The Achilles tendon is the strongest and thickest tendon in the human body, connecting the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). It plays a crucial role in walking, running, and jumping by facilitating plantar flexion of the foot. Despite its strength, the Achilles tendon is prone to injuries, particularly in athletes, due to the high loads it endures, which can be up to 12.5 times body weight during activities like running. The tendon is susceptible to overuse injuries, tendinopathy, and ruptures, often resulting from repetitive strain and degenerative changes. The blood supply to the tendon is relatively limited, especially in the mid-portion, making it a common site for problems. Treatment of Achilles tendon injuries varies from conservative management to surgical intervention, depending on the severity and type of injury.
Anatomy of the Achilles Tendon
The Achilles tendon is a vital part of the musculoskeletal system, essential for mobility and athletic performance. It connects the calf muscles to the heel bone, facilitating movements such as walking and jumping. Below, we explore its anatomy, focusing on its location, structure, and role.
1. Location
The Achilles tendon is located in the posterior, superficial compartment of the calf, connecting the calf muscles to the heel bone. Specifically, it is the conjoined tendon of the gastrocnemius and soleus muscles, and it may also have a small contribution from the plantaris muscle. This tendon inserts on the calcaneus, or heel bone, making it a crucial structure for the movement of the foot and ankle. The Achilles tendon is subjected to the highest loads in the body, with tensile forces reaching up to ten times body weight during activities such as running and jumping.
2. Structure
The Achilles tendon is composed primarily of collagen fibers, which are designed to provide both strength and flexibility. The tendon is the strongest and thickest in the human body, and its fibers originate from the soleus muscle and the medial and lateral heads of the gastrocnemius muscle. These fibers twist around each other as they descend toward the insertion point at the calcaneus. The tendon also has a specialized calcaneal insertion that aids in stress dissipation. The blood supply to the tendon comes from the musculotendinous junction, surrounding connective tissue, and the osteotendinous junction, with a relatively hypovascular area in the mid-portion where most problems occur.
3. Role
The Achilles tendon plays a vital role in enabling walking, running, and jumping by allowing the foot to point downward, a movement known as plantar flexion. It serves as the main plantar flexor of the ankle, absorbing the load of the body’s weight and flexing the ankle joint to propel the body forward. This function is crucial for normal calf muscle activity and overall mobility. The tendon is subjected to repetitive strain from activities such as running, jumping, and sudden acceleration or deceleration, making it susceptible to injuries and degenerative changes.
Function and Importance of Achilles Tendon
The Achilles tendon is a fundamental component of the musculoskeletal system, essential for movement and stability. It facilitates various functions, from powering locomotion to absorbing shock. Below, we delve into its functions and importance, detailing its role in human biomechanics.
1. Powering Movement
The Achilles tendon plays a crucial role in powering movement by acting as a conduit for force generated by the calf muscles. It connects the gastrocnemius and soleus muscles to the calcaneus (heel bone), enabling plantar flexion of the foot, which is essential for activities such as walking, running, and jumping. The tendon stores elastic energy during the stance phase of gait and releases it during push-off, thereby amplifying muscle power and contributing to efficient movement. This energy storage and release mechanism reduces the metabolic cost of locomotion, allowing for sustained and powerful movements.
2. Force Transmission
The primary function of the Achilles tendon is to transmit forces from the calf muscles to the foot, facilitating movement. It is composed of dense, regularly arranged collagen fibers that provide the tensile strength necessary to withstand high loads, sometimes up to ten times body weight during activities like running and jumping. This force transmission is critical for effective locomotion, as it allows the muscles to generate the necessary power to propel the body forward. The tendon’s viscoelastic properties also enable it to absorb and release energy efficiently, further enhancing its role in force transmission.
3. Shock Absorption
The Achilles tendon also serves as a shock absorber, protecting muscles and bones from the impact forces generated during activities such as running and jumping. Its viscoelastic nature allows it to dampen mechanical oscillations and reduce the risk of muscle injuries by absorbing and dissipating energy. This shock-absorbing capability is crucial for minimizing the stress on the musculoskeletal system, thereby preventing overuse injuries and enhancing overall movement efficiency. The tendon’s ability to store and release elastic energy also contributes to its shock-absorbing function, making it a vital component in the biomechanics of movement.
