Migraine is a complex neurological disorder characterized by recurrent attacks of head pain and a variety of neurological symptoms. It is defined clinically by the occurrence of at least five attacks of unprovoked headache lasting 4-72 hours, severe enough to significantly impair daily activities, and often accompanied by nausea or sensitivity to light and sound. The condition can manifest with or without aura, and the headache need not always be pulsatile or lateralized. Migraine is believed to originate from a genetically induced hypersensitivity of neurons within the central nervous system, which can be triggered by environmental or internal changes. The International Classification of Headache Disorders (ICHD-3) provides diagnostic criteria for distinguishing between episodic and chronic migraine, with chronic migraine defined as headaches occurring on at least 15 days per month for at least three months, with migraine features on at least eight days per month. Additionally, resistant and refractory migraines are defined based on the failure of multiple preventive treatments and the persistence of debilitating headache days. The disorder is also associated with a range of symptoms beyond pain, including nausea, hypersensitivity to light and sound, speech deficits, and mood alterations, reflecting the involvement of various brain regions during an attack.
Migraine is a complex neurological disorder characterized by recurrent attacks of head pain and a variety of neurological symptoms. It is defined clinically by the occurrence of at least five attacks of unprovoked headache lasting 4-72 hours, severe enough to significantly impair daily activities, and often accompanied by nausea or sensitivity to light and sound. The condition can manifest with or without aura, and the headache need not always be pulsatile or lateralized. Migraine is believed to originate from a genetically induced hypersensitivity of neurons within the central nervous system, which can be triggered by environmental or internal changes. The International Classification of Headache Disorders (ICHD-3) provides diagnostic criteria for distinguishing between episodic and chronic migraine, with chronic migraine defined as headaches occurring on at least 15 days per month for at least three months, with migraine features on at least eight days per month. Additionally, resistant and refractory migraines are defined based on the failure of multiple preventive treatments and the persistence of debilitating headache days. The disorder is also associated with a range of symptoms beyond pain, including nausea, hypersensitivity to light and sound, speech deficits, and mood alterations, reflecting the involvement of various brain regions during an attack.
Types of migraine
Understanding the different types of migraine can help in better diagnosing, managing, and treating the condition. Whether triggered by environmental factors, genetics, or lifestyle choices, migraines affect individuals in unique ways. Here’s a breakdown of the most common types of migraine you should be aware of
- Migraine without aura (common migraine)
- Migraine with aura (classic migraine)
- Chronic migraine
- Menstrual migraine
- Hemiplegic migraine
- Retinal migraine (ocular migraine)
- Vestibular migraine
- Abdominal migraine
- Basilar migraine (migraine with brainstem aura)
- Silent migraine (acephalgic migraine)
- Status migrainosus
- Alternating hemiplegic migraine
Common Causes of Migraine
Migraine attacks are often set off by a variety of internal and external factors. While the exact causes may vary from person to person, certain triggers are more common and can lead to the onset of a migraine episode. Understanding these triggers can help manage and prevent the frequency and intensity of migraines. Here’s a look at some of the most common causes of migraine that you should be aware of:
- Hormonal changes (especially in women)
- Stress
- Changes in sleep patterns or lack of sleep
- Skipping meals or fasting
- Certain foods and drinks (e.g. alcohol, caffeine, chocolate, aged cheese)
- Food additives (e.g. MSG, aspartame)
- Sensory stimuli (bright lights, loud sounds, strong smells)
- Weather changes
- Physical exertion
- Dehydration
- Medications (e.g. oral contraceptives, vasodilators)
- Caffeine withdrawal
- Alcohol consumption
- Emotional changes (anxiety, depression, excitement)
- Environmental factors (humidity, temperature changes)
- Neck and shoulder tension
