Chemotherapy is a widely used cancer treatment that involves the use of powerful drugs to destroy rapidly dividing cancer cells throughout the body. It works by targeting cells that grow and divide quickly, which is a characteristic of most cancer cells. However, chemotherapy can also affect healthy cells that divide rapidly, such as those in the bone marrow, digestive tract, and hair follicles, leading to various side effects. Chemotherapy can be administered in different ways, including orally, intravenously, or through injections, and it may be used alone or in combination with other treatments like surgery or radiation therapy. The goal of chemotherapy can vary depending on the type and stage of cancer, ranging from curing the disease to controlling its growth or providing palliative care to alleviate symptoms. While chemotherapy has been a cornerstone of cancer treatment for decades, ongoing research continues to refine its use and develop more targeted therapies to improve efficacy and reduce side effects.
How Does Chemotherapy Work?
Chemotherapy works by targeting rapidly dividing cancer cells, exploiting their high proliferation rate compared to normal cells. Different chemotherapeutic agents function through various mechanisms, such as inducing apoptosis, autophagy, or disrupting the cell cycle. For instance, some drugs interfere with DNA synthesis and replication, while others inhibit specific signaling pathways crucial for tumor growth. Treatment cycles are essential as they allow normal cells time to recover from the cytotoxic effects, thereby reducing side effects and improving patient tolerance to the therapy. Additionally, chemotherapy can enhance the immune response against tumors by increasing the immunogenicity of cancer cells and modulating the tumor microenvironment, which can be further leveraged in combination with immunotherapy for improved outcomes.
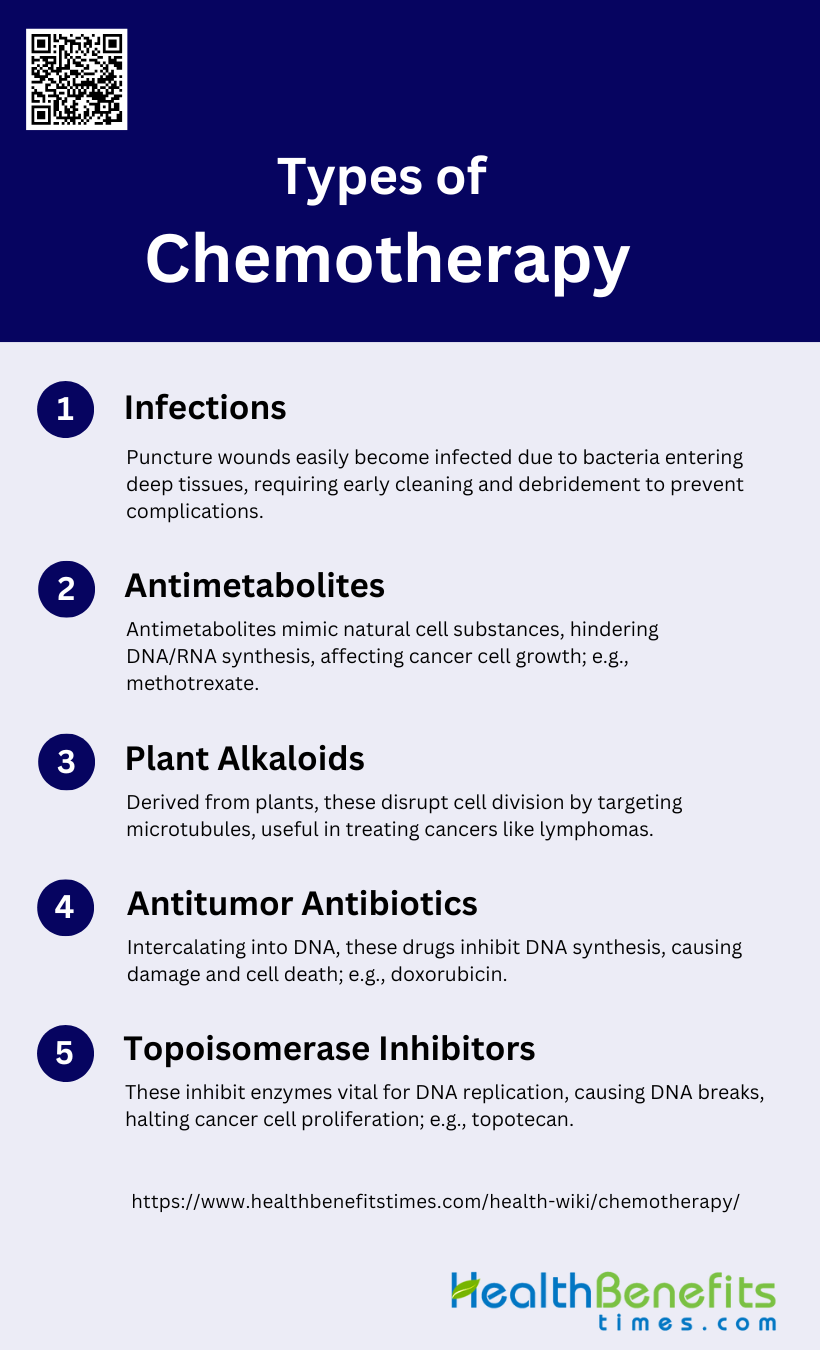
Types of Chemotherapy
Chemotherapy is a cornerstone in the treatment of various cancers, utilizing different classes of drugs to target and destroy cancer cells. Each type of chemotherapy works in a unique way to interfere with the growth and division of cancer cells. Below are some of the main types of chemotherapy:
1. Alkylating Agents
Alkylating agents are a class of chemotherapeutic drugs that work by adding alkyl groups to DNA, which leads to the cross-linking of DNA strands and prevents the DNA from uncoiling and separating. This action inhibits cell replication and ultimately leads to cell death. Cyclophosphamide is a well-known alkylating agent extensively used in treating various cancers, including leukemia, ovarian cancer, and small-cell lung cancer. These agents are effective but can cause significant side effects, such as the production of reactive oxygen species (ROS), which can lead to oxidative stress and toxicity. The combination of alkylating agents with other drugs, such as topoisomerase inhibitors, has shown enhanced antitumor effects without increasing toxicity.
