Telehealth, also known as telemedicine, refers to the use of electronic communication technologies to exchange medical information from one site to another to improve a patient’s health. It encompasses a wide range of applications, including videoconferencing, remote monitoring, and electronic consultations, which can be used to deliver healthcare services to patients in remote or underserved areas, thereby reducing the need for travel and improving access to care. Telehealth has been shown to be effective in managing various health conditions, including chronic diseases and mental health issues, and is associated with high levels of patient satisfaction due to its convenience and the quality of care provided. Despite its benefits, the integration of telehealth into mainstream healthcare systems faces challenges such as technological barriers and the need for sustainable models of care.
Differentiation between telehealth and telemedicine
Telehealth and telemedicine, while often used interchangeably, have distinct definitions and applications within the healthcare framework. Telemedicine specifically refers to the use of information and communication technology (ICT) by clinicians to deliver clinical services such as diagnosis, treatment, and prevention of diseases remotely. It is a subset of telehealth, which encompasses a broader range of services beyond clinical care, including remote patient monitoring, health education, public health, and health administration. Telehealth thus serves as an umbrella term that includes telemedicine but also extends to non-clinical services aimed at improving overall health outcomes and healthcare delivery. The distinction is crucial for understanding the scope and implementation of these technologies in various healthcare settings, especially as their adoption has surged in response to the COVID-19 pandemic.
Examples of telehealth services
Telehealth services encompass a wide range of healthcare delivery methods that utilize digital technology to provide medical care remotely. These services improve access to healthcare, especially for individuals in remote or underserved areas, and enhance the efficiency of medical consultations. Below are some examples of telehealth services that are transforming the healthcare landscape:
1. Live Video Conferencing
Live video conferencing is a cornerstone of telehealth services, enabling real-time interaction between patients and healthcare providers. This method is particularly beneficial for individuals in rural or remote areas, as it eliminates the need for travel and provides immediate access to medical consultations. Studies have shown high levels of satisfaction among patients and caregivers using telehealth videoconferencing, citing improved access to care and convenience as key benefits. Additionally, during the COVID-19 pandemic, live video conferencing was rapidly integrated into prenatal care to minimize exposure risks while maintaining essential health services.
2. Store-and-Forward
Store-and-forward telehealth involves the collection and transmission of medical data, such as images or biosignals, to a healthcare provider for later review. This asynchronous method is particularly useful for specialties like dermatology, radiology, and pathology, where immediate interaction is not necessary. For example, spirometry results can be stored over a period and then forwarded to a healthcare provider for analysis and feedback. This method enhances the efficiency of healthcare delivery by allowing providers to review and respond to patient data at their convenience, thus optimizing resource utilization and patient care.
3. Remote Patient Monitoring (RPM)
Remote patient monitoring (RPM) uses technology to track patients’ health data outside traditional clinical settings, often in real-time. This approach is particularly beneficial for managing chronic conditions such as diabetes, heart disease, and respiratory illnesses. RPM has been shown to reduce hospital readmissions and improve health outcomes by enabling continuous monitoring and timely interventions. In pediatric settings, RPM helps manage chronic conditions and reduces the need for frequent hospital visits, thereby improving the quality of life for both patients and their families.
4. Mobile Health (mHealth)
Mobile health (mHealth) leverages mobile devices like smartphones and tablets to deliver healthcare services and information. This modality includes mobile apps for health monitoring, reminders for medication adherence, and educational resources. mHealth is particularly effective in supporting self-management of chronic conditions and promoting healthy behaviors. For adolescents with allergic conditions, mobile applications have been used to enhance self-management skills, showing positive effects on health outcomes and engagement. The flexibility and accessibility of mHealth make it a valuable tool in modern healthcare.
5. Virtual Visits
Virtual visits involve remote consultations between patients and healthcare providers using video conferencing technology. These visits can cover a wide range of medical services, from routine check-ups to specialist consultations. During the COVID-19 pandemic, virtual visits became a critical component of healthcare delivery, helping to reduce exposure risks while maintaining continuity of care. Patients have reported high satisfaction with virtual visits due to their convenience and the ability to receive timely medical advice without the need for physical travel.
6. Remote Specialist Consultations
Remote specialist consultations allow patients to access expert medical advice without the need to travel to specialized healthcare facilities. This is particularly beneficial for individuals in rural or underserved areas. Telehealth platforms enable specialists to review patient data, conduct virtual examinations, and provide recommendations remotely. This approach not only improves access to specialized care but also enhances the efficiency of healthcare delivery by reducing wait times and travel burdens. The integration of remote specialist consultations into routine practice has shown promise in various medical fields, including neurology and cardiology.
