The tibia, commonly known as the shinbone, is the larger of the two bones in the lower leg and one of the strongest weight-bearing bones in the human body. It extends from the knee to the ankle, articulating with the femur at the knee joint and with the talus bone of the foot at the ankle joint. The tibia plays a crucial role in supporting body weight and facilitating movement of the lower limb. It has a triangular cross-section with a sharp anterior border that can be felt beneath the skin. The tibia also serves as an attachment site for various muscles and ligaments, including the anterior cruciate ligament, which is important for knee stability. In medical imaging and orthopedic assessments, the tibia’s alignment and structure are often analyzed to diagnose and treat conditions affecting lower limb function and mobility.
Key parts of the tibia
The tibia, commonly known as the shinbone, is a vital component of the lower leg, playing a crucial role in weight-bearing and movement. It is anatomically divided into three main sections, each with distinct features and functions. Below are the key parts of the tibia:
1. Proximal (upper) end
The proximal end of the tibia is a crucial component of the knee joint, featuring two condyles that articulate with the femur. This region includes the tibial plateau, which is divided into medial and lateral compartments to accommodate the femoral condyles. The intercondylar eminence, located between these compartments, serves as an attachment point for the cruciate ligaments. The proximal tibia also houses the tibial tuberosity, a prominent bony projection on the anterior surface where the patellar tendon attaches. Understanding the anatomy of this area is essential for procedures such as total knee arthroplasty and ACL reconstruction.
2. Shaft (diaphysis)
The tibial shaft, or diaphysis, is the long, cylindrical portion of the bone connecting the proximal and distal ends. It has a triangular cross-section with three surfaces: medial, lateral, and posterior. The anterior border of the shaft is sharp and can be palpated beneath the skin, forming the shin. This region serves as an attachment site for various muscles and fascia of the lower leg. The shaft plays a crucial role in weight-bearing and transferring forces between the knee and ankle joints. In cases of fractures, the tibial shaft may be treated with intramedullary nailing, a common surgical technique for stabilizing long bone fractures.
3. Distal (lower) end
The distal end of the tibia forms the medial portion of the ankle joint, articulating with the talus bone. This region features the medial malleolus, a bony prominence on the inner ankle, and the tibial plafond, which forms the weight-bearing surface of the ankle joint. The distal tibia has a complex anatomy with various ligament attachments that contribute to ankle stability. Fractures in this area can be challenging to treat due to the thin soft tissue coverage and potential for compromised blood supply. Surgical interventions for distal tibial fractures or osteonecrosis may involve techniques such as internal fixation, bone grafting, or in severe cases, ankle fusion to restore function and stability.
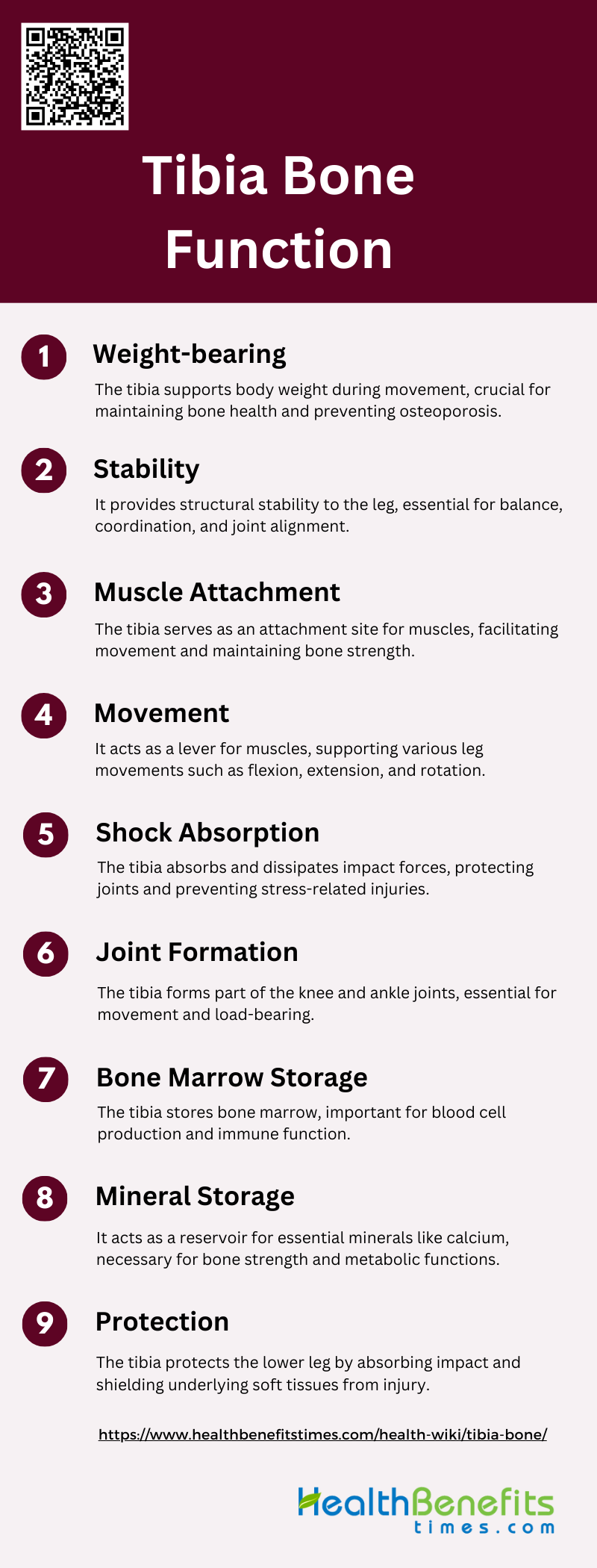
Tibia Bone Function
The tibia is a crucial bone in the lower leg that serves multiple functions essential for movement and overall leg mechanics. It plays a significant role in weight-bearing, stability, and muscle attachment, among other functions. Below are the key functions of the tibia:
