Systemic diseases are medical conditions that affect multiple organs or tissues throughout the body, rather than being confined to a single area or system. These disorders can impact various bodily functions and often involve complex interactions between different physiological systems. Examples of systemic diseases include cardiovascular diseases, diabetes, autoimmune disorders like rheumatoid arthritis and systemic lupus erythematosus, and certain infectious diseases. The widespread nature of systemic diseases means that they can manifest with a diverse range of symptoms and complications, potentially affecting the heart, lungs, kidneys, nervous system, and other vital organs. Due to their complexity and far-reaching effects, systemic diseases often require comprehensive medical management and may involve multiple medical specialties in their diagnosis and treatment.
Difference between systemic diseases and localized diseases
Systemic diseases and localized diseases differ primarily in the scope and impact of their manifestations. Systemic diseases affect the entire body or multiple organ systems, often presenting with widespread symptoms and secondary complications. For instance, cancer can be viewed as a systemic disease where local manifestations like carcinoma or lymphoma can lead to secondary systemic sequelae such as metastasis. Similarly, systemic inflammatory response syndrome (SIRS) exemplifies a systemic disease where an exaggerated inflammatory response affects the whole body, potentially leading to multiple organ dysfunction. In contrast, localized diseases are confined to a specific area or organ. For example, in plant pathology, diseases like apple scab or corn smut are localized, affecting only particular parts of the plant. The management of systemic diseases often requires a holistic approach, considering the interconnectedness of body systems, whereas localized diseases can often be treated by targeting the specific affected area.
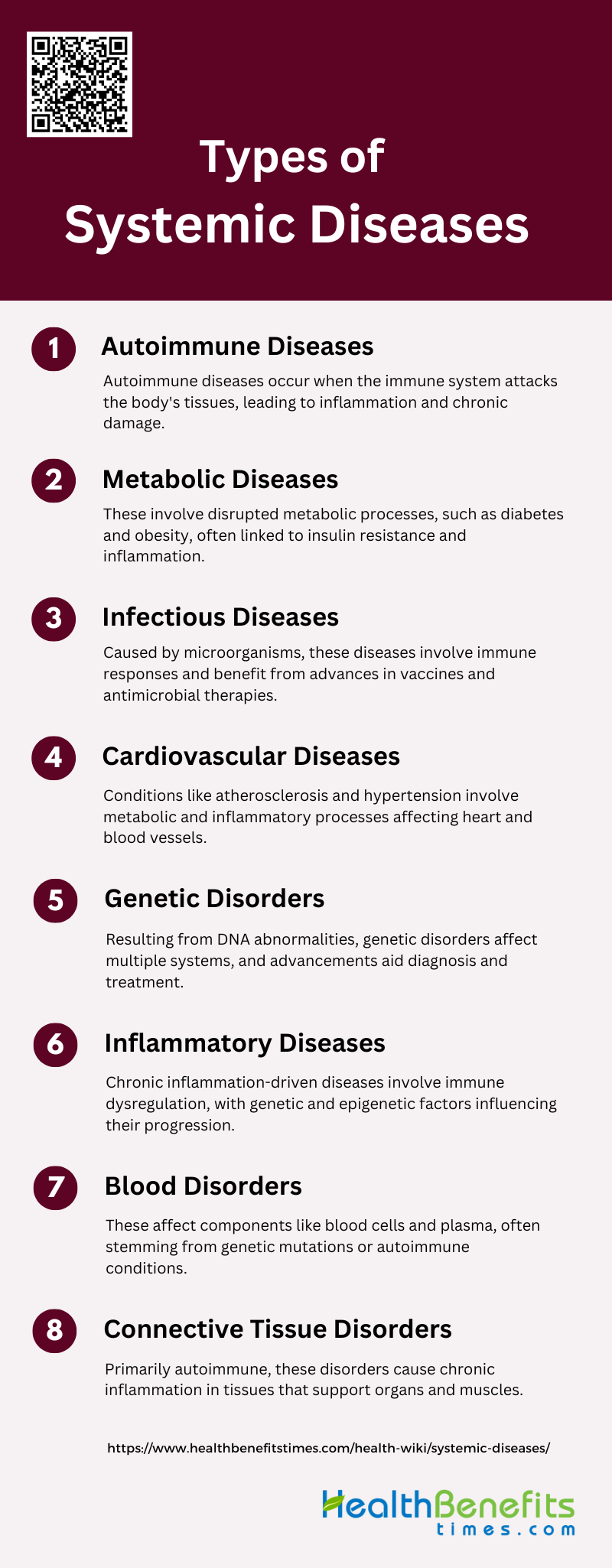
Types of Systemic Diseases
Systemic diseases are conditions that affect multiple organs or the entire body, rather than a single organ or part. These diseases can have widespread effects and often require comprehensive management strategies. Below is a list of various types of systemic diseases:
1. Autoimmune Diseases
Autoimmune diseases are characterized by the immune system mistakenly attacking the body’s own tissues. These conditions can affect various organs and systems, leading to chronic inflammation and tissue damage. Common autoimmune diseases include rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis. Genetic predisposition and environmental triggers play significant roles in the development of these diseases. Advances in understanding the mechanisms of autoimmunity have led to improved diagnostic tools and therapies, particularly targeting cytokines and chemokines to mitigate inflammatory responses.
