Puncture wounds are a type of injury characterized by a small, deep hole in the skin and underlying tissues, typically caused by a sharp, narrow object penetrating the body. These wounds can be caused by various objects such as nails, needles, animal bites, or other pointed instruments. Unlike cuts or lacerations, puncture wounds tend to have a smaller surface area but can extend deep into the body, potentially damaging internal structures. This depth makes puncture wounds particularly concerning due to the increased risk of infection, as bacteria can be introduced deep into the tissues where they may thrive in the absence of oxygen. Puncture wounds require careful attention and proper treatment, as they can lead to serious complications such as tetanus or, in some cases, osteomyelitis if not managed appropriately.
Characteristics of Puncture Wounds
Depth vs. Width
Puncture wounds are characterized by their depth relative to their width, distinguishing them from other types of wounds such as abrasions or cuts. A puncture wound typically has a small entry hole caused by a pointed object, such as a nail, which penetrates deeply into the tissue. In contrast, cuts are open wounds that create a long tear in the skin without significant depth, and abrasions are superficial injuries that scrape off the top layer of skin. The depth of puncture wounds can conceal serious injuries and increase the risk of complications like infections, making immediate and appropriate treatment crucial.
Types of Objects That Cause Puncture Wounds
Puncture wounds are caused by various pointed objects that can penetrate the skin and underlying tissues. Common culprits include nails, splinters, and animal teeth. These objects create small but deep entry points that can introduce foreign materials and bacteria into the body, leading to potential infections. For instance, stepping on a nail is a frequent cause of puncture wounds, especially in the foot. Animal bites, particularly from cats and dogs, can also result in puncture wounds due to their sharp teeth. The nature of these objects often necessitates prompt medical attention to prevent complications.
Common Areas Affected by Puncture Wounds
Puncture wounds frequently affect areas of the body that are more exposed or prone to contact with pointed objects, such as the hands and feet. The foot is particularly susceptible, especially during warm weather when people are more likely to go barefoot. This increases the risk of stepping on sharp objects like nails or splinters. The hands are also common sites for puncture wounds due to their involvement in various activities that may involve handling sharp tools or materials. Prompt and proper treatment of puncture wounds in these areas is essential to prevent infections and other complications.
Common Causes of Puncture Wounds
Puncture wounds are injuries that occur when a pointed object pierces the skin, creating a small but deep hole. These wounds can be caused by various factors and often require immediate attention to prevent infection and other complications. Below are some common causes of puncture wounds:
1. Sharp Objects
Puncture wounds caused by sharp objects are a common occurrence, particularly in medical settings. A study conducted in a tertiary care hospital revealed that over a 12-month period, 233 puncture wounds were reported, with the nursing department accounting for the majority of these injuries (68%). The clinical areas with the highest incidence rates included the clinical research center, the emergency room, and the surgical intensive care unit. Activities involving direct contact with sharp instruments, such as disposable syringes and loose needles, were the primary causes of these injuries. Recommendations from the study include redesigning sharp instruments and focusing educational programs on high-risk personnel to reduce the incidence of puncture wounds.
2. Animal Bites
Animal bites are a significant cause of puncture wounds, often resulting in severe injuries. A study highlighted that approximately 5000 patients are treated annually at the Peking University People’s Hospital in Beijing, China, for animal-induced injuries. The types of injuries vary depending on the species of the attacking animal. For instance, dogs, which are the most common culprits, can cause puncture wounds, degloving injuries, lacerations, and crushing injuries. The study also noted that large animals like horses and cattle could cause blunt force injuries through kicking, crushing, or trampling. The high incidence of dog bites underscores the need for well-designed prospective studies to better understand and manage these injuries.
3. Industrial and Home Accidents
Industrial and home accidents are another prevalent source of puncture wounds. In industrial settings, workers are often exposed to sharp tools and machinery, increasing the risk of puncture injuries. Similarly, in home environments, common household items such as knives, nails, and gardening tools can cause puncture wounds. The study from the tertiary care hospital also noted that areas with high activity involving sharp instruments, such as the emergency room and surgical intensive care unit, had higher incidences of puncture injuries. This suggests that both industrial and home environments share similar risks, emphasizing the need for safety measures and proper handling of sharp objects to prevent such injuries.
4. Sports Injuries
Sports activities can also lead to puncture wounds, particularly in contact sports or those involving sharp equipment. An epidemiologic study from Iceland found that horse-riding accidents were a leading cause of traumatic spinal cord injuries in sport and leisure activities, followed by winter sports accidents. While the study primarily focused on spinal injuries, it highlights the broader risks associated with sports, including puncture wounds from falls or collisions. The findings suggest that participants in high-risk sports should take precautions, such as wearing protective gear and receiving proper training, to minimize the risk of puncture injuries and other traumatic incidents.
