Back pain is a multifaceted condition with various definitions depending on the context and specific type of pain being discussed. Low back pain (LBP) is often defined as pain localized in the lower back, lasting for more than 24 hours, and separated by at least one month without pain. Chronic back pain, on the other hand, is typically described as pain persisting for more than 7-12 weeks or beyond the expected period of healing, and it may not always have a clear pathological cause. Recurrent low back pain is characterized by multiple episodes of pain, with the frequency of these episodes being a common defining feature. Additionally, back pain can be classified into different types such as discogenic pain, which is related to internal disc disruption, and radicular pain, often caused by disc herniation or canal stenosis. The complexity of back pain definitions is further compounded by the need for standardized definitions in research to ensure comparability of study results.
Back pain is a multifaceted condition with various definitions depending on the context and specific type of pain being discussed. Low back pain (LBP) is often defined as pain localized in the lower back, lasting for more than 24 hours, and separated by at least one month without pain. Chronic back pain, on the other hand, is typically described as pain persisting for more than 7-12 weeks or beyond the expected period of healing, and it may not always have a clear pathological cause. Recurrent low back pain is characterized by multiple episodes of pain, with the frequency of these episodes being a common defining feature. Additionally, back pain can be classified into different types such as discogenic pain, which is related to internal disc disruption, and radicular pain, often caused by disc herniation or canal stenosis. The complexity of back pain definitions is further compounded by the need for standardized definitions in research to ensure comparability of study results.
Types of Back Pain
Understanding the different types of back pain is crucial for diagnosing the underlying causes and finding the right treatment. In this article, we’ll explore the most common types of back pain, their causes, symptoms, and potential treatments, so you can better manage your condition and find relief.
- Acute back pain
- Subacute back pain
- Chronic back pain
- Nonspecific back pain
- Mechanical back pain
- Radicular back pain
- Axial back pain
- Referred back pain
- Neuropathic back pain
- Inflammatory back Pain
Common Causes of Back pain
Understanding the common causes of back pain is the first step toward finding effective relief and preventing future episodes. In this article, we’ll explore the most frequent culprits behind back pain, from muscle strains and poor posture to more serious underlying conditions, helping you identify what’s triggering your discomfort and how to address it.
- Dermatologic problems and conditions resulting from saddle trauma
- Injured paraspinal muscles
- Supraspinous ligament damage
- Osseous pain and nerve dysfunction related to the spine and sacroiliac area
- Neurologic diseases
- Internal disc disruption (IDD)
- Disc herniation
- Canal stenosis
- Facet joint pain
- Degenerative instability
- Congenital anomalies
- Degenerative changes
- Inflammation
- Cancer
- Injuries
- Muscle and joint overload
- Metabolic disorders
- Psychological and social problems
- Spinal cord compression by metastatic tumor
- Intervertebral disc pathologies
- Dynamic instabilities
- Spondylosis and stenosis
- Spondylolisthesis
- Osteoporotic compression fractures
- Spinal infections
- Nonspecific pain or muscle strain
- Herniated disk
- Spondylolysis
- Scoliosis
- Scheuermann’s kyphosis
- Tumor
- Infection
- Sickle cell crisis
- Nociceptive and neuropathic pain
- Traumatic injury
- Radiculopathy and cauda equina syndrome
- Stress and anxiety
- Fibromyalgia
- Injuries from accidents or falls
- Pregnancy
- Sleeping on a poor mattress
- Wearing high heels frequently
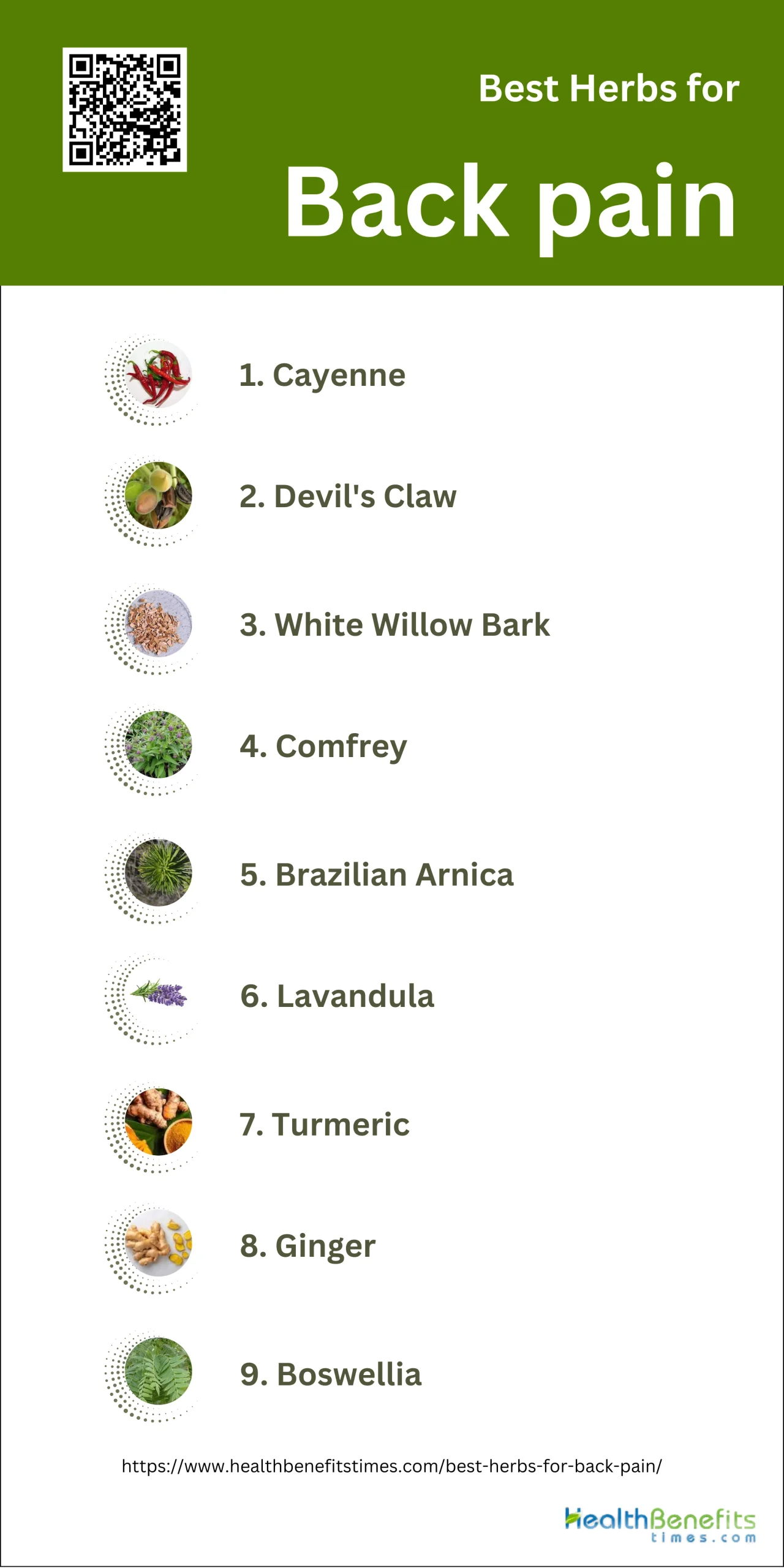
Best herbs for Back pain