2. Metabolic Diseases
Metabolic diseases encompass a range of disorders that disrupt normal metabolic processes, often leading to conditions like diabetes, obesity, and metabolic syndrome. These diseases are frequently associated with insulin resistance, dyslipidemia, and hypertension, contributing to cardiovascular morbidity. The interplay between metabolic and immune systems is crucial, with inflammatory mediators such as adipokines playing a significant role in the pathogenesis of these conditions. Recent research highlights the importance of genetic, nutritional, and microbiome factors in regulating these interactions.
3. Infectious Diseases
Infectious diseases are caused by pathogenic microorganisms such as bacteria, viruses, fungi, and parasites. These diseases can range from mild to life-threatening and can spread directly or indirectly from one individual to another. The immune system’s response to these pathogens involves both innate and adaptive mechanisms. Advances in understanding the molecular and cellular basis of infections have led to the development of vaccines and antimicrobial therapies, significantly reducing the burden of infectious diseases globally.
4. Cardiovascular Diseases
Cardiovascular diseases (CVD) include a range of conditions affecting the heart and blood vessels, such as atherosclerosis, hypertension, and heart failure. These diseases are often linked to metabolic and inflammatory processes. Atherosclerosis, for instance, is now understood to be an autoimmune-inflammatory disease characterized by lipid metabolism alterations and immune system activation. Both traditional risk factors like smoking and novel factors contribute to the pathogenesis of CVD, particularly in patients with autoimmune diseases.
5. Genetic Disorders
Genetic disorders are caused by abnormalities in an individual’s DNA, which can be inherited or occur de novo. These disorders can affect various bodily functions and systems, leading to a wide range of clinical manifestations. Advances in genetic research have identified specific mutations responsible for many genetic disorders, enabling better diagnostic and therapeutic strategies. Understanding the genetic basis of these diseases also provides insights into their pathophysiology and potential interventions.
6. Inflammatory Diseases
Inflammatory diseases are characterized by chronic inflammation, which can affect various tissues and organs. These conditions include autoimmune diseases, autoinflammatory disorders, and other systemic inflammatory conditions. The underlying mechanisms often involve dysregulated immune responses and genetic predispositions. Epigenetic modifications also play a crucial role in the pathogenesis of these diseases, influencing gene expression and cellular functions without altering the DNA sequence.
7. Blood Disorders
Blood disorders encompass a variety of conditions affecting the blood’s components, including red and white blood cells, platelets, and plasma. These disorders can result from genetic mutations, autoimmune reactions, or other underlying diseases. Autoimmune connective tissue diseases, for instance, often involve hematologic abnormalities, which can serve as important prognostic factors. Understanding the cellular and molecular networks driving these abnormalities is crucial for developing targeted therapies.
8. Connective Tissue Disorders
Connective tissue disorders primarily affect the tissues that support, bind, or separate other tissues and organs. These disorders, such as systemic lupus erythematosus and rheumatoid arthritis, are often autoimmune in nature and involve chronic inflammation. They can lead to multisystem involvement with variable clinical manifestations. Epigenetic modifications and environmental factors play significant roles in the development and progression of these disorders, highlighting the need for comprehensive diagnostic and therapeutic approaches.