1. Weight-bearing
The tibia plays a crucial role in weight-bearing, as it supports a significant portion of the body’s weight during standing, walking, and running. Studies have shown that weight-bearing exercises, such as running, significantly enhance the bone mineral density of the tibia, making it stronger and more resilient to mechanical stress. The tibia’s ability to bear weight is essential for maintaining bone health and preventing conditions like osteoporosis. Weight-bearing activities stimulate bone formation and remodeling, which are vital for maintaining bone strength and integrity. This function is particularly important in the context of rehabilitation and recovery from bone injuries, where weight-bearing exercises are often prescribed to promote healing and bone regeneration.
2. Stability
The tibia contributes significantly to the stability of the lower leg and overall body posture. It forms the medial part of the lower leg and works in conjunction with the fibula and surrounding muscles to provide structural support. The stability provided by the tibia is essential for activities that require balance and coordination, such as walking, running, and jumping. The bone’s geometry and density, which are influenced by mechanical loading and muscle forces, play a critical role in its ability to provide stability. The tibia’s structural integrity is crucial for maintaining proper alignment and function of the knee and ankle joints, thereby preventing injuries and enhancing overall mobility.
3. Muscle Attachment
The tibia serves as a major site for muscle attachment, which is vital for movement and force generation. Several muscles, including the quadriceps, hamstrings, and calf muscles, attach to the tibia, enabling various movements of the lower leg. The interaction between muscle forces and the tibia is essential for maintaining bone strength and geometry. Muscle contractions during physical activities exert forces on the tibia, stimulating bone remodeling and adaptation. This relationship underscores the importance of maintaining muscle strength to support bone health and prevent conditions like sarcopenia and osteoporosis.
4. Movement
The tibia plays a pivotal role in facilitating movement by acting as a lever for muscles to exert force. It is involved in various movements of the lower leg, including flexion, extension, and rotation. The bone’s structural properties, such as its density and geometry, are adapted to withstand the mechanical stresses associated with these movements. The tibia’s ability to support dynamic activities is crucial for athletic performance and daily activities. Exercise-induced changes in the tibia, such as increased cortical area and bone strength, enhance its capacity to support movement and resist fractures.
5. Shock Absorption
The tibia contributes to shock absorption during activities that involve impact, such as running and jumping. Its ability to absorb and dissipate forces helps protect the joints and other bones from injury. The bone’s mechanical properties, including its density and elasticity, are essential for effective shock absorption. Weight-bearing exercises have been shown to improve the tibia’s shock-absorbing capacity by enhancing its structural integrity and mechanical strength. This function is particularly important in preventing stress fractures and other impact-related injuries.
