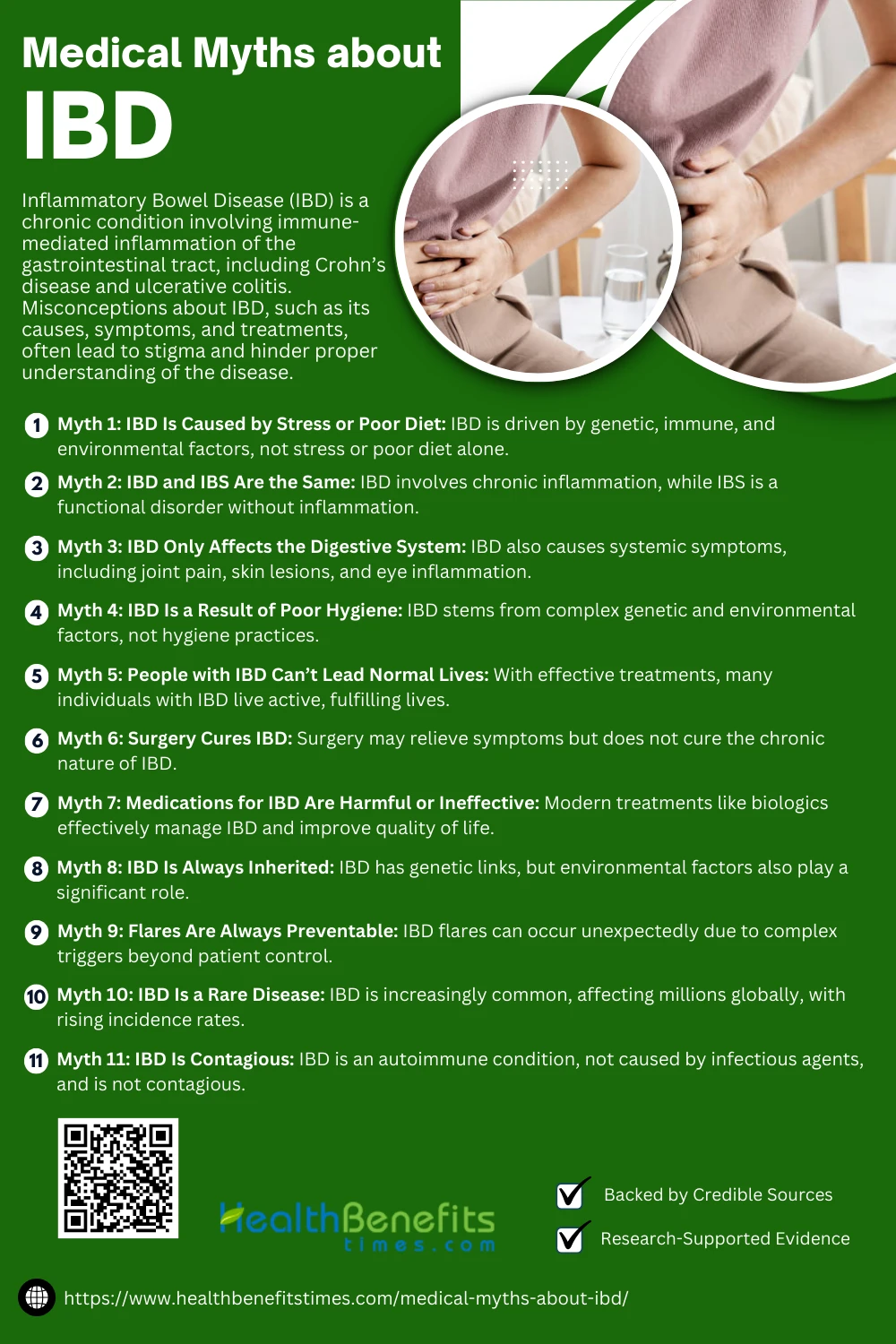
- Inflammatory Bowel Disease (IBD) is a chronic condition involving immune-mediated inflammation of the gastrointestinal tract, including Crohn’s disease and ulcerative colitis.
- Misconceptions about IBD, such as its causes, symptoms, and treatments, often lead to stigma and hinder proper understanding of the disease.
- Addressing these myths with scientific evidence improves awareness, reduces stigma, and empowers patients with accurate knowledge about managing IBD effectively.
 Inflammatory Bowel Disease (IBD) encompasses chronic inflammatory conditions, including Crohn’s disease and ulcerative colitis, that affect the gastrointestinal tract (1). Despite advancements in understanding, misconceptions persist. Myths, such as associating IBD with a direct link to colon cancer, can misguide patients (2). Misconceptions about anemia management in IBD are also prevalent (3). Patients often mistakenly attribute IBD exacerbations solely to NSAID use (4). Myths around fertility concerns and IBD add undue stress to patients (5). The belief that IBD is rooted purely in psychological issues further stigmatizes sufferers (6). Misinformation on diet and its role in triggering IBD symptoms continues to circulate (7). Furthermore, probiotic use is often misunderstood as a definitive cure (8). Addressing these misconceptions is vital to improving patient outcomes (9).
