Nocturnal cough is a persistent cough that occurs predominantly at night, often disrupting sleep. It can be a symptom of various underlying conditions, such as asthma, upper respiratory tract infections, or gastroesophageal reflux disease (GERD). In children, nocturnal cough is commonly associated with upper respiratory tract infections and can lead to sleep disturbances for both the child and their parents, resulting in increased school absenteeism. In adults, it may indicate conditions like cough variant asthma, where the cough is the only symptom, or heart failure, where it is accompanied by other symptoms like dyspnea and exercise intolerance. The frequency and severity of nocturnal cough can also serve as an indicator of asthma control, with increased cough frequency potentially signaling poor asthma management. Treatments such as honey have been found to provide symptomatic relief for nocturnal cough in children with URIs, improving both cough frequency and sleep quality.
Common Causes of Nocturnal Cough
Nocturnal cough can disrupt sleep and affect overall health. Understanding the common causes of nocturnal cough is essential for effective management and treatment. Here are some of the primary reasons why nocturnal cough may occur:
1. Postnasal Drip
Postnasal drip, also known as upper airway cough syndrome (UACS), is a prevalent cause of chronic cough. It occurs when excess mucus from the nasal passages drips down the back of the throat, leading to irritation and coughing. This condition can be triggered by various rhinosinus conditions such as allergic rhinitis, bacterial sinusitis, and vasomotor rhinitis. The symptoms and signs of UACS are nonspecific, making it challenging to diagnose based solely on medical history and physical examination. Effective treatment often involves addressing the underlying rhinosinus condition, which can significantly alleviate the cough.
2. Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD) is another common cause of nocturnal cough. GERD occurs when stomach acid flows back into the esophagus, causing irritation and inflammation. This reflux can reach the throat and respiratory tract, leading to coughing, especially at night when lying down. Studies have shown a strong association between nocturnal GER and respiratory symptoms, including wheezing and breathlessness. GERD is also frequently found in patients with asthma, exacerbating their respiratory symptoms. Managing GERD through lifestyle changes and medications can help reduce nocturnal cough and improve sleep quality.
3. Asthma
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, shortness of breath, and coughing. Nocturnal cough is a common symptom in asthma patients, often worsening at night due to increased airway reactivity and mucus production. Asthma-related cough can be triggered by allergens, cold air, or respiratory infections. Effective asthma management, including the use of inhaled corticosteroids and bronchodilators, can help control symptoms and reduce the frequency of nocturnal cough.
4. Allergies
Allergies, particularly allergic rhinitis, are a significant cause of nocturnal cough. Allergic reactions to airborne allergens such as pollen, dust mites, and pet dander can lead to inflammation and increased mucus production in the nasal passages. This excess mucus can drip down the throat, causing irritation and coughing, especially at night. Identifying and avoiding allergens, along with using antihistamines and nasal corticosteroids, can help manage allergic symptoms and reduce nocturnal cough.
5. Infections
Respiratory infections, including the common cold, influenza, and bronchitis, can cause a persistent cough that worsens at night. These infections lead to inflammation and increased mucus production in the airways, which can trigger coughing. Post-infectious cough can linger for weeks after the initial infection has resolved. Managing the symptoms with rest, hydration, and over-the-counter medications can help alleviate the cough. In some cases, antibiotics may be necessary if a bacterial infection is present.
6. Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by airflow obstruction and chronic respiratory symptoms, including cough. Nocturnal cough in COPD patients can be due to increased mucus production, airway inflammation, and reduced lung function. Smoking is the primary cause of COPD, and quitting smoking is crucial for managing the disease. Inhaled bronchodilators, corticosteroids, and pulmonary rehabilitation can help improve symptoms and reduce the frequency of nocturnal cough in COPD patients.
7. Heart Failure
Heart failure can lead to a condition known as cardiac cough, which often worsens at night. In heart failure, the heart’s reduced ability to pump blood effectively can cause fluid buildup in the lungs, leading to congestion and coughing. This nocturnal cough is typically accompanied by other symptoms such as shortness of breath, fatigue, and swelling in the legs. Managing heart failure with medications, lifestyle changes, and, in some cases, surgical interventions can help alleviate the symptoms and reduce nocturnal cough.