4. Balance and Stability
The Achilles tendon contributes significantly to balance and stability by providing proprioceptive feedback and maintaining the alignment of the foot and ankle. Its connection to the calf muscles allows for fine-tuned adjustments in muscle tension, which are essential for maintaining posture and stability during dynamic activities. The tendon’s ability to transmit forces efficiently also aids in stabilizing the ankle joint, reducing the likelihood of falls and enhancing overall balance. This function is particularly important in activities that require rapid changes in direction or uneven terrain, where stability is crucial.
5. Biomechanics
The biomechanics of the Achilles tendon are complex and involve various factors such as tendon twisting, intratendinous interactions, and differential muscle forces. These factors contribute to the nonuniform displacement patterns observed in the tendon during movement. The tendon’s ability to store and release elastic energy efficiently is a key biomechanical feature that enhances movement performance and reduces energy expenditure. Understanding these biomechanical properties is essential for developing effective rehabilitation strategies and improving athletic performance.
6. Locomotion
The Achilles tendon is integral to human locomotion, providing the necessary force and flexibility for efficient movement. Its ability to store and release elastic energy reduces the metabolic cost of walking and running, allowing humans to move at faster speeds for longer durations. The tendon’s role in force transmission and shock absorption also enhances locomotor efficiency, making it a critical component in activities that involve repetitive motion. The evolutionary significance of the Achilles tendon in bipedalism underscores its importance in human locomotion.
7. Anatomical Significance
Anatomically, the Achilles tendon is the strongest and thickest tendon in the human body, connecting the gastrocnemius and soleus muscles to the calcaneus. Its unique structure, including the spiralization of fibers and specialized calcaneal insertion, provides mechanical advantages and aids in stress dissipation. The tendon’s blood supply and innervation are also specialized, with a relatively hypovascular midsection that is prone to injury. Understanding the anatomical features of the Achilles tendon is crucial for diagnosing and treating tendon-related injuries and conditions.
Common Injuries and Disorders of Achilles tendon
The Achilles tendon is susceptible to various injuries and disorders due to its pivotal role in movement and weight-bearing activities. Understanding these common issues is essential for prevention and effective treatment. Below is a list of common injuries and disorders associated with the Achilles tendon.
1. Tendinopathy
Achilles tendinopathy is a prevalent overuse injury characterized by pain, swelling, and impaired function of the Achilles tendon. It is commonly seen in athletes and individuals who engage in repetitive activities such as running and jumping. The etiology of tendinopathy is multifactorial, involving mechanical overload, degenerative changes, and possibly genetic predispositions. Histopathologic studies have shown that tendinopathy often precedes tendon ruptures, indicating degenerative changes within the tendon tissue.
2. Paratenonitis
Paratenonitis refers to the inflammation of the paratenon, the sheath surrounding the Achilles tendon. This condition is often associated with overuse and repetitive strain, leading to pain and swelling in the posterior aspect of the ankle. It is commonly seen in athletes, particularly runners, and can occur in conjunction with other Achilles tendon disorders such as tendinosis and bursitis. Treatment typically involves rest, anti-inflammatory medications, and physical therapy.
3. Insertional Tendinitis
Insertional tendinitis affects the point where the Achilles tendon attaches to the calcaneus (heel bone). This condition is characterized by pain and swelling at the insertion site and is often associated with calcific deposits and bone spurs. It is commonly seen in older athletes and those with a history of chronic overuse. Treatment options include rest, physical therapy, and in severe cases, surgical intervention to remove calcific deposits and repair the tendon.
4. Retrocalcaneal Bursitis
Retrocalcaneal bursitis is the inflammation of the bursa located between the Achilles tendon and the calcaneus. This condition often coexists with other Achilles tendon disorders and is characterized by pain and swelling at the back of the heel. It is commonly caused by repetitive stress and friction from activities such as running and jumping. Treatment includes rest, anti-inflammatory medications, and modifications in footwear to reduce pressure on the affected area .