Symptoms and Signs of Puncture Wounds
Symptoms and signs of puncture wounds can vary based on the severity, depth, and location of the wound, as well as whether an infection develops. Common symptoms include:
1. Pain: Immediate sharp pain at the site of the puncture, which may increase if the wound is deep or affects nerves or muscles.
2. Bleeding: Depending on the depth, there may be minimal or profuse bleeding.
3. Swelling: Swelling around the puncture site is common, especially if the wound becomes infected or involves tissue damage.
4. Redness: The skin around the puncture may become red and inflamed.
5. Tenderness: The area around the puncture is typically sensitive to touch.
6. Bruising: Discoloration around the wound can occur, especially if blood vessels are damaged.
7. Limited movement: If the puncture affects muscles, tendons, or joints, it can restrict movement.
8. Tetanus: If the puncture is caused by a rusty object, a risk of tetanus exists, with symptoms such as muscle stiffness or spasms.
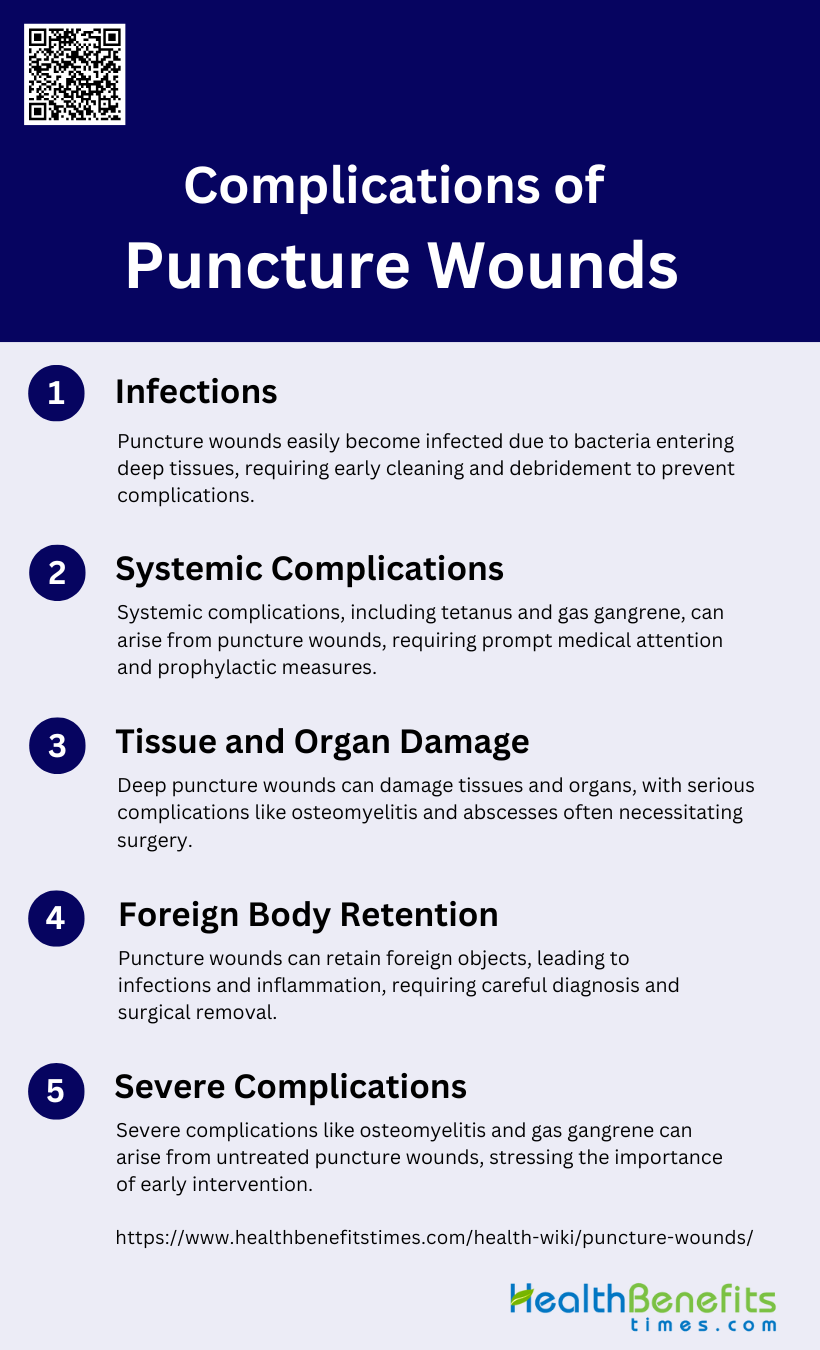
Complications of Puncture Wounds
Puncture wounds can lead to various complications if not properly treated. These complications can range from localized infections to severe systemic issues. Understanding the potential risks associated with puncture wounds is crucial for effective treatment and prevention.
