Gums, also known as gingivae, are the fibrous tissues covered by mucous membrane that envelop the alveolar processes of the upper and lower jaws and surround the necks of the teeth. They serve as a protective barrier, closely adapted to the necks of the teeth and covering the bone that holds the roots of the teeth. Healthy gums are typically coral pink, though they may exhibit physiological pigmentation, and they play a crucial role in maintaining oral health by protecting the teeth and their supporting structures. Inflammation of the gums, known as gingivitis, is characterized by redness, swelling, and a tendency to bleed easily, often due to the accumulation of bacterial plaque. If left untreated, gingivitis can progress to periodontitis, leading to the loss of soft tissue and bone that support the teeth.
Anatomy of Gums
Structure of the Gingivae
The gingiva, commonly known as the gums, is composed of three main parts: the attached gingiva, free gingiva, and interdental papilla. The attached gingiva is firmly bound to the underlying bone, providing stability and protection to the teeth and jawbone. The free gingiva, also known as marginal gingiva, is the unattached portion that forms the soft tissue wall of the gingival sulcus around the teeth. The interdental papilla is the part of the gingiva that occupies the space between adjacent teeth. It has a unique molecular composition, with higher expression of wound healing molecules like integrin alphavbeta6 and cytokeratin 19, indicating its distinct cellular properties compared to other gingival parts.
The Tissue Composition
The gingiva consists of both keratinized and non-keratinized tissues. The attached gingiva and the outer surface of the free gingiva are keratinized, providing a tough, protective layer that resists mechanical stress and bacterial invasion. This keratinized tissue is crucial for maintaining periodontal health, as it forms a barrier against pathogens. In contrast, the inner lining of the gingival sulcus and the interdental papilla are non-keratinized, making them more susceptible to inflammation and disease. Studies have shown that the width of the keratinized gingiva increases with age, particularly after the eruption of permanent teeth, which enhances its protective function.
How Gums Support the Teeth and Jawbone
The gums play a vital role in supporting the teeth and jawbone by providing a stable and protective environment. The attached gingiva anchors the teeth to the alveolar bone, preventing tooth movement and protecting the underlying bone from bacterial invasion. The free gingiva forms a seal around the teeth, preventing food particles and bacteria from entering the periodontal pockets. The interdental papilla fills the spaces between teeth, preventing food impaction and protecting the interdental bone. Research indicates that even in the absence of attached gingiva, meticulous plaque control can maintain periodontal health, highlighting the importance of oral hygiene in conjunction with the structural support provided by the gums.
Function of Gums
Gums play a vital role in maintaining oral health and functionality. They provide essential support and protection to the teeth and underlying structures, contributing to overall dental well-being. Below are the key functions of gums:
1. Support and Anchor Teeth
Gums play a crucial role in supporting and anchoring teeth. They form a protective barrier around the teeth, helping to hold them in place within the jawbone. This support is essential for maintaining the stability and alignment of teeth, which is vital for proper chewing and speaking functions. The connective tissues within the gums, such as collagen fibers, attach the teeth to the alveolar bone, providing the necessary support to withstand the forces exerted during mastication. Without healthy gums, teeth can become loose and may eventually fall out, leading to significant oral health issues.
2. Protect Underlying Structures
Gums serve as a protective shield for the underlying structures of the mouth, including the roots of the teeth and the jawbone. They help to prevent the invasion of bacteria and other harmful agents that can cause infections and diseases such as periodontitis. By maintaining a tight seal around the teeth, gums prevent the exposure of sensitive areas to external irritants. This protective function is crucial for preserving the overall health of the oral cavity and preventing conditions that can lead to tooth loss and other complications.
3. Seal and Protect
The gums create a seal around the teeth, which is essential for protecting the deeper periodontal structures from bacterial invasion and mechanical damage. This seal helps to prevent food particles and bacteria from entering the spaces between the teeth and gums, which can lead to infections and inflammation. The integrity of this seal is vital for maintaining oral health, as any breach can result in periodontal pockets where bacteria can thrive, leading to gum disease and other oral health issues.
4. Aid in Chewing
Gums play a significant role in the process of chewing by providing a cushioning effect that helps to absorb the forces generated during mastication. This cushioning protects the teeth and the underlying bone from excessive stress and potential damage. Additionally, healthy gums contribute to the overall efficiency of the chewing process by ensuring that the teeth remain stable and properly aligned, which is essential for effective grinding and breaking down of food.