Using herbs to care for back pain instead of medication offers several advantages, primarily due to their potential for fewer side effects and lower risk of addiction. Herbal remedies such as Harpagophytum procumbens (devil’s claw), Salix alba (white willow bark), and Capsicum frutescens (cayenne) have shown efficacy in reducing pain more than placebo, with some studies indicating their equivalence to conventional pain medications like rofecoxib. Additionally, herbs like Symphytum officinale L. (comfrey) and Solidago chilensis (Brazilian arnica) have demonstrated benefits in improving pain and function in patients with low back pain. Unlike conventional medications, which can lead to tolerance and addiction, herbal treatments are generally associated with fewer adverse effects, making them a safer long-term option for managing chronic pain. Moreover, the use of herbal medicine aligns with the growing preference for complementary and alternative medicine (CAM) among patients seeking holistic and integrative approaches to health care.
1. Cayenne
Cayenne pepper, a potent natural remedy, has shown promising benefits for alleviating back pain. This fiery spice contains capsaicin, a compound known for its powerful pain-relieving properties. When applied topically, cayenne can help reduce inflammation and numb pain receptors, offering relief to sore back muscles. Additionally, consuming cayenne orally may improve circulation, promoting healing and reducing stiffness in the back. Some studies suggest that capsaicin can deplete substance P, a neurotransmitter that sends pain signals to the brain, potentially providing long-term pain management. While more research is needed, many people find that incorporating cayenne into their pain management routine, either through topical creams or dietary supplements, can offer a natural alternative to traditional pain medications.
What Research Says?
- Based on research carried out by Cochrane Database of Systematic Reviews, Cayenne pepper (Capsicum frutescens) reduces pain more effectively than placebo in individuals with chronic low back pain.
- As per studies undertaken by Cochrane Database of Systematic Reviews, Capsicum frutescens cream or plaster shows favorable results in reducing pain compared to placebo in people with chronic low back pain.
- According to investigations conducted by Journal Of Pharmacy and Science, Cayenne pepper gel exhibits anti-inflammatory effects in animal models, although it is not as effective as some standard treatments like Voltaren® Emulgel.
- As demonstrated by research from European Journal of Translational Myology, A 5% concentration of Cayenne pepper in cataplasm is optimal for pain relief without significant side effects, as higher concentrations do not provide additional benefits.
How to Use
One popular method is to create a warming tea by mixing 1/4 to 1/2 teaspoon of cayenne powder with hot water and a splash of lemon juice; this can be sipped slowly to help reduce inflammation and improve circulation. For those who prefer supplements, cayenne capsules are available and can be taken as directed, typically with meals to minimize stomach irritation. Adding fresh or dried cayenne peppers to your meals is another tasty way to incorporate this spice into your diet. For topical application, cayenne-infused creams or ointments can be gently massaged into the affected area, but it’s crucial to do a patch test first to ensure no skin sensitivity. Some people find relief by mixing cayenne powder with warm coconut oil to create a homemade salve. Remember, while cayenne can be a powerful natural remedy, it’s essential to start with small amounts and gradually increase to avoid digestive discomfort or skin irritation.
Potential side effects of Cayenne
Common side effects include gastrointestinal discomfort, such as stomach irritation, heartburn, and a burning sensation in the mouth and throat. Some people may experience skin irritation or a burning sensation when cayenne is applied topically. In rare cases, high-dose cayenne pepper supplements have been linked to more serious side effects, including irregular heartbeat and elevated blood pressure.