Inflammatory Bowel Disease (IBD) encompasses chronic inflammatory conditions, including Crohn’s disease and ulcerative colitis, that affect the gastrointestinal tract (1). Despite advancements in understanding, misconceptions persist. Myths, such as associating IBD with a direct link to colon cancer, can misguide patients (2). Misconceptions about anemia management in IBD are also prevalent (3). Patients often mistakenly attribute IBD exacerbations solely to NSAID use (4). Myths around fertility concerns and IBD add undue stress to patients (5). The belief that IBD is rooted purely in psychological issues further stigmatizes sufferers (6). Misinformation on diet and its role in triggering IBD symptoms continues to circulate (7). Furthermore, probiotic use is often misunderstood as a definitive cure (8). Addressing these misconceptions is vital to improving patient outcomes (9).
Medical Myths about IBD
Inflammatory Bowel Disease (IBD) is often misunderstood, leading to myths that hinder awareness and treatment. Debunking these misconceptions is crucial for accurate understanding and patient support.
 Myth 1: IBD Is Caused by Stress or Poor Diet
Myth 1: IBD Is Caused by Stress or Poor Diet
The belief that Inflammatory Bowel Disease (IBD) is caused solely by stress or poor diet is a persistent myth. Scientific evidence suggests IBD arises from a combination of genetic predisposition, immune dysregulation, and environmental triggers rather than psychological or dietary factors alone (10). While stress and diet can exacerbate symptoms, they are not primary causes (11).
Fact
Factually, dietary imbalances like high-fat intake may worsen colitis symptoms (12). Psychological stress has been linked to symptom severity but not as a root cause (13). Misconceptions like these hinder patient care by promoting unfounded fears (14). Instead, evidence-based interventions focus on immunological and genetic research (15).
Myth 2: IBD and IBS Are the Same
Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) are often mistakenly considered the same due to overlapping symptoms like abdominal pain and diarrhea. However, IBD is a chronic inflammatory condition affecting the digestive tract, while IBS is a functional disorder with no detectable inflammation (16). IBD can lead to complications such as strictures and malnutrition, unlike IBS (17).
Fact
IBD involves immune dysregulation, while IBS is linked to gut-brain axis disturbances (18). Unlike IBS, IBD shows clear markers like mucosal inflammation (19). Diagnosis of IBD involves endoscopic evaluations, while IBS is diagnosed symptomatically (4). Furthermore, IBD has autoimmune characteristics absent in IBS (8).
Myth 3: IBD Only Affects the Digestive System
Inflammatory Bowel Disease (IBD) is often mischaracterized as affecting only the digestive system. While IBD primarily involves inflammation in the gastrointestinal tract, it also causes extraintestinal manifestations like joint pain, skin lesions, and eye inflammation (20). Such systemic effects arise from immune dysregulation, impacting various organs (2).
Fact
IBD can lead to conditions like primary sclerosing cholangitis, affecting the liver (21). Arthritis is a common extraintestinal symptom in IBD patients (7). Additionally, complications like anemia and osteoporosis have been observed (4). These systemic impacts highlight the importance of comprehensive management beyond gut health (22).
Myth 4: IBD Is a Result of Poor Hygiene
The misconception that Inflammatory Bowel Disease (IBD) results from poor hygiene is unfounded. IBD is primarily caused by genetic, immunological, and environmental factors, not cleanliness levels (20). In fact, the hygiene hypothesis suggests that improved sanitation and reduced microbial exposure might increase autoimmune conditions like IBD (23).
Fact
Studies reveal that areas with higher hygiene standards often have increased IBD prevalence due to altered microbiomes (24). Exposure to specific gut bacteria or helminths may even protect against IBD (25). Poor hygiene has no direct correlation with disease onset (26). These findings emphasize the complexity of IBD causation beyond simplistic hygiene-related myths (27).
Myth 5: People with IBD Can’t Lead Normal Lives
The notion that individuals with Inflammatory Bowel Disease (IBD) cannot lead normal lives is a myth. With advancements in treatment, including biologics and dietary management, many IBD patients achieve remission and maintain high quality of life (20). Effective coping mechanisms and access to healthcare further support their well-being (13).
Fact
IBD patients can engage in daily activities, pursue careers, and maintain relationships (28). Physical symptoms, while challenging, are manageable with tailored interventions (29). The integration of mental health support combats stigma and improves life satisfaction (30). Research underscores that modern therapies enable individuals to lead fulfilling lives despite their condition (11).