5. Complete Rupture
A complete rupture of the Achilles tendon is a severe injury that typically occurs during activities requiring sudden acceleration or deceleration, such as jumping or sprinting. This injury is characterized by a sudden, sharp pain in the back of the ankle, often accompanied by an audible pop. Complete ruptures are more common in middle-aged athletes and those with pre-existing degenerative changes in the tendon. Surgical repair is generally recommended for active individuals to restore function and minimize the risk of re-rupture.
6. Partial Rupture
Partial ruptures of the Achilles tendon involve a tear that does not extend through the entire thickness of the tendon. These injuries are often the result of chronic overuse and degenerative changes within the tendon. Symptoms include pain, swelling, and weakness in the affected area. Conservative treatment, including rest, physical therapy, and bracing, is typically effective, although surgical intervention may be necessary for chronic or severe cases.
7. Pediatric Achilles Tendon Injuries
Achilles tendon injuries are less common in the pediatric population compared to adults. When they do occur, they are often the result of traumatic events such as penetrating or blunt trauma. Older adolescents are more likely to experience ruptures due to forceful muscular contractions. Treatment usually involves surgical repair, followed by immobilization and rehabilitation. Most pediatric patients return to normal activities within six months post-injury.
8. Degenerative Changes
Degenerative changes in the Achilles tendon are often observed in individuals with chronic overuse injuries. These changes include collagen disorganization, increased vascularity, and the presence of microtears. Degenerative changes can predispose the tendon to partial or complete ruptures and are commonly seen in older athletes and those with a history of repetitive strain. Management includes conservative treatments such as physical therapy and, in some cases, surgical intervention to debride the degenerated tissue.
9. Myotendineal Junction Pain
Pain at the myotendineal junction, where the muscle transitions to tendon, is another common issue associated with Achilles tendon disorders. This condition is often seen in athletes and is typically the result of overuse and repetitive strain. Conservative treatment, including rest, physical therapy, and anti-inflammatory medications, is usually effective in managing symptoms.
10. Surgical Interventions
Surgical interventions for Achilles tendon disorders are considered when conservative treatments fail. Procedures may include debridement of diseased tissue, direct tendon repair, and tendon transfer to augment strength. Surgical outcomes are generally favorable, particularly for complete ruptures in active individuals, with most patients returning to pre-injury activity levels.
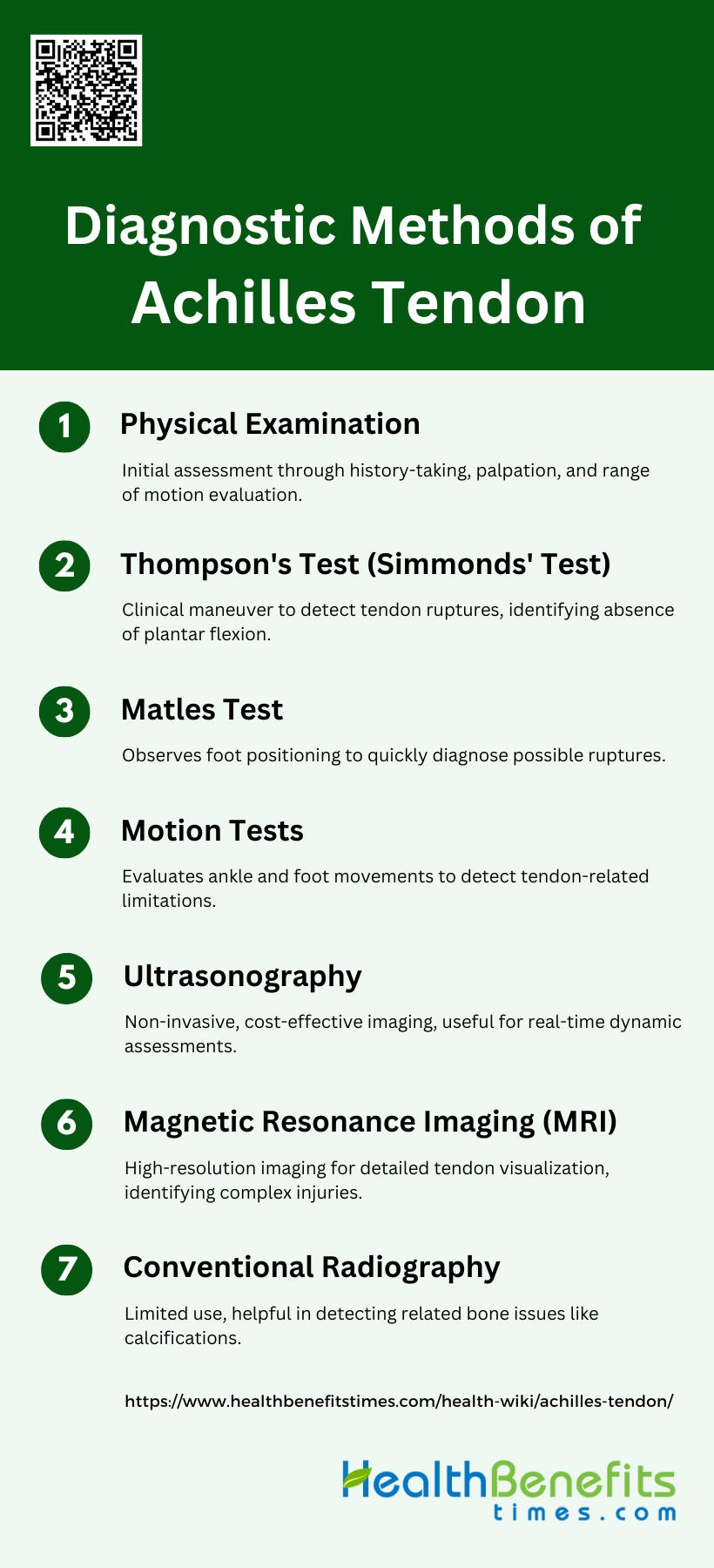