5. Contribute to Oral Health
Gums are integral to maintaining overall oral health. They help to prevent dental caries by providing a barrier against bacteria and by supporting the teeth in their proper positions. Healthy gums also contribute to the prevention of bad breath and other oral health issues by reducing the accumulation of plaque and food particles. Regular oral hygiene practices, including brushing and flossing, are essential for maintaining healthy gums and, consequently, overall oral health.
6. Sensory Function
Gums have a sensory function that helps to detect changes in pressure, temperature, and pain. This sensory feedback is crucial for protecting the teeth and oral structures from potential harm. For example, the gums can sense when a piece of food is too hard or when there is an injury, prompting a protective response. This sensory capability helps to prevent damage to the teeth and other oral structures by alerting the individual to potential dangers.
7. Blood Supply
Gums have a rich blood supply that is essential for delivering nutrients and oxygen to the tissues, promoting healing and maintaining overall gum health. This blood supply also helps to remove waste products and toxins from the gum tissues, reducing the risk of infections and inflammation. A healthy blood supply is crucial for the regeneration and repair of gum tissues, which is vital for maintaining the integrity and function of the gums.
Types of Gum Tissues
Gum tissues, or gingiva, are essential for maintaining oral health and protecting the teeth and underlying structures. Different types of gum tissues serve various functions and are located in specific areas of the mouth. Below are the main types of gum tissues:
1. Marginal or Free Gingiva
The marginal or free gingiva is the part of the gum tissue that surrounds the teeth and forms a collar around the tooth. It is not directly attached to the underlying bone, allowing it to be flexible and adapt to the movements of the teeth. This tissue plays a crucial role in protecting the periodontal ligament and the underlying bone from bacterial invasion and mechanical trauma. According to a study using optical coherence tomography (OCT), the marginal gingiva can be assessed noninvasively to determine its health and structural integrity, which is essential for diagnosing periodontal diseases. The study highlights the importance of this tissue in maintaining overall periodontal health.
2. Attached Gingiva
The attached gingiva is the portion of the gum tissue that is firmly bound to the underlying alveolar bone. It extends from the free gingiva to the mucogingival junction. This tissue is essential for withstanding the mechanical forces of mastication and providing stability to the teeth. A longitudinal study examining children during the mixed dentition period found that the width of the attached gingiva increases significantly as permanent teeth erupt, which is crucial for maintaining periodontal health. The study also noted that the attached gingiva becomes wider over time, contributing to the overall stability and health of the periodontal structure.
3. Alveolar Mucosa
The alveolar mucosa is the soft tissue that covers the alveolar bone and extends from the mucogingival junction to the vestibular area of the mouth. Unlike the attached gingiva, the alveolar mucosa is loosely attached to the underlying bone, making it more flexible. This tissue is less keratinized and more vascular, which makes it more susceptible to injury and inflammation. The use of advanced imaging techniques like OCT has shown that the alveolar mucosa has distinct structural and vascular characteristics compared to other types of gingival tissues, which can be crucial for diagnosing and treating periodontal diseases. Understanding these differences is essential for effective periodontal therapy.
4. Interdental Gingiva
The interdental gingiva, also known as the interdental papilla, is the part of the gum tissue that occupies the space between adjacent teeth. This tissue is crucial for preventing food impaction and protecting the underlying periodontal structures. The health of the interdental gingiva is a key indicator of overall periodontal health. Studies have shown that the interdental gingiva can vary significantly in thickness and vascularity, which can affect its susceptibility to inflammation and disease. Noninvasive imaging techniques like OCT can provide detailed information about the microstructure and vascularity of the interdental gingiva, aiding in the early diagnosis and treatment of periodontal conditions.
Common Gum Issues
Gum issues can significantly impact oral health and overall well-being. Understanding the common problems that affect the gums is essential for prevention and treatment. Below are some of the most prevalent gum issues:
1. Gingivitis
Gingivitis is a reversible inflammatory condition of the gums caused by the accumulation of dental plaque. It is characterized by redness, swelling, and a tendency for the gums to bleed easily. If left untreated, gingivitis can progress to periodontitis, leading to the loss of soft tissue and bone support for the teeth. Effective management includes mechanical oral hygiene procedures such as toothbrushing and flossing, and the use of adjunctive treatments like chlorhexidine mouthrinse, which has been shown to significantly reduce plaque and gingival inflammation. However, prolonged use of chlorhexidine can cause adverse effects like tooth staining and taste disturbances.