Who should avoid Cayenne
Certain groups of people should be cautious or avoid consuming cayenne pepper. This includes individuals with gastrointestinal disorders such as irritable bowel syndrome (IBS) or gastroesophageal reflux disease (GERD), as cayenne can exacerbate these conditions. Pregnant and breastfeeding women should avoid taking cayenne pepper supplements, as they may lead to heartburn, vomiting, or affect the infant. People with ulcers should limit their consumption of cayenne pepper, as it can irritate the stomach lining.
Interaction with medications
Cayenne pepper can interact with several medications, potentially affecting their efficacy or increasing the risk of side effects. It may interfere with blood-thinning medications such as warfarin, aspirin, naproxen, or ibuprofen, increasing the risk of bleeding. Cayenne can also reduce the effectiveness of stomach acid reducers like cimetidine, famotidine, ranitidine, omeprazole, and esomeprazole. ACE inhibitors used for blood pressure control may interact with cayenne, potentially increasing the risk of cough associated with these medications.
2. Devil’s Claw

Devil’s Claw, a plant native to southern Africa, has shown promising results in alleviating back pain. This herb contains compounds called iridoid glycosides, particularly harpagoside, which possess anti-inflammatory and analgesic properties. Several studies have demonstrated its effectiveness in reducing lower back pain and improving mobility. In one randomized, double-blind, placebo-controlled trial, participants taking Devil’s Claw extract experienced significant pain relief compared to those taking a placebo. The herb works by inhibiting the production of inflammatory mediators and reducing the perception of pain signals in the body. Additionally, Devil’s Claw may help improve overall joint health and function, making it a potentially valuable natural remedy for individuals suffering from chronic back pain.
What Research Says?
- According to the research carried out by Phytotherapy Research and Der Schmerz, Devil’s Claw has shown significant improvement in pain symptoms and mobility in patients with chronic non-radicular back pain.
- As shown by research done by Phytotherapy Research, Clinical studies indicate a reduction in pain and symptoms of osteoarthritis, with improvements in pain scales and physical function.
- As evidenced by research led by Journal of Primary Health Care and The Journal of Alternative and Complementary Medicine, Devil’s Claw has been found to provide short-term pain relief comparable to conventional treatments like NSAIDs, with fewer adverse effects.
- According to studies led by Phytochemistry Reviews and Holistic Nursing Practice, the herb’s efficacy is attributed to its anti-inflammatory and analgesic properties, although the exact mechanisms are still under investigation.
- Based on research carried out by The orthopedist, Studies report good tolerability and minor adverse effects, such as mild gastrointestinal issues, making it a safer alternative to synthetic analgesics.
How to Use
The most common and convenient method is through standardized capsules or tablets, typically containing 50-100 mg of harpagoside, the active compound. These supplements are usually taken 2-3 times daily with meals. Alternatively, Devil’s Claw can be consumed as a tea by steeping 1-2 teaspoons of dried root in hot water for 8-10 minutes. For those who prefer liquid extracts, tinctures are available and can be added to water or juice, with dosages typically ranging from 0.5-1 ml taken three times daily. Topical applications, such as creams or ointments containing Devil’s Claw extract, can also be applied directly to the affected area for localized relief.
Potential side effects of Devil’s Claw
The most common adverse reactions include gastrointestinal disturbances such as diarrhea, nausea, vomiting, and stomach pain. Some individuals may experience headaches, ringing in the ears (tinnitus), loss of appetite, or changes in their sense of taste. In rare cases, more serious side effects have been reported, including allergic skin reactions, changes in blood pressure, and abnormal heart rhythms. There have also been isolated reports of Devil’s Claw causing bleeding issues and potentially worsening gallstone problems.
Who should avoid Devil’s Claw
Pregnant and breastfeeding women should not use this herb due to potential risks to the fetus or infant. Individuals with heart conditions, including high or low blood pressure, should consult their healthcare provider before using Devil’s Claw, as it may affect heart rate and blood pressure. People with gallstones should avoid it due to its potential to increase bile production. Those with peptic ulcers or other gastrointestinal disorders should also be cautious, as Devil’s Claw may increase stomach acid production. Diabetics should monitor their blood sugar levels closely if using Devil’s Claw, as it may affect blood glucose levels.
Interaction with medications
Devil’s Claw has the potential to interact with various medications, which can lead to altered drug effectiveness or increased side effects. It may interact with blood-thinning medications such as warfarin, potentially increasing the risk of bleeding. Devil’s Claw can also affect the metabolism of certain drugs processed by the liver, including some antidepressants, anti-anxiety medications, and drugs used to treat HIV, cancer, and other conditions. It may interact with medications for diabetes, potentially enhancing their blood sugar-lowering effects. Devil’s Claw can interfere with the action of antacids and medications that reduce stomach acid.
3. White Willow Bark
White Willow Bark has been used for centuries as a natural remedy for pain relief, including back pain. The bark contains salicin, a compound that the body converts into salicylic acid, which is similar to the active ingredient in aspirin. This natural analgesic and anti-inflammatory property makes White Willow Bark effective in reducing back pain and inflammation. Studies have shown that it can help alleviate acute and chronic lower back pain, as well as provide relief for conditions like osteoarthritis and rheumatoid arthritis. Unlike synthetic pain relievers, White Willow Bark tends to work more slowly but may have longer-lasting effects.