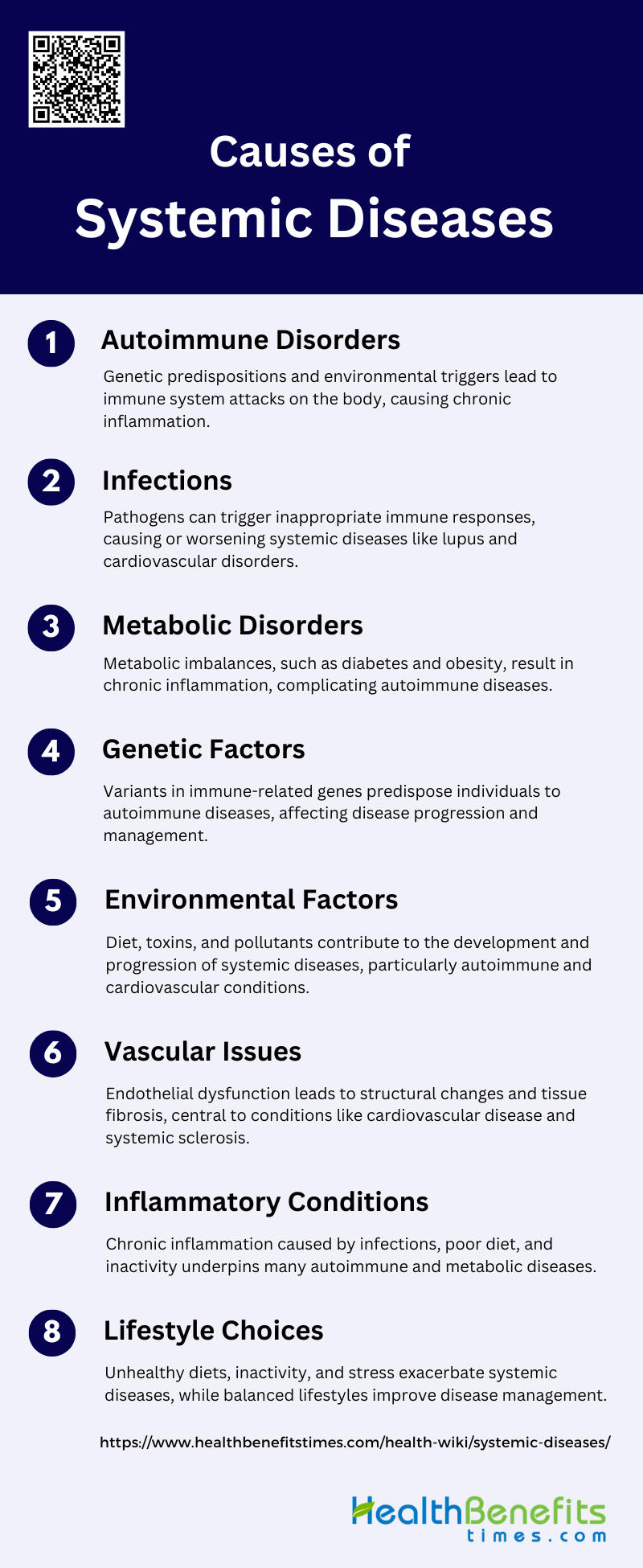
Causes of Systemic Diseases
Systemic diseases can arise from a variety of causes, each affecting the body in different ways. Understanding these causes is crucial for effective diagnosis and treatment. Below is a list of the primary causes of systemic diseases:
1. Autoimmune Disorders
Autoimmune disorders arise when the immune system mistakenly attacks the body’s own tissues. This can be due to a combination of genetic predisposition and environmental triggers. For instance, diseases like rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and multiple sclerosis (MS) are influenced by genetic factors such as HLA gene variants and environmental factors like infections and stress. The interplay between these factors leads to chronic inflammation and tissue damage, often requiring long-term management. Recent studies also highlight the role of epigenetic modifications in the pathogenesis of these diseases.
2. Infections
Infections can act as triggers for systemic diseases by activating the immune system inappropriately. Pathogens such as viruses and bacteria can initiate or exacerbate autoimmune responses, leading to diseases like SLE and RA. Chronic infections can also contribute to systemic chronic inflammation (SCI), which is linked to various diseases including cardiovascular disease, diabetes, and autoimmune disorders. The molecular mechanisms involve the activation of immune pathways that perpetuate inflammation, thereby contributing to disease progression.
3. Metabolic Disorders
Metabolic disorders, such as diabetes mellitus and non-alcoholic fatty liver disease, are significant contributors to systemic diseases. These conditions often result from metabolic imbalances that lead to chronic inflammation and organ damage. For example, obesity is a known risk factor for both type 1 diabetes and multiple sclerosis, as it promotes a state of low-grade chronic inflammation. Metabolic disorders can also exacerbate existing autoimmune conditions, complicating their management and increasing the risk of comorbidities.
4. Genetic Factors
Genetic factors play a crucial role in the development of systemic diseases. Variants in genes related to immune function, such as HLA, are commonly associated with autoimmune diseases like RA, SLE, and MS. These genetic predispositions can influence the severity and progression of the disease. Genome-wide association studies have identified multiple loci that contribute to disease susceptibility, highlighting the complex genetic landscape of these conditions. Understanding these genetic factors can aid in early diagnosis and personalized treatment strategies.