7. Prenatal and Postpartum Care
Telehealth has been effectively integrated into prenatal and postpartum care, especially during the COVID-19 pandemic. Virtual visits and remote monitoring have allowed healthcare providers to maintain essential prenatal screenings and consultations while minimizing the risk of virus exposure. Telehealth services have been tailored to address high-risk pregnancies, providing increased surveillance and specialized counseling for conditions such as preeclampsia and gestational diabetes. This approach ensures that expectant mothers receive continuous care and support throughout their pregnancy and postpartum period, improving maternal and fetal health outcomes.
8. Physical Therapy
Telehealth has expanded into physical therapy, offering remote sessions that include guided exercises, real-time feedback, and progress monitoring. This modality is particularly useful for patients recovering from surgery or managing chronic musculoskeletal conditions. Telephysical therapy allows patients to receive personalized care in the comfort of their homes, reducing the need for travel and increasing adherence to rehabilitation programs. Studies have shown that telephysical therapy can be as effective as in-person sessions, with the added benefits of convenience and flexibility.
9. Chronic Disease Management
Telehealth plays a crucial role in the management of chronic diseases by providing continuous monitoring, education, and support. Technologies such as RPM and mHealth apps enable patients to track their health metrics, receive medication reminders, and access educational resources. This continuous engagement helps in early detection of potential issues and timely interventions, thereby improving health outcomes and reducing hospitalizations. For conditions like diabetes, heart failure, and COPD, telehealth has proven to be an effective tool in enhancing patient self-management and overall quality of life.
How Telehealth Works
Process of a Typical Telehealth Appointment
A typical telehealth appointment begins with scheduling, which can be done through a hospital’s app or public platforms like WeChat. Patients are often required to set up an online patient portal account and download the necessary applications, such as Epic’s MyChart. On the day of the appointment, patients log in to the video conferencing platform at the scheduled time. The consultation itself is conducted via video, where the healthcare provider can discuss symptoms, provide diagnoses, and recommend treatments. If necessary, prescriptions can be sent electronically to the patient’s pharmacy. This process ensures that patients receive timely care without the need for in-person visits, which is particularly beneficial for those in remote areas.
Types of Technology Used
Telehealth leverages a variety of technologies to facilitate remote healthcare. Video conferencing platforms like Zoom Health and Video are commonly used for live consultations. Mobile apps, such as those developed by Epic Systems, allow patients to access their health records and communicate with healthcare providers. Additionally, health monitoring devices, including home blood pressure monitors and glucose meters, enable patients to track their vital signs and share this data with their providers during virtual visits. Advanced systems like VIGIL offer multi-point, multi-view video conferencing and can integrate data from wireless medical devices, enhancing the interactivity and effectiveness of telehealth sessions.
Privacy and Security Considerations
Privacy and security are critical in telehealth to protect patient data. Telehealth providers must comply with the Health Insurance Portability and Accountability Act (HIPAA), which mandates stringent data protection measures. Encryption is used to secure video consultations and data transmissions, ensuring that patient information remains confidential. To help telehealth providers assess their compliance with privacy and security standards, tools like the telehealth privacy and security self-assessment questionnaire have been developed. This questionnaire helps identify potential vulnerabilities and ensures that sufficient actions are taken to protect patient data. Despite these measures, ongoing vigilance is required to address new security challenges as telehealth technology evolves.