- Poor posture
- Low blood sugar
- Genetics and family history
- Certain medical conditions (e.g. depression, anxiety, sleep disorders)
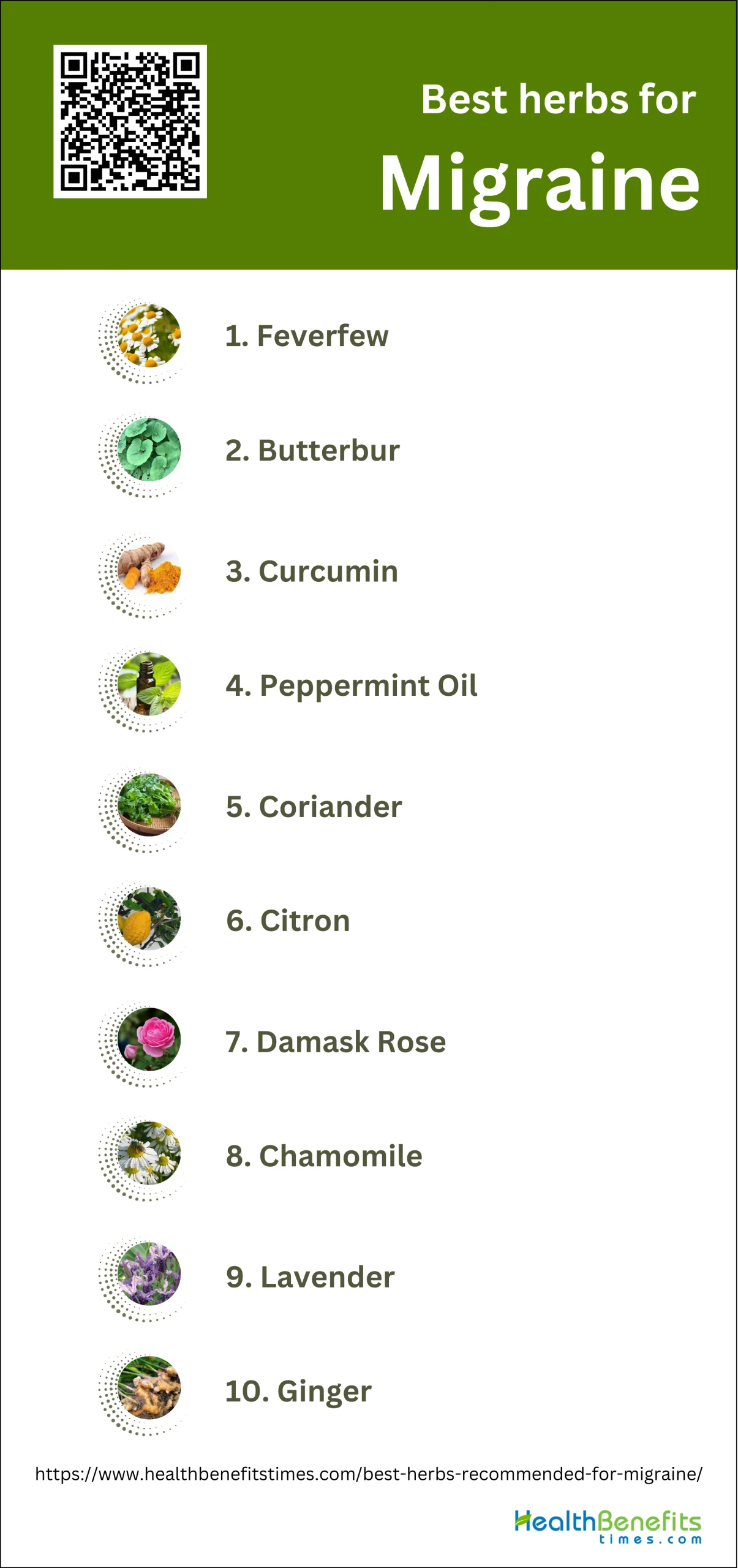
Best herbs Recommended for Migraine
Herbal treatments for migraine offer several advantages over conventional medications, primarily due to their multifaceted physiological effects and lower incidence of side effects. Studies have shown that herbs such as feverfew, butterbur, curcumin, and ginger possess significant antimigraine properties, providing both acute relief and prophylactic benefits. Unlike conventional drugs, which often come with a range of adverse effects, herbal remedies tend to be better tolerated by patients, making them a preferable option for those seeking natural and holistic approaches to migraine management. Additionally, traditional Chinese medicine (TCM) and other herbal therapies not only address the symptoms but also target the root causes of migraines, offering a more comprehensive treatment strategy. Despite the need for further high-quality research to fully establish their efficacy and safety, the existing evidence suggests that herbal treatments can be a valuable alternative or complement to conventional pharmacotherapies for migraine sufferers.
1. Feverfew
Feverfew has shown promising potential as a natural remedy for migraine prevention. Clinical studies have demonstrated that feverfew may help reduce the frequency and severity of migraine attacks. A rigorous, larger study involving 218 participants found that feverfew reduced migraine frequency by 1.9 attacks per month, compared to a 1.3 reduction with placebo, resulting in a difference of 0.6 fewer attacks per month for those taking feverfew. The active compound parthenolide, found in feverfew leaves, is believed to be responsible for its anti-migraine effects by inhibiting prostaglandin production, interfering with blood vessel mechanisms, and potentially inhibiting serotonin secretion.
What Research Says?
- Based on research carried out by Cochrane Database of Systematic Reviews, Several studies indicate that feverfew may reduce the frequency and severity of migraine attacks, but the evidence is not consistent across all trials.
- As per studies undertaken by Cephalalgia, Some high-quality trials found no significant difference between feverfew and placebo in preventing migraines.
- According to studies performed by Cephalalgia and Public Health Nutrition, Many trials had small sample sizes and varying methodological quality, which affects the reliability of the results. Larger, more rigorous studies are needed to draw firm conclusions.
- Research undertaken by Public Health Nutrition and Cochrane Database of Systematic Reviews reveals Feverfew is generally associated with mild and transient adverse effects, such as gastrointestinal complaints and mouth ulcers, with no major safety concerns reported.
How to Use
To use feverfew for migraine prevention, take 100-300 mg of a standardized extract containing 0.2-0.4% parthenolides daily. This can be taken as a single dose or divided into 2-4 doses throughout the day. Feverfew is available in capsules, tablets, or as dried leaves for tea. Start with a lower dose and gradually increase if needed. Consistency is key, as studies have shown benefits after several weeks of regular use. Always consult a healthcare professional before starting feverfew, especially if you’re taking other medications or have existing health conditions.
Potential side effects of Feverfew
Feverfew may cause gastrointestinal discomfort, including heartburn, nausea, vomiting, diarrhea, and constipation. Some users experience headaches, dizziness, and difficulty sleeping. Allergic reactions can occur, resulting in skin rashes or mouth ulcers. In rare cases, it may lead to increased heart rate or menstrual changes. Long-term use might cause withdrawal symptoms like rebound headaches, anxiety, and muscle stiffness when discontinued abruptly.
Who should avoid Feverfew
Pregnant women should avoid feverfew due to its potential to cause uterine contractions and miscarriage. Breastfeeding mothers should also refrain from using it due to insufficient safety data. Individuals with allergies to plants in the Asteraceae family (e.g., ragweed, daisies) should avoid feverfew. People with bleeding disorders or scheduled for surgery should not use it. Children under two years old and those with liver or kidney problems should also avoid feverfew.