Myth 6: Surgery Cures IBD
The idea that surgery cures Inflammatory Bowel Disease (IBD) is a common misconception. While surgical removal of the colon can alleviate symptoms in ulcerative colitis, it does not cure the underlying immune dysregulation or prevent extraintestinal manifestations (31). For Crohn’s disease, surgery often addresses complications but cannot eliminate the disease entirely (32).
Fact
Patients undergoing surgery frequently require ongoing treatments, including biologics and immunosuppressants, to manage disease activity (33). Post-surgical recurrence is common in Crohn’s, underscoring the chronic nature of IBD (11). These facts emphasize the importance of viewing surgery as part of a comprehensive treatment strategy, not a definitive cure (20).
Myth 7: Medications for IBD Are Harmful or Ineffective
The belief that medications for Inflammatory Bowel Disease (IBD) are harmful or ineffective is a misconception. Modern treatments, such as biologics and immunosuppressants, significantly improve patient outcomes by controlling inflammation and preventing complications (33). Although side effects may occur, proper monitoring ensures safety (8).
Fact
Biologics like infliximab effectively reduce disease activity and improve quality of life (29). Corticosteroids are helpful for acute flare-ups but require caution to avoid long-term effects (11). Probiotics can also support gut health alongside medications (34).
Myth 8: IBD Is Always Inherited
The belief that Inflammatory Bowel Disease (IBD) is always inherited is a myth. While genetics play a role, not everyone with IBD has a family history of the condition. Studies reveal that environmental factors, such as diet and gut microbiota, also significantly contribute to IBD development (10). For example, infections and antibiotic usage have been linked to disease onset (25).
Fact
While Crohn’s disease has a stronger genetic component, with specific risk genes identified (35), most individuals do not inherit the condition directly. Ulcerative colitis appears less linked to inheritance (36). This complexity highlights the interplay of genetic predisposition and environmental triggers (37).
Myth 9: Flares Are Always Preventable
The myth that flares in Inflammatory Bowel Disease (IBD) are always preventable misrepresents the condition. Flares result from complex factors, including immune dysregulation, genetic predisposition, and environmental triggers like infections or stress (35).
Fact
IBD flares can occur unpredictably even with diligent management (38). External factors like viral infections or medication changes are common triggers (39).
Myth 10: IBD is a rare disease
he claim that Inflammatory Bowel Disease (IBD) is a rare disease is a myth. IBD, including Crohn’s disease and ulcerative colitis, affects millions worldwide, with increasing incidence rates in both developed and developing countries (7). Studies show IBD prevalence in the U.S. alone exceeds 3 million people (40).
Fact
IBD’s rising global presence is attributed to factors like diet and urbanization (41). Historical views that IBD was rare are outdated as modern diagnostics reveal otherwise (42). Increased awareness and research have identified previously underdiagnosed populations (9.). These findings emphasize IBD’s commonality rather than rarity (17).
Myth 11: IBD is contagious
The misconception that Inflammatory Bowel Disease (IBD) is contagious is false. IBD, encompassing Crohn’s disease and ulcerative colitis, is an autoimmune condition caused by genetic predispositions and environmental factors, not by infectious agents (43). Unlike infectious diseases, IBD does not spread from person to person (44).
Fact
Stigma related to IBD’s perceived contagiousness exacerbates patient isolation (28). Education about the condition’s non-infectious nature is crucial (45). While bacteria like Mycobacterium avium have been studied, they do not prove contagiousness (46).
Differences between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS).
| Aspect | Inflammatory Bowel Disease (IBD) | Irritable Bowel Syndrome (IBS) |
| Definition | Chronic autoimmune disease causing inflammation and damage to the GI tract. | Functional GI disorder with no visible inflammation or damage. |
| Conditions Included | Crohn’s disease, ulcerative colitis. | IBS-C (constipation-predominant), IBS-D (diarrhea-predominant), IBS-M (mixed). |
| Cause | Autoimmune response, genetic factors, environmental triggers. | Gut-brain axis dysregulation, stress, food sensitivities. |
| Pathology | Structural damage to the GI tract, such as ulcers, strictures, and fistulas. | No structural damage or inflammation; altered gut motility. |
| Symptoms | Diarrhea (often bloody), abdominal pain, weight loss, fatigue, fever. | Abdominal cramps, bloating, alternating diarrhea and constipation. |
| Extra-intestinal Symptoms | Joint pain, skin rashes, eye inflammation, liver issues. | None. |
| Diagnostic Tests | Endoscopy, colonoscopy, imaging (CT/MRI), blood tests for inflammation. | Diagnosed using Rome IV criteria; tests rule out other conditions. |
| Treatment | Anti-inflammatory drugs, immunosuppressants, biologics, surgery if needed. | Dietary changes, stress management, antispasmodics, probiotics. |
| Prognosis | Chronic condition with flares and remission, can lead to complications. | Does not cause permanent damage; symptoms vary by triggers. |
| Complications | Strictures, fistulas, malnutrition, increased cancer risk. | None, as IBS does not cause structural damage. |
How to Address Myths and Educate Others
Educating others about Inflammatory Bowel Disease (IBD) involves addressing myths through factual awareness and empathy. Sharing accurate information, like the non-contagious nature of IBD, dispels misconceptions (9). Highlighting the effectiveness of modern therapies reduces fear (29). Peer support groups help combat stigma (28). Raising awareness through campaigns in diverse communities addresses cultural misunderstandings (47). Collaborative strategies with healthcare providers improve public education (13).