6. Joint Formation
The tibia is a key component in the formation of the knee and ankle joints. It articulates with the femur and patella at the knee joint and with the talus at the ankle joint. These joints are essential for a wide range of movements and load-bearing activities. The tibia’s role in joint formation is critical for maintaining joint stability and function. Proper alignment and health of the tibia are necessary to ensure smooth and pain-free movement of the knee and ankle joints. Any deformities or injuries to the tibia can significantly impact joint function and overall mobility.
7. Bone Marrow Storage
The tibia contains bone marrow, which is essential for the production of blood cells. The bone marrow within the tibia is involved in hematopoiesis, the process of generating red blood cells, white blood cells, and platelets. This function is vital for maintaining overall health and supporting the body’s immune system. The tibia’s role in bone marrow storage highlights its importance beyond structural support and movement. Conditions that affect the bone marrow, such as leukemia, can have significant implications for the tibia’s function and overall health.
8. Mineral Storage
The tibia serves as a reservoir for essential minerals, including calcium and phosphorus, which are crucial for various physiological processes. These minerals are stored in the bone matrix and can be mobilized to maintain mineral homeostasis in the body. The tibia’s role in mineral storage is vital for bone health and metabolic functions. Adequate mineralization of the tibia is necessary to maintain its strength and structural integrity. Weight-bearing exercises have been shown to enhance mineral density in the tibia, thereby improving its capacity to store and release minerals as needed.
9. Protection
The tibia provides protection to the lower leg by acting as a shield against external forces. Its robust structure helps safeguard the underlying muscles, nerves, and blood vessels from injury. The bone’s ability to absorb and distribute impact forces is crucial for preventing damage to the soft tissues of the lower leg. The tibia’s protective function is particularly important in high-impact sports and activities where the risk of injury is elevated. Maintaining the health and strength of the tibia is essential for ensuring its protective capabilities and overall function.
Tibia in Comparison with Fibula
Differences between the Tibia and Fibula
The tibia and fibula are two distinct bones in the lower leg with different roles and structural characteristics. The tibia, also known as the shinbone, is the larger and more robust of the two, primarily responsible for weight-bearing and providing structural support to the leg. In contrast, the fibula is thinner and less involved in weight-bearing, serving mainly as a site for muscle attachment and contributing to the stability of the ankle joint. The fibula’s morphology varies significantly among different species and even within human populations, reflecting its secondary role in load transmission and its adaptation to different locomotor behaviors.
How They Function Together to Stabilize the Leg
The tibia and fibula work in tandem to stabilize the leg, particularly at the ankle joint. The fibula, although not a primary weight-bearing bone, plays a crucial role in maintaining the structural integrity of the lower leg. It helps distribute loads and provides lateral stability to the ankle joint, especially during movements such as dorsiflexion and eversion. The interosseous membrane between the tibia and fibula also aids in load distribution and stabilizes the bones during various activities. This collaborative function is essential for activities that require balance and agility, such as running and directional changes in sports.
Key Weight-Bearing Role of the Tibia Compared to the Non-Weight-Bearing Fibula
The tibia is the primary weight-bearing bone in the lower leg, transmitting the majority of the body’s weight from the femur to the foot. This role is evident in its larger size and robust structure, which are adapted to withstand significant mechanical loads. In contrast, the fibula bears only a small fraction of the load, approximately 6.4% under normal conditions, with variations depending on the position of the ankle joint. The fibula’s main function is to provide lateral stability and support to the tibia, rather than bearing weight. This distinction is crucial for understanding the biomechanics of the lower leg and the different roles these bones play in movement and stability.
Common Injuries and Conditions of the Tibia
The tibia is susceptible to various injuries and conditions. These can range from fractures and stress injuries to chronic conditions like shin splints and osteoarthritis. Below are some common injuries and conditions affecting the tibia:
1. Tibial Shaft Fractures
Tibial shaft fractures are prevalent injuries, particularly in adolescents and adults, often resulting from high-energy trauma. These fractures can range from low-energy, minimally displaced fractures to severe, limb-threatening injuries with associated nerve and arterial damage. Treatment options include closed reduction and cast immobilization, flexible and rigid intramedullary nailing, plate and screw osteosynthesis, and external fixation. Complications such as infection, malunion, nonunion, and compartment syndrome are common, necessitating careful management and follow-up. Proximal tibiofibular joint dislocation can also occur with tibial shaft fractures, requiring precise anatomical reduction to prevent chronic instability and nerve palsy.