5. Environmental Factors
Environmental factors, including lifestyle, diet, and exposure to toxins, significantly impact the development and progression of systemic diseases. For instance, low levels of Vitamin D have been linked to higher incidence and severity of autoimmune diseases like MS and SLE. Environmental pollutants and industrial chemicals can also trigger chronic inflammation, leading to diseases such as cardiovascular disease and diabetes. Lifestyle modifications, such as a balanced diet and regular exercise, have been shown to improve clinical outcomes in patients with systemic diseases.
6. Vascular Issues
Vascular issues, such as vasculopathy and endothelial dysfunction, are central to the pathogenesis of systemic diseases like systemic sclerosis (SSc) and cardiovascular disease. These conditions involve the abnormal activation or damage of endothelial cells, leading to vascular structural changes and tissue fibrosis. Chronic inflammation and immune dysregulation further exacerbate these vascular issues, contributing to disease progression and complications. Early diagnosis and targeted therapies are essential to manage these vascular-related systemic diseases effectively.
7. Inflammatory Conditions
Inflammatory conditions are a hallmark of many systemic diseases, including autoimmune and metabolic disorders. Chronic systemic inflammation (SCI) can result from various factors such as infections, poor diet, and physical inactivity, leading to diseases like diabetes, cardiovascular disease, and autoimmune disorders. The underlying mechanisms involve the persistent activation of immune pathways, which perpetuate inflammation and tissue damage. Addressing the root causes of inflammation through lifestyle changes and targeted therapies can help manage these conditions.
8. Lifestyle Choices
Lifestyle choices including diet, physical activity, and stress management, play a significant role in the development and management of systemic diseases. Poor lifestyle choices, such as a high-fat diet and sedentary behavior, can lead to obesity and chronic inflammation, increasing the risk of diseases like MS and SLE. Conversely, healthy lifestyle choices, such as a balanced diet and regular exercise, have been shown to improve clinical outcomes and quality of life in patients with systemic diseases. Public health measures aimed at promoting healthy lifestyles can be an effective strategy for preventing and managing these conditions.
Symptoms of Systemic Diseases
Systemic diseases often present with a wide range of symptoms that can affect multiple organs and systems in the body. Recognizing these symptoms early is essential for timely diagnosis and treatment. Below is a list of common symptoms of systemic diseases:
1. Neurological Symptoms: Systemic autoimmune diseases can affect both the peripheral and central nervous systems, leading to various neurological symptoms. Common conditions include rheumatoid arthritis, Sjogren’s syndrome, systemic lupus erythematosus, and others.
2. Type 1 and Type 2 Symptoms in Autoimmune Diseases: In systemic lupus erythematosus (SLE) and other rheumatic diseases, symptoms can be categorized into type 1 (inflammatory) and type 2 (non-inflammatory). Type 2 symptoms include fatigue, pain, and anxiety-depression, which are often poorly correlated with disease activity.
3. Chronic Systemic Symptoms in Cancer Patients: Cancer patients, particularly those with head and neck cancer, often experience clusters of systemic symptoms such as inflammation, fatigue, and sickness behavior. These symptoms can be both acute and chronic.
4. Oral Manifestations: Systemic diseases can manifest in the oral cavity and orofacial region. These manifestations can be the first signs of systemic conditions, impacting oral health and function.
5. Hematologic Symptoms: Systemic diseases can cause various blood-related symptoms, including anemia, changes in platelet count, and alterations in white blood cell counts. These conditions can lead to thromboembolism, hemorrhage, or disseminated intravascular coagulation.
6. Nasal Symptoms: Systemic diseases can present with nasal and paranasal sinus symptoms. Conditions like Wegener’s granulomatosis and Churg-Strauss syndrome can cause chronic vasculitis and other nasal issues.
7. Ocular Symptoms: Systemic inflammatory diseases can affect the eyes, leading to conditions such as scleritis, keratitis, and retinopathy. These diseases can pose a serious threat to vision and may mimic infections.
8. Gastrointestinal Symptoms: Systemic disorders can manifest with gastrointestinal symptoms such as nausea, vomiting, diarrhea, constipation, abdominal pain, and jaundice. These symptoms can be indicative of various immunologic, infectious, and endocrine diseases.
9. Psychiatric Symptoms: Patients with systemic sclerosis often experience psychiatric symptoms such as depression and anxiety, which significantly impact their quality of life. These symptoms are influenced by the physical and psychological burden of the disease.
10. Multi-System Symptoms in SLE: Systemic lupus erythematosus (SLE) can affect every organ in the body, presenting with symptoms such as rash, arthritis, fatigue, nephritis, neurological problems, anemia, and thrombocytopenia. The disease is characterized by the presence of autoantibodies and has a relapsing and remitting course.