Diagnostic Methods of Achilles tendon
Diagnosing Achilles tendon injuries requires a combination of clinical assessments and imaging techniques to ensure accurate identification and effective treatment. These methods help in evaluating the extent of injury, determining the appropriate intervention, and monitoring recovery progress. Below are the key diagnostic methods used for assessing the Achilles tendon.
1. Physical Examination
Physical examination is a fundamental step in diagnosing Achilles tendon injuries. It involves a thorough assessment of the patient’s medical history, symptoms, and physical condition. Clinicians typically look for signs such as swelling, tenderness, and a palpable gap in the tendon, which may indicate a rupture. The examination also includes evaluating the range of motion and strength of the affected ankle. Physical examination is crucial as it provides immediate insights and helps guide further diagnostic testing if necessary.
2. Thompson’s Test (Simmonds’ Test)
The Thompson’s Test, also known as the Simmonds’ Test, is a widely used clinical maneuver to diagnose Achilles tendon ruptures. During the test, the patient lies prone with feet hanging off the edge of the examination table. The examiner squeezes the calf muscle, and a normal response would be plantar flexion of the foot. Absence of this movement suggests a rupture of the Achilles tendon. This test is valued for its simplicity and effectiveness in a clinical setting.
3. Matles Test
The Matles Test is another clinical test used to diagnose Achilles tendon ruptures. In this test, the patient lies prone and is asked to flex their knees to 90 degrees. The examiner observes the position of the feet; a foot that remains in a neutral or dorsiflexed position indicates a possible rupture. This test is useful as it can be performed quickly and does not require any special equipment, making it a practical choice in various clinical settings.
4. Motion Tests
Motion tests involve assessing the range of motion and functional capabilities of the ankle and foot. These tests help in identifying limitations in movement that may be caused by Achilles tendon injuries. Clinicians may ask patients to perform specific movements such as dorsiflexion, plantarflexion, and heel raises. Observing the patient’s ability to perform these movements can provide valuable information about the extent and nature of the injury.
5. Ultrasonography
Ultrasonography is a non-invasive imaging technique that uses high-frequency sound waves to create images of the Achilles tendon. It is highly effective in diagnosing tendon pathologies such as tendinopathy, partial tears, and complete ruptures. Ultrasonography is preferred for its accessibility, cost-effectiveness, and ability to provide real-time dynamic assessment. Studies have shown that it has high sensitivity and specificity in detecting Achilles tendon abnormalities.
6. Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is considered the gold standard for detailed visualization of the Achilles tendon. It provides high-resolution images that can reveal the extent of tendon damage, including partial and complete tears, tendinopathy, and other degenerative changes. MRI is particularly useful in complex cases where other imaging modalities may not provide sufficient detail. However, it is more expensive and less accessible than ultrasonography.
7. Conventional Radiography
Conventional radiography, or X-ray imaging, is less commonly used for diagnosing Achilles tendon injuries as it primarily visualizes bone structures rather than soft tissues. However, it can be useful in identifying associated conditions such as calcifications, bone spurs, or avulsion fractures that may accompany tendon injuries. While not the primary diagnostic tool for tendon pathologies, it can provide supplementary information that aids in the overall assessment.
Treatment Options of Achilles tendon
Achilles tendon injuries require a tailored approach to treatment, depending on the severity and nature of the condition. Both non-surgical and surgical options are available, each with specific benefits and considerations. Below are the primary treatment methods used to address Achilles tendon issues.
A. Non-surgical treatments
1. Rest, ice, compression, and elevation (RICE): RICE is a common initial treatment for Achilles tendon injuries to reduce pain and swelling. It is often used in conjunction with other conservative treatments to manage symptoms and promote healing.
2. Physical therapy and exercises: Physical therapy, including eccentric strengthening exercises, is highly effective in improving pain and function in chronic Achilles tendinopathy. Early mobilization and weight-bearing exercises post-injury can lead to better outcomes and faster return to activities.
3. Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for pain relief, although their long-term effectiveness is limited. Corticosteroid injections may provide temporary pain relief but are generally not recommended for long-term management.
B. Surgical interventions
1. Open surgery to repair the tendon: Open surgical repair significantly reduces the risk of rerupture compared to nonoperative treatments but is associated with higher risks of complications such as infections and adhesions. It is generally reserved for severe cases or when conservative treatments fail.
2. Minimally invasive procedures: Minimally invasive techniques, including percutaneous repair, offer comparable functional outcomes to open surgery with fewer complications. These techniques are increasingly preferred due to their lower risk of soft tissue complications and faster recovery times.
C. Other Methods
1. Taping: Taping can provide support and reduce strain on the Achilles tendon during the healing process. It is often used as an adjunct to other treatments to enhance stability and reduce pain.
2. Night splints: Night splints help maintain the Achilles tendon in a stretched position overnight, which can reduce morning stiffness and pain. They are particularly useful in managing chronic tendinopathy.
3. Ultrasound therapy: Therapeutic ultrasound is used to promote tissue healing and reduce pain. It is considered a reasonable second-line treatment for patients who do not respond to initial conservative therapies.
4. Shockwave therapy: Extracorporeal shockwave therapy (ESWT) has shown promise in treating chronic Achilles tendinopathy by promoting tissue regeneration and reducing pain. It is a non-invasive option that can be considered before surgical intervention.
5. Rehabilitation: A structured rehabilitation program, including early mobilization and weight-bearing exercises, is crucial for recovery post-surgery or injury. Accelerated rehabilitation protocols have been shown to improve patient satisfaction and functional outcomes without increasing the risk of rerupture.