2. Periodontitis
Periodontitis is a chronic inflammatory condition resulting from the accumulation of plaque and tartar between the teeth and gums, leading to the destruction of the supporting tissues of the teeth. Symptoms include swollen, red, and bleeding gums, bad breath, and increased tooth sensitivity. If untreated, it can result in tooth loss and changes in tooth alignment. Treatment involves professional cleaning to remove plaque and tartar, the use of antibiotics, and in severe cases, surgery. Regular dental check-ups and good oral hygiene practices are essential for managing and preventing periodontitis.
3. Gum Recession
Gum recession is the process where the margin of the gum tissue surrounding the teeth wears away, exposing more of the tooth or its root. This can result from periodontal diseases like gingivitis and periodontitis, aggressive tooth brushing, or genetic factors. Symptoms include tooth sensitivity, visible roots, and longer-looking teeth. Treatment options vary depending on the severity and may include deep cleaning, scaling, root planning, and surgical procedures like gum grafting. Maintaining good oral hygiene and using a soft-bristled toothbrush can help prevent further gum recession.
4. Gum Abscesses
A gum abscess is a localized collection of pus within the gum tissue, often resulting from bacterial infection. It can cause severe pain, swelling, and redness in the affected area, and may lead to fever and general malaise. The primary treatment involves draining the abscess to remove the pus, followed by cleaning the infected area. Antibiotics may be prescribed to control the infection. Good oral hygiene and regular dental visits are crucial in preventing gum abscesses, as they often arise from untreated periodontal diseases.
5. Pregnancy Gingivitis
Pregnancy gingivitis is a common condition characterized by gum inflammation, swelling, and bleeding due to hormonal fluctuations during pregnancy. Elevated levels of estrogen and progesterone increase blood circulation to the gums, making them more sensitive to plaque and prone to inflammation. Factors such as morning sickness, dietary changes, and decreased dental care practices can exacerbate the condition. Maintaining good oral hygiene and regular dental check-ups are essential to manage pregnancy gingivitis and prevent its progression to more severe periodontal diseases.
6. Gum Inflammation
Gum inflammation, or gingivitis, is a common condition that can progress to periodontitis if left untreated. It is often caused by the accumulation of dental plaque and is characterized by redness, swelling, and bleeding gums. Good oral hygiene practices, including regular brushing and flossing, can effectively manage and prevent gum inflammation. In some cases, professional dental cleaning and the use of antiseptic mouthrinse like chlorhexidine may be necessary to control the condition. Early detection and treatment are crucial to prevent the progression to more severe periodontal diseases.
Common Causes of Gum Problems
Gum problems can arise from a variety of factors, many of which are preventable with proper care and lifestyle choices. Understanding these causes is crucial for maintaining healthy gums and overall oral health. Below are some common causes of gum problems:
1. Poor Oral Hygiene
Poor oral hygiene is a significant contributor to gum problems. Inadequate brushing and flossing can lead to the accumulation of plaque, which harbors bacteria that cause gum inflammation and periodontal disease. Studies have shown that good oral hygiene practices, such as daily tooth brushing and regular dental visits, can reduce the risk of head and neck cancers, which are often associated with poor oral health. Additionally, structured oral hygiene, including the use of fluoridated toothpaste and interdental brushes, is essential in preventing gingivitis and periodontitis.
2. Smoking and Tobacco Use
Smoking and the use of tobacco products are well-known risk factors for gum disease. Tobacco use can exacerbate periodontal disease by impairing blood flow to the gums, reducing the immune response, and promoting the growth of harmful bacteria. Research indicates that the habit of chewing tobacco is associated with an elevated risk of severe periodontitis and upper aerodigestive tract cancers. Moreover, the application of tobacco products like mishri on gums significantly increases the risk of gum problems.
3. Hormonal Changes
Hormonal changes, particularly during pregnancy, menstruation, and menopause, can affect gum health. These changes can increase blood flow to the gums, making them more sensitive and prone to inflammation and bleeding. Although specific studies on hormonal changes were not provided, it is well-documented that hormonal fluctuations can exacerbate existing gum conditions and make the gums more susceptible to plaque and bacteria.