2. Antimetabolites
Antimetabolites are chemotherapeutic agents that interfere with DNA and RNA synthesis by mimicking the natural substances within the cell, thereby inhibiting cell growth and proliferation. Common antimetabolites include methotrexate and 6-mercaptopurine, which are used to treat various leukemias and solid tumors. These drugs are often used in combination with other chemotherapeutic agents to enhance their efficacy and reduce the likelihood of resistance. For example, the combination of 5-fluorouracil (5FU) with leucovorin has been effective in treating colon cancer. Despite their effectiveness, antimetabolites can cause side effects such as skin reactions and gastrointestinal toxicity.
3. Plant Alkaloids
Plant alkaloids are derived from natural plant sources and are used in chemotherapy to disrupt cell division. This class includes vinca alkaloids, taxanes, and podophyllotoxins, which target microtubules and inhibit mitosis. Vinca alkaloids, such as vincristine and vinblastine, are used to treat various cancers, including lymphomas and leukemias. Taxanes, like paclitaxel and docetaxel, are effective against breast and ovarian cancers. These agents can cause side effects such as neuropathy and hypersensitivity reactions. The combination of plant alkaloids with other chemotherapeutic agents has shown promising results in enhancing antitumor activity and reducing resistance.
4. Antitumor Antibiotics
Antitumor antibiotics, such as doxorubicin and dactinomycin, are derived from Streptomyces bacteria and work by intercalating into DNA, thereby inhibiting DNA and RNA synthesis. These drugs also generate free radicals that cause DNA damage and cell death. Doxorubicin is widely used to treat various cancers, including breast cancer, lymphomas, and sarcomas. However, these agents can cause significant side effects, including cardiotoxicity and hand-foot syndrome. The development of new formulations, such as liposomal doxorubicin, aims to reduce these side effects while maintaining therapeutic efficacy.
5. Topoisomerase Inhibitors
Topoisomerase inhibitors, such as topotecan and etoposide, target the topoisomerase enzymes that are essential for DNA replication and transcription. By inhibiting these enzymes, topoisomerase inhibitors cause DNA strand breaks and prevent cancer cells from proliferating. These drugs are used to treat various cancers, including ovarian cancer, small-cell lung cancer, and certain leukemias. The combination of topoisomerase inhibitors with other chemotherapeutic agents, such as alkylating agents, has shown enhanced antitumor effects and reduced resistance. However, these drugs can cause side effects such as myelosuppression and gastrointestinal toxicity.