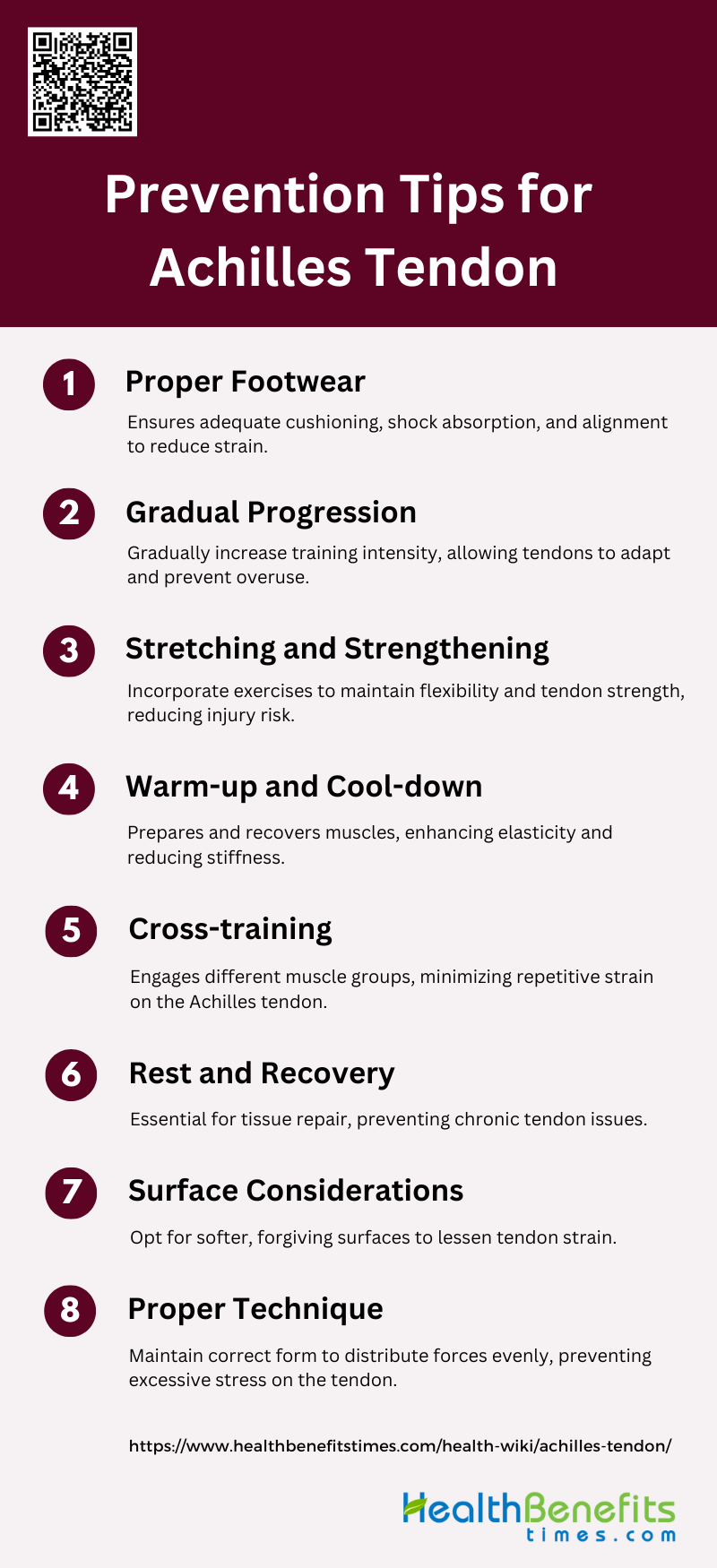
Prevention Tips for Achilles tendon
Preventing Achilles tendon injuries involves adopting proactive measures to maintain tendon health and flexibility. By incorporating specific exercises, proper footwear, and mindful activity adjustments, individuals can significantly reduce the risk of injury. Below are key prevention tips for Achilles tendon:
1. Proper Footwear
Wearing appropriate footwear is crucial in preventing Achilles tendon injuries. Shoes with adequate cushioning and arch support can help absorb shock and reduce the strain on the Achilles tendon. Shock-absorbing insoles have been shown to have a preventive effect on Achilles tendinopathy, particularly in active individuals. Proper footwear can also help maintain proper alignment and biomechanics during physical activities, reducing the risk of overuse injuries. Ensuring that shoes are well-fitted and replaced regularly can further contribute to the prevention of Achilles tendon issues.
2. Gradual Progression
Gradual progression in training intensity and volume is essential to prevent Achilles tendon injuries. Sudden increases in activity levels can overload the tendon, leading to microtears and inflammation. A systematic approach to increasing exercise intensity allows the tendon to adapt and strengthen over time, reducing the risk of injury. This method is particularly important for athletes and individuals returning to physical activity after a period of inactivity. Monitoring and adjusting training loads based on individual responses can help in maintaining tendon health and preventing overuse injuries.