8. Respiratory Infections
Respiratory infections, such as pneumonia and bronchitis, can cause significant inflammation and mucus production in the airways, leading to a persistent cough that often worsens at night. These infections can be viral or bacterial, and the treatment approach varies accordingly. Rest, hydration, and medications to manage symptoms are essential for recovery. In bacterial infections, antibiotics may be necessary. Post-infectious cough can persist for weeks, requiring ongoing management to alleviate symptoms.
9. Medication Side Effects
Certain medications can cause a persistent cough as a side effect, which may worsen at night. Angiotensin-converting enzyme (ACE) inhibitors, commonly used to treat high blood pressure and heart failure, are known to cause a dry, persistent cough in some patients. If a medication-induced cough is suspected, consulting with a healthcare provider to adjust the medication or switch to an alternative treatment can help resolve the cough. Monitoring and managing side effects are crucial for maintaining overall health and well-being.
10. Environmental Factors
Environmental factors such as exposure to smoke, pollution, and allergens can contribute to nocturnal cough. Poor indoor air quality, including the presence of dust, mold, and pet dander, can exacerbate respiratory symptoms and lead to coughing at night. Using air purifiers, maintaining a clean living environment, and avoiding exposure to irritants can help reduce the impact of environmental factors on nocturnal cough. Identifying and mitigating these factors is essential for improving respiratory health and reducing nighttime symptoms.
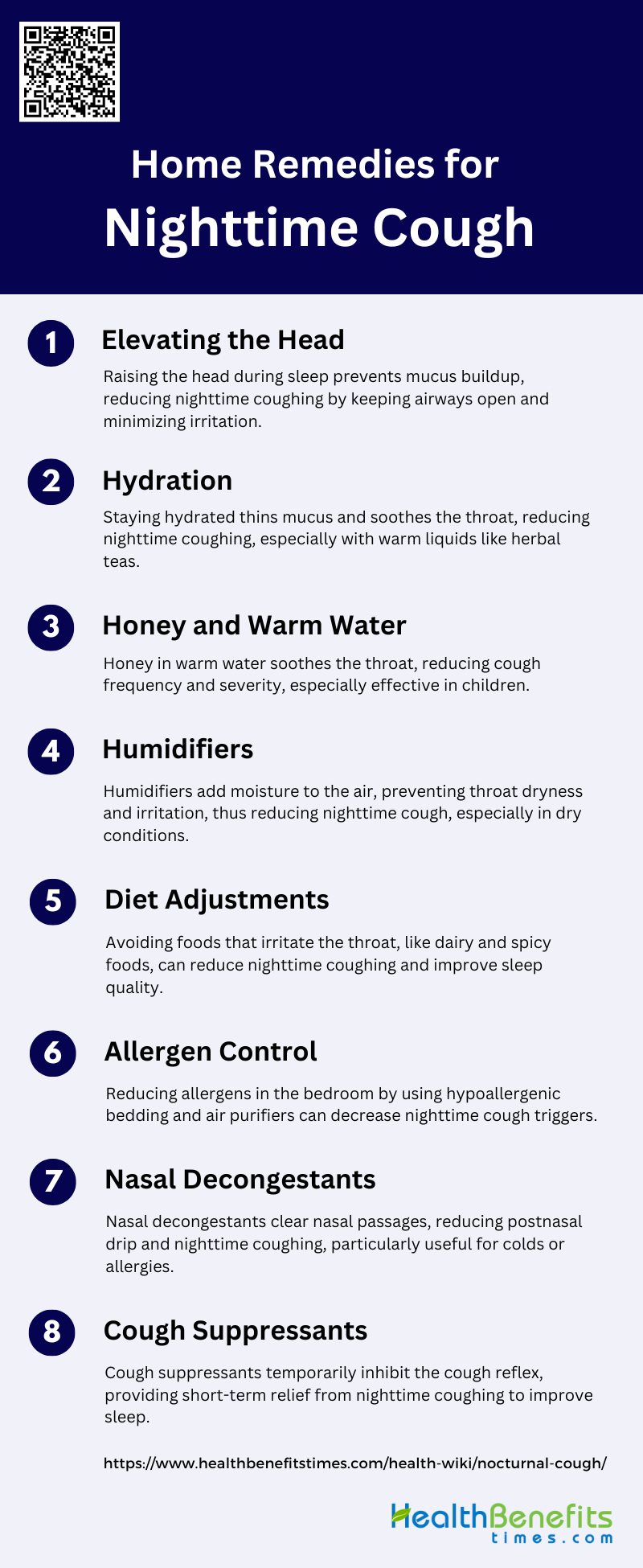
Home Remedies for Nighttime Cough
Nighttime cough can be particularly bothersome, disrupting sleep and overall well-being. Fortunately, several home remedies can help alleviate this condition and provide relief. Here are some effective home remedies for nighttime cough:
1. Elevating the Head
Elevating the head during sleep can help reduce nighttime coughing by preventing mucus from pooling in the throat, which can trigger coughing. This position helps keep the airways open and reduces postnasal drip, which is a common cause of nighttime cough. By using extra pillows or a wedge pillow, individuals can maintain an elevated position throughout the night, thereby minimizing the frequency and severity of coughing episodes.