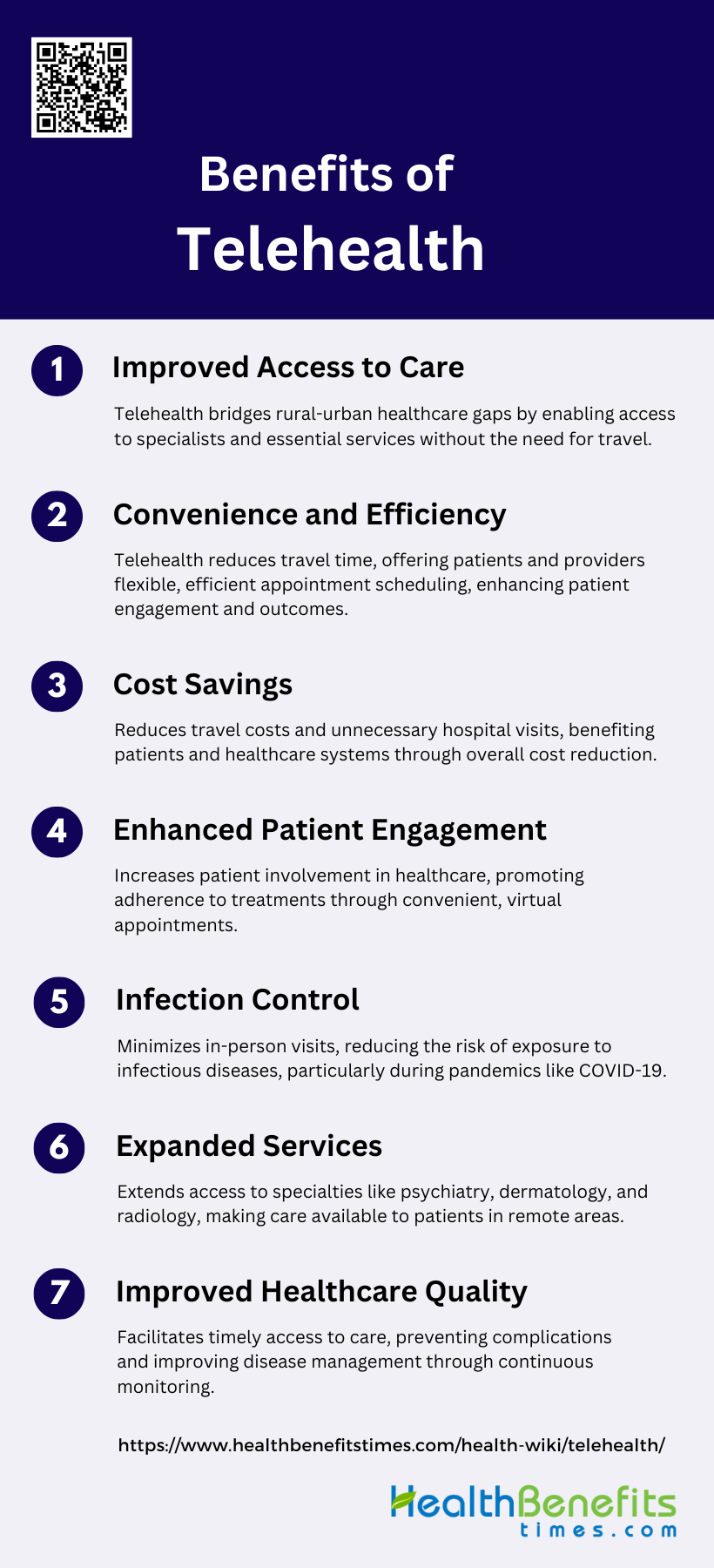
Benefits of Telehealth
Telehealth has revolutionized the healthcare industry by leveraging digital technologies to deliver medical services remotely. This approach offers numerous advantages that enhance the overall quality of care and patient experience. Below are some key benefits of telehealth:
1. Improved Access to Care
Telehealth significantly enhances access to healthcare services, particularly for individuals in rural and remote areas. By utilizing telehealth, patients can connect with specialists and receive high-quality care without the need to travel long distances, thereby reducing the urban-rural health disparities. This increased accessibility is especially beneficial for populations with limited healthcare resources, such as rural Australians and pediatric heart transplant patients, who can now receive timely consultations and follow-ups through telehealth platforms. Additionally, telehealth has been shown to improve access to mental health services, which are often scarce in remote locations.
2. Convenience and Efficiency
Telehealth offers unparalleled convenience and efficiency for both patients and healthcare providers. Patients can schedule and attend appointments from the comfort of their homes, eliminating the need for travel and reducing time off work. This convenience extends to healthcare providers as well, who can manage their schedules more flexibly and efficiently. The use of telehealth for transitions of care has demonstrated improved medication adherence and patient engagement, further enhancing the overall efficiency of healthcare delivery. Moreover, telehealth’s ability to provide real-time video consultations ensures that patients receive timely care, which can be crucial in managing acute conditions.
3. Cost Savings
Telehealth has the potential to generate significant cost savings for both patients and healthcare systems. By reducing the need for in-person visits, telehealth can lower travel expenses and associated costs for patients. For healthcare systems, telehealth can decrease the utilization of more expensive services, such as emergency department visits and hospital readmissions, leading to overall cost reductions. However, it is important to note that while some studies have found telehealth to be cost-effective, others have reported mixed results, indicating that the economic impact of telehealth may vary depending on the specific context and implementation.