1. Infections
Puncture wounds are particularly prone to infections due to the nature of the injury, which often introduces bacteria deep into the tissue. Studies have shown that up to 10% of pedal puncture wounds can become infected, with osteomyelitis caused by Pseudomonas aeruginosa being one of the most severe complications. Infections can range from superficial to deep, involving fascia and muscles, and can be caused by various organisms including Staphylococcus, Streptococcus, and anaerobes. Early and adequate primary care, including thorough cleansing and debridement, is crucial to prevent these infections. In some cases, infections can be complicated by the presence of foreign bodies, which may not be easily detected and can lead to delayed diagnosis and treatment.
2. Systemic Complications
Systemic complications from puncture wounds, although less common, can be severe and life-threatening. One of the most serious systemic infections is tetanus, which can develop following deep puncture wounds and is characterized by muscle spasms, trismus, and potentially fatal convulsions. The introduction of anaerobic bacteria in deep wounds can also lead to gas gangrene, a condition marked by intense pain, rapid pulse, and a distinct, pungent odor. Prophylactic measures such as the administration of tetanus antitoxin and early debridement are essential to prevent these severe systemic complications. Additionally, systemic signs of osteomyelitis, although rare, can occur and are often refractory to medical management alone, necessitating combined surgical and medical interventions.
3. Tissue and Organ Damage
Puncture wounds can cause significant tissue and organ damage, particularly when they penetrate deep into the body. Osteomyelitis, an infection of the bone, is a common and serious complication, especially when the wound involves cartilaginous surfaces such as the physeal plate or articular cartilage. This condition often requires extensive surgical debridement and prolonged antibiotic therapy. Soft tissue abscesses and osteochondritis are other potential complications that can arise from infected puncture wounds. The depth and location of the puncture wound play a critical role in determining the extent of tissue and organ damage, with deeper wounds posing a higher risk of severe complications.
4. Foreign Body Retention
Foreign body retention is a frequent complication of puncture wounds, particularly when the injury involves organic materials like plant thorns or rubber fragments from shoes. These foreign bodies can be challenging to detect with standard imaging techniques, leading to delayed diagnosis and treatment. Retained foreign bodies can cause persistent pain, inflammation, and infection, necessitating surgical removal for resolution. The presence of foreign bodies can also complicate the healing process and increase the risk of secondary infections, as seen in cases where rubber fragments were embedded in the foot following puncture wounds. Accurate diagnosis and timely intervention are crucial to prevent long-term complications associated with foreign body retention.
5. Severe Complications
Severe complications from puncture wounds, although rare, can have devastating consequences. One of the most severe complications is osteomyelitis, which can lead to bone destruction and require extensive surgical intervention. Gas gangrene, characterized by rapid tissue necrosis and systemic toxicity, is another life-threatening complication that can arise from deep puncture wounds contaminated with anaerobic bacteria. These severe complications underscore the importance of early and appropriate management of puncture wounds, including thorough cleansing, debridement, and prophylactic measures such as tetanus antitoxin administration. Prompt medical attention within the first 24 hours of injury is critical to prevent these severe outcomes.