2. Stress Fractures
Stress fractures of the tibia are overuse injuries commonly seen in athletes and military personnel. They result from repetitive mechanical loading that exceeds the bone’s ability to repair itself. Diagnosis is often clinical, supported by imaging modalities such as MRI or bone scans. Treatment typically involves rest and activity modification to allow the bone to heal. In some cases, immobilization or surgical intervention may be necessary if the fracture is severe or does not respond to conservative measures. Preventive strategies include proper training techniques, adequate nutrition, and addressing biomechanical abnormalities.
3. Shin Splints
Shin splints, or medial tibial stress syndrome, are characterized by pain along the inner edge of the tibia. This condition is common among runners and athletes who engage in repetitive impact activities. The pain results from inflammation of the muscles, tendons, and bone tissue around the tibia. Treatment focuses on rest, ice, compression, and elevation (RICE), along with physical therapy to strengthen the affected muscles and improve flexibility. Gradual return to activity and proper footwear are essential to prevent recurrence. In severe cases, imaging may be required to rule out stress fractures.
4. Compartment Syndrome
Acute compartment syndrome (ACS) is a serious condition characterized by increased pressure within a muscle compartment, leading to ischemia and potential muscle and nerve damage. It is often associated with tibial fractures, particularly high-energy injuries. Early recognition and prompt surgical intervention, typically fasciotomy, are crucial to prevent permanent damage. Risk factors include younger age, male gender, high-energy trauma, and certain fracture patterns. Delayed treatment can result in complications such as muscle necrosis, nerve damage, and even amputation.
5. Osteomyelitis
Osteomyelitis of the tibia is a severe bone infection that can occur following open fractures, surgical procedures, or hematogenous spread. It presents with localized pain, swelling, and systemic symptoms such as fever. Diagnosis involves clinical evaluation, imaging studies, and microbiological cultures. Treatment typically includes prolonged antibiotic therapy and surgical debridement to remove infected tissue. Chronic osteomyelitis may require more extensive surgical intervention, including bone grafting or reconstruction. Preventive measures include meticulous surgical technique and early intervention in cases of open fractures.
6. Osteoarthritis
Osteoarthritis (OA) of the tibia, particularly the knee joint, is a degenerative condition characterized by the breakdown of cartilage and underlying bone. It leads to pain, stiffness, and reduced joint function. Risk factors include age, obesity, previous joint injuries, and genetic predisposition. Management includes lifestyle modifications, physical therapy, pain relief medications, and intra-articular injections. In advanced cases, surgical options such as osteotomy or joint replacement may be considered. Early intervention and weight management are crucial to slow the progression of OA and maintain joint function.
7. Proximal Tibia Fractures
Proximal tibia fractures involve the upper part of the tibia and can be complex due to the involvement of the knee joint. These fractures are often the result of high-energy trauma and are associated with a higher risk of complications such as compartment syndrome and arterial injury. Treatment options include external fixation, plating, and intramedullary nailing, depending on the fracture pattern and soft tissue condition. Proper alignment and stabilization are crucial to prevent malunion and ensure good functional outcomes. Early recognition and management of associated injuries are essential for optimal recovery.
8. Distal Tibia Fractures
Distal tibia fractures, also known as pilon fractures, involve the lower part of the tibia and often extend into the ankle joint. These fractures are typically caused by high-energy trauma and can be challenging to treat due to the involvement of the weight-bearing surface. Treatment options include external fixation, open reduction and internal fixation, and intramedullary nailing. Complications such as malunion, nonunion, and post-traumatic arthritis are common, necessitating careful surgical planning and follow-up. Early intervention and appropriate rehabilitation are crucial to restore function and prevent long-term disability.
Treatment methods for tibia injuries
Tibia injuries can range from minor stress fractures to severe breaks requiring comprehensive care. Treatment methods vary based on the severity and type of injury, and may include non-surgical approaches, surgical interventions, medications, and rehabilitation. Below are the primary treatment methods for tibia injuries:
1. Non-surgical Treatment
Non-surgical treatment of tibia injuries, particularly for undisplaced fractures, often involves conservative management techniques such as casting or bracing. This approach is typically reserved for stable fractures where the bone fragments remain aligned. Nonoperative treatment can be complicated by issues such as loss of reduction and subsequent malunion, which may necessitate further intervention. Studies have shown that non-surgical management of tibial shaft fractures results in a longer return-to-sport time compared to surgical methods, with return times ranging from 28 to 182 weeks. Despite these challenges, non-surgical treatment remains a viable option for certain types of tibia fractures, particularly when surgical risks are deemed too high.