2. Hydration
Staying hydrated is crucial for soothing the throat and reducing cough. Fluids help thin mucus, making it easier to expel and less likely to irritate the throat. Warm liquids, such as herbal teas or broths, can be particularly effective as they provide additional soothing effects on the throat lining. Consistent hydration throughout the day and before bedtime can significantly alleviate coughing by keeping the throat moist and reducing irritation.
3. Honey and Warm Water
Honey mixed with warm water is a traditional remedy that has been shown to reduce the frequency and severity of coughs, particularly in children. Studies indicate that honey is more effective than no treatment and placebo in alleviating cough symptoms and improving sleep quality for both children and their parents. Honey’s soothing properties help coat the throat, reducing irritation and the urge to cough.
4. Humidifiers
Using a humidifier in the bedroom can improve air quality by adding moisture to the air, which helps keep the throat and nasal passages hydrated. This can reduce the irritation that leads to coughing. Humidifiers are particularly beneficial in dry climates or during winter months when indoor air tends to be dry. Maintaining optimal humidity levels can prevent the throat from becoming dry and irritated, thereby reducing nighttime cough.
5. Diet Adjustments
Certain foods and beverages can exacerbate coughing, especially when consumed close to bedtime. Dairy products, for example, can thicken mucus, while spicy foods can irritate the throat. Avoiding these foods in the evening can help reduce the likelihood of nighttime coughing. Instead, opting for lighter, non-irritating meals can contribute to a more restful sleep without the interruption of cough.
6. Allergen Control
Reducing exposure to allergens in the bedroom can significantly decrease nighttime coughing. Simple steps include using hypoallergenic bedding, regularly washing bed linens in hot water, and keeping pets out of the bedroom. Additionally, using air purifiers and keeping windows closed during high pollen seasons can help minimize allergen exposure, thereby reducing cough triggers.
7. Nasal Decongestants
Nasal decongestants can help reduce postnasal drip, which is a common cause of nighttime cough. By clearing nasal passages, these medications prevent mucus from dripping down the throat and causing irritation. Decongestants can be particularly useful for individuals suffering from colds or allergies, providing temporary relief and allowing for a more restful sleep.
8. Cough Suppressants
Cough suppressants can provide temporary relief from persistent coughing, especially when it disrupts sleep. These medications work by inhibiting the cough reflex, thereby reducing the urge to cough. They are best used for short-term relief and should be taken as directed to avoid potential side effects. Consulting with a healthcare provider can help determine the appropriate use and dosage of cough suppressants.