Conclusion
Understanding and debunking medical myths about IBD is essential for fostering awareness, reducing stigma, and empowering patients. Misconceptions can lead to misinformation, delayed treatment, and unnecessary fears, but with accurate knowledge, individuals can better manage their condition and support others. IBD is a complex, manageable disease requiring a holistic approach involving medical care, lifestyle adjustments, and emotional support. By addressing these myths, we can promote informed discussions, encourage timely interventions, and improve the quality of life for those living with IBD. Always rely on trusted medical professionals and evidence-based resources for guidance.
References:
- James, S.D., et al. The MYTHS of De Novo Crohn’s Disease.
- Sachar, D.B. Cancer in Crohn’s Disease: Dispelling the Myths.
- Gisbert, J.P., Gomollón, F. Common Misconceptions in Anemia Management.
- Kefalakes, H., et al. NSAIDs and IBD Exacerbations: Myth or Reality?.
- Ellul, P., et al. Reproductive Health Myths in Women With IBD.
- Casati, J., et al. Patient Concerns With IBD.
- Hunt, R.H., et al. Myths About Anti-Inflammatory Drugs.
- Wah, C.S. Probiotics: Myths and Clinical Use.
- Rajindrajith, S., et al. Childhood Constipation and Misconceptions.
- Zingone, F., et al. Food Intolerance Myths and Facts.
- Wright, A.M. Psychosomatic Mislabeling of Crohn’s Disease.
- Zhang, X., et al. High-Fat Diet and Colitis.
- Kemp, K., et al. Health Needs of IBD Patients.
- Verbanac, D., et al. Nutrition Myths in IBD.
- Wu, J.C.Y. Facts About Complementary Medicine for IBS.
- Quigley, E.M.M. IBS and IBD: Interrelated Diseases?.
- Pomirleanu, C., et al. Paradoxical Crohn’s Disease.
- Sahoo, S., Padhy, S.K. Psychological Issues in IBS.
- Rutka, M., et al. Mucosal Healing in Ulcerative Colitis.
- Adak, S., et al. Mesenchymal Stem Cell Therapy for IBD.
- Sinagra, E., et al. Inflammation in IBD.
- Tsimmerman, Y.S. Systemic Impacts of Dysbiosis.
- Guss, M. Hygiene Hypothesis and IBD.
- Stefano, K., et al. Hygiene Standards and IBD Prevalence.
- Lim, Y.L. Helminths and Gut Microbiota in IBD.
- Qin, X. Etiology of IBD.
- Lu, L., et al. Hygiene and Disease Perception.
- Muse, K., et al. Stigma and IBD.
- Schmidt, K.J., et al. Targeted Therapy in Crohn’s Disease.
- Saunders, B. Young Adults with IBD.
- M’Koma, A.E. IBD: Clinical and Surgical Overview.
- Alexander-Williams, J. Surgical Management of IBD.
- Herrlinger, K.R., Stange, E.F. Biologicals and IBD Surgery.
- Verbanac, D., et al. Nutrition and Probiotics in IBD.
- Woodward, J. Inflammatory Bowel Diseases Overview.
- Kornbluth, A., Sachar, D.B. Ulcerative Colitis Guidelines.
- Amaya, L.J. Environmental Triggers in IBD.
- D’Amico, F., et al. Management of IBD Flares.
- Boyle, B. Flares and Patient Perspectives.
- Rosen, H. Increasing IBD Incidence.
- de Sousa, M.H.P.T. IBD and Environmental Influences.
- Monif, G.R.G. Historical Views of IBD.
- Alluwaimi, A.M. Etiology of Crohn’s Disease.
- Singh, S.B. Non-Contagious Nature of IBD.
- Ferri, B.A. Contagion Metaphors and Autoimmune Conditions.
- Grech, V.E. Debunking MMR Vaccine Myths.
- Aswani-Omprakash, T., et al. Cultural Awareness in IBD Education.