2. Surgical Treatment
Surgical treatment of tibia fractures is often necessary for displaced or complex fractures. Techniques such as intramedullary nailing and plate-and-screw fixation are commonly employed. Intramedullary nailing is considered the gold standard for midshaft fractures due to its biomechanical stability and minimal invasiveness, which allows for early mobilization. For distal tibia fractures, both intramedullary nailing and plate fixation are used, though each has its own set of challenges and complications. Surgical management generally results in faster healing and higher return-to-sport rates compared to non-surgical methods, with return times ranging from 12 to 54 weeks. The choice of surgical technique often depends on the specific fracture characteristics and associated soft-tissue injuries.
3. Medications
Medications play a crucial role in the management of tibia fractures, primarily for pain control and infection prevention. Analgesics, including nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids, are commonly prescribed to manage pain during the initial recovery phase. Antibiotics are essential in cases of open fractures to prevent infection, particularly when surgical intervention is involved. Additionally, medications such as bone morphogenetic proteins (BMPs) may be used to promote bone healing in certain cases. The use of negative pressure wound therapy (NPWT) has also been shown to reduce infection rates and improve outcomes in open tibia fractures.
4. Rehabilitation
Rehabilitation is a critical component of the recovery process for tibia fractures, aiming to restore function and strength to the affected limb. Early functional rehabilitation, including weight-bearing exercises, is encouraged to prevent joint contractures and promote faster healing. For surgical cases, rehabilitation protocols often begin with limited weight-bearing and progress to full weight-bearing as tolerated, typically starting around 10 to 12 weeks postoperatively. Physical therapy exercises focus on improving range of motion, strength, and proprioception. Successful rehabilitation can significantly reduce the overall treatment time and improve long-term functional outcomes.
Preventative Measures of Tibia Bone
Maintaining the health and integrity of the tibia bone is essential for overall leg function and injury prevention. Implementing preventative measures can significantly reduce the risk of tibia-related injuries and enhance performance. Below are some key preventative measures for tibia bone health:
1. Proper warm-up and cool-down
Proper warm-up and cool-down routines are essential in preventing tibia bone injuries. Warm-up exercises, such as dynamic stretching and light aerobic activities, prepare the muscles and joints for more intense physical activity by increasing blood flow and flexibility. Cool-down exercises, including static stretching and gradual reduction in activity intensity, help in reducing muscle stiffness and soreness post-exercise. Studies have shown that neuromuscular warm-up strategies, which include stretching, strengthening, and balance exercises, significantly reduce lower limb injuries in athletes and military recruits. These routines are particularly effective in preventing overuse injuries and enhancing overall performance.
2. Use appropriate protective gear
Using appropriate protective gear, such as braces and insoles, can significantly reduce the risk of tibia bone injuries. Patellofemoral braces have been found effective in preventing anterior knee pain, which is a common issue among runners and athletes. Custom-made biomechanical insoles are particularly beneficial for military recruits, as they help in reducing the incidence of shin splints, a condition closely related to tibia bone stress. These protective devices provide additional support and cushioning, thereby minimizing the impact on the tibia during high-intensity activities.
3. Strengthen leg muscles
Strengthening leg muscles is crucial for the prevention of tibia bone injuries. Strong muscles provide better support and stability to the bones, reducing the risk of fractures and stress injuries. Weight-bearing exercises, such as squats and lunges, are particularly effective in enhancing muscle strength and bone density. Additionally, functional electrical stimulation (FES) combined with physical activities like rowing has shown promising results in improving bone health and reducing fracture risk in individuals with spinal cord injuries. Regular strength training should be incorporated into fitness routines to maintain optimal leg muscle strength and bone health.
4. Improve flexibility
Improving flexibility through regular stretching exercises can help in preventing tibia bone injuries. Flexibility exercises enhance the range of motion in joints and reduce muscle stiffness, which in turn lowers the risk of injuries during physical activities. Although some studies have shown mixed results regarding the effectiveness of stretching in preventing lower limb injuries, it remains a recommended practice for overall musculoskeletal health. Incorporating dynamic stretching before workouts and static stretching post-exercise can contribute to better flexibility and injury prevention.