4. Medications
Certain medications can contribute to gum problems by causing dry mouth, which reduces saliva flow and its protective effects on the gums. Medications such as antihypertensives, antidepressants, and antihistamines can lead to xerostomia, increasing the risk of gum disease. While the provided data did not specifically address medications, it is widely recognized that dry mouth can lead to an increased risk of periodontal disease and other oral health issues.
5. Nutritional Deficiencies
Nutritional deficiencies, particularly in vitamins and minerals, can adversely affect gum health. A diet lacking in essential nutrients like vitamin C, vitamin D, and calcium can weaken the immune system and the structural integrity of the gums. Research highlights the importance of a balanced diet and the role of micronutrients in preventing periodontal diseases. Proper nutrition, including antioxidants and probiotics, is crucial for maintaining good oral health and preventing gum problems.
6. Systemic Diseases
Systemic diseases such as diabetes, cardiovascular diseases, and respiratory infections can have a profound impact on gum health. Periodontitis has been linked to systemic inflammation and is associated with an increased risk of cardiovascular diseases and diabetes complications. The presence of systemic diseases can exacerbate gum problems, making it essential to manage these conditions to maintain oral health.
7. Genetics
Genetics play a role in an individual’s susceptibility to gum disease. Genetic factors can influence the immune response, the structure of the gums, and the body’s ability to fight off infections. Although the provided data did not specifically address genetics, it is well-established that genetic predisposition can increase the risk of developing periodontal disease and other gum-related issues.
8. Age
Age is a significant factor in gum health, with older adults being more susceptible to gum problems. The ageing population, particularly those in institutionalized settings, often experiences poor oral health due to factors like reduced self-care ability and systemic conditions. Studies have shown that a high percentage of elderly residents have moderate to severe periodontitis, which is associated with poor oral health-related quality of life.
9. Stress
Stress can negatively impact gum health by weakening the immune system and increasing the production of harmful substances like cortisol. Chronic stress can lead to behaviors such as teeth grinding and poor oral hygiene, further exacerbating gum problems. While the provided data did not specifically address stress, it is widely recognized that stress management is crucial for maintaining overall health, including oral health.
10. Teeth Grinding or Clenching
Teeth grinding or clenching, also known as bruxism, can cause significant damage to the gums and supporting structures of the teeth. This habit can lead to gum recession, increased tooth mobility, and periodontal disease. Although the provided data did not specifically address bruxism, it is well-known that managing this condition through dental interventions and stress reduction techniques is essential for preventing gum problems.
11. Crooked Teeth or Misaligned Bite
Crooked teeth or a misaligned bite can create areas that are difficult to clean, leading to plaque accumulation and gum disease. Proper functional tooth alignment is important for optimal mechanical cleaning and preventing plaque accumulation. The use of removable aligners, as opposed to fixed orthodontic appliances, is recommended for better accessibility for mechanical hygiene measures.
How to Maintain Healthy Gums
Maintaining healthy gums is essential for overall oral health and can prevent various dental issues. By following a few key practices, you can ensure your gums remain strong and disease-free. Below are some effective ways to maintain healthy gums:
1. Practice proper oral hygiene
Maintaining proper oral hygiene is essential for healthy gums and overall oral health. Regular brushing and flossing help remove dental plaque, which is the primary cause of gum disease and tooth decay. Studies have shown that using interdental cleaning devices, such as floss and interdental brushes, in addition to toothbrushing, can significantly reduce gingivitis and plaque more than toothbrushing alone. Additionally, good oral hygiene practices, including daily tooth brushing and regular dental check-ups, have been associated with a reduced risk of head and neck cancers. Therefore, incorporating a comprehensive oral hygiene routine is crucial for maintaining healthy gums.
2. Get regular dental check-ups
Regular dental check-ups are vital for maintaining healthy gums and preventing oral diseases. Dental visits allow for early detection and treatment of gum disease, cavities, and other oral health issues. Research indicates that annual dental visits are associated with a lower risk of head and neck cancers, as they help in maintaining good oral hygiene and identifying potential problems early. Moreover, dental check-ups can provide professional cleaning that removes plaque and tartar buildup, which are difficult to eliminate with regular brushing and flossing alone. Therefore, scheduling regular dental appointments is essential for long-term gum health.