Interaction with medications
Feverfew may interact with blood-thinning medications, increasing the risk of bleeding. It can enhance the effects of antiplatelet drugs and NSAIDs. Feverfew may interfere with the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6. It can potentially interact with blood pressure medications, diabetes drugs, and immunosuppressants. Always consult a healthcare provider before using feverfew alongside any medications, especially those affecting blood clotting or liver function.
2. Butterbur
Butterbur has shown promising potential as a natural remedy for migraine prevention. Clinical studies have demonstrated that butterbur, particularly the root extract, may help reduce the frequency and severity of migraine attacks. A rigorous study involving 218 participants found that butterbur reduced migraine frequency by 1.9 attacks per month, compared to a 1.3 reduction with placebo. The active compound petasin, found in butterbur, is believed to be responsible for its anti-migraine effects by inhibiting prostaglandin production and potentially interfering with blood vessel mechanisms. In 2012, the American Academy of Neurology recommended butterbur for migraine prevention based on its effectiveness and safety profile.
What Research Says?
- Findings from research done by Current Pain and Headache Reports and Complementary Therapies in Clinical Practice show Butterbur has shown positive effects in reducing the frequency of migraine attacks in both adults and children.
- As research performed by British Journal of Pharmacology and Frontiers in Neurology suggests the active components, petasins, are believed to contribute to its anti-migraine properties by desensitizing nociceptors and inhibiting inflammatory mediators.
- Research completed by Toxicological Sciences indicates some studies have reported rare cases of hepatobiliary toxicity, but these were associated with high doses or extracts rich in petasin.
- According to investigations conducted by Phytotherapy Research and European Neurology, Systematic reviews and randomized controlled trials have generally supported the efficacy of butterbur in migraine prophylaxis, though some studies highlight the need for further high-quality research.
How to Use
To use butterbur for migraine prevention, take 50-75 mg of a standardized extract containing 15% petasins twice daily with meals. Only use PA-free (pyrrolizidine alkaloid-free) products from reputable manufacturers. Start with a lower dose and gradually increase if needed. Consistency is key, as studies have shown benefits after several weeks of regular use. The specific extract Petadolex has been most extensively studied, at a dose of 75 mg twice daily. Always consult a healthcare professional before starting butterbur, especially if you’re taking other medications or have existing health conditions.
Potential side effects of Butterbur
Butterbur may cause gastrointestinal discomfort, including belching, nausea, and stomach upset. Some users experience headaches, itchy eyes, drowsiness, and fatigue. Allergic reactions can occur, especially in those sensitive to plants in the Asteraceae family. Breathing difficulties have been reported in rare cases. It’s crucial to use only PA-free butterbur products, as those containing pyrrolizidine alkaloids can cause serious liver damage and other health issues.
Who should avoid Butterbur
Pregnant and breastfeeding women should avoid butterbur due to potential risks to fetal development and lack of safety data. Individuals with liver disease or a history of liver problems should not use butterbur. Those allergic to plants in the Asteraceae family (e.g., ragweed, daisies) should avoid it. Children under 12 years old and people with kidney disease should consult a healthcare provider before use. Always use PA-free products to minimize health risks.
Interaction with medications
Butterbur may interact with certain medications, potentially affecting their efficacy or increasing side effects. It can enhance the effects of sedatives and anti-anxiety medications, causing excessive drowsiness. Butterbur may interfere with the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6. It could potentially interact with blood thinners, increasing the risk of bleeding. Always consult a healthcare provider before using butterbur alongside any medications, especially those affecting liver function or the central nervous system.
3. Curcumin

Curcumin, the active compound in turmeric, has shown promising potential as a natural remedy for migraine prevention and relief. Studies have demonstrated that curcumin supplementation can improve pro-inflammatory markers and clinical features of migraine headaches, likely due to its potent anti-inflammatory and antioxidant properties. A randomized, double-blind, placebo-controlled clinical trial involving 44 women with migraine found that curcumin supplementation significantly reduced serum levels of calcitonin gene-related peptide (CGRP) and interleukin-6 (IL-6), both of which play crucial roles in migraine pathophysiology. Additionally, curcumin was shown to decrease the severity, duration, and frequency of migraine headaches compared to placebo. The compound’s ability to inhibit prostaglandin production, interfere with blood vessel mechanisms, and potentially inhibit serotonin secretion contributes to its anti-migraine effects.
What Research Says?
- Research efforts by International Journal of Preventive Medicine and the Avicenna Journal of Phytomedicine show that Curcumin supplementation significantly reduces pro-inflammatory markers such as IL-6 and CGRP, and improves clinical symptoms including headache severity, duration, and frequency.
- As demonstrated by research from Complementary Therapies in Clinical Practice, Nano-curcumin specifically reduces IL-17 levels, which are associated with inflammation in migraine patients.
- Research initiated by International Journal of Nanomedicine and Pain Research and Management suggests Curcumin, especially in liposomal or nano forms, decreases oxidative stress markers like TOS, MDA, and NOx, and increases antioxidative capacity, which may help in reducing migraine symptoms.
- According to the research carried out by Nutritional Neuroscience and CNS & Neurological Disorders – Drug Targets, Combining curcumin with other supplements like CoQ10 or omega-3 fatty acids shows synergistic effects, further reducing migraine frequency, severity, and duration, and improving quality of life.
- Studies conducted by Nutritional Neuroscience and Phytotherapy Research indicate Curcumin, in various formulations, has shown promising results in clinical trials for reducing migraine symptoms without significant side effects, suggesting it as a potential therapeutic option.