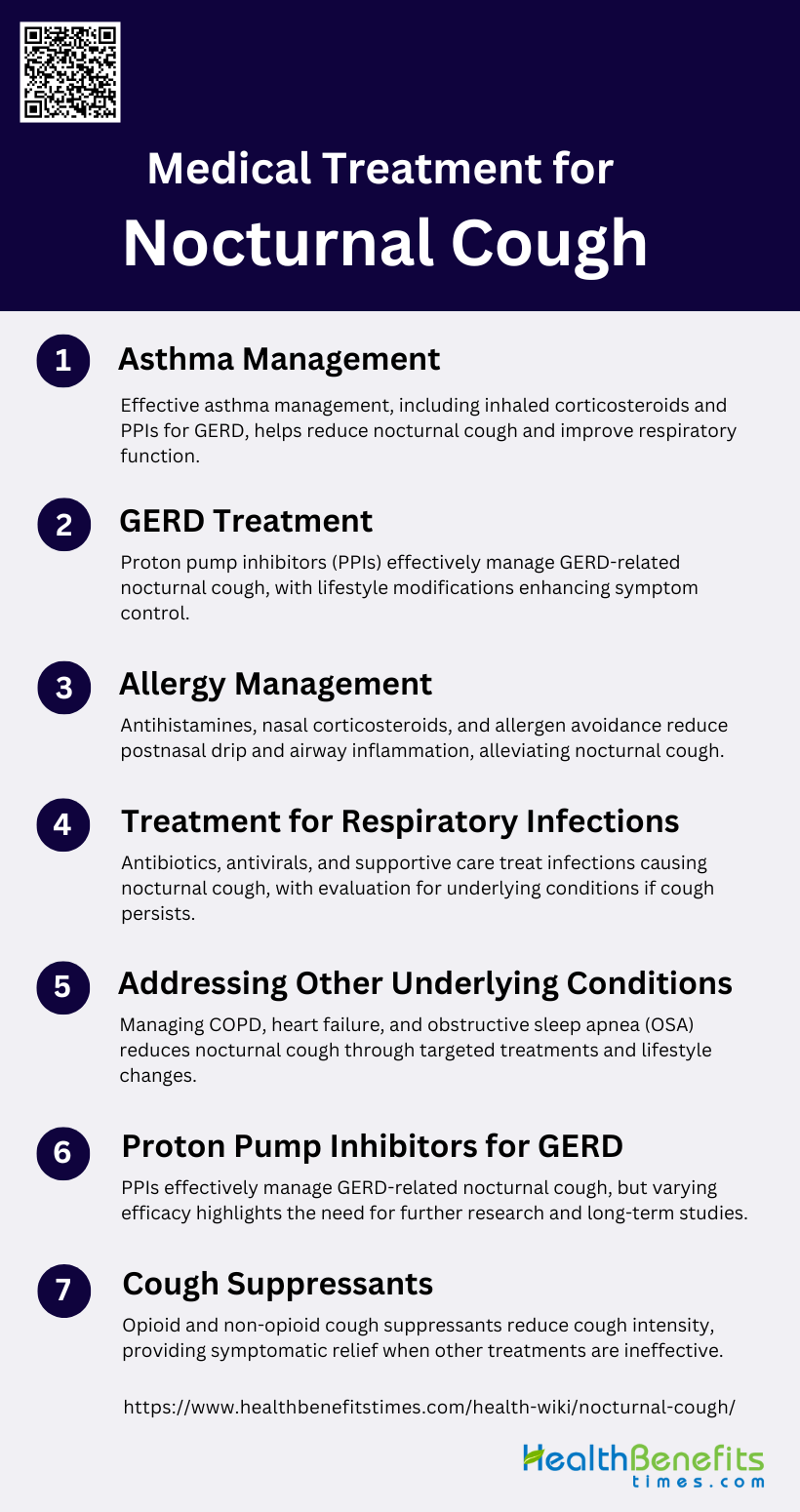
Medical Treatment for Nocturnal Cough
Nocturnal cough can significantly impact sleep quality and overall health, making medical intervention necessary in many cases. Various treatments are available to address the underlying causes and provide relief. Here are some common medical treatments for nocturnal cough:
1. Asthma Management
Asthma is a common cause of nocturnal cough, and its management often involves the use of anti-inflammatory medications such as inhaled corticosteroids. Studies have shown that gastroesophageal reflux disease (GERD) can exacerbate asthma symptoms, including nocturnal cough. Therefore, managing GERD in asthma patients can be crucial. Proton pump inhibitors (PPIs) have been found to improve nocturnal asthma symptoms in patients with GERD, although the results are inconsistent and more research is needed to confirm these findings. Effective asthma management may also include the use of long-acting beta2-agonists, which have shown improvements in peak expiratory flow in patients with both GERD and nocturnal symptoms.