3. Quit smoking and limit alcohol consumption
Quitting smoking and limiting alcohol consumption are crucial steps in maintaining healthy gums. Smoking and high alcohol intake are significant risk factors for oral cancer and gum disease. Studies have shown that smoking more than 10 cigarettes per day and long-term alcohol consumption significantly increase the risk of oral cancer. Additionally, smoking is associated with gum disease, peri-implantitis, and delayed wound healing after dental procedures. Reducing or eliminating these habits can significantly lower the risk of developing serious oral health issues and contribute to healthier gums.
4. Maintain a balanced, nutritious diet
A balanced, nutritious diet plays a vital role in maintaining healthy gums. Consuming a diet rich in fruits, vegetables, and whole grains provides essential nutrients that support gum health and overall oral hygiene. Research has shown that a diet adequate in green, yellow, and cruciferous vegetables, as well as citrus fruits, can protect against oral cancer and improve oral health. Additionally, limiting sugary foods and beverages helps prevent tooth decay and gum disease. Therefore, adopting a nutritious diet is essential for promoting healthy gums and preventing oral health problems.
5. Stay hydrated
Staying hydrated is important for maintaining healthy gums and overall oral health. Adequate water intake helps in the production of saliva, which is essential for neutralizing acids produced by bacteria in the mouth and washing away food particles. Saliva also contains enzymes that aid in the digestion of food and protect against tooth decay and gum disease. Dehydration can lead to dry mouth, which increases the risk of cavities and gum disease. Therefore, drinking plenty of water throughout the day is crucial for keeping the gums healthy and maintaining good oral hygiene.
6. Manage stress
Managing stress is important for maintaining healthy gums, as stress can negatively impact oral health. High stress levels can lead to behaviors such as teeth grinding, poor oral hygiene, and unhealthy eating habits, which can contribute to gum disease and other oral health issues. Additionally, stress can weaken the immune system, making it harder for the body to fight off infections, including those affecting the gums. Therefore, adopting stress management techniques, such as regular exercise, meditation, and adequate sleep, can help in maintaining healthy gums and overall well-being.
7. Be gentle when brushing