How to Use
To use curcumin for migraine prevention, take 500 mg of a standardized curcumin extract twice daily with meals. Look for formulations with enhanced bioavailability, such as phytosomal curcumin or those combined with piperine. Start with a lower dose and gradually increase if needed. Consistency is key, as studies have shown benefits after several weeks of regular use. Some research suggests combining curcumin with omega-3 fatty acids may enhance its effects. Always consult a healthcare professional before starting curcumin supplementation, especially if you’re taking other medications or have existing health conditions.
Potential side effects of Curcumin
Curcumin may cause gastrointestinal discomfort, including nausea, diarrhea, and stomach upset. Some individuals may experience headaches, dizziness, or skin rashes. In rare cases, it can lead to liver function abnormalities or increased risk of bleeding. High doses may cause iron deficiency due to reduced iron absorption. Prolonged use or excessive intake might result in kidney stones due to increased urinary oxalate levels.
Who should avoid Curcumin
Pregnant and breastfeeding women should avoid curcumin supplements due to insufficient safety data. Individuals with gallbladder problems, bleeding disorders, or scheduled for surgery should refrain from using curcumin. People with iron deficiency anemia, liver disease, or hormone-sensitive conditions should consult a healthcare provider before use. Those with a history of kidney stones or at risk of developing them should be cautious with curcumin intake.
Interaction with medications
Curcumin may interact with blood thinners like warfarin, aspirin, and clopidogrel, increasing the risk of bleeding. It can enhance the effects of diabetes medications, potentially causing hypoglycemia. Curcumin may interfere with the absorption of iron and certain antibiotics. It can also interact with drugs metabolized by liver enzymes CYP3A4 and CYP2C9, potentially affecting their efficacy. Always consult a healthcare provider before combining curcumin with any medications.
4. Peppermint Oil
Peppermint oil has shown promising potential as a natural remedy for migraine relief. Studies have demonstrated that peppermint oil can help reduce the intensity and frequency of migraine attacks due to its analgesic, anti-inflammatory, and muscle-relaxant properties. The active compound menthol in peppermint oil creates a cooling sensation when applied topically, which can help soothe throbbing pain associated with migraines. Additionally, peppermint oil may improve blood flow and oxygen supply to the brain by dilating blood vessels, potentially alleviating migraine symptoms. A clinical trial found that peppermint oil significantly decreased headache intensity within 15 minutes compared to a placebo, with pain reduction persisting for up to an hour. Furthermore, the oil’s anti-nausea properties can help alleviate common migraine-related symptoms like nausea and vomiting.
What Research Says?
- Research executed by International Journal of Preventive Medicine reveals Peppermint oil significantly reduces the intensity and frequency of migraine headaches, showing comparable effectiveness to intranasal lidocaine.
- As shown by research done by Headache and Der Nervenarzt, Topical application of peppermint oil in ethanol has been shown to be as effective as acetaminophen in reducing headache intensity in tension-type headaches, suggesting potential benefits for migraine sufferers as well.
- Research organized by Phytomedicine and Cephalalgia suggests Peppermint oil induces a cooling effect on the skin, which may contribute to its analgesic properties by altering calcium channels in cold receptors and increasing skin blood flow.
- Findings from studies performed by Phytotherapy Research and Korean Journal of Family Medicine indicate Systematic reviews and meta-analyses indicate that while peppermint oil shows promise, the evidence is mixed and further high-quality research is needed to confirm its efficacy and safety for migraine treatment.
How to Use
To use peppermint oil for migraine relief, apply a few drops diluted with a carrier oil to your temples, forehead, and back of the neck. Gently massage the area for a cooling effect. Alternatively, add 3-5 drops to a bowl of hot water and inhale the steam for 5-10 minutes. For internal use, take 0.2 to 0.4 mL of peppermint oil in enteric-coated capsules three times daily. You can also add a few drops to your bath or use a peppermint oil roll-on for easy application. Always perform a patch test first and consult a healthcare professional before use.
Potential side effects of Peppermint Oil
Peppermint oil may cause heartburn, nausea, and vomiting when taken orally. Topical application can lead to skin irritation, allergic reactions, or burning sensations. Some people may experience headaches, flushing, or mouth sores. In rare cases, it can cause anal burning during bouts of diarrhea. Excessive use may result in dry mouth or gastrointestinal discomfort. Always dilute peppermint oil before use to minimize potential side effects.
Who should avoid Peppermint Oil
Pregnant and breastfeeding women should avoid peppermint oil due to insufficient safety data. Individuals with gastroesophageal reflux disease (GERD) or hiatal hernias should use caution, as it may worsen symptoms. People with gallbladder problems or severe liver damage should avoid it. Peppermint oil should not be applied to the face of infants or young children due to the risk of life-threatening breathing problems. Those with known allergies to mint plants should also avoid peppermint oil.
Interaction with medications
Peppermint oil may interact with medications that reduce stomach acid, potentially decreasing their effectiveness. It can enhance the effects of certain medications metabolized by liver enzymes, including cyclosporine. Peppermint oil may interact with drugs for diabetes, high blood pressure, and high cholesterol. It can also increase the risk of bleeding when used with blood thinners. Always consult a healthcare provider before using peppermint oil alongside any medications, especially those affecting the digestive system or liver function.
5. Coriander

Coriander has shown promising potential as a natural remedy for migraine relief. A randomized, triple-blind, placebo-controlled trial found that Coriandrum sativum syrup significantly decreased the duration, severity, and frequency of migraine attacks compared to placebo. The study revealed that coriander has a significant effect on both the probability of being migraine-free and the duration of migraine attacks. Coriander’s beneficial effects on migraines may be attributed to its anti-inflammatory, antioxidant, and analgesic properties. Traditional Ayurvedic medicine has long used coriander to relieve sinus pressure and headaches, typically by pouring hot water over fresh seeds and inhaling the steam. Additionally, coriander essential oil has been shown to improve spatial memory performance in animal studies, suggesting potential neuroprotective effects.