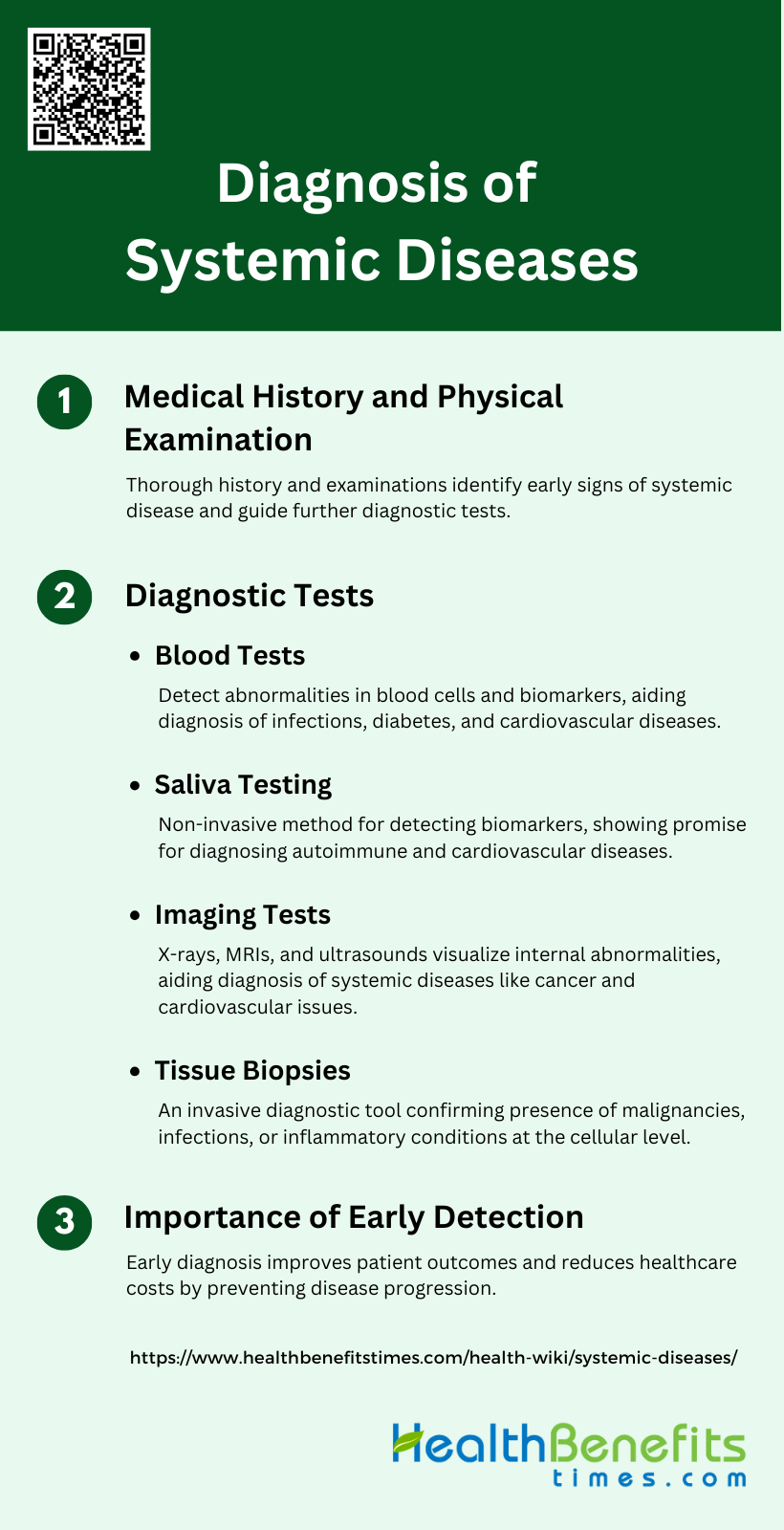
Diagnosis of Systemic Diseases
Diagnosing systemic diseases involves a comprehensive approach that includes evaluating medical history, conducting physical examinations, and performing various diagnostic tests. Early detection is crucial for effective management and treatment. Below is a detailed list of Diagnosis of Systemic Diseases:
1. Medical history and physical examination
Medical history and physical examination are foundational steps in diagnosing systemic diseases. A thorough medical history provides critical insights into the patient’s past and present health conditions, lifestyle, and genetic predispositions, which can guide the diagnostic process. Physical examination allows clinicians to observe and assess physical signs and symptoms that may indicate underlying systemic issues. Together, these steps help in forming a preliminary diagnosis and determining the need for further diagnostic tests. Early detection through these methods can significantly improve patient outcomes by enabling timely intervention.