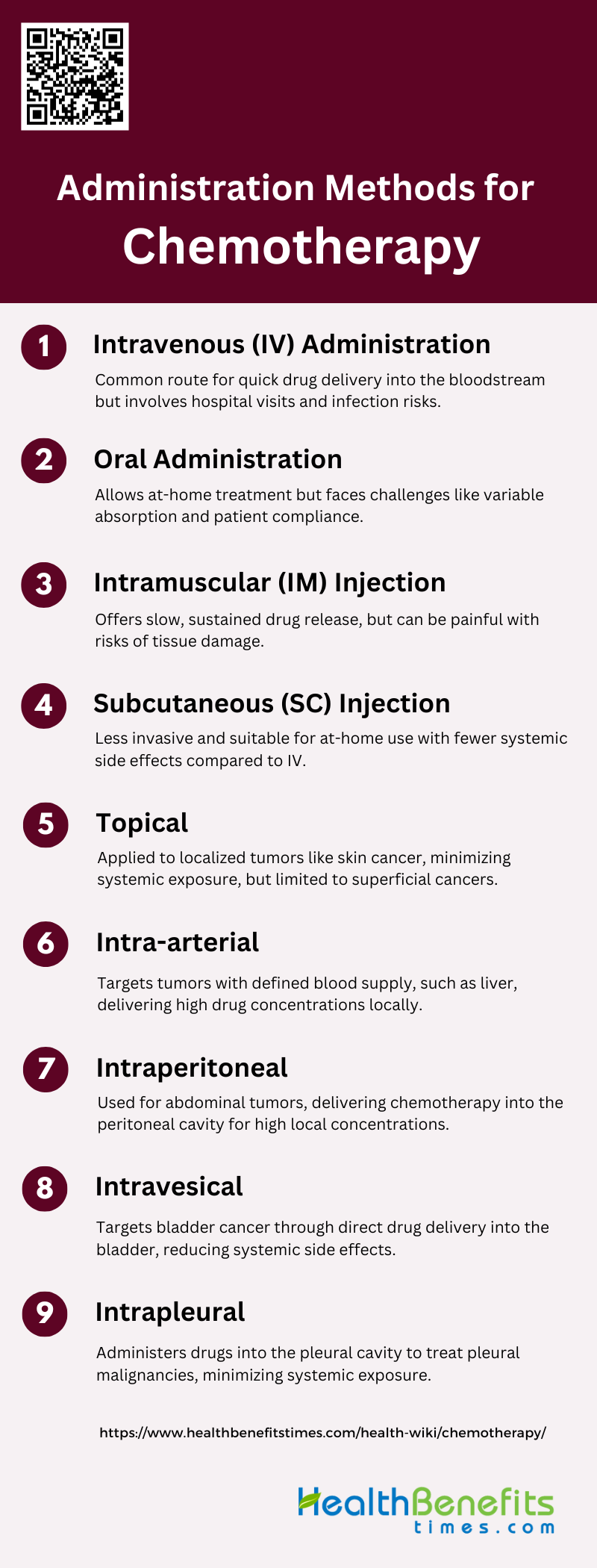
Administration Methods for Chemotherapy
Chemotherapy can be administered through various methods, each tailored to the type of cancer and the patient’s specific needs. These methods ensure that the drugs effectively reach the cancer cells while minimizing side effects. Below are some of the primary administration methods for chemotherapy:
1. Intravenous (IV) Administration
Intravenous (IV) administration is a common method for delivering chemotherapy directly into the bloodstream, ensuring rapid and complete drug availability. This route is particularly advantageous for drugs that are poorly absorbed orally or require immediate therapeutic effects. However, IV administration has several drawbacks, including the need for hospital visits, trained medical personnel, and the risk of catheter-related infections and complications. Studies have shown that while IV administration can achieve high peak plasma concentrations quickly, it may also lead to higher systemic toxicity compared to other routes. Despite these challenges, IV remains a standard route for many chemotherapeutic agents due to its efficacy and reliability.
2. Oral Administration
Oral administration of chemotherapy offers the convenience of at-home treatment, which can significantly improve patient quality of life and adherence to therapy. This route is particularly beneficial for chronic treatments and maintenance therapy. However, oral administration faces challenges such as variable absorption rates, gastrointestinal side effects, and the need for patient compliance. Some chemotherapeutic agents are not suitable for oral administration due to poor bioavailability or instability in the gastrointestinal tract. Despite these limitations, oral chemotherapy is a growing field, with ongoing research aimed at improving drug formulations to enhance absorption and reduce side effects.
3. Intramuscular (IM) Injection
Intramuscular (IM) injection is another method for administering chemotherapy, offering a balance between the rapid absorption of IV administration and the convenience of subcutaneous (SC) injection. IM injections are particularly useful for drugs that require slow, sustained release into the bloodstream. However, this route can be painful and may cause local tissue damage or infection. Research indicates that IM administration can extend the dwell time of therapeutic agents, making it a viable option for certain treatments. For example, IM administration of mesenchymal stromal cells has shown prolonged cell survival compared to other routes, highlighting its potential for specific clinical applications.
4. Subcutaneous (SC) Injection
Subcutaneous (SC) injection is a less invasive alternative to IV administration, offering the potential for at-home treatment and improved patient comfort. SC administration is particularly advantageous for drugs that require slow, sustained release. Studies have shown that SC administration can achieve comparable efficacy to IV administration for certain drugs, with a better safety profile and fewer systemic side effects. For instance, SC administration of bortezomib in patients with multiple myeloma has demonstrated non-inferior efficacy and reduced peripheral neuropathy compared to IV administration. This route is increasingly being explored for various chemotherapeutic agents to enhance patient convenience and reduce healthcare costs.