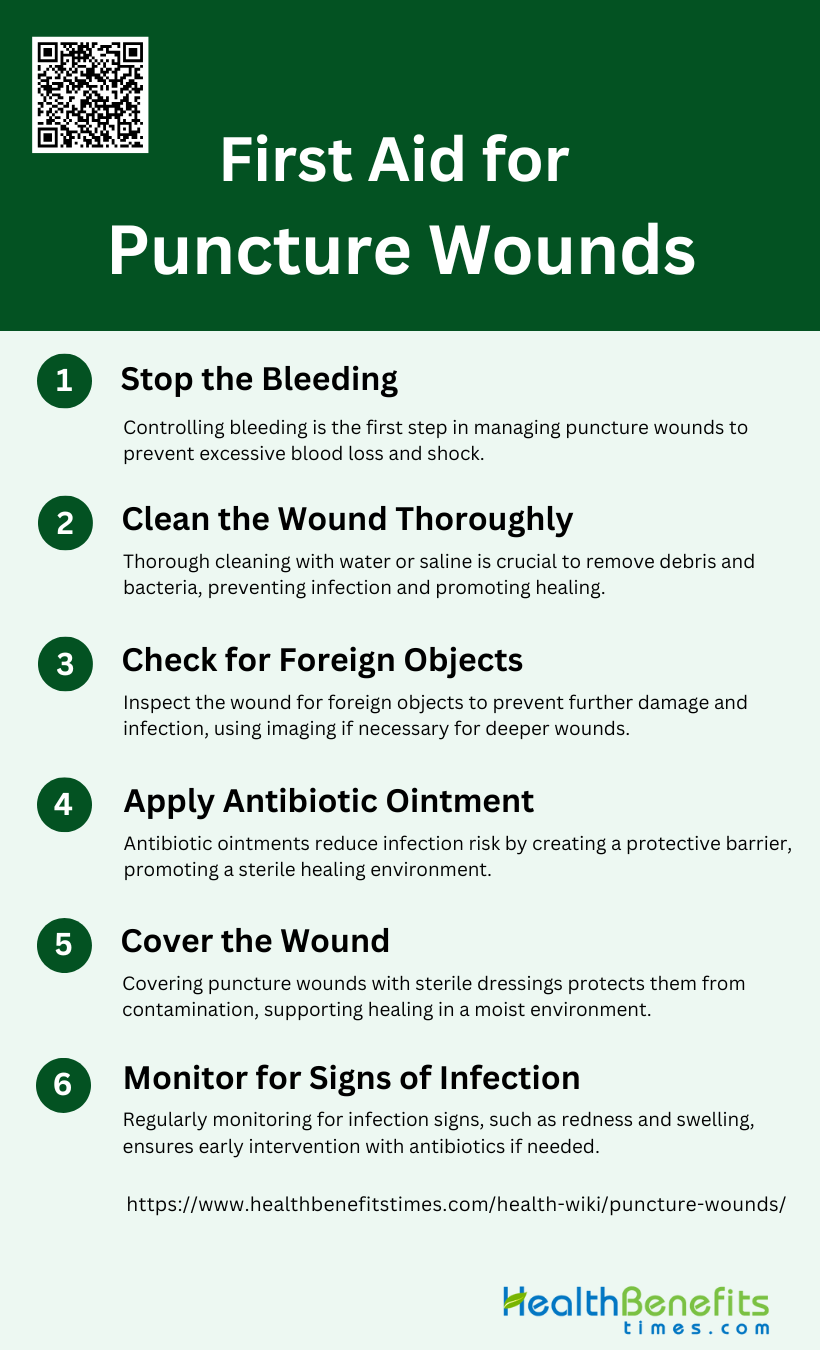
First Aid for Puncture Wounds
Puncture wounds require immediate and proper first aid to prevent complications such as infections and tissue damage. Following a systematic approach ensures the wound is treated effectively and reduces the risk of further issues. Here are the essential steps for providing first aid for puncture wounds:
1. Stop the bleeding
Stopping the bleeding is the first and most critical step in managing a puncture wound. Immediate action is necessary to prevent excessive blood loss and reduce the risk of shock. Applying direct pressure to the wound with a clean cloth or bandage can help control the bleeding. In some cases, specialized tissue adhesives with hemostatic properties, such as four-arm-PEG-CHO/PEI hydrogels, can be used to quickly stop bleeding and provide a temporary seal over the wound. These adhesives not only control hemorrhage but also offer antibacterial benefits, making them ideal for emergency care.
2. Clean the wound thoroughly
Thoroughly cleaning the wound is essential to prevent infection. This involves irrigating the wound with clean water or saline solution to remove debris and bacteria. High-pressure irrigation is often recommended to ensure that all foreign particles are flushed out. In emergency settings, using tissue adhesives with antibacterial properties can further reduce the risk of infection by providing an additional layer of protection against pathogens. Proper cleaning minimizes the chances of complications and promotes faster healing.
3. Check for foreign objects
After cleaning, it is crucial to check the wound for any foreign objects that may have been embedded during the injury. These objects can include dirt, glass, or metal fragments, which can cause further damage and increase the risk of infection if not removed. Careful inspection and, if necessary, debridement should be performed to ensure that the wound is free of any contaminants. The use of advanced imaging techniques may also be helpful in identifying deeply embedded objects that are not visible to the naked eye.