2. Diagnostic tests
1. Blood tests
Blood tests are a cornerstone in the diagnosis of systemic diseases, offering a wealth of information about the body’s internal environment. They can detect abnormalities in blood cells, electrolytes, proteins, and other substances, providing clues to conditions such as infections, anemia, diabetes, and cardiovascular diseases. Blood tests are often used to measure levels of specific biomarkers that indicate disease presence or progression. Despite their invasiveness, blood tests remain a highly reliable and widely used diagnostic tool in clinical practice.
2. Saliva testing
Saliva testing has emerged as a promising non-invasive alternative for diagnosing systemic diseases. Saliva contains various biomarkers, including proteins, DNA, and RNA, which can reflect the body’s health status. Studies have shown that salivary diagnostics can effectively detect conditions such as cancer, autoimmune diseases, and cardiovascular diseases. The ease of collection and patient comfort make saliva testing an attractive option, especially for vulnerable populations like children and the elderly. Advances in salivaomics are paving the way for its broader clinical application
3. Imaging tests
Imaging tests, such as X-rays, CT scans, MRI, and ultrasound, play a crucial role in diagnosing systemic diseases by providing detailed visualizations of internal organs and structures. These tests can identify abnormalities such as tumors, organ damage, and structural anomalies, aiding in the diagnosis of conditions like cancer, cardiovascular diseases, and neurological disorders. Imaging tests are non-invasive and can offer real-time insights, making them invaluable in both initial diagnosis and ongoing disease monitoring.
4. Tissue biopsies
Tissue biopsies involve the removal and examination of tissue samples to diagnose diseases at a cellular level. This invasive procedure is often used to confirm the presence of malignancies, infections, and inflammatory conditions. While highly accurate, biopsies can be uncomfortable and carry risks such as infection and bleeding. Despite these drawbacks, tissue biopsies remain a gold standard for definitive diagnosis, particularly in oncology, where they provide critical information about tumor type, grade, and stage.
3. Importance of early detection
Early detection of systemic diseases is paramount for improving patient outcomes and survival rates. Identifying diseases at an early stage allows for timely intervention, which can prevent disease progression and complications. Non-invasive diagnostic methods, such as saliva testing, are particularly valuable for early detection as they are more comfortable for patients and can be easily repeated. Early diagnosis not only enhances the effectiveness of treatment but also reduces healthcare costs by minimizing the need for extensive and prolonged medical care.
Impact of Systemic Diseases on Daily Life
Systemic diseases can profoundly affect various aspects of daily life, including physical health, mental well-being, and the ability to perform everyday tasks. Understanding these impacts is crucial for developing effective coping strategies. Below is a list detailing the various ways systemic diseases can influence daily life:
1. Affect physical and mental well-being
Systemic diseases such as systemic sclerosis (SSc) and systemic lupus erythematosus (SLE) significantly impact both physical and mental well-being. Patients with SSc report symptoms like pain, fatigue, and gastrointestinal issues, which severely disrupt daily activities and quality of life (QoL). Similarly, SLE patients experience a range of physical symptoms and organ damage that negatively correlate with health-related quality of life (HRQoL), particularly affecting physical functioning more than mental health. These physical burdens often lead to emotional distress, including depression, anxiety, and low self-esteem, further exacerbating the overall well-being of patients.
2. Challenges in managing daily activities, work, and social life
Managing daily activities, work, and social life becomes a significant challenge for individuals with systemic diseases. For instance, thyroid diseases can lead to long-term sick leave and reduced working capacity, particularly in severe cases. Patients with Systemic sclerosis face palpable physical limitations and social impairments, such as difficulty maintaining work and fulfilling family responsibilities, which lead to a loss of independence. Asthma patients also report activity limitations and negative effects on social life and relationships, making it difficult to find and keep employment. These challenges necessitate comprehensive management strategies to support patients in their personal, social, and professional lives.
3. Emotional and psychological effects of living with a systemic disease
Living with a systemic disease often results in profound emotional and psychological effects. Patients with SSc experience significant emotional distress, including depression, anxiety, and fear of disease progression, which impact their health-related quality of life (HRQL). The psychological burden is also evident in vitiligo patients, who suffer from low self-esteem and social withdrawal due to the visible nature of their condition. The COVID-19 pandemic has further highlighted the vulnerability of individuals with chronic conditions to psychological distress, emphasizing the need for tailored psychological support to improve their quality of life. Overall, the emotional and psychological toll of systemic diseases underscores the importance of addressing mental health in patient care.