5. Topical
Topical administration of chemotherapy involves applying the drug directly to the skin or mucous membranes, targeting localized lesions or tumors. This route is particularly useful for treating superficial cancers, such as skin cancer or localized precancerous conditions. Topical administration minimizes systemic exposure and associated side effects, making it a safer option for certain patients. However, its efficacy is limited to accessible and superficial tumors, and it may not be suitable for more aggressive or deep-seated cancers. Research is ongoing to develop more effective topical formulations and delivery systems to enhance drug penetration and therapeutic outcomes.
6. Intra-arterial
Intra-arterial administration involves delivering chemotherapy directly into the artery supplying the tumor, achieving high local drug concentrations while minimizing systemic exposure. This method is particularly beneficial for treating tumors with a well-defined blood supply, such as liver or brain tumors. Studies have shown that intra-arterial administration can improve drug response and overall survival in patients with brain tumors, although it carries risks of vascular and neural toxicity. Research is focused on optimizing this route through techniques like blood-brain barrier disruption and high-resolution imaging to enhance targeting accuracy and reduce side effects.
7. Intraperitoneal
Intraperitoneal (IP) administration involves delivering chemotherapy directly into the peritoneal cavity, targeting abdominal tumors such as ovarian cancer. This method allows for high local drug concentrations and improved tumor penetration, potentially enhancing therapeutic efficacy. However, IP administration can also increase toxic side effects, limiting its use in some patients. Recent studies have explored the use of nanoparticle-conjugated drugs to improve targeting and reduce toxicity, showing promising results in selectively delivering chemotherapy to ovarian tumors while sparing normal tissue. This approach may offer a more effective and safer alternative to traditional IP chemotherapy.
8. Intravesical
Intravesical administration involves delivering chemotherapy directly into the bladder via a catheter, primarily used for treating bladder cancer. This method allows for high local drug concentrations with minimal systemic absorption, reducing the risk of systemic side effects. Intravesical chemotherapy is particularly effective for non-muscle invasive bladder cancer, where it can help prevent recurrence and progression. However, it requires repeated catheterization, which can be uncomfortable and carries a risk of urinary tract infections. Ongoing research aims to improve drug formulations and delivery techniques to enhance the efficacy and patient experience of intravesical chemotherapy.
9. Intrapleural
Intrapleural administration involves delivering chemotherapy directly into the pleural cavity, targeting pleural malignancies such as mesothelioma or metastatic pleural effusions. This method allows for high local drug concentrations, potentially improving therapeutic outcomes while minimizing systemic exposure. However, intrapleural administration can be associated with complications such as pleuritis, infection, and pain. Research is focused on developing more effective and less toxic intrapleural therapies, including the use of targeted drug delivery systems and novel chemotherapeutic agents. This approach holds promise for improving the management of pleural malignancies and enhancing patient quality of life.
Benefits of Chemotherapy
Chemotherapy offers several advantages in the treatment of cancer, ranging from destroying cancer cells to enhancing the effectiveness of other treatments. These benefits make chemotherapy a crucial component in many cancer treatment plans. Below are some of the primary benefits of chemotherapy:
1. Destroying Cancer Cells
Chemotherapy is a cornerstone in cancer treatment due to its ability to destroy cancer cells. The primary mechanism involves the use of cytotoxic drugs that target rapidly dividing cells, which include cancer cells. This approach is effective in reducing tumor size and eliminating cancerous cells from the body. For instance, chemotherapy has been shown to significantly reduce the recurrence and mortality rates in breast cancer by targeting and destroying malignant cells. Additionally, the use of nanomedicines in chemotherapy has enhanced the precision and efficacy of drug delivery, ensuring that cancer cells are effectively targeted and destroyed.
2. Preventing Cancer Spread
One of the critical benefits of chemotherapy is its ability to prevent the spread of cancer, also known as metastasis. Chemotherapy drugs can circulate throughout the body, targeting and killing cancer cells that have spread from the primary tumor site to other parts of the body. This is particularly important in high-risk cancers where metastasis is a significant concern. For example, studies have shown that chemotherapy can inhibit the proliferation and metastasis of primary tumor cells, thereby preventing the spread of cancer to distant organs. This systemic approach is crucial in managing cancers that are prone to spreading.
