiting, abdominal pain, dizziness, and wheezing. Some users may experience increased appetite, headaches, or skin irritation when applied topically. In rare cases, lemon balm might cause anxiety, irritability, or sleep disturbances. Long-term use or high doses may lead to dependency and withdrawal symptoms upon discontinuation.
Who should avoid Lemon Balm
Pregnant and breastfeeding women should avoid lemon balm due to insufficient safety data. Individuals with thyroid disorders should consult a healthcare professional before use, as lemon balm may affect thyroid function. Those scheduled for surgery should discontinue use at least two weeks prior, as it may interact with anesthesia. People with liver disease or a history of liver problems should exercise caution when using lemon balm.
Interaction with medications
Lemon balm may interact with various medications, potentially enhancing their effects. It can increase the sedative effects of drugs like benzodiazepines, barbiturates, and other sleep aids. Lemon balm may interfere with thyroid hormone medications, reducing their effectiveness. It can also interact with medications metabolized by the liver, potentially altering their efficacy. Those taking any prescription medications, especially for thyroid issues, anxiety, or sleep disorders, should consult their healthcare provider before using lemon balm.
9. Californian Poppy

California poppy (Eschscholzia californica) has shown promise as a natural remedy for insomnia. Research suggests that this herb contains alkaloids, particularly californidine, protopine, and allocryptopine, which interact with GABA receptors in the brain, promoting relaxation and sedation. California poppy extract can help reduce the time it takes to fall asleep, increase total sleep time, and improve overall sleep quality. In one clinical trial, participants who consumed a supplement containing California poppy extract reported significantly better sleep quality compared to those who took a placebo. The herb’s ability to modulate neurotransmitters involved in sleep regulation, combined with its anxiolytic properties, may contribute to its effectiveness in treating insomnia.
What Research Says?
- According to the research carried out by Complementary Therapies in Medicine, A combination of melatonin, vitamin B6, and medicinal plants, including Californian poppy, significantly improved sleep quality, reduced sleep onset latency, and increased total sleep duration in individuals with mild-to-moderate insomnia.
- Studies conducted by Nutrients and Journal for Research in Applied Sciences and Biotechnology indicate Herbal treatments, including Californian poppy, have been shown to reduce sleep latency and improve both subjective and objective measures of sleep quality.
How to Use
To use California poppy for insomnia, prepare a tea by steeping 1-2 teaspoons of dried herb in a cup of hot water for 10-15 minutes. Drink 1-2 cups 30-60 minutes before bedtime. Alternatively, take 250-500 mg of standardized extract in capsule form or 15-25 drops of tincture under the tongue before bed. For a stronger effect, some studies have used doses up to 1000 mg. Start with a lower dose and increase gradually if needed. Always consult a healthcare professional before using, especially if you have existing health conditions or take medications.
Potential side effects of California Poppy
California poppy may cause drowsiness, dizziness, and mild nausea in some individuals. Allergic reactions, though rare, can occur and may include symptoms such as rash, itching, or difficulty breathing. Long-term use or high doses may potentially lead to tolerance or dependence, although more research is needed to confirm these effects.
Who should avoid California Poppy
Pregnant and breastfeeding women should avoid California poppy due to insufficient safety data. Individuals with liver disease, scheduled for surgery, or those with a history of substance abuse should also refrain from using it. People with known allergies to plants in the Papaveraceae family should exercise caution.
Interaction with medications
California poppy may interact with sedative medications, including benzodiazepines and CNS depressants, potentially increasing drowsiness and slowing down the central nervous system. It may also interact with blood thinners and blood pressure medications. Always consult a healthcare provider before combining California poppy with any prescription or over-the-counter medications.
10. Lavender
Lavender has been widely recognized for its potential benefits in treating insomnia and improving sleep quality. The soothing aroma of lavender has been shown to have calming effects on the nervous system, promoting relaxation and reducing anxiety, which can contribute to better sleep. Studies have demonstrated that inhaling lavender essential oil before bedtime can increase slow-wave sleep, the deepest phase of sleep, and improve overall sleep efficiency. Additionally, lavender has been found to increase total sleep time and reduce the time it takes to fall asleep, making it a natural and effective remedy for those struggling with insomnia.
What Research Says?
- Research executed by Journal of Ethnopharmacology reveals Inhaled lavender significantly improved sleep quality and quantity in diabetic patients with insomnia compared to placebo.
- As shown by research done by Sleep and Complementary Therapies in Medicine, Lavender essential oil inhalation led to a significant increase in sleep quality and efficiency in postmenopausal women with insomnia.
- Research organized by Evidence-Based Complementary and Alternative Medicine suggests Lavender aromatherapy showed a significant improvement in sleep quality in midlife women with insomnia.