2. GERD Treatment
GERD is a significant contributor to nocturnal cough, and its treatment can alleviate symptoms. Proton pump inhibitors (PPIs) are the most effective pharmaceutical therapy for GERD, providing acid suppression and improving both daytime and nighttime symptoms. Studies suggest that a double-standard dose of PPIs for a minimum of 2 to 3 months can be effective in managing GERD-related chronic cough. Lifestyle modifications, such as dietary changes and head-of-bed elevation, can also help manage nocturnal GERD symptoms.
3. Allergy Management
Allergies can trigger nocturnal cough through postnasal drip and airway inflammation. Managing allergies typically involves the use of antihistamines, nasal corticosteroids, and avoiding known allergens. While the provided data does not specifically address allergy management, it is well-documented that controlling allergic reactions can reduce cough symptoms. Effective allergy management can improve overall respiratory health and reduce the frequency and severity of nocturnal cough.
4. Treatment for Respiratory Infections
Respiratory infections, such as the common cold, bronchitis, and pneumonia, can cause persistent cough, including nocturnal cough. Treatment typically involves addressing the underlying infection with antibiotics (for bacterial infections) or antiviral medications (for viral infections). Supportive care, such as hydration, rest, and the use of cough suppressants, can also help alleviate symptoms. Persistent cough following a respiratory infection may require further evaluation to rule out other underlying conditions, such as asthma or GERD.
5. Addressing Other Underlying Conditions
Nocturnal cough can be a symptom of various underlying conditions, including chronic obstructive pulmonary disease (COPD), heart failure, and obstructive sleep apnea (OSA). Effective management of these conditions is crucial in reducing nocturnal cough. For instance, treating COPD with bronchodilators and inhaled corticosteroids can improve respiratory function and reduce cough. Addressing heart failure with appropriate medications and lifestyle changes can alleviate fluid buildup in the lungs, reducing cough. Continuous positive airway pressure (CPAP) therapy is effective in managing OSA, which can also reduce nocturnal cough.
6. Proton Pump Inhibitors for GERD
Proton pump inhibitors (PPIs) are a cornerstone in the treatment of GERD-related nocturnal cough. Studies have shown that PPIs can improve both daytime and nighttime GERD symptoms, including chronic cough. However, the efficacy of PPIs can vary, and some studies have reported inconsistent results. It is recommended to use a double-standard dose of PPIs for at least 2 to 3 months to achieve significant improvement in GERD-related cough. Despite their effectiveness, larger and more rigorously designed studies are needed to confirm the role of PPIs in managing GERD-related chronic cough.
7. Cough Suppressants
Cough suppressants, or antitussives, are used to reduce the frequency and intensity of coughing. Opioids such as codeine and morphine are effective cough suppressants but come with side effects like drowsiness and constipation. Non-opioid alternatives, including neurokinin and bradykinin receptor antagonists, are being explored as potential treatments. While specific treatments targeting the underlying cause of cough, such as asthma or GERD, are preferred, nonspecific antitussives can provide symptomatic relief when other treatments are ineffective. The development of novel antitussives continues to be an area of active research.
When to See a Doctor for Nocturnal cough
Signs That Your Nocturnal Cough Requires Medical Attention
Nocturnal cough can be a symptom of various underlying health conditions, and recognizing when to seek medical attention is crucial. If your nocturnal cough is persistent and disrupts your sleep regularly, it may be indicative of a more serious condition such as asthma or obstructive sleep apnea. Additionally, if the cough is accompanied by other symptoms like wheezing, shortness of breath, or chest pain, it is advisable to consult a healthcare professional. Chronic nocturnal cough can also be related to treatable disorders like rhinitis and asthma, or avoidable factors such as tobacco smoke exposure. Early medical intervention can help in diagnosing the underlying cause and initiating appropriate treatment.