3. Slowing Cancer Growth
Chemotherapy is also effective in slowing the growth of cancer cells. By interfering with the cell division process, chemotherapy drugs can halt the progression of cancer, providing patients with more time and potentially improving their quality of life. Research has demonstrated that increasing the dose density of chemotherapy can significantly reduce disease recurrence and mortality by slowing down the growth of cancer cells. This approach not only helps in managing the disease but also in prolonging the survival of patients.
4. Curative Potential
In some cases, chemotherapy has the potential to cure cancer, especially when used in combination with other treatments such as surgery and radiation therapy. The goal of curative chemotherapy is to eliminate all cancer cells from the body, leading to complete remission. For instance, adjuvant chemotherapy has been shown to improve survival rates in patients with stage III colon cancer by eradicating micro-metastatic disease. This curative potential makes chemotherapy a vital component of comprehensive cancer treatment plans.
5. Enhancing Other Treatments
Chemotherapy can enhance the effectiveness of other cancer treatments, such as surgery and radiation therapy. By reducing the size of tumors, chemotherapy can make surgical removal easier and more effective. Additionally, it can sensitize cancer cells to radiation, improving the overall treatment outcome. For example, the combination of chemotherapy with Chinese herbal formula PRM1201 has been shown to improve the efficacy of adjuvant treatment in colon cancer, leading to better disease-free survival rates. This synergistic effect underscores the importance of chemotherapy in multimodal cancer treatment strategies.
6. Reduce Recurrence Risk
Reducing the risk of cancer recurrence is another significant benefit of chemotherapy. By targeting residual cancer cells that may remain after surgery, chemotherapy can help prevent the cancer from coming back. Studies have shown that localized chemotherapy, such as the use of injectable hexapeptide hydrogel, can effectively prevent breast cancer recurrence by ensuring sustained drug release at the tumor site. Additionally, increasing the dose density of adjuvant chemotherapy has been associated with fewer disease recurrences in breast cancer patients. These findings highlight the role of chemotherapy in long-term cancer management and recurrence prevention.
How Chemotherapy Targets Cancer Cells
Chemotherapy targets cancer cells primarily by exploiting their rapid division rates, which distinguishes them from most normal cells. This specificity allows chemotherapeutic agents to inhibit DNA synthesis and mitosis, thereby killing or impeding the proliferation of rapidly dividing cells. Chemotherapy disrupts cancer cell growth and division by inducing DNA damage, which is recognized and repaired by the DNA damage response machinery. If the damage is irreparable, it leads to cell death. A critical aspect of chemotherapy’s effectiveness is its ability to induce apoptosis, or programmed cell death, in cancer cells. This process can be triggered through intrinsic pathways involving mitochondrial signals or extrinsic pathways involving death receptors on the cell surface. The induction of DNA damage and subsequent apoptosis is a cornerstone of many chemotherapeutic strategies, as it ensures the elimination of cancer cells while minimizing the survival of resistant clones. By targeting these pathways, chemotherapy not only halts the proliferation of cancer cells but also promotes their systematic destruction through apoptosis, thereby enhancing the overall efficacy of cancer treatment.
Common Side Effects of Chemotherapy
Chemotherapy, while effective in treating cancer, often comes with a range of side effects that can impact a patient’s quality of life. These side effects vary depending on the type of drugs used and the individual’s response to treatment. Below are some of the most common side effects of chemotherapy:
1. Fatigue
Fatigue is one of the most frequently reported side effects of chemotherapy, significantly impacting patients’ daily lives. It is often described as a persistent sense of tiredness that does not improve with rest. In a study involving breast cancer patients, fatigue was noted as a major issue both during and six months after treatment, interfering with daily activities and causing considerable concern. Another study highlighted that 55% of patients rated fatigue as highly bothersome, affecting their ability to work, socialize, and maintain relationships. Effective management strategies, including psycho-education and exercise, have shown some promise in alleviating fatigue.
2. Nausea and Vomiting
Nausea and vomiting are common and distressing side effects of chemotherapy, often leading to significant discomfort and reduced quality of life. Studies have shown that these symptoms are among the most feared by patients starting chemotherapy. Despite advancements in antiemetic treatments, a substantial number of patients still experience these side effects. For instance, a study on lung cancer patients receiving cisplatin-based regimens found that ginger, as an adjuvant to standard antiemetic therapy, did not significantly reduce the incidence or severity of nausea and vomiting. Cognitive distraction and relaxation techniques have been suggested as nonpharmacologic strategies to manage these symptoms.
3. Hair Loss
Hair loss, or alopecia, is a highly visible and emotionally distressing side effect of chemotherapy. It was reported by over 80% of patients in a study involving breast cancer and malignant lymphoma patients. Hair loss can significantly affect a patient’s self-esteem and body image. In another study, hair problems persisted even six months after completing chemotherapy, highlighting the long-term impact of this side effect. Scalp cooling has been identified as a potential strategy to reduce hair loss, although its effectiveness varies.