3. Stretching and Strengthening
Stretching and strengthening exercises are commonly recommended for Achilles tendon health, although their effectiveness is debated. Some studies suggest that stretching may not significantly impact injury prevention, while others highlight potential benefits such as increased tendon tensile strength and load-induced hypertrophy. Strengthening exercises, particularly eccentric training, have shown promise in improving tendon resilience and reducing injury risk. A balanced approach that includes both stretching and strengthening can help maintain tendon flexibility and strength, potentially preventing injuries.
4. Warm-up and Cool-down
Incorporating proper warm-up and cool-down routines is vital for Achilles tendon injury prevention. Warm-up exercises increase blood flow and muscle temperature, enhancing tendon elasticity and reducing stiffness. This preparation can help prevent sudden stress on the tendon during physical activity. Similarly, cool-down exercises aid in gradually reducing the heart rate and muscle temperature, promoting recovery and reducing muscle soreness. Both warm-up and cool-down routines should be tailored to the individual’s activity level and specific needs to maximize their preventive benefits.
5. Cross-training
Cross-training involves incorporating a variety of exercises and activities into a training regimen to prevent overuse injuries like Achilles tendinopathy. By varying the types of physical activities, different muscle groups are engaged, reducing repetitive strain on the Achilles tendon. Activities such as swimming, cycling, and strength training can complement running or jumping exercises, providing a balanced workout that promotes overall fitness while minimizing the risk of tendon overuse. Cross-training also helps in maintaining cardiovascular fitness and muscle strength, contributing to overall injury prevention.
6. Rest and Recovery
Adequate rest and recovery are essential components of Achilles tendon injury prevention. Allowing sufficient time for the tendon to recover between training sessions helps prevent overuse injuries and promotes tissue repair. Incorporating rest days and ensuring proper sleep can enhance recovery and reduce the risk of chronic tendon issues. Monitoring for signs of overtraining, such as persistent pain or fatigue, and adjusting training schedules accordingly can further support tendon health and prevent injuries.
7. Surface Considerations
The type of surface on which physical activities are performed can significantly impact the risk of Achilles tendon injuries. Hard, uneven, or slippery surfaces can increase the strain on the tendon, leading to a higher risk of injury. Opting for softer, more forgiving surfaces, such as grass or synthetic tracks, can help reduce the impact forces transmitted to the Achilles tendon. Additionally, being mindful of surface conditions and avoiding activities on hazardous terrains can further contribute to injury prevention.
8. Proper Technique
Using proper technique during physical activities is crucial for preventing Achilles tendon injuries. Incorrect form or biomechanics can place excessive stress on the tendon, increasing the risk of injury. Ensuring that movements are performed correctly, whether in running, jumping, or strength training, can help distribute forces more evenly and reduce strain on the Achilles tendon. Seeking guidance from coaches or trainers to learn and maintain proper technique can be beneficial in preventing tendon injuries and promoting overall musculoskeletal health.
Recovery and Rehabilitation for Achilles Tendon
Rehabilitation Process
The rehabilitation process for Achilles tendon injuries involves a structured physical therapy regimen aimed at reducing pain and swelling, restoring ankle motion, and strengthening the tendon and surrounding muscles. Early functional rehabilitation, which includes immediate weightbearing and controlled ankle mobilization, has been shown to significantly improve patient satisfaction and expedite the return to pre-injury activities. This approach typically involves a combination of weightbearing exercises, range of motion activities, and isometric strengthening exercises initiated within the first two weeks post-injury. Studies have demonstrated that early mobilization and weightbearing can lead to better functional outcomes, including increased calf muscle strength and reduced tendon elongation.
Timeline for Recovery
The timeline for recovery from Achilles tendon injuries varies depending on the severity of the injury and the rehabilitation protocol followed. Generally, the recovery period can extend up to 12 months for full functional recovery. Early weightbearing and mobilization protocols have been shown to shorten the time to return to work and sports significantly, with many patients beginning controlled ankle mobilization by the second postoperative week. However, tendon elongation and muscle strength may continue