Treatment and Management of Systemic Diseases
Effectively treating and managing systemic diseases requires a multifaceted approach that includes medication, lifestyle changes, and sometimes alternative therapies or surgical interventions. Each strategy aims to alleviate symptoms, improve quality of life, and prevent disease progression. Below is a detailed list of treatment and management of systemic diseases:
1. Medication
Types of drugs used in the treatment of systemic diseases vary widely depending on the specific condition. For instance, in systemic lupus erythematosus (SLE), belimumab has shown strong evidence of efficacy in managing fatigue, a common symptom. In cancer treatment, traditional Chinese medicine (TCM) including herbal medicines and acupuncture, is often used to alleviate symptoms and improve quality of life, while also reducing the adverse effects of conventional therapies like chemotherapy and radiotherapy. Managing side effects is crucial, as many pharmacological interventions can lead to significant adverse events. For example, acupuncture has been explored for its potential to manage symptoms in chronic kidney disease (CKD) patients, although the evidence is of very low quality and the safety profile remains uncertain.
2. Lifestyle Changes
Diet and exercise adjustments are essential components in managing systemic diseases. Aerobic exercise has been identified as an effective strategy for alleviating fatigue in patients with SLE. Dietary modifications, such as low-calorie or low-glycemic index diets, have also shown potential benefits in managing fatigue and other symptoms in SLE patients. Stress management techniques, including mindfulness and relaxation training, have been found to be beneficial in managing symptoms of inflammatory bowel diseases (IBD). These lifestyle changes not only help in symptom management but also improve the overall quality of life for patients.
3. Alternative Therapies
Alternative therapies like acupuncture and herbal treatments play a significant role in symptom management for various systemic diseases. Acupuncture has been used to manage symptoms in chronic kidney disease (CKD) and cancer patients, although the evidence varies in quality. Herbal medicines, such as those used in traditional Chinese medicine (TCM), have been shown to alleviate symptoms and reduce the toxicity of conventional cancer treatments. In breast cancer patients, acupuncture-related therapies and herbal medicine have demonstrated potential in managing side effects like chemotherapy-induced peripheral neuropathy and lymphedema, thereby improving quality of life.
4. Surgical Interventions
Surgical interventions are sometimes necessary in the management of systemic diseases, particularly when other treatments are ineffective. For example, in severe cases of inflammatory bowel diseases (IBD), surgery may be required to remove damaged sections of the gastrointestinal tract. However, the focus is often on less invasive treatments first, such as pharmacological and alternative therapies, to manage symptoms and improve patient outcomes. The decision to proceed with surgery is typically based on the severity of the disease, the patient’s overall health, and the effectiveness of other treatments.
Preventive Measures of Systemic Diseases
Preventing systemic diseases involves adopting a holistic approach that includes regular physical activity, a healthy diet, and effective stress management. These measures not only reduce the risk of developing systemic diseases but also enhance overall well-being. Below is a list of preventive measures of Systemic Diseases:
1. Physical Activity and Exercise
Engaging in regular physical activity is crucial for the prevention and management of systemic diseases. Physical activity has been shown to play a significant role in the primary prevention and clinical treatment of various mental disorders, including depression, anxiety, and stress-related disorders. Additionally, it is a key component in reducing the risk of cardiovascular diseases (CVD) and other chronic conditions. Despite its benefits, physical inactivity remains a leading risk factor for non-communicable diseases, highlighting the need for increased efforts in promoting exercise as a preventive measure. Effective interventions include media campaigns, educational programs, and environmental changes to encourage more active lifestyles.
2. Healthy Diet and Nutrition
A healthy diet is fundamental in preventing systemic diseases such as cardiovascular diseases, diabetes, and certain cancers. Guidelines consistently recommend diets rich in fruits, vegetables, whole grains, and fish while limiting saturated fats, trans fats, and sugars. Dietary interventions have shown moderate success in improving health outcomes, particularly when combined with other lifestyle changes like physical activity. Mobile technology-based interventions have also demonstrated modest benefits in promoting healthier dietary habits, which can reduce the incidence of non-communicable diseases. However, more research is needed to establish the most effective dietary patterns for mental health and overall well-being.
3. Weight Management
Maintaining a healthy weight is essential for reducing the risk of systemic diseases, including cardiovascular diseases, diabetes, and certain cancers. Weight management strategies often involve a combination of diet, physical activity, and behavioral interventions. Effective weight management can improve periodontal health and reduce the risk of chronic diseases. Mobile-based interventions have shown some success in promoting weight loss and improving metabolic health, although the benefits are often modest. Regular monitoring and support from healthcare providers can enhance the effectiveness of weight management programs.