4. Decreased Immune Function
Chemotherapy can lead to decreased immune function, making patients more susceptible to infections. This is often due to myelosuppression, where the bone marrow’s ability to produce blood cells is impaired. Patients frequently report weakened immune systems and fear of infections, which can isolate them from social activities and impact their daily lives. Hematologic toxicity, such as neutropenia, has been associated with worse changes in fatigue and nausea/vomiting, underscoring the need for supportive care during chemotherapy.
5. Anemia
Anemia is a common side effect of chemotherapy, resulting from the treatment’s impact on red blood cell production. It can cause symptoms such as fatigue, shortness of breath, and dizziness. In a study on the side effects of platinum-based chemotherapy drugs, anemia was identified as a significant issue, often requiring dose reductions and additional treatments. Patients experiencing anemia may find it challenging to perform daily tasks and maintain their usual level of physical activity.
6. Easy Bruising and Bleeding
Chemotherapy can lead to easy bruising and bleeding due to its effects on platelet production. This side effect is particularly concerning as it can indicate severe hematologic toxicity. A study found that only 41% of patients would seek immediate medical attention for unusual bleeding or bruising, highlighting a gap in patient education and awareness. Effective communication between patients and healthcare providers is crucial to ensure timely reporting and management of these symptoms.
7. Loss of Appetite
Loss of appetite is a common side effect of chemotherapy, often leading to weight loss and nutritional deficiencies. Patients frequently report a decreased desire to eat, which can exacerbate other side effects such as fatigue and weakness. In a study on patients’ fears regarding chemotherapy, loss of appetite was initially ranked as a significant concern, although its prominence decreased after effective management strategies were implemented. Addressing appetite changes through dietary modifications and supportive care is essential for maintaining patients’ overall health during treatment.
8. Skin and Nail Changes
Chemotherapy can cause various skin and nail changes, including rashes, dryness, and discoloration. These side effects, while not life-threatening, can be bothersome and affect patients’ quality of life. A study found that nail problems were commonly reported six months after completing chemotherapy, indicating the long-term nature of these side effects. Patients often do not report these issues immediately, as they are not perceived as urgent, but they can still significantly impact daily comfort and self-esteem.
9. Nerve Problems (Neuropathy)
Neuropathy, or nerve damage, is a dose-limiting side effect of certain chemotherapy drugs, such as oxaliplatin. It can cause symptoms like tingling, numbness, and pain, primarily in the hands and feet. In a review of platinum-based chemotherapy drugs, neurotoxicity was identified as a major concern, often requiring dose adjustments and additional treatments. Neuropathy can severely affect patients’ ability to perform daily activities and maintain their quality of life.
10. Organ Damage (Heart, Lungs, Kidneys)
Chemotherapy can cause damage to vital organs, including the heart, lungs, and kidneys. For example, cisplatin is known for its nephrotoxicity, while other drugs can cause cardiotoxicity and pulmonary toxicity. These side effects can be severe and may limit the use of certain chemotherapy agents. Patients undergoing treatment require extensive monitoring of their organ functions to detect and manage any damage early. Effective management strategies and supportive care are essential to mitigate the risks of organ damage during chemotherapy.
Managing Side Effects of Chemotherapy
Chemotherapy can cause a variety of side effects, but there are several strategies to manage them effectively. These strategies can help improve the patient’s quality of life and overall treatment experience. Below are some key methods for managing the side effects of chemotherapy:
1. Medications and Therapies to Manage Nausea, Pain, and Other Symptoms
Chemotherapy-induced nausea and vomiting (CINV) are among the most distressing side effects of cancer treatment. Effective management often involves a combination of pharmacological and non-pharmacological interventions. The use of 5-HT(3)-receptor antagonists, often combined with corticosteroids, is considered the gold standard for preventing acute and delayed CINV. Additionally, behavioral interventions such as mindfulness relaxation and the use of immersive virtual reality (IVR) have shown promise in managing anticipatory nausea and vomiting, particularly in pediatric patients. Despite these advancements, there is still a need for additional antiemetic drugs and therapies to further alleviate these symptoms.
2. Dietary and Lifestyle Changes to Cope with Side Effects
Dietary and lifestyle changes can play a significant role in managing the side effects of chemotherapy. Patients are often advised to consume small, frequent meals and avoid foods that are spicy, fatty, or have strong odors to minimize nausea and vomiting. Ginger, although not conclusively proven, has been explored as an adjuvant to standard antiemetic therapy. Additionally, maintaining hydration and incorporating light physical activities, such as walking or yoga, can help manage fatigue and improve overall well-being. These lifestyle modifications, combined with medical treatments, can significantly enhance the quality of life for chemotherapy patients.