What Research Says?
- As per studies undertaken by the American Journal of Medicine and Rheumatology, Willow bark extract significantly reduces pain in patients with chronic low back pain, with higher doses (240 mg salicin) being more effective than lower doses (120 mg salicin) and placebo.
- According to studies performed by Cochrane Database of Systematic Reviews, Willow bark extract shows comparable effectiveness to the COX-2 inhibitor rofecoxib in reducing pain and improving function in patients with low back pain.
- As demonstrated by research from Phytotherapy Research, The anti-inflammatory effects of willow bark are attributed to the inhibition of inflammatory mediators such as tumor necrosis factor-alpha (TNF-α) and nuclear factor-kappa B (NF-κB), as well as the reduction of cyclooxygenase-2 (COX-2) expression.
- According to the research carried out by Phytomedicine, Long-term use of willow bark extract for musculoskeletal disorders, including back pain, shows good tolerability and can be safely combined with NSAIDs and opioids if necessary.
- As shown by research done by Phytomedicine, Treatment with willow bark extract is less expensive compared to synthetic COX-2 inhibitors, making it a cost-effective option for managing low back pain.
How to Use
The most common method is through standardized capsules or tablets, typically containing 120-240 mg of salicin, taken 1-2 times daily. For those who prefer a more traditional approach, White Willow Bark tea can be prepared by steeping 1-2 teaspoons of dried bark in hot water for 10-15 minutes. Tinctures are another option, with a typical dose being 1-2 ml taken three times daily, mixed with water or juice. Some people opt for powdered White Willow Bark, which can be added to smoothies or sprinkled over food. Topical applications, such as creams or ointments containing White Willow Bark extract, can also be applied directly to the affected area for localized relief.
Potential side effects of White Willow Bark
Common side effects include gastrointestinal discomfort, such as nausea, stomach upset, and diarrhea. Some individuals may experience headaches, dizziness, or ringing in the ears (tinnitus). Skin reactions, including itching and rashes, have been reported in some cases, especially in people with aspirin sensitivity. In rare instances, more severe side effects can occur, such as increased bleeding risk, allergic reactions, and liver or kidney problems.
Who should avoid White Willow Bark
Several groups of people should exercise caution or avoid using White Willow Bark altogether. This includes individuals with known allergies or sensitivities to aspirin or other salicylates, as they may experience similar reactions to White Willow Bark. People with bleeding disorders, peptic ulcers, or other gastrointestinal conditions should avoid its use due to the increased risk of stomach irritation and bleeding. Pregnant and breastfeeding women should not use White Willow Bark, as its safety during pregnancy and lactation has not been established.
Interaction with medications
White Willow Bark can interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. It may enhance the effects of blood-thinning medications such as warfarin, aspirin, and other anticoagulants, increasing the risk of bleeding. White Willow Bark can also interact with nonsteroidal anti-inflammatory drugs (NSAIDs), potentially increasing the risk of gastrointestinal side effects. It may interfere with the action of beta-blockers and diuretics, reducing their effectiveness in treating heart conditions and high blood pressure. Additionally, White Willow Bark can interact with methotrexate and phenytoin, potentially leading to toxic levels of these drugs in the body.
4. Comfrey

Comfrey, a plant with a long history of traditional use, has shown potential benefits for alleviating back pain. The herb contains compounds called allantoin and rosmarinic acid, which possess anti-inflammatory and pain-relieving properties. These active ingredients can help reduce swelling and promote healing of damaged tissues. When applied topically, comfrey has been found to be particularly effective in treating acute lower back pain. Comfrey ointments or creams can significantly reduce pain intensity and improve mobility in individuals suffering from back pain. The herb works by penetrating the skin and targeting the affected area directly, providing localized relief.
What Research Says?
- As evidenced by research led by British Journal of Sports Medicine, Multiple randomized controlled trials (RCTs) have demonstrated that comfrey root extract ointment significantly reduces acute upper and lower back pain compared to placebo. Patients experienced a marked reduction in pain intensity, with some studies reporting up to a 95.2% decrease in pain on active movement.
- According to studies led by Planta Medica and Phytotherapy Research, Comfrey root extract combined with methylnicotinate (MN) also showed superior efficacy in reducing back pain compared to MN alone and placebo, with significant improvements in pain scores and patient satisfaction.
- Based on research carried out by Complementary Therapies in Medicine and Advances in Therapy, the topical application of comfrey root extract is generally safe with few adverse events reported. Studies indicate good to excellent tolerability among patients.
How to Use
The most common and recommended method of application is through creams, ointments, or salves containing comfrey extract. These topical preparations are typically applied directly to the affected area of the back 3-4 times daily, or as directed on the product label. When using comfrey-based products, gently massage the cream or ointment into the skin until it’s fully absorbed. Some people find it helpful to apply a warm compress over the area after application to enhance absorption and provide additional soothing relief. It’s crucial to use only products specifically formulated for external use and to follow the manufacturer’s instructions carefully.
Potential side effects of Comfrey
Comfrey, while traditionally used for various medicinal purposes, can cause several serious side effects, particularly when taken internally or used extensively. The most concerning side effect is liver damage, which can be severe and potentially fatal. This is due to the pyrrolizidine alkaloids present in comfrey, which are toxic to the liver. Other potential side effects include lung damage, cancer, and veno-occlusive disease (a condition where small veins in the liver become obstructed).