4. Apply antibiotic ointment
Applying antibiotic ointment to the wound can significantly reduce the risk of infection. Studies have shown that topical antibiotics like bacitracin zinc and neomycin sulfate are effective in lowering infection rates in soft-tissue wounds. These ointments create a protective barrier that prevents bacteria from entering the wound, thereby promoting a sterile environment conducive to healing. The use of antibiotic ointments is particularly important in puncture wounds, which are more prone to infections due to their depth and the potential for anaerobic bacterial growth.
5. Cover the wound
Covering the wound with a sterile bandage or dressing is essential to protect it from further contamination and injury. Modern first-aid supplies, such as liquid bandages and hydrogel-based adhesives, offer robust adhesive, hemostatic, and antibacterial properties, making them ideal for wound management. These advanced dressings not only keep the wound clean but also support the healing process by maintaining a moist environment, which is beneficial for tissue regeneration. Regularly changing the dressing and monitoring the wound are also important to ensure optimal healing.
6. Monitor for signs of infection
Monitoring the wound for signs of infection is a critical ongoing step in wound care. Symptoms such as increased redness, swelling, warmth, pus, and fever indicate that the wound may be infected. Early detection and prompt treatment with appropriate antibiotics can prevent the infection from spreading and causing more severe complications. In some cases, advanced tissue adhesives with antibacterial properties can provide continuous protection against infection, reducing the need for frequent dressing changes and additional interventions. Regular follow-up with a healthcare provider is recommended to ensure proper wound healing.
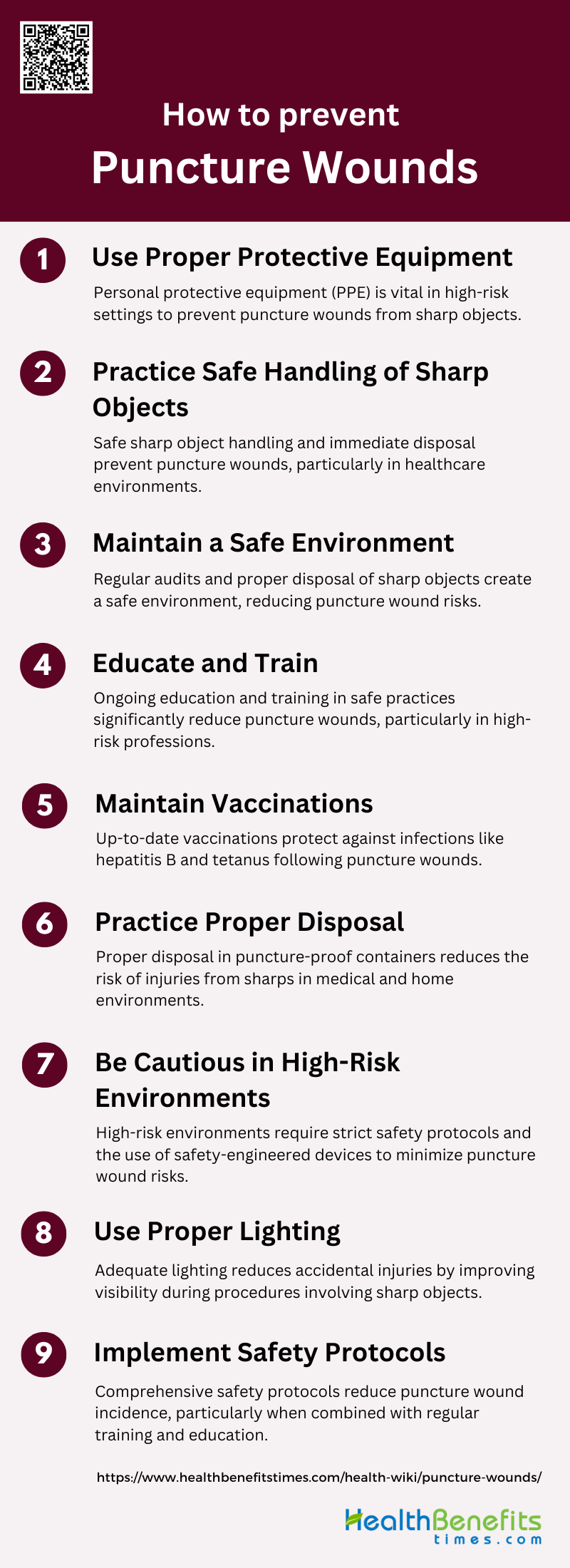
Prevent puncture wounds
Preventing puncture wounds is essential to ensure safety in both personal and professional environments. By adopting proactive measures and following best practices, the risk of such injuries can be significantly minimized. Here are key strategies to prevent puncture wounds:
1. Use Proper Protective Equipment
Using proper protective equipment (PPE) is essential in preventing puncture wounds, especially in high-risk environments such as healthcare settings. PPE includes gloves, gowns, masks, and eye protection, which act as barriers against sharp objects and potential bloodborne pathogens. Studies have shown that the use of safety-engineered devices and PPE can significantly reduce the incidence of sharps injuries among healthcare workers. Ensuring that all staff are equipped with and properly use PPE can mitigate the risks associated with handling sharp instruments, thereby enhancing overall safety and reducing the likelihood of injuries.