3. Psychological Support and Counseling for Emotional Health
The emotional toll of chemotherapy can be profound, necessitating psychological support and counseling. Psychological interventions, including cognitive-behavioral therapy, progressive muscle relaxation, and guided imagery, have been shown to alleviate chemotherapy-induced nausea and vomiting and improve emotional well-being. Regular psychological support can help patients manage anxiety, depression, and other emotional distress associated with cancer treatment. Effective communication between patients and healthcare providers is also crucial, as it ensures that patients’ concerns are addressed and that they receive the necessary emotional support.
4. Importance of Regular Follow-Ups with Healthcare Providers
Regular follow-ups with healthcare providers are essential for the early detection and management of chemotherapy side effects. Telehealth interventions, such as the Patient Remote Intervention and Symptom Management System (PRISMS), enable real-time monitoring of patient-reported health data, allowing for rapid clinical decision-making and intervention. These follow-ups help in adjusting treatment plans, managing side effects promptly, and providing continuous support to patients. Regular interactions with healthcare providers also ensure that patients adhere to their treatment regimens and receive comprehensive care, ultimately improving their outcomes and quality of life.
Chemotherapy Success and Challenges
Success Stories and the Effectiveness of Chemotherapy
Chemotherapy has been a cornerstone in cancer treatment for decades, demonstrating significant success in various cancer types. For instance, chemotherapy has shown to extend overall survival in advanced gastric cancer by approximately 6.7 months compared to best supportive care. In advanced breast cancer, chemotherapy regimens have yielded a median overall survival of 2 years, with comparable efficacy across different agents. Additionally, chemotherapy remains the mainstay treatment for advanced gastric cancer, particularly in HER-2 positive cases treated with trastuzumab in combination with chemotherapy. These examples underscore the critical role of chemotherapy in improving patient outcomes across different cancer types.
Limitations of Chemotherapy
Despite its successes, chemotherapy faces several significant limitations. One major challenge is the development of resistance, where initially sensitive tumors rapidly become resistant to treatment. This resistance can arise from various mechanisms, including impaired drug delivery, increased drug efflux, and alterations in drug targets. Additionally, chemotherapy is often associated with severe side effects, such as toxicity, which can significantly impact the patient’s quality of life. For example, combining chemotherapy agents in advanced breast cancer did not improve overall survival but caused greater toxicity compared to single-agent chemotherapy. These limitations highlight the need for ongoing research to overcome resistance and reduce side effects.
Ongoing Research and Advancements in Chemotherapy Treatments
Ongoing research is focused on addressing the limitations of traditional chemotherapy and improving its efficacy. One promising area is supramolecular chemotherapy, which leverages host-guest molecular recognition to enhance drug delivery and reduce side effects. This approach aims to improve the solubility, stability, and targeting capability of chemotherapeutic drugs, thereby increasing their anticancer efficacy while minimizing harm to normal tissues. Additionally, studies are exploring the benefits of combination modality therapy, which integrates chemotherapy with other treatments like surgery and radiation, to enhance overall treatment outcomes. These advancements represent significant strides towards more effective and less toxic chemotherapy options for cancer patients.
Common Myths and misconceptions about Chemotherapy
Chemotherapy is often surrounded by myths and misconceptions that can cause unnecessary fear and anxiety. Understanding the facts can help patients make informed decisions about their treatment. Below are some common myths and misconceptions about chemotherapy:
1. Chemotherapy always causes severe nausea and vomiting
While chemotherapy-induced nausea and vomiting (CINV) are common side effects, they are not inevitable for all patients. Advances in antiemetic treatments, such as the use of 5-HT3 antagonists, dexamethasone, and neurokinin-1 antagonists, have significantly reduced the incidence and severity of CINV. Additionally, innovative approaches like immersive virtual reality (IVR) are being explored to manage these symptoms effectively in pediatric patients. Despite these advancements, some patients still experience delayed nausea and vomiting, which can impact their quality of life. However, the notion that severe nausea and vomiting are unavoidable is a misconception, as many patients achieve good symptom control with appropriate prophylactic measures.
2. Everyone loses their hair during chemotherapy
Hair loss, or alopecia, is a well-known side effect of certain chemotherapy drugs, but it does not affect everyone. The likelihood of experiencing hair loss depends on the specific chemotherapy regimen and individual patient factors. For instance, some chemotherapy drugs are more likely to cause hair loss than others. Additionally, newer treatments and supportive care measures, such as scalp cooling, can help reduce the risk of hair loss. Therefore, while hair loss is a common concern, it is not a universal outcome for all chemotherapy patients.