Who should avoid Comfrey
Pregnant and breastfeeding women should not use comfrey due to the risk of birth defects and potential harm to the infant. Children should never be given comfrey orally or have it applied to their skin. Individuals with liver disease, alcoholism, or cancer should avoid comfrey entirely. People with a history of liver problems or those taking medications that affect the liver should also steer clear of comfrey. Additionally, comfrey should not be used by anyone with broken or damaged skin, as this can increase the absorption of toxic compounds.
Interaction with medications
Comfrey can interact with various medications, potentially increasing the risk of adverse effects or altering the effectiveness of certain drugs. It may enhance the effects of blood-thinning medications such as warfarin, aspirin, and other anticoagulants, increasing the risk of bleeding. Comfrey can also interact with nonsteroidal anti-inflammatory drugs (NSAIDs), potentially increasing the risk of gastrointestinal side effects. It may interfere with the action of medications that affect liver function, including acetaminophen and certain antidepressants.
5. Brazilian Arnica
Brazilian Arnica, also known as Lychnophora ericoides, is a plant native to Brazil that has gained recognition for its potential benefits in alleviating back pain. This herb contains compounds with anti-inflammatory and analgesic properties, making it a popular natural remedy in traditional Brazilian medicine. The active ingredients in Brazilian Arnica, including flavonoids and sesquiterpene lactones, work to reduce inflammation and provide pain relief when applied topically. Unlike its European counterpart (Arnica montana), Brazilian Arnica is considered safer for internal use, although topical application remains the most common method for treating back pain. Studies have shown that Brazilian Arnica can help reduce muscle soreness, joint pain, and inflammation associated with various types of back pain, including lower back pain and sciatica.
What Research Says?
- As per studies undertaken by Cochrane Database of Systematic Reviews and Phytotherapy Research, a study found that a gel containing Brazilian Arnica significantly reduced pain perception and improved flexibility in patients with lumbago when applied twice daily for 15 days compared to a placebo.
- According to studies performed by Phytotherapy Research, Another study confirmed the pain-reducing effects of Brazilian Arnica in treating tendonitis, showing significant pain reduction in the test group compared to the placebo group.
- According to investigations conducted by Medicines, Arnica, including Brazilian Arnica, has shown promising effects for pain relief in various conditions, including low back pain, due to its anti-inflammatory and antioxidant properties.
- As demonstrated by research from Cochrane Database of Systematic Reviews, a review highlighted that while Brazilian Arnica and other herbal medicines like Capsicum frutescens and Harpagophytum procumbens reduce pain more than placebo, the evidence quality is moderate at best, necessitating further well-designed trials.
How to Use
Brazilian Arnica is primarily used topically for back pain relief, although internal use is considered safer compared to its European counterpart. The most common and effective method of application is through creams, ointments, or gels containing Brazilian Arnica extract. These topical preparations should be gently massaged into the affected area of the back 2-3 times daily, or as directed on the product label. Some practitioners recommend using Brazilian Arnica oil, which can be diluted with a carrier oil like coconut or jojoba oil before application. For those who prefer internal use, Brazilian Arnica tinctures or capsules are available, but it’s crucial to follow the recommended dosage and consult with a healthcare professional before ingesting any form of the herb.
Potential side effects of Brazilian Arnica
Brazilian Arnica (Solidago chilensis or Lychnophora ericoides) may cause several side effects, particularly when used in high doses or for extended periods. Common side effects include gastrointestinal discomfort, such as nausea, stomach irritation, and diarrhea. Topical application may lead to skin reactions like rashes, itching, or contact dermatitis in sensitive individuals. When taken orally, especially in high concentrations, more severe side effects can occur, including liver and kidney toxicity. Some studies have reported hepatotoxicity and nephrotoxicity following histopathological analysis in animal models.
Who should avoid Brazilian Arnica
Several groups of people should exercise caution or avoid using Brazilian Arnica altogether. Pregnant and breastfeeding women should not use Brazilian Arnica due to potential risks to the fetus or infant, as its safety during pregnancy and lactation has not been established. Individuals with liver or kidney problems should avoid Brazilian Arnica, especially in oral form, due to the potential for hepatotoxicity and nephrotoxicity. People with allergies to plants in the Asteraceae family (which includes ragweed, chrysanthemums, and daisies) should be cautious, as Brazilian Arnica may cause allergic reactions in sensitive individuals.
Interaction with medications
Brazilian Arnica may interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. It may enhance the effects of blood-thinning medications such as warfarin, aspirin, and other anticoagulants, increasing the risk of bleeding. Brazilian Arnica might interact with nonsteroidal anti-inflammatory drugs (NSAIDs), potentially increasing the risk of gastrointestinal side effects. It may interfere with the action of medications that affect liver function, including acetaminophen and certain antidepressants. Due to its potential effects on blood clotting, Brazilian Arnica should not be used in combination with antiplatelet drugs.
6. Lavandula

Lavandula, commonly known as lavender, has shown promising benefits for alleviating back pain. This aromatic herb contains compounds with analgesic and anti-inflammatory properties, making it a natural option for pain relief. Lavender’s active components, including linalool and linalyl acetate, work to reduce inflammation and muscle tension, which are often underlying causes of back pain. Lavender essential oil, when used in aromatherapy or massage, can significantly reduce pain intensity and improve overall well-being in individuals suffering from chronic back pain. The herb’s calming effects also contribute to its pain-relieving properties by promoting relaxation and reducing stress, which can exacerbate back pain.