4. Enhanced Patient Engagement
Telehealth has been shown to enhance patient engagement by providing patients with more control over their healthcare. The convenience of virtual visits encourages patients to be more proactive in managing their health, leading to better adherence to treatment plans and improved health outcomes. Studies have reported high levels of patient satisfaction with telehealth, with many patients expressing enthusiasm and confidence in the technology’s ability to improve their healthcare. Additionally, telehealth can facilitate better communication between patients and providers, fostering a more collaborative and engaged approach to healthcare.
5. Infection Control
Telehealth plays a crucial role in infection control by minimizing the need for in-person visits, thereby reducing the risk of exposure to infectious diseases. This benefit has been particularly evident during the COVID-19 pandemic, where telehealth has allowed patients to receive care while adhering to social distancing guidelines. By limiting physical interactions, telehealth helps protect both patients and healthcare providers from potential infections, contributing to safer healthcare environments. This aspect of telehealth is especially important for vulnerable populations, such as those with chronic conditions or compromised immune systems, who are at higher risk of severe infections.
6. Expanded Services
Telehealth enables the expansion of healthcare services to include a broader range of specialties and treatments. For example, telehealth has been successfully used in areas such as telepsychiatry, teledermatology, and teleradiology, providing patients with access to specialized care that may not be available locally. Additionally, telehealth can support the delivery of home care services, allowing patients with long-term conditions to receive continuous monitoring and support from their homes. This expansion of services through telehealth can lead to more comprehensive and integrated care, improving overall health outcomes.
7. Improved Healthcare Quality
The use of telehealth has been associated with improvements in the quality of healthcare delivery. By facilitating timely access to care and enabling continuous monitoring, telehealth can help prevent complications and improve disease management. Studies have shown that telehealth can lead to better medication adherence, enhanced patient satisfaction, and improved health outcomes. Furthermore, telehealth can support healthcare providers by offering opportunities for professional development and collaboration, ultimately contributing to higher standards of care. While some studies have reported mixed results regarding the effectiveness of telehealth, the overall trend suggests that telehealth can enhance the quality of healthcare services.
Challenges and Limitations of Telehealth
While telehealth offers numerous benefits, it also comes with its own set of challenges and limitations that can impact its effectiveness. These issues range from technological barriers to regulatory hurdles, each posing unique obstacles to the seamless delivery of remote healthcare. Below are some of the key challenges and limitations of telehealth:
1. Limited Physical Examination
One of the primary challenges of telehealth is the inability to conduct a thorough physical examination. This limitation can hinder accurate diagnosis and treatment, particularly in specialties that rely heavily on physical assessments, such as neurology and primary care. For instance, the absence of direct physical presence can make it difficult to perform comprehensive neurological exams, which are crucial for diagnosing conditions like brain tumors and vascular pathologies. Additionally, the lack of hands-on experience and diminished fidelity of observations can affect the quality of care provided through telehealth. These limitations necessitate the development of innovative solutions to enhance remote diagnostic capabilities.
2. Technology Issues
Technology-related challenges are significant barriers to the effective implementation of telehealth. Issues such as unreliable network connections, lack of access to necessary technology, and insufficient technology skills among both patients and healthcare providers can impede the delivery of telehealth services. Moreover, technical difficulties can disrupt the flow of consultations, leading to patient and provider frustration. The need for stable infrastructure, comprehensive training, and user-friendly platforms is critical to overcoming these barriers and ensuring the smooth operation of telehealth services.
3. Privacy and Security Concerns
Privacy and security concerns are paramount in telehealth, as the transmission of sensitive patient information over digital platforms poses risks of data breaches and unauthorized access. Ensuring the confidentiality and protection of patient data is a complex challenge that involves adhering to stringent regulations and implementing robust security measures. Ethical aspects such as informed consent and data protection are critical to maintaining patient trust and compliance with legal standards. Addressing these concerns requires continuous updates to security protocols and adherence to best practices in data management.
4. Regulatory and Legal Challenges
Regulatory and legal challenges significantly impact the adoption and implementation of telehealth. Variations in state licensure requirements, medicolegal issues surrounding provider reimbursement, and malpractice liability are some of the barriers that complicate the widespread use of telehealth. The COVID-19 pandemic has prompted temporary regulatory changes to facilitate telehealth, but long-term solutions are needed to standardize practices and ensure compliance across different jurisdictions. Policymakers must address these regulatory hurdles to create a conducive environment for telehealth expansion.