3. Chemotherapy will drastically interrupt your life
The impact of chemotherapy on daily life varies widely among patients. While some may experience significant side effects that require adjustments to their routines, others may continue their normal activities with minimal disruption. Advances in supportive care, including effective management of side effects like nausea, vomiting, and fatigue, have improved patients’ ability to maintain their quality of life during treatment. Additionally, individualized treatment plans and the use of less toxic chemotherapy regimens can help minimize the impact on daily life. Thus, the belief that chemotherapy will drastically interrupt one’s life is not universally true and depends on various factors, including the type of cancer, treatment regimen, and individual patient response.
4. You can’t have children after chemotherapy
Fertility preservation is a significant concern for many cancer patients undergoing chemotherapy. While some chemotherapy drugs can affect fertility, this is not always the case, and many patients can still have children after treatment. Advances in fertility preservation techniques, such as sperm banking, egg freezing, and ovarian tissue preservation, offer options for patients who wish to have children in the future. It is essential for patients to discuss their fertility concerns with their healthcare team before starting treatment to explore available options. Therefore, the belief that chemotherapy inevitably leads to infertility is a misconception, as many patients successfully preserve their fertility and have children post-treatment.
5. Chemotherapy means the cancer is very serious
Chemotherapy is used to treat various stages and types of cancer, not just the most serious cases. It can be part of a curative treatment plan, used to shrink tumors before surgery, or administered to prevent cancer recurrence. Additionally, chemotherapy is sometimes used for palliative purposes to relieve symptoms and improve quality of life in advanced cancer cases. The decision to use chemotherapy depends on multiple factors, including the type of cancer, its stage, and the overall treatment goals. Therefore, the use of chemotherapy does not necessarily indicate that the cancer is very serious; it is a versatile treatment option employed in various clinical scenarios.
FAQs
1. Can chemotherapy be personalized for each patient?
Yes, personalized or precision chemotherapy is an evolving area of oncology. Oncologists can sometimes tailor chemotherapy regimens based on the genetic makeup of the tumor and the patient’s response to previous treatments. Biomarker testing and genomic profiling of tumors are increasingly used to select the most effective chemotherapeutic agents, minimizing side effects.
2. What lifestyle changes can help manage chemotherapy side effects?
Adopting a healthy diet, staying hydrated, engaging in light physical activity like walking or yoga, and managing stress through mindfulness or relaxation techniques can help alleviate side effects such as fatigue, nausea, and anxiety. Consulting with a nutritionist or physical therapist can provide tailored strategies during chemotherapy.
3. Can chemotherapy be used with alternative treatments?
Some patients explore complementary therapies like acupuncture, meditation, or herbal supplements to help manage side effects. However, it is essential to consult with a healthcare provider before integrating any alternative treatments, as some may interfere with chemotherapy’s effectiveness or cause unwanted side effects.
4. How is the dosage of chemotherapy determined?
The dosage is usually calculated based on factors such as the patient’s body surface area (BSA), the type and stage of cancer, previous treatments, and overall health. Oncologists also adjust doses to minimize side effects while maintaining treatment efficacy.
5. What are “chemo brain” or cognitive side effects of chemotherapy?
Some patients experience memory problems, difficulty concentrating, or cognitive impairments during or after chemotherapy, commonly referred to as “chemo brain.” These issues can vary in severity and duration but often improve over time. Cognitive exercises and support from healthcare professionals can help manage these symptoms.
6. Is chemotherapy safe for elderly patients?
Chemotherapy can be used in elderly patients, but treatment plans may be adjusted based on the individual’s overall health, co-existing medical conditions, and ability to tolerate the side effects. Geriatric assessments are often used to determine the best approach for older patients.
7. Can chemotherapy affect mental health?
Chemotherapy can have emotional and psychological impacts, including anxiety, depression, and mood swings. It’s important for patients to seek mental health support or counseling if needed, as emotional well-being is crucial during cancer treatment.
8. How can I prepare for chemotherapy sessions?
Patients can prepare by discussing the treatment plan with their healthcare team, arranging for transportation, packing comfort items, staying hydrated, and ensuring they have adequate nutritional support. It’s also helpful to bring a friend or family member for emotional support.
9. What happens if chemotherapy isn’t effective?
If a particular chemotherapy regimen isn’t working, oncologists may recommend changing the treatment plan, exploring other therapies like immunotherapy or targeted therapy, or considering clinical trials. Treatment goals may shift from curative to palliative care if necessary.
10. How long after chemotherapy does it take for normal cells to recover?
The recovery of normal cells varies by individual and the type of chemotherapy used. Some cells, like those in the bone marrow, may take a few weeks to recover, while others may take longer. Regular follow-up appointments are important to monitor recovery.