What Research Says?
- According to the research carried out by Coluna/Columna, Lavender essential oil, when used in massage therapy, significantly reduces spinal pain, including cervical and lumbar regions, in obese women compared to control and placebo groups.
- As shown by research done by Journal of Ethnopharmacology and Revista Brasileira de Farmacognosia, Lavender essential oil and extracts have demonstrated significant analgesic and anti-inflammatory effects in various pain models, including formalin and acetic acid-induced pain in mice. These effects are comparable to those of standard pain relief medications like morphine and dexamethasone.
- As evidenced by research led by Journal of Neuroimmunology, The analgesic effects of lavender essential oil are mediated through the activation of peripheral and central opioid and cannabinoid receptors, suggesting a complex mechanism involving multiple pathways.
How to Use
The most common and effective method is through aromatherapy using lavender essential oil. You can add 5-10 drops of lavender oil to a diffuser or inhale it directly from the bottle for 10-15 minutes, 2-3 times daily. For topical application, dilute 2-3 drops of lavender essential oil in a tablespoon of carrier oil (such as coconut or jojoba oil) and gently massage it into the affected area of your back. Alternatively, you can add 10-15 drops of lavender oil to a warm bath and soak for 15-20 minutes to help relax muscles and reduce pain. Lavender tea is another option, which can be prepared by steeping 1-2 teaspoons of dried lavender flowers in hot water for 5-10 minutes. Drink this tea 1-2 times daily for its calming and pain-relieving effects.
Potential side effects of Lavandula
The most common side effects include gastrointestinal discomfort, such as constipation, diarrhea, or increased appetite. Some people may experience headaches or drowsiness, especially when using lavender essential oil or taking it in high doses. Topical application of lavender products can occasionally lead to skin irritation or allergic reactions in sensitive individuals, manifesting as rashes or dermatitis.
Who should avoid Lavandula
Several groups of people should exercise caution or avoid using Lavandula altogether. Pregnant and breastfeeding women should avoid lavender due to a lack of sufficient safety data and potential hormonal effects. Young boys who haven’t reached puberty should not use lavender products topically, as it may disrupt normal hormones and potentially cause breast growth. Individuals with known allergies to plants in the Lamiaceae family (which includes mint and sage) should be cautious, as they may be more likely to experience allergic reactions to lavender. People scheduled for surgery should discontinue lavender use at least two weeks before the procedure, as it may interact with anesthesia and increase the risk of bleeding.
Interaction with medications
Lavandula can interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. One of the most significant interactions is with central nervous system (CNS) depressants, including sedatives, barbiturates, and benzodiazepines. Lavender may enhance the sedative effects of these medications, potentially leading to excessive drowsiness or respiratory depression. It may also interact with blood-thinning medications like warfarin, aspirin, and other anticoagulants, increasing the risk of bleeding. Lavender can potentially interfere with the action of cholesterol-lowering drugs and diabetes medications. Additionally, it may interact with drugs metabolized by the liver’s cytochrome P450 system, which includes many antidepressants, antipsychotics, and some antibiotics.
7. Turmeric
Turmeric, a vibrant yellow spice commonly used in Indian cuisine, has shown promising potential in alleviating back pain due to its potent anti-inflammatory properties. The active compound in turmeric, called curcumin, has been found to inhibit inflammatory enzymes and reduce pain-causing molecules in the body. Curcumin can be as effective as some over-the-counter pain medications in reducing inflammation and discomfort associated with various types of back pain, including osteoarthritis and rheumatoid arthritis. Additionally, turmeric’s antioxidant properties may help protect against oxidative stress and tissue damage, potentially supporting overall spine health and reducing the risk of chronic back pain conditions.
What Research Says?
- According to studies led by Nutrients, Turmeric bioactive compounds, such as curcumin and bisdemethoxycurcumin, significantly decrease mechanical hypersensitivity and reduce markers of glial activation, oxidative stress, and mitochondrial dysfunction in neuropathic pain models.
- Based on research carried out by Journal of Vocational Health Studies, combined therapy of acupuncture and turmeric significantly reduces the scale and frequency of low back pain, demonstrating a reduction from pain scale 8 to 0 and spasm scale from 3 to 0.
- As per studies undertaken by JURNAL KEPERAWATAN DAN FISIOTERAPI (JKF), Turmeric extract, when combined with acupressure, effectively reduces the intensity of low back pain in primary dysmenorrhea.
- According to studies performed by Journal of Vocational Health Studies, a combination of Swedish massage, acupressure, and turmeric herbs significantly alleviates low back pain, with turmeric’s curcumin inhibiting pain-related enzymes.
- As demonstrated by research from Phytotherapy Research, Turmeric and its active constituent, curcumin, possess anti-inflammatory, antinociceptive, and antioxidant effects, making them beneficial for various inflammatory disorders and pain, including neuropathic pain.