5. Proper footwear
Wearing proper footwear is essential for preventing tibia bone injuries. Footwear that provides adequate support, cushioning, and stability can significantly reduce the impact on the tibia during activities like running and jumping. Studies have shown that foot orthoses, such as custom-made insoles, can help in preventing bone stress injuries by providing additional support and reducing mechanical stress on the tibia. However, the effectiveness of specific footwear designs in preventing injuries remains inconclusive, highlighting the need for further research in this area.
6. Gradual training progression
Gradual training progression is a key strategy in preventing tibia bone injuries. Sudden increases in training intensity, duration, or frequency can lead to overuse injuries, including stress fractures. It is important to follow a structured training plan that allows for gradual adaptation to increased physical demands. Studies have shown that reducing the distance, frequency, and duration of running can be effective in preventing lower limb injuries. A well-designed training regimen that includes adequate rest and recovery periods can help in minimizing the risk of tibia bone injuries.
7. Maintain proper form
Maintaining proper form during physical activities is crucial for preventing tibia bone injuries. Incorrect techniques can place undue stress on the bones and joints, leading to injuries. Proper form ensures that the body is aligned correctly, distributing the forces evenly across the musculoskeletal system. Neuromuscular training programs that focus on improving technique, balance, and coordination have been shown to reduce the incidence of lower limb injuries. Regularly reviewing and correcting form with the help of a coach or trainer can help in preventing tibia bone injuries.
8. Stay hydrated and eat a balanced diet
Staying hydrated and eating a balanced diet is fundamental for maintaining bone health and preventing tibia bone injuries. Adequate hydration ensures that the body functions optimally, while a balanced diet provides essential nutrients, such as calcium and vitamin D, which are vital for bone strength. Nutritional interventions, combined with physical activity, have been shown to mitigate bone loss and improve bone density. Ensuring a diet rich in fruits, vegetables, lean proteins, and whole grains, along with sufficient fluid intake, supports overall bone health and reduces the risk of injuries.
FAQs
1. What are common symptoms of a tibia bone fracture?
Symptoms of a tibia bone fracture may include severe pain, swelling, bruising, an inability to bear weight on the affected leg, deformity, or a noticeable misalignment of the leg.
2. How long does it take for a tibia fracture to heal?
The healing time for a tibia fracture varies depending on the severity of the fracture and treatment method. In general, it can take anywhere from 3 to 6 months for a tibia fracture to heal completely.
3. Can the tibia bone be affected by osteoporosis?
Yes, the tibia, like other bones in the body, can be weakened by osteoporosis, a condition that causes bones to become brittle and more prone to fractures.
4. Are there any exercises to strengthen the tibia bone?
Weight-bearing exercises, such as walking, running, and resistance training, can help strengthen the tibia by improving bone density. Exercises targeting leg muscles, such as squats and lunges, also support the tibia.
5. What is the risk of developing arthritis after a tibia fracture?
Post-traumatic arthritis can occur after a tibia fracture, especially if the fracture involves the knee or ankle joints. Proper treatment and rehabilitation are important to minimize the risk of developing arthritis.
6. Can children experience tibia fractures, and do they heal differently than in adults?
Children can experience tibia fractures, and their bones generally heal faster than adult bones. However, growth plate injuries in children may require special attention to ensure proper bone growth and alignment.
7. How is a stress fracture of the tibia different from a complete tibia fracture?
A stress fracture is a small crack in the tibia caused by repetitive stress or overuse, while a complete fracture involves a break through the entire bone, typically resulting from a traumatic injury.
8. What complications can arise from tibia fractures?
Complications can include delayed healing, malunion (improper alignment), infection (especially in open fractures), and compartment syndrome, a serious condition where pressure builds up within muscle compartments.
9. Can you walk with a broken tibia?
In most cases, walking on a broken tibia is not advised, especially immediately after the injury. It is important to seek medical attention to stabilize the bone and prevent further damage.
10. What role does the fibula play in tibia injuries?
Although the fibula is not primarily a weight-bearing bone, it supports the tibia and contributes to ankle stability. Injuries to the tibia can sometimes affect the fibula, requiring a comprehensive treatment approach.