Importance of Early Diagnosis and Treatment
Early diagnosis and treatment of nocturnal cough are essential to prevent complications and improve quality of life. Persistent nocturnal cough can significantly disrupt sleep, leading to daytime fatigue and reduced cognitive function. In children, it can affect school performance and overall well-being, causing considerable parental anxiety. Identifying the underlying cause, whether it is asthma, rhinitis, or another condition, allows for targeted treatment that can alleviate symptoms and prevent further health deterioration. Moreover, early intervention can help manage conditions like nocturnal asthma more effectively, reducing the frequency and severity of symptoms. Therefore, seeking timely medical advice is crucial for effective management and improved health outcomes.
FAQs
1. Can a nocturnal cough be a sign of sleep apnea?
Yes, a nocturnal cough can be a symptom of obstructive sleep apnea (OSA). In OSA, the airway collapses during sleep, leading to breathing interruptions and triggering a cough reflex. If you experience a chronic cough at night along with symptoms like loud snoring, gasping for air during sleep, or excessive daytime sleepiness, it is important to consult a healthcare provider for evaluation.
2. Is it possible for nocturnal cough to be caused by psychological factors?
Psychological factors such as stress or anxiety can contribute to nocturnal cough, particularly in individuals who may unconsciously cough due to nervousness or tension. This type of cough is often referred to as a psychogenic cough. Addressing the underlying psychological stress or anxiety through counseling or stress management techniques may help alleviate the cough.
3. Can nocturnal cough be related to diet, aside from GERD?
Yes, certain foods consumed close to bedtime, aside from those causing GERD, can contribute to nocturnal cough. Foods that are spicy, fatty, or dairy-based may irritate the throat or increase mucus production, leading to coughing. Identifying and avoiding trigger foods can help reduce the incidence of nocturnal cough.
4. Are there specific over-the-counter medications that can help with nocturnal cough?
Over-the-counter (OTC) medications such as antihistamines, decongestants, and cough suppressants may provide temporary relief from nocturnal cough. Antihistamines can reduce allergic reactions and postnasal drip, while decongestants help clear nasal congestion. However, it’s important to use these medications as directed and consult with a healthcare provider to ensure they are appropriate for your specific condition.
5. Can using essential oils in a diffuser help with nocturnal cough?
Some people find relief from nocturnal cough by using essential oils such as eucalyptus, peppermint, or lavender in a diffuser. These oils can help open up the airways, reduce congestion, and provide a soothing effect that may reduce coughing at night. However, essential oils should be used with caution, especially around children and pets, as some oils may cause irritation or allergic reactions.
6. How does smoking or exposure to secondhand smoke affect nocturnal cough?
Smoking and exposure to secondhand smoke are significant irritants that can exacerbate nocturnal cough. The chemicals in tobacco smoke can cause inflammation of the airways and increase mucus production, leading to coughing. Quitting smoking and avoiding exposure to secondhand smoke are crucial steps in reducing nocturnal cough and improving overall respiratory health.
7. Can dehydration during the day contribute to nocturnal cough?
Yes, dehydration can lead to a dry throat, which may increase the likelihood of coughing at night. Ensuring adequate hydration throughout the day helps keep the throat moist and reduces irritation, which can help prevent nocturnal cough.
8. What is the role of air quality in managing nocturnal cough?
Poor air quality, both indoors and outdoors, can contribute to nocturnal cough. Exposure to pollutants, dust, mold, and allergens can irritate the airways and lead to coughing. Improving indoor air quality by using air purifiers, keeping the environment clean, and reducing exposure to irritants can help manage nocturnal cough. Additionally, monitoring outdoor air quality and staying indoors on days with high pollution levels may be beneficial
9. Can postural changes during sleep help reduce nocturnal cough?
Yes, certain postural changes can help reduce nocturnal cough. Elevating the head of the bed or sleeping on your side can help prevent mucus from pooling in the throat and reduce the likelihood of coughing. These changes can be particularly effective for individuals with GERD or postnasal drip.
10. Are there any long-term consequences of untreated nocturnal cough?
Untreated nocturnal cough can lead to chronic sleep disturbances, which may result in daytime fatigue, decreased cognitive function, and overall reduced quality of life. Additionally, if the underlying cause of the cough is a condition like asthma, GERD, or heart failure, leaving it untreated can lead to worsening symptoms and complications related to those conditions. Therefore, it is important to address nocturnal cough promptly and seek appropriate medical care.