How to Use
To harness the potential benefits of turmeric for back pain, there are several effective ways to incorporate it into your daily routine. The most common method is to consume turmeric as a supplement in capsule form, typically containing 500-2000mg of curcumin per day, depending on the severity of pain and individual needs. Alternatively, you can add fresh or powdered turmeric to your meals, particularly in curries, soups, or smoothies. For enhanced absorption, it’s recommended to combine turmeric with black pepper, as the piperine in black pepper can increase curcumin bioavailability by up to 2000%. Another popular option is to prepare a turmeric latte or “golden milk” by mixing turmeric powder with warm milk (dairy or plant-based) and a pinch of black pepper.
Potential side effects of Turmeric:
The most common side effects include gastrointestinal issues such as nausea, diarrhea, and stomach upset. Some people may experience dizziness, headaches, or skin rashes. In rare cases, high doses of turmeric have been associated with liver problems. Additionally, turmeric may increase the risk of bleeding due to its blood-thinning properties.
Who should avoid Turmeric
Certain individuals should exercise caution or avoid turmeric supplements altogether. Pregnant and breastfeeding women should avoid turmeric supplements, as they may stimulate uterine contractions and potentially lead to complications. People with gallbladder problems, such as gallstones or bile duct obstructions, should also avoid turmeric as it may worsen these conditions. Those with bleeding disorders or scheduled for surgery should consult their healthcare provider before using turmeric due to its blood-thinning effects.
Interaction with medications
Turmeric can interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. It may enhance the effects of blood-thinning medications like warfarin, aspirin, and clopidogrel, increasing the risk of bleeding. Turmeric can also interact with diabetes medications, potentially leading to hypoglycemia (low blood sugar). It may interfere with the action of antacids and increase stomach acid production when taken with drugs that reduce stomach acid. Additionally, turmeric can interact with certain chemotherapy drugs, statins, and medications metabolized by CYP450 enzymes.
8. Ginger

Ginger, a popular root known for its pungent flavor and medicinal properties, has shown promising potential in alleviating back pain. This natural remedy contains potent anti-inflammatory compounds, primarily gingerols and shogaols, which can help reduce inflammation and discomfort associated with various types of back pain. Studies have demonstrated that ginger can be as effective as nonsteroidal anti-inflammatory drugs (NSAIDs) in reducing pain and inflammation, particularly in cases of osteoarthritis and chronic low back pain. The analgesic properties of ginger may help inhibit pain-producing prostaglandins, providing relief from muscle soreness and stiffness.
What Research Says?
- As shown by research done by Phytotherapy Research and Plants (Basel), Ginger reduces pain through multiple mechanisms, including inhibition of prostaglandins, antioxidant activity, and modulation of pain receptors.
- As evidenced by research led by Complementary Therapies in Medicine, One study found that Swedish massage with aromatic ginger oil significantly reduced pain in patients with chronic low back pain.
- According to studies led by Family Medicine, Another study demonstrated that a standardized extract of ginger root significantly decreased pain intensity and improved quality of life in patients with low back pain over two months.
- Based on research carried out by Electronic Journal of General Medicine, Ginger supplementation led to significant reductions in inflammatory markers (CRP, IL-6) and pain severity in adults with low back pain, comparable to vitamin D3.
How to Use
One popular method is consuming ginger tea, which can be made by steeping fresh ginger slices or ginger powder in hot water for 5-10 minutes, optionally adding honey or lemon for flavor. For a more concentrated dose, you can take ginger supplements in capsule form, typically containing 250-1000 mg of ginger extract, following the recommended dosage on the product label. Alternatively, you can add fresh or powdered ginger to your meals, such as stir-fries, soups, or smoothies. Some people find relief by applying ginger topically, either as a compress made with grated ginger wrapped in cloth and applied to the affected area, or by using ginger-infused creams or oils.
Potential side effects of Ginger
The most common side effects include gastrointestinal discomfort, such as heartburn, diarrhea, and stomach upset. Some people may experience bloating, gas, or nausea. In rare cases, ginger might cause mouth irritation, throat discomfort, or a burning sensation. High doses of ginger (more than 4 grams per day) may increase the risk of bleeding due to its blood-thinning properties.
Who should avoid Ginger
Certain groups of people should exercise caution or avoid ginger altogether. Pregnant women, especially those in late stages of pregnancy, should consult their healthcare provider before consuming ginger, as high doses might increase the risk of complications. Individuals with bleeding disorders or those taking blood thinners should be cautious due to ginger’s potential to increase bleeding risk. People with gallbladder issues, such as gallstones, should avoid ginger as it can increase bile production. Those scheduled for surgery should stop consuming ginger at least two weeks before the procedure to prevent excessive bleeding.
Interaction with medications
Ginger can interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. It may enhance the effects of blood-thinning medications like warfarin, aspirin, and clopidogrel, increasing the risk of bleeding. Ginger can also interact with diabetes medications, potentially leading to hypoglycemia when combined with insulin or oral diabetes drugs. It may interfere with blood pressure medications, causing blood pressure to drop too low when used alongside antihypertensive drugs. Ginger might counteract the effects of immunosuppressant medications.
9. Boswellia
Boswellia, also known as Indian frankincense, has emerged as a promising natural remedy for back pain due to its potent anti-inflammatory properties. The active compounds in Boswellia, particularly boswellic acids, have been shown to inhibit the production of inflammatory molecules in the body, potentially reducing pain and swelling associated with various types of back pain, including osteoarthritis and rheumatoid arthritis. Boswellia extract can be as effective as some non-steroidal anti-inflammatory drugs (NSAIDs) in managing chronic low back pain, with the added benefit of fewer side effects. Boswellia’s ability to improve blood flow to joints and prevent the breakdown of cartilage may contribute to its pain-relieving effects and support overall spine health.