5. Reimbursement Issues
Reimbursement policies play a crucial role in the adoption of telehealth services. Inconsistent and inadequate reimbursement for telehealth consultations can deter healthcare providers from offering these services. Medicaid reimbursement policies that promote live video and store-and-forward services have been associated with greater telehealth adoption, highlighting the importance of supportive reimbursement frameworks. Ensuring parity in reimbursement for telehealth and in-person visits is essential to incentivize providers and sustain telehealth services.
6. Implementation Barriers
Implementation barriers encompass a range of factors that hinder the effective deployment of telehealth services. These include operational workflow challenges, organizational readiness, and patient engagement issues. Additionally, the lack of clear clinical care guidelines and training for telehealth can impede its integration into routine practice. Addressing these barriers requires a multifaceted approach that includes developing comprehensive guidelines, enhancing organizational readiness, and fostering patient engagement to ensure the successful implementation and sustainability of telehealth services.
Who Can Benefit from Telehealth
Telehealth offers significant benefits to various patient groups, particularly the elderly, individuals with mobility issues, and residents of rural areas who face challenges in accessing traditional healthcare services. For instance, rural residents often experience high satisfaction with telehealth due to improved access to care and the convenience of avoiding long travel distances. Common conditions effectively managed through telehealth include mental health issues, chronic disease management such as type 2 diabetes, and dermatological conditions. In specialized care, telehealth has shown promise in pediatrics, physical therapy, and palliative home care, enhancing patient satisfaction and access to necessary services. Additionally, telehealth has been integrated into obstetrics and gynecology, demonstrating comparable health outcomes to traditional care while improving patient engagement and satisfaction. Overall, telehealth is a versatile tool that can enhance healthcare delivery across various patient demographics and medical conditions.
FAQs
1. What types of healthcare professionals can provide telehealth services?
Telehealth services can be provided by a range of healthcare professionals, including doctors, nurses, mental health professionals, physical therapists, nutritionists, and pharmacists. Each professional may utilize telehealth differently depending on their field of expertise.
2. How does telehealth impact patient-provider relationships?
While telehealth offers convenience, some patients and providers worry that it may limit the personal connection found in face-to-face visits. However, many studies suggest that telehealth can still foster strong relationships through consistent, accessible communication.
3. Can telehealth be used for emergency medical situations?
Telehealth is generally not recommended for emergencies. For situations like heart attacks or severe injuries, in-person medical attention or emergency services are essential. However, telehealth may provide immediate advice on minor urgent conditions.
4. How does telehealth address language barriers or cultural differences?
Some telehealth platforms offer language translation services or interpreters, but not all systems may have this capability. It’s important to check if the service supports language assistance or cultural accommodations before scheduling.
5. What are the equipment requirements for telehealth?
To use telehealth, patients typically need a device with internet access, such as a smartphone, tablet, or computer, and in some cases, peripherals like a webcam or microphone. For remote monitoring, specific health devices like glucose monitors or blood pressure cuffs may be required.
6. Are telehealth services covered by private insurance plans?
Coverage for telehealth services varies by insurance provider. While many insurers expanded coverage due to the COVID-19 pandemic, it is important to check with your insurance provider to understand what services are covered and at what cost.
7. Can prescriptions be issued through telehealth?
Yes, healthcare providers can issue prescriptions through telehealth consultations. The prescriptions are typically sent electronically to the patient’s preferred pharmacy for easy pick-up or delivery.
8. How are follow-up appointments managed with telehealth?
Follow-up appointments can be scheduled via telehealth platforms in much the same way as in-person visits. Patients may receive notifications or reminders through email, apps, or patient portals to ensure continuity of care.
9. What is the role of artificial intelligence (AI) in telehealth?
AI can be integrated into telehealth platforms to assist with diagnostics, patient monitoring, and even personalized care recommendations. For example, AI algorithms can analyze patient data from wearable devices and suggest interventions.
10. How can patients ensure they are using a secure telehealth platform?
Patients can ensure platform security by confirming that the telehealth service complies with healthcare privacy laws, such as HIPAA in the U.S., and by using encrypted video conferencing platforms. Additionally, they should ensure their own device security through regular updates and secure internet connections.