Being gentle when brushing is crucial for maintaining healthy gums and preventing damage. Using a soft-bristled toothbrush and gentle brushing techniques can effectively remove plaque without causing harm to the gums. Aggressive brushing can lead to gum recession, enamel wear, and increased sensitivity. Studies emphasize the importance of selecting the appropriate toothbrush and mastering the correct brushing technique to avoid potential damage to the gums while effectively removing dental plaque. Therefore, adopting gentle brushing habits is essential for preserving gum health and preventing oral health issues.
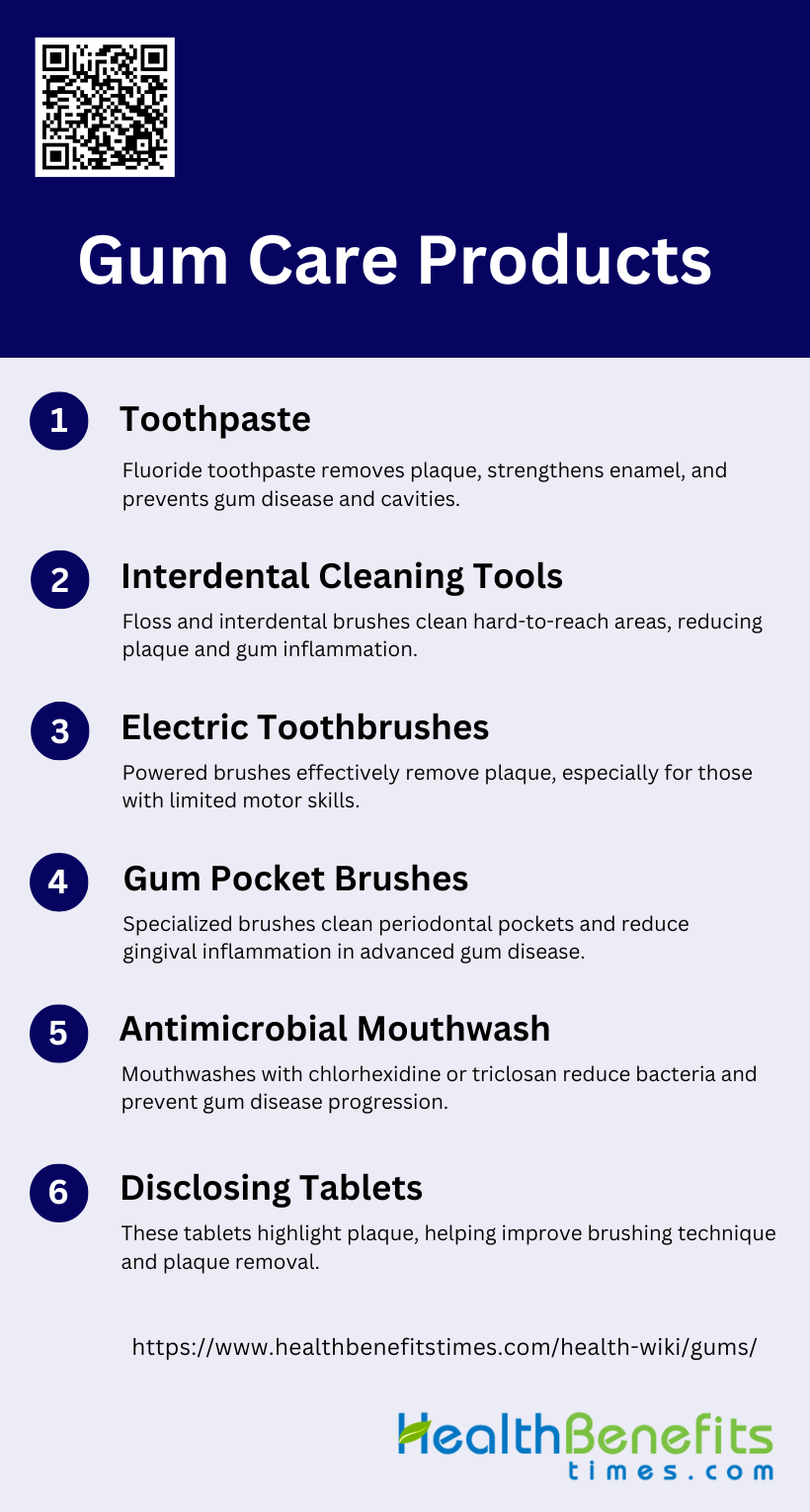
Gum Care Products
Using the right gum care products can significantly enhance your oral hygiene routine and promote healthier gums. These products are designed to target specific areas and issues, ensuring comprehensive care. Below are some essential gum care products:
1. Toothpaste
Toothpaste plays a crucial role in daily oral hygiene by helping to remove plaque and prevent dental caries and periodontal diseases. Fluoride toothpaste is particularly effective in strengthening enamel and preventing tooth decay. Detergents like sodium lauryl sulfate in toothpaste enhance cleaning action but may irritate sensitive mucous membranes, especially in patients undergoing chemotherapy or radiotherapy. Additionally, antimicrobial agents such as triclosan and chlorhexidine in toothpaste can significantly reduce bacterial load, contributing to better oral health outcomes. Therefore, selecting the right toothpaste, especially one with fluoride, is essential for maintaining optimal oral hygiene.
2. Interdental Cleaning Tools
Interdental cleaning tools, such as floss, interdental brushes, and oral irrigators, are essential for removing plaque from areas that toothbrushes cannot reach. Studies have shown that using these tools in addition to toothbrushing can reduce gingivitis and plaque more effectively than toothbrushing alone. Interdental brushes have been found to be superior to floss in reducing plaque, although their impact on gingival inflammation is less clear. Oral irrigators also show beneficial effects on bleeding and gingival indices, making them a valuable adjunct to daily oral hygiene routines. Proper instruction on the use of these tools is crucial for maximizing their effectiveness.
3. Electric Toothbrushes
Electric toothbrushes have gained popularity due to their efficacy in biofilm removal and ease of use, which can lead to increased patient compliance. Although no specific type of toothbrush has been consistently proven superior, powered brushes have shown promising results in short-term studies. They are particularly beneficial for individuals with limited motor skills, such as the elderly or those recovering from chemotherapy, as they can more effectively remove plaque without causing mucosal trauma. However, long-term studies are needed to fully understand their impact on periodontal health.