What Research Says?
- As per studies undertaken by Cochrane Database of Systematic Reviews and Annals of the Rheumatic Diseases, High-quality evidence indicates that Boswellia serrata extract significantly reduces pain and improves physical function in osteoarthritis patients. Studies show a reduction in pain scores and an improvement in function scores compared to placebo.
- According to studies performed by BMC Complementary Medicine and Therapies, a meta-analysis of randomized controlled trials found that Boswellia serrata effectively relieves pain and stiffness and improves joint function in osteoarthritis patients.
- As demonstrated by research from Nutrients, Combining Boswellia serrata with other supplements, such as omega-3 fatty acids, has shown additional benefits in reducing pain and improving quality of life and functionality in patients with persistent knee pain.
How to Use
The most common and convenient method is to take Boswellia as a supplement in capsule or tablet form, typically containing 300-500 mg of Boswellia extract standardized to 60% boswellic acids. For optimal results, it’s generally recommended to take the supplement two to three times daily with meals, or as directed by a healthcare professional. Some people prefer to use Boswellia in its traditional form as frankincense resin, which can be chewed or made into a tea by steeping small pieces in hot water. Topical application is another option, with Boswellia-infused creams or oils available for direct application to the affected area.
Potential side effects of Boswellia
Common side effects include gastrointestinal discomfort, such as stomach pain, nausea, acid reflux, and diarrhea. Some individuals may experience headaches, skin rashes, or itching. In rare cases, people have reported general weakness or swelling. When applied topically, Boswellia may cause allergic skin reactions in some users. It’s important to note that these side effects are typically mild and tend to resolve on their own.
Who should avoid Boswellia
Certain groups of people should exercise caution or avoid using Boswellia altogether. Pregnant and breastfeeding women should not use Boswellia, as it may stimulate blood flow in the uterus and pelvis, potentially leading to miscarriage or other complications. Individuals with autoimmune diseases such as multiple sclerosis, lupus, or rheumatoid arthritis should be cautious, as Boswellia might increase immune system activity and potentially worsen symptoms. People with liver conditions should consult their healthcare provider before using Boswellia, as it may affect liver enzyme function.
Interaction with medications
Boswellia can interact with various medications, potentially altering their effectiveness or increasing the risk of side effects. It may enhance the effects of anti-inflammatory medications, including non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, potentially increasing the risk of bleeding or stomach irritation. Boswellia might interfere with the action of certain medications metabolized by liver enzymes, particularly those affected by Cytochrome P450 1A2 (CYP1A2) and Cytochrome P450 2C19 (CYP2C19). This interaction could potentially increase the effects and side effects of medications such as antidepressants, antipsychotics, and some heart medications. Additionally, Boswellia may interact with blood thinners, potentially increasing the risk of bleeding.
FAQs
- Can I use more than one herb for back pain relief at the same time?
Yes, combining multiple herbs like turmeric, ginger, and Boswellia may enhance pain relief due to their complementary anti-inflammatory and analgesic properties. However, it’s essential to consult a healthcare professional to avoid potential interactions and ensure safety.
- How long should I use herbal remedies before noticing an improvement in back pain?
The time frame can vary depending on the herb and individual response. Some people may notice relief within a few days, while others may take several weeks. Consistent use as per recommended dosage is key to observing results.
- Are there any lifestyle changes I should consider along with herbal remedies for back pain?
Yes, combining herbal remedies with lifestyle changes such as maintaining proper posture, engaging in regular physical activity, managing stress, and using ergonomic furniture can enhance pain relief and prevent recurrence.
- Can herbal remedies completely replace prescription medications for back pain?
Herbal remedies can provide significant relief for many people, but they may not be sufficient for everyone, especially those with severe or chronic back pain. Consult a healthcare professional before replacing any prescribed medication with herbs.
- Is there a risk of developing an allergy to herbal remedies for back pain?
Yes, some individuals may develop an allergic reaction to certain herbs, such as lavender, comfrey, or Brazilian Arnica. It is crucial to perform a patch test before using topical herbal products and consult a healthcare professional if you have known allergies.
- What should I do if I experience side effects from using an herbal remedy for back pain?
If you experience mild side effects like gastrointestinal discomfort or skin irritation, discontinue use and consult a healthcare professional. For severe side effects, seek immediate medical attention.
- Are there any herbs that should be avoided if I have a specific medical condition like diabetes or hypertension?
Yes, some herbs like cayenne, devil’s claw, ginger, and turmeric can interact with medications for diabetes or hypertension. People with these conditions should consult their healthcare provider before using these herbs.
- Can children use herbal remedies for back pain relief?
Generally, herbal remedies are not recommended for children, especially without professional guidance, as they can have unpredictable effects on young bodies and may interact with other medications or supplements.
- Is it safe to use herbal remedies for back pain during pregnancy or breastfeeding?
Most herbal remedies are not recommended during pregnancy or breastfeeding due to potential risks to the mother or child. Always consult with a healthcare provider before using any herbal products during these periods.
- Do herbal remedies for back pain require a prescription?
Most herbal remedies are available over-the-counter and do not require a prescription. However, it is advisable to consult with a healthcare professional before beginning any new herbal treatment, especially if you are taking other medications.