What Research Says?
- Research performed by Phytotherapy Research shows Systematic reviews indicate positive preliminary findings for coriander as a prophylactic treatment for migraine, though further high-quality research is needed to confirm these results.
- According to the findings from research conducted by Natural Resources for Human Health, Coriander contains bioactive compounds like linalool, which have neuroprotective, analgesic, and anti-inflammatory properties, potentially contributing to its migraine-relieving effects.
How to Use
To use coriander for migraine relief, prepare a tea by crushing 3 teaspoons of coriander seeds and soaking them in 300ml of room temperature water overnight. In the morning, filter the liquid and drink 100-150ml before breakfast, either at room temperature or with a little added warm water. For a more potent effect, you can expose the soaking seeds to moonlight. Alternatively, you can take 1-5 grams of powdered coriander seed three times daily between meals. Always consult a healthcare professional before starting any new treatment regimen, especially if you’re taking other medications.
Potential side effects of Coriander
Coriander may cause allergic reactions in some individuals, leading to symptoms like hives, difficulty breathing, and swelling of the face or throat. Excessive consumption can result in gastrointestinal discomfort, including nausea, stomach upset, and diarrhea. Some people might experience sun sensitivity, increasing the risk of sunburns. In rare cases, coriander can cause liver problems or respiratory issues when used in large quantities over prolonged periods. Always start with small amounts to test for any adverse reactions.
Who should avoid Coriander
Pregnant and breastfeeding women should avoid medicinal doses of coriander due to insufficient safety data. Individuals with allergies to plants in the Apiaceae family (e.g., carrots, celery) should be cautious. People with low blood pressure or those taking blood pressure medications should consult a healthcare provider before using coriander. Those with liver or kidney problems should exercise caution. Individuals scheduled for surgery should stop using coriander at least two weeks prior, as it may interfere with blood sugar control during the procedure.
Interaction with medications
Coriander may interact with several medications. It can enhance the effects of blood-thinning drugs, increasing the risk of bleeding. Coriander might lower blood sugar levels, potentially interacting with diabetes medications and causing hypoglycemia. It may also interact with medications metabolized by liver enzymes CYP3A4 and CYP2D6, affecting their efficacy. Coriander can potentially interfere with sedative medications, causing excessive drowsiness. Always consult a healthcare provider before combining coriander with any medications, especially those affecting blood sugar, blood pressure, or liver function.
6. Citron
Citron (Citrus medica L.) has shown promising potential as a natural remedy for migraine relief. A double-blind, randomized, placebo-controlled clinical trial published in 2016 found that Citron syrup was effective in reducing the intensity and duration of migraine attacks. The study revealed that Citron syrup was superior to placebo in decreasing headache intensity and duration, and its effectiveness was comparable to propranolol, a commonly prescribed medication for migraine prevention. The beneficial effects of Citron are attributed to its rich content of bioactive compounds, including flavonoids, limonoids, and phenolic acids, which possess anti-inflammatory, antioxidant, and analgesic properties. These compounds may help modulate pain pathways and reduce neurogenic inflammation associated with migraines.
What Research Says?
- Studies executed by Journal of Ethnopharmacology indicate Citron syrup significantly reduces the intensity and duration of migraine attacks compared to placebo, and its effectiveness is comparable to propranolol, a common migraine medication.
- Research work done by Phytotherapy Research suggests Preliminary findings suggest that Citron may be effective as a prophylactic treatment for migraine, although further high-quality research is needed to confirm these results.
How to Use
To use citron for migraine relief, prepare a syrup by boiling 50 grams of dried citron peel in 200 ml of water until the volume reduces to half. Strain and add 100 grams of sugar, then boil again until it reaches a syrupy consistency. Take 15 ml of this syrup three times daily, preferably before meals. Alternatively, you can consume fresh citron fruit or juice. For aromatherapy benefits, inhale citron essential oil or apply a diluted solution to your temples. Always consult a healthcare professional before starting any new treatment regimen.
Potential side effects of Citron
Citron may cause gastrointestinal discomfort, including nausea, stomach upset, and diarrhea when consumed in large quantities. Some individuals may experience allergic reactions, such as skin rashes or itching. Excessive consumption of citron can lead to increased acidity in the body, potentially causing heartburn or exacerbating acid reflux symptoms. In rare cases, it may cause headaches or migraines in sensitive individuals. As with other citrus fruits, citron may increase sun sensitivity, potentially leading to sunburn or skin irritation.
Who should avoid Citron
Individuals with citrus allergies or sensitivities should avoid citron. People with gastroesophageal reflux disease (GERD) or other digestive issues may need to limit or avoid citron due to its high acidity. Those with kidney problems should consult a healthcare provider before consuming citron, as its high potassium content may be problematic. Pregnant and breastfeeding women should exercise caution and consult their doctor before incorporating citron into their diet. Individuals prone to migraines may want to avoid citron, as it contains tyramine, a potential migraine trigger.
Interaction with medications
Citron may interact with certain medications, potentially affecting their efficacy or increasing side effects. It can enhance the effects of blood-thinning medications like warfarin, increasing the risk of bleeding. Citron may interfere with the absorption of some antibiotics, particularly those in the quinolone and tetracycline classes. It can also interact with statins, potentially increasing the risk of side effects. As with other citrus fruits, citron may affect the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6. Always consult a healthcare provider before consuming citron alongside any medications.