2. Practice Safe Handling of Sharp Objects
Safe handling of sharp objects is crucial to prevent puncture wounds. This involves using techniques such as not recapping needles, disposing of sharps immediately after use, and using tools designed to minimize direct contact with sharp edges. Training and education on the proper handling of sharps have been shown to reduce injury rates significantly. For instance, implementing safety protocols and using needle protective devices can lower the risk of injuries during procedures like blood withdrawal and intravenous insertions. Continuous education and adherence to safe handling practices are vital in maintaining a safe working environment.
3. Maintain a Safe Environment
Maintaining a safe environment involves ensuring that the workspace is free from hazards that could lead to puncture wounds. This includes proper storage and disposal of sharp objects, regular maintenance of equipment, and ensuring that safety devices are in place and functional. Studies highlight the importance of having designated sharps disposal containers and eliminating unnecessary needles to reduce the risk of injuries. Regular audits and risk assessments can help identify potential hazards and implement corrective measures to maintain a safe environment for all workers.
4. Educate and Train
Education and training are fundamental in preventing puncture wounds. Comprehensive training programs that include interactive demonstrations, educational presentations, and web-based information systems have been shown to decrease the incidence of sharps injuries. These programs should cover the proper use of PPE, safe handling and disposal of sharps, and emergency procedures in case of an injury. Continuous education ensures that all staff are aware of the latest safety protocols and are competent in implementing them, thereby reducing the risk of injuries.
5. Maintain Vaccinations
Maintaining vaccinations is a critical preventive measure against infections that can result from puncture wounds. Healthcare workers, in particular, should be vaccinated against hepatitis B and other bloodborne pathogens to reduce the risk of infection following a sharps injury. Vaccination programs should be part of the occupational health policies in healthcare settings, ensuring that all staff are immunized and protected. Regular monitoring and updating of vaccination status can further enhance the safety and well-being of workers.
6. Practice Proper Disposal
Proper disposal of sharp objects is essential to prevent puncture wounds. This involves using puncture-proof containers for disposing of needles and other sharps immediately after use. Studies have shown that compliance with proper disposal practices significantly reduces the risk of injuries. Training staff on the importance of not recapping needles and ensuring that disposal containers are readily available and correctly used can further minimize the risk of sharps injuries. Regular audits and feedback can help maintain high compliance rates with disposal protocols.
7. Be Cautious in High-Risk Environments
Being cautious in high-risk environments, such as operating rooms and laboratories, is crucial to prevent puncture wounds. These settings often involve procedures that increase the risk of sharps injuries, such as phlebotomy and suturing. Implementing strict safety protocols, using safety-engineered devices, and ensuring that all staff are trained in safe practices can significantly reduce the risk of injuries. Continuous monitoring and evaluation of safety practices in high-risk environments are essential to identify potential hazards and implement necessary improvements.
8. Use Proper Lighting
Proper lighting is an often-overlooked factor in preventing puncture wounds. Adequate lighting ensures that workers can see clearly and handle sharp objects safely, reducing the risk of accidental injuries. Poor lighting can lead to mistakes and increase the likelihood of puncture wounds, especially during intricate procedures. Ensuring that all work areas are well-lit and that lighting is regularly maintained can help prevent injuries and enhance overall safety. Proper lighting should be a standard part of workplace safety protocols.
9. Implement Safety Protocols
Implementing safety protocols is essential in preventing puncture wounds. These protocols should include guidelines for the safe handling and disposal of sharps, use of PPE, and emergency procedures in case of an injury. Studies have shown that comprehensive safety protocols, combined with regular training and education, can significantly reduce the incidence of sharps injuries. Regular reviews and updates of safety protocols ensure that they remain effective and relevant, addressing any new risks or changes in procedures. Compliance with these protocols is crucial for maintaining a safe working environment.