4. Gum Pocket Brushes
Gum pocket brushes are specialized tools designed to clean periodontal pockets and reduce gingival inflammation. These brushes can reach areas that regular toothbrushes and even some interdental cleaning tools cannot, making them particularly useful for patients with advanced periodontal disease. While evidence on their effectiveness is limited, they are often recommended as part of a comprehensive oral hygiene routine to manage periodontitis and prevent further progression of the disease. Proper use and regular cleaning of these brushes are essential to avoid introducing bacteria into the periodontal pockets.
5. Antimicrobial Mouthwash
Antimicrobial mouthwashes, containing agents like chlorhexidine and triclosan, are effective in reducing plaque and gingivitis when used correctly. These mouthwashes can significantly lower the bacterial load in the mouth, contributing to better oral health outcomes. They are particularly beneficial for patients with compromised oral hygiene, such as those undergoing chemotherapy or radiotherapy, as they help manage sensitive mucosal conditions and prevent infections. However, long-term use of some antimicrobial agents may lead to side effects, so they should be used as directed by a healthcare professional.
6. Disclosing Tablets
Disclosing tablets are a valuable tool for visualizing plaque on teeth, helping individuals identify areas that need more thorough cleaning. These tablets stain plaque, making it easier to see and remove during brushing and interdental cleaning. They are particularly useful for educating patients about effective oral hygiene practices and improving their brushing techniques. By highlighting missed areas, disclosing tablets can motivate individuals to adopt better oral hygiene habits, ultimately leading to improved periodontal health. Regular use of disclosing tablets can enhance the effectiveness of daily oral care routines.
FAQs
1. Can gum health affect overall body health?
Yes, gum health can have a significant impact on overall body health. Poor gum health, especially conditions like periodontitis, has been linked to systemic issues such as cardiovascular diseases, diabetes, and respiratory infections. The inflammation in the gums can spread and affect other parts of the body, potentially worsening or contributing to other health conditions.
2. Can healthy gums still bleed?
While bleeding gums are often a sign of gum disease or irritation, healthy gums may sometimes bleed due to vigorous brushing or flossing. However, consistent bleeding, even with gentle brushing, is a sign that you should visit a dentist to check for underlying gum issues.
3. What are the signs of healthy gums?
Healthy gums are typically firm, coral pink in color (though they can have pigmentation depending on the individual), and do not bleed easily. They should fit tightly around the teeth and provide support for them without showing signs of swelling or inflammation.
4. How do hormonal changes affect gum health?
Hormonal fluctuations during pregnancy, menstruation, or menopause can increase the sensitivity of gums, making them more prone to inflammation, swelling, and bleeding. These hormonal changes can worsen existing gum problems or trigger new ones, making good oral hygiene and regular dental check-ups especially important during these times.
5. Are gum diseases reversible?
Gingivitis, the early stage of gum disease, is reversible with proper oral care and treatment. However, if it progresses to periodontitis, the damage to the gums and bone is usually irreversible, though the disease can be managed to prevent further deterioration.
6. Can receding gums grow back?
Receding gums do not grow back naturally. However, treatments like gum grafting or pinhole surgery can help restore gum coverage over the teeth. Maintaining good oral hygiene and seeing a dentist regularly can help prevent further gum recession.
7. How does age impact gum health?
As people age, they are more prone to gum recession and periodontal disease due to factors like reduced saliva production, wear and tear on the gums, and the cumulative effects of oral hygiene over time. Older adults may need more diligent care to maintain gum health.
8. Is gum inflammation always painful?
Not necessarily. While gum inflammation (gingivitis) can cause discomfort or tenderness, it is not always painful. This is why many people may not realize they have gum disease until it progresses to a more severe stage.
9. What are the differences between gingivitis and periodontitis?
Gingivitis is the early, reversible stage of gum disease characterized by inflamed, red, and bleeding gums. Periodontitis is a more advanced form of gum disease, where the inflammation affects the bone and tissue supporting the teeth, potentially leading to tooth loss if left untreated.
10. Can medications affect gum health?
Yes, certain medications, such as antihistamines, antidepressants, and blood pressure drugs, can cause dry mouth or reduce saliva production, which can increase the risk of gum disease. Other medications, such as anti-seizure drugs, may cause gum overgrowth, leading to further gum issues.