7. Damask Rose

Damask Rose (Rosa damascena) has shown promising potential as a natural remedy for migraine relief. Studies have demonstrated that the essential oil and hydrosol of Damask Rose possess analgesic, anti-inflammatory, and anxiolytic properties, which can help alleviate migraine symptoms. A clinical trial found that vapor therapy using rose oil was helpful for some types of headaches and migraines. The aromatic compounds in Damask Rose, particularly citronellol and geraniol, are believed to modulate pain pathways and reduce neurogenic inflammation associated with migraines. Additionally, the calming and stress-reducing effects of rose aromatherapy may help prevent migraine triggers related to anxiety and tension.
What Research Says?
- As evidenced by research led by Complementary Therapies in Medicine, One study found that topical application of Damask Rose oil did not significantly reduce the mean pain intensity of migraine headaches compared to a placebo. However, it showed a significant reduction in pain intensity for patients with “hot” type migraine syndrome at specific time points after application.
- Research undertaken by CNS Drugs shows Another review indicated that Damask Rose, when used in topical preparations, did not show efficacy in one clinical trial for migraine treatment.
- According to studies led by Complementary Therapies in Medicine, a systematic review and meta-analysis concluded that aromatherapy with Damask Rose significantly reduced the severity of acute pain in adults, although the quality of evidence was low.
- Research carried out by Complementary Therapies in Medicine indicates a comprehensive review of Rosa damascena’s phytopharmacological properties suggested promising evidence for its effectiveness and safety in pain relief, but emphasized the need for confirmatory studies with standardized products.
How to Use
To use Damask Rose for migraine relief, prepare a tea by steeping dried rose petals in boiling water for 10 minutes, then strain and drink 1-2 cups daily. For aromatherapy, add a few drops of Damask Rose essential oil to a diffuser or inhale directly from the bottle. Alternatively, dilute the essential oil with a carrier oil and apply to temples and pulse points. You can also create a steam inhalation by adding rose oil to hot water or use rose hydrosol as a facial mist for relaxation. Always consult a healthcare professional before starting any new treatment regimen.
Potential side effects of Damask Rose
Damask Rose essential oil may cause skin irritation, allergic reactions, or contact dermatitis in sensitive individuals. Some people may experience headaches, nausea, or dizziness when inhaling the strong scent. Excessive internal use can lead to gastrointestinal discomfort, including nausea and vomiting. In rare cases, it may cause photosensitivity, making the skin more susceptible to sunburn. Always perform a patch test before using Damask Rose products and discontinue use if any adverse reactions occur.
Who should avoid Damask Rose
Pregnant women, especially during the first trimester, should avoid using Damask Rose essential oil due to its potential to stimulate uterine contractions. Breastfeeding mothers should also exercise caution. Individuals with sensitive skin or known allergies to plants in the Rosaceae family should avoid Damask Rose products. People with hormone-sensitive conditions, such as certain cancers or endometriosis, should consult a healthcare provider before use. Children under 6 years old should not use Damask Rose essential oil without professional guidance.
Interaction with medications
Damask Rose may interact with certain medications, potentially affecting their efficacy or increasing side effects. It may enhance the effects of sedative medications, causing excessive drowsiness. The oil could interact with blood thinners, increasing the risk of bleeding. Damask Rose may also interfere with the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6. Individuals taking hormone-related medications, including birth control pills, should consult their healthcare provider before using Damask Rose products.
8. Chamomile
Chamomile has shown promising potential as a natural remedy for migraine relief. Its anti-inflammatory and analgesic properties may help reduce the intensity and duration of migraine attacks. A randomized, double-blind, placebo-controlled study found that chamomile oleogel significantly decreased pain, nausea, vomiting, photophobia, and phonophobia in patients with migraine without aura after 30 minutes of application. Chamomile contains compounds like apigenin, which acts on brain receptors and may produce a relaxing and calming effect, potentially helping to alleviate migraine symptoms. Additionally, chamomile tea has been traditionally used to reduce stress and promote relaxation, both of which can be beneficial in managing migraine symptoms.
What Research Says?
- Based on research carried out by Neurological Sciences, Chamomile oleogel significantly reduced pain, nausea, vomiting, photophobia, and phonophobia in patients with migraine without aura, as evidenced by a randomized controlled trial.
- As per studies undertaken by Medical Hypotheses, Chamomile oil, when applied topically, showed promising results in reducing migraine pain, supported by its anti-inflammatory and neuroprotective properties.
- According to studies performed by Phytotherapy Research, a systematic review highlighted positive preliminary findings on the use of chamomile as an acute treatment for migraine, although further high-quality research is needed.
- Research undertaken by Modern Chemistry & Applications reveals The anti-inflammatory properties of chamomile, particularly through the inhibition of prostaglandin E2 (PGE2) and other pro-inflammatory biomarkers, support its use in migraine management.
How to Use
To use chamomile for migraine relief, steep 2-3 teaspoons of dried chamomile flowers in a cup of hot water for 5-10 minutes. Strain and drink this tea 2-3 times daily, especially at the onset of migraine symptoms. For topical application, mix a few drops of chamomile essential oil with a carrier oil and gently massage onto temples and neck. Alternatively, add chamomile oil to a warm bath or use a cold compress infused with chamomile tea. For aromatherapy benefits, inhale chamomile essential oil directly or use a diffuser. Always consult a healthcare professional before starting any new treatment regimen.