- Findings from studies performed by Sleep indicate Participants using lavender essential oil reported significant improvements in overall quality of life and reduced menopausal symptoms.
- Research performed by Cogent Medicine shows Participants reported subjective improvements in sleep quality when using a lavender-containing herbal supplement.
- According to the findings from research conducted by Holistic Nursing Practice, Lavender essential oil was associated with improved sleep quality in individuals without diagnosed insomnia.
How to Use
To use lavender for insomnia, there are several effective methods. Add a few drops of lavender essential oil to a diffuser in your bedroom before sleep, or place a sachet of dried lavender under your pillow. Alternatively, apply diluted lavender oil to your temples, wrists, or the soles of your feet before bedtime. You can also try adding lavender to a warm bath, drinking lavender tea, or using lavender-scented linen sprays on your bedding. For a more immersive experience, consider using lavender-infused pillows or eye masks.
Potential side effects of Lavender
Lavender may cause mild side effects in some individuals, including constipation, headache, and increased appetite. When applied topically, it can occasionally lead to skin irritation. In rare cases, lavender may cause drowsiness or dizziness. Some people may experience allergic reactions, manifesting as rash, itching, or difficulty breathing. Long-term use or high doses might potentially lead to hormonal imbalances, particularly in young males.
Who should avoid Lavender
Pregnant and breastfeeding women should avoid using lavender due to insufficient safety data. Young boys who haven’t reached puberty should not use lavender-containing products topically, as it may disrupt normal hormones and potentially cause breast growth. Individuals with known allergies to plants in the Lamiaceae family should exercise caution. Those scheduled for surgery should discontinue lavender use at least two weeks prior.
Interaction with medications
Lavender may interact with sedative medications and central nervous system (CNS) depressants, potentially increasing drowsiness and slowing down the nervous system. It might also interact with blood pressure medications. While lavender has shown weak inhibitory effects on CYP3A4 and CYP1A2 enzymes, clinical studies suggest a low risk of significant drug interactions. However, always consult a healthcare provider before combining lavender with prescription or over-the-counter medications.
FAQs
- Can I combine multiple herbs to treat insomnia?
Yes, combining certain herbs like valerian, chamomile, and passionflower can enhance the sleep-inducing effects due to their complementary properties. However, it is important to consult with a healthcare provider to avoid potential interactions or side effects.
- Are there any specific dosage guidelines for children using herbal remedies for insomnia?
Herbal remedies for children must be used with caution. Some herbs, like chamomile, may be safe for older children, but others, such as valerian and kava, should generally be avoided in young children unless recommended by a healthcare provider.
- How long does it take for herbal remedies to show results for insomnia?
The effects of herbal remedies may vary depending on the individual. Some herbs, such as valerian or chamomile, may provide immediate sleep benefits when taken before bedtime. However, long-term herbs like ashwagandha may take several weeks of consistent use to show noticeable improvements in sleep quality.
- Can herbs for insomnia cause dependency or withdrawal symptoms?
Most herbs used for insomnia, like chamomile, valerian, and lavender, have a low risk of dependency compared to conventional sleep medications. However, herbs like kava and California poppy can lead to tolerance or withdrawal symptoms if used in high doses or over a long period.
- Are there lifestyle changes that can enhance the effects of herbs for insomnia?
Yes, combining herbal remedies with sleep hygiene practices such as maintaining a regular sleep schedule, reducing screen time before bed, and creating a relaxing bedtime routine can enhance the effectiveness of herbs in treating insomnia.
- Can I take herbs for insomnia along with melatonin?
Melatonin, a natural sleep hormone, can be used in combination with herbs like valerian or chamomile for better sleep. However, it’s important to consult a healthcare provider to ensure safe and effective use of both together.
- Are there any dietary restrictions when using herbs for insomnia?
Certain dietary habits, like consuming caffeine, nicotine, or alcohol, can counteract the sedative effects of herbal remedies. It is recommended to avoid these substances, especially in the evening, to maximize the benefits of herbs for sleep.
- What time of day should I take herbs for insomnia?
Herbs for insomnia are generally most effective when taken 30 minutes to an hour before bedtime. However, some herbs like ashwagandha can be taken earlier in the evening to help reduce overall stress and promote better sleep.
- Can herbs for insomnia help with other sleep disorders like sleep apnea?
Herbal remedies can improve sleep quality but are not typically recommended as primary treatments for serious sleep disorders like sleep apnea. These conditions often require medical treatment such as CPAP therapy.
- Are there any long-term risks of using herbs for insomnia?
Most herbs for insomnia are safe for long-term use when taken in recommended doses. However, herbs like kava have been associated with liver toxicity in rare cases. It’s advisable to consult with a healthcare provider for long-term use of any herbal remedy.