4. Stress Management
Effective stress management is vital for preventing and managing systemic diseases. Chronic stress is a known risk factor for mental health disorders, cardiovascular diseases, and other chronic conditions. Interventions such as mindfulness, cognitive-behavioral therapy, and relaxation techniques can significantly reduce stress levels and improve overall health. Guidelines for cardiovascular risk reduction also emphasize the importance of addressing psychological factors to improve clinical outcomes. Healthcare providers play a crucial role in offering stress management support and integrating these practices into routine care.
5. Sleep Optimization
Optimizing sleep is crucial for preventing systemic diseases and maintaining overall health. Poor sleep quality is associated with an increased risk of mental health disorders, cardiovascular diseases, and metabolic conditions. Non-pharmacological interventions, such as cognitive-behavioral therapy for insomnia and sleep hygiene education, have shown promise in improving sleep quality and reducing the risk of chronic diseases. Guidelines for cardiovascular risk reduction also highlight the importance of adequate sleep as part of a comprehensive lifestyle approach. Further research is needed to fully understand the bidirectional relationship between sleep and systemic diseases.
6. Smoking Cessation
Smoking cessation is one of the most effective measures for preventing systemic diseases, including cardiovascular diseases, respiratory conditions, and cancers. Interventions such as counseling, nicotine replacement therapy, and mobile-based support have been shown to significantly increase quit rates. Smoking cessation not only improves overall health but also enhances the effectiveness of other lifestyle interventions, such as physical activity and healthy eating. Guidelines consistently recommend smoking cessation as a primary strategy for reducing the risk of chronic diseases and improving long-term health outcomes.
FAQs
1. Can systemic diseases affect mental health?
Yes, systemic diseases can have a profound impact on mental health. Many systemic conditions, such as autoimmune diseases and chronic inflammatory disorders, are associated with increased rates of depression, anxiety, and cognitive issues due to the physical and emotional toll they take on the body. Chronic pain, fatigue, and reduced quality of life from these diseases can further exacerbate mental health challenges.
2. Are systemic diseases always chronic?
While many systemic diseases are chronic and require long-term management, not all are permanent. Some infectious systemic diseases, for example, can be acute and resolved with treatment. However, autoimmune and genetic systemic diseases often require lifelong care and monitoring.
3. How do systemic diseases influence other medical conditions?
Systemic diseases can complicate or exacerbate other medical conditions. For example, systemic inflammation from autoimmune diseases like lupus or rheumatoid arthritis can worsen cardiovascular health, increasing the risk of heart disease or stroke. Similarly, diabetes, a systemic metabolic disease, can affect multiple organs, including the kidneys, nerves, and eyes.
4. Can lifestyle changes help manage systemic diseases?
Yes, lifestyle changes such as a healthy diet, regular exercise, stress management, and quitting smoking can help manage many systemic diseases. These changes can reduce inflammation, improve immune function, and enhance overall well-being, potentially slowing disease progression or reducing symptoms.
5. How are systemic diseases diagnosed when symptoms overlap with other conditions?
Diagnosing systemic diseases can be complex because their symptoms often overlap with other conditions. Doctors typically use a combination of medical history, physical examination, blood tests, imaging studies, and biopsies to diagnose systemic diseases. They may also rule out other conditions through differential diagnosis to pinpoint the underlying systemic disorder.
6. Can systemic diseases be hereditary?
Yes, many systemic diseases have a genetic component. Autoimmune diseases like rheumatoid arthritis and lupus, as well as metabolic disorders like diabetes, can run in families due to shared genetic predispositions. Genetic testing may help assess an individual’s risk for certain systemic diseases.
7. Can systemic diseases go into remission?
Some systemic diseases, particularly autoimmune conditions, can enter periods of remission where symptoms reduce or disappear entirely. However, remission is not a cure, and the disease may flare up again in the future. Treatment during remission often focuses on maintenance and preventing flare-ups.
8. Are children susceptible to systemic diseases?
Yes, children can develop systemic diseases, including autoimmune diseases like juvenile rheumatoid arthritis and systemic lupus erythematosus. In fact, some systemic diseases have early-onset forms that specifically affect children. Early diagnosis and treatment are crucial in managing these conditions in young patients.
9. Can systemic diseases be prevented?
While not all systemic diseases can be prevented, certain lifestyle choices can reduce the risk of developing some types of systemic conditions. For example, maintaining a healthy diet and weight, exercising regularly, managing stress, and avoiding smoking can help prevent cardiovascular diseases, diabetes, and other systemic metabolic disorders.
10. How do systemic diseases impact the immune system?
Systemic diseases can either weaken the immune system, as seen in some genetic and infectious diseases, or cause it to become overactive, leading to autoimmune conditions. In autoimmune systemic diseases, the immune system mistakenly attacks the body’s own tissues, causing inflammation and damage to various organs.