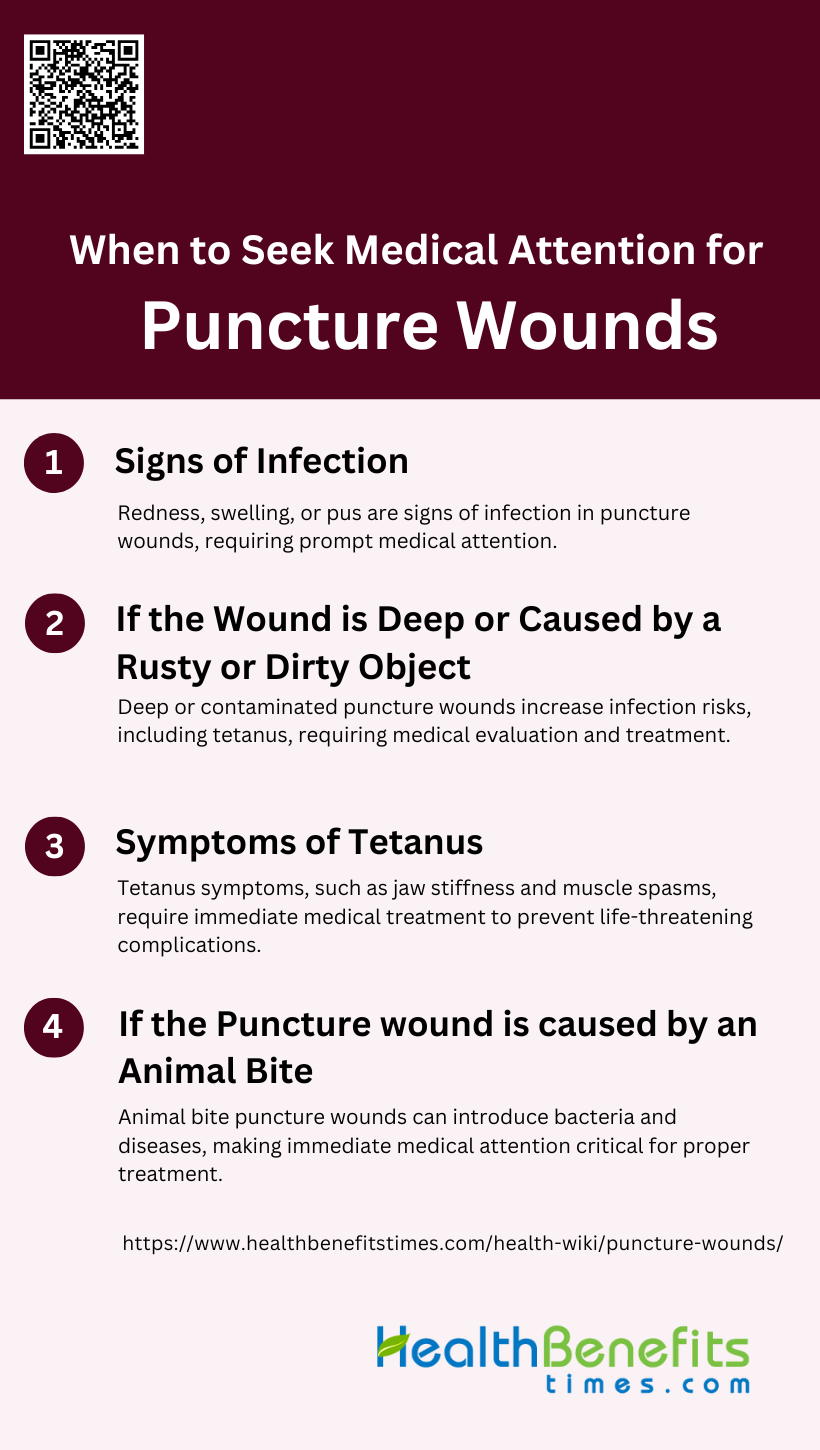
When to Seek Medical Attention for Puncture wounds
Puncture wounds can sometimes lead to serious complications that require medical attention. Recognizing the signs and knowing when to seek help can prevent further health issues. Here are key situations when you should seek medical attention for puncture wounds:
1. Signs of Infection
Puncture wounds can easily become infected due to the nature of the injury, which often drives bacteria deep into the tissue. Signs of infection include redness, swelling, and the presence of pus. These symptoms indicate that the body’s immune system is responding to a bacterial invasion. If you notice any of these signs, it is crucial to seek medical attention promptly to prevent the infection from spreading and causing more severe complications. Proper wound care and timely medical intervention can significantly reduce the risk of serious infections and promote faster healing.