Potential side effects of Chamomile
Chamomile may cause allergic reactions in some individuals, ranging from mild skin irritation to severe anaphylaxis. Common side effects include nausea, vomiting, and gastrointestinal discomfort, especially when consumed in large doses. Some people may experience drowsiness, dizziness, or skin reactions like contact dermatitis. In rare cases, chamomile can cause eye irritation when used in eye washes. Long-term use may lead to increased sensitivity to sunlight, potentially causing skin damage or sunburn.
Who should avoid Chamomile
Pregnant and breastfeeding women should avoid chamomile due to potential risks to fetal development and lack of safety data. Individuals with allergies to plants in the Asteraceae family (e.g., ragweed, daisies, chrysanthemums) should not use chamomile. People with hormone-sensitive conditions, such as breast cancer or endometriosis, should consult a healthcare provider before use. Those with liver or kidney problems, as well as individuals scheduled for surgery, should avoid chamomile. Children under six years old should not use chamomile without professional guidance.
Interaction with medications
Chamomile may interact with various medications, potentially affecting their efficacy or increasing side effects. It can enhance the effects of blood-thinning drugs like warfarin, increasing the risk of bleeding. Chamomile may interact with sedatives, anticonvulsants, and antidepressants, causing excessive drowsiness. It can interfere with the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6, affecting medications such as statins, birth control pills, and some antifungals. Always consult a healthcare provider before combining chamomile with any medications, especially those affecting blood clotting or liver function.
9. Lavender

Lavender has shown promising potential as a natural remedy for migraine relief. Clinical studies have demonstrated that lavender, particularly its essential oil, may help reduce the frequency, intensity, and duration of migraine attacks. A randomized, placebo-controlled study found that inhaling lavender essential oil for 15 minutes significantly decreased the severity of migraine headaches compared to a placebo. Lavender’s effectiveness is attributed to its anti-inflammatory, analgesic, and anxiolytic properties, which can help alleviate pain, reduce stress, and promote relaxation – all crucial factors in managing migraines. The active compounds in lavender, such as linalool and linalyl acetate, are believed to modulate pain pathways and reduce neurogenic inflammation associated with migraines. Additionally, lavender’s calming effects may help improve sleep quality and reduce stress, both of which are common migraine triggers.
What Research Says?
- Findings from research done by Journal of Herbal Medicine show Lavender essential oil has been shown to significantly reduce the frequency and severity of migraine attacks when used as a prophylactic therapy over a period of three months.
- As research performed by European Neurology suggests Inhalation of lavender essential oil for 15 minutes significantly reduced headache severity in migraine patients compared to a placebo.
- Research completed by Journal of Medicinal Plants indicates Lavender essential oil also helped in reducing depression associated with chronic migraine, indicating its potential dual benefits for both headache and mood improvement.
- According to investigations conducted by Phytotherapy Research and Alternative and Complementary Therapies, Systematic reviews and studies on various herbal treatments, including lavender, suggest that plant essential oils can effectively relieve migraine symptoms by inhibiting neurogenic inflammation and balancing vasorelaxation.
How to Use
To use lavender for migraine relief, inhale lavender essential oil directly from the bottle or add 2-4 drops to a diffuser for 15-30 minutes during a migraine attack. For topical application, mix 2-3 drops of lavender oil with a carrier oil and gently massage onto temples, forehead, and neck. You can also add a few drops to a warm bath or create a cold compress infused with lavender. Alternatively, drink lavender tea by steeping 1-2 teaspoons of dried lavender flowers in hot water for 10 minutes. Always consult a healthcare professional before starting any new treatment regimen.
Potential side effects of Lavender
Lavender may cause skin irritation, allergic reactions, or contact dermatitis in some individuals. Common side effects include nausea, headache, and increased appetite. Some people may experience drowsiness, dizziness, or constipation. In rare cases, lavender can lead to sun sensitivity, making the skin more susceptible to sunburn. Excessive use or ingestion of lavender essential oil may cause gastrointestinal discomfort, including vomiting and diarrhea.
Who should avoid Lavender
Pregnant and breastfeeding women should avoid using lavender due to potential risks to fetal development and lack of safety data. Individuals with hormone-sensitive conditions, such as breast cancer or endometriosis, should consult a healthcare provider before use. People with known allergies to plants in the Lamiaceae family should avoid lavender. Those scheduled for surgery should stop using lavender at least two weeks prior, as it may interfere with anesthesia. Children, especially young boys, should avoid prolonged use of lavender products due to potential hormonal effects.
Interaction with medications
Lavender may interact with various medications, potentially affecting their efficacy or increasing side effects. It can enhance the effects of central nervous system depressants, including sedatives and anti-anxiety medications, causing excessive drowsiness. Lavender may interact with blood thinners, increasing the risk of bleeding. It can also interfere with the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6, affecting medications such as statins, antidepressants, and some antifungals. Always consult a healthcare provider before combining lavender with any medications.
10. Ginger
Ginger has shown promising potential as a natural remedy for migraine relief. Clinical studies have demonstrated that ginger may help reduce the frequency, intensity, and duration of migraine attacks. A meta-analysis of randomized controlled trials found that ginger treatment was associated with significantly improved pain relief at 2 hours compared to placebo, as well as reduced pain scores. Ginger’s effectiveness is attributed to its anti-inflammatory, analgesic, and antiemetic properties, which can help alleviate pain, reduce nausea, and decrease inflammation associated with migraines. The active compounds in ginger, such as gingerols and shogaols, are believed to modulate pain pathways and inhibit prostaglandin synthesis. Additionally, ginger has been found to be as effective as sumatriptan, a common migraine medication, in achieving headache relief within 2 hours of ingestion, but with fewer side effects.
What Research Says?
- Research efforts by Cephalalgia show that Ginger has been shown to significantly reduce pain and improve functional status within 2 hours of treatment in patients experiencing acute migraine attacks.