2. If the Wound is Deep or Caused by a Rusty or Dirty Object
Deep puncture wounds or those caused by rusty or dirty objects pose a higher risk of infection, including tetanus. Tetanus is a serious bacterial infection caused by Clostridium tetani, which is commonly found in soil, dust, and animal feces. The bacteria can enter the body through deep wounds and produce a toxin that affects the nervous system, leading to muscle stiffness and spasms. Even if you have been vaccinated, it is essential to seek medical attention for deep or contaminated wounds to receive appropriate treatment, such as a tetanus booster or antibiotics, to prevent infection.
3. Symptoms of Tetanus
Tetanus is characterized by symptoms such as jaw stiffness (trismus) and muscle spasms, which can be life-threatening if not treated promptly. The incubation period for tetanus is typically around seven days, but symptoms can appear sooner or later depending on the severity of the wound and the bacterial load. Despite vaccination, individuals can still contract tetanus if their immunity has waned over time. Therefore, any puncture wound, especially those caused by rusty or dirty objects, should be evaluated by a healthcare professional to rule out tetanus and administer necessary treatments.
4. If the Puncture wound is caused by an Animal Bite
Animal bites are particularly concerning when it comes to puncture wounds because they can introduce a variety of bacteria into the body, leading to severe infections. In addition to common bacterial infections, animal bites can also transmit diseases such as rabies and tetanus. Immediate medical attention is crucial to clean the wound thoroughly, assess the risk of infection, and administer appropriate prophylactic treatments, including tetanus and rabies vaccinations if necessary. Early intervention can prevent complications and ensure proper healing of the wound.
FAQs
1. Can puncture wounds heal on their own without medical attention?
Puncture wounds may appear minor due to their small entry point, but because they can be deep and introduce bacteria, they have a higher risk of infection. Minor puncture wounds might heal on their own, but deeper ones or those involving dirty or rusty objects should be checked by a healthcare professional to prevent complications like tetanus or abscess formation.
2. How long does it take for a puncture wound to heal?
The healing time for a puncture wound varies depending on the depth, location, and severity. Superficial wounds may heal within a few days to a week, while deeper wounds can take several weeks to fully heal, especially if they become infected or if tissue damage occurs.
3. What should I do if a foreign object remains stuck in the wound?
If a foreign object, such as a splinter or piece of glass, remains embedded in the wound, it’s important to avoid trying to remove it yourself, especially if it’s deep. Seek medical attention to prevent further tissue damage or infection. A healthcare provider can safely remove the object and clean the wound.
4. Are puncture wounds more likely to leave a scar than other types of wounds?
Puncture wounds may leave a scar depending on their depth and how well they are treated. Proper wound care, including cleaning and covering, can help minimize scarring. Deep or infected wounds are more likely to result in visible scars.
5. Can I use home remedies to treat puncture wounds?
Home remedies like honey or aloe vera are sometimes suggested for wound healing, but for puncture wounds, medical treatment is recommended due to the risk of infection. Applying a topical antibiotic ointment and keeping the wound clean is the best approach for minor puncture wounds. Home remedies should not replace proper wound care.
6. Is it safe to cover a puncture wound, or should it be left open to air?
Covering a puncture wound with a sterile bandage or dressing helps protect it from dirt and bacteria, reducing the risk of infection. Keeping the wound moist under a bandage also promotes faster healing. Leaving a wound open to air might be necessary for some injuries, but medical guidance is recommended.
7. What happens if a puncture wound does not bleed much?
Puncture wounds may not bleed profusely because the small surface area can close quickly. However, lack of bleeding can trap bacteria inside the wound, increasing the risk of infection. Proper cleaning and attention to infection signs are important for these types of wounds.
8. Can puncture wounds cause nerve damage?
Yes, depending on the depth and location, puncture wounds can damage nerves, especially if they occur in areas with dense nerve distribution, like the hands or feet. If you experience numbness, tingling, or loss of function after a puncture wound, medical evaluation is necessary.
9. How can I tell if my puncture wound is healing properly?
A puncture wound that is healing properly will gradually decrease in pain, swelling, and redness. Any signs of increasing discomfort, heat, pus, or foul odor may indicate infection and should be checked by a healthcare professional. Monitoring the wound daily for changes is important.
10. Do I need a tetanus shot if my puncture wound isn’t deep?
Even shallow puncture wounds caused by dirty or rusty objects, such as nails or animal bites, can pose a risk of tetanus. If you haven’t had a tetanus booster within the past 10 years, or if you’re unsure, it’s best to consult a healthcare provider to determine if a booster is needed.