- As demonstrated by research from Journal of Clinical Psychiatry, a meta-analysis found that ginger was associated with a higher proportion of patients being pain-free 2 hours after treatment compared to placebo (RR, 1.79; 95% CI, 1.04-3.09).
- Research initiated by The American Journal of Emergency Medicine suggests Ginger also reduced the incidence of migraine-related nausea and vomiting (RR, 0.48; 95% CI, 0.30-0.77).
- According to the research carried out by Phytotherapy Research, Ginger’s effectiveness in treating acute migraine attacks was found to be comparable to sumatriptan, a commonly used migraine medication, with fewer side effects reported for ginger.
- Studies conducted by Cephalalgia indicate studies on the prophylactic use of ginger for migraine prevention have shown mixed results. One study found no significant difference between ginger and placebo in reducing the frequency of migraine attacks.
How to Use
To use ginger for migraine relief, take 250-500 mg of ginger powder or extract at the onset of symptoms. For a natural approach, steep 1-2 teaspoons of freshly grated ginger in hot water for 10 minutes to make a tea. Alternatively, mix 1/8-1/4 teaspoon of powdered ginger in water and drink. For topical relief, dilute ginger essential oil with a carrier oil and apply to temples and neck. Ginger can also be consumed in capsule form, with a typical dose of 550 mg. Always consult a healthcare professional before starting any new treatment regimen.
Potential side effects of Ginger
Ginger may cause gastrointestinal discomfort, including heartburn, diarrhea, and stomach upset, especially when consumed in large quantities. Some individuals may experience allergic reactions, such as skin rashes or breathing difficulties. Excessive consumption can lead to increased bleeding risk, low blood sugar, and low blood pressure. In rare cases, ginger may cause central nervous system depression and arrhythmia. Prolonged use or high doses might result in gastrointestinal irritation and gallstone formation.
Who should avoid Ginger
Pregnant women, particularly in late stages, should limit ginger intake due to potential risks. Individuals with bleeding disorders, gallstones, or scheduled for surgery should avoid ginger. People with low blood pressure or heart conditions should consult a healthcare provider before use. Those with known allergies to plants in the Zingiberaceae family should avoid ginger. Patients with gastrointestinal issues like acid reflux or GERD may need to limit or avoid ginger consumption.
Interaction with medications
Ginger may interact with various medications, potentially affecting their efficacy or increasing side effects. It can enhance the effects of blood-thinning drugs like warfarin, aspirin, and clopidogrel, increasing bleeding risk. Ginger may interact with diabetes medications, potentially causing hypoglycemia. It can also affect the metabolism of drugs processed by liver enzymes CYP3A4 and CYP2D6, impacting medications such as nifedipine, cyclosporine, and metronidazole. Always consult a healthcare provider before combining ginger with any medications.
FAQs
- Can I use more than one herb for migraine relief at the same time?
Yes, you can use a combination of herbs for migraine relief, but it’s important to consult with a healthcare provider before doing so. Some herbs may interact with each other or with medications you are taking, so a professional can guide you on safe combinations and appropriate dosages.
- How long does it take for herbs to show results in migraine prevention?
The time it takes for herbs to show results in migraine prevention can vary based on the herb and the individual. For example, feverfew and butterbur may take several weeks to a few months of consistent use to reduce migraine frequency, while ginger might provide more immediate relief during acute attacks.
- Are herbal treatments for migraine safe for children?
Some herbs, like ginger, may be safe for children in small doses, but other herbs like feverfew and butterbur may not be recommended for young children. It’s important to consult a pediatrician before giving any herbal treatments to children for migraines.
- Are there any dietary restrictions while using herbs for migraines?
While using herbs for migraines, certain dietary restrictions may enhance the efficacy of the herbs. For example, avoiding known migraine triggers like caffeine, alcohol, and foods with preservatives may help reduce the frequency of migraine attacks while using herbal treatments.
- Can herbal treatments for migraines be used during pregnancy?
Not all herbal treatments for migraines are safe during pregnancy. Herbs like feverfew and butterbur should be avoided due to their potential to cause complications. Pregnant women should always consult with a healthcare provider before using any herbal remedies.
- Can herbal treatments be combined with conventional migraine medications?
Some herbal treatments can be combined with conventional migraine medications, but it’s crucial to consult a healthcare provider first. Certain herbs, like ginger, may complement conventional treatments, while others, like feverfew, may interact with medications such as blood thinners.
- Are there any specific herbal remedies for hormonal or menstrual migraines?
Yes, some herbs, such as feverfew and ginger, may help with menstrual migraines. Additionally, other hormone-balancing herbs like black cohosh and chasteberry are sometimes used to manage hormonal migraines, although more research is needed to confirm their effectiveness.
- Can essential oils be used as an alternative to consuming herbs for migraine relief?
Yes, essential oils like peppermint and lavender can be effective for relieving migraine symptoms when applied topically or inhaled. These oils offer an alternative to consuming herbs and may provide faster relief for some individuals.
- How do I know if a migraine trigger is food-related, and can herbs help in managing food-triggered migraines?
Keeping a food diary can help you identify food-related migraine triggers. Once identified, herbs like ginger may help manage symptoms related to food-triggered migraines by reducing nausea and inflammation. However, avoiding the trigger food is the most effective way to prevent such migraines.
- Are there any herbs that can help with migraines accompanied by aura?
Herbs like feverfew and butterbur may help reduce the frequency and severity of migraines with aura, but it’s important to consult with a healthcare provider to determine the best approach. Lavender and chamomile may also provide relief from the stress and anxiety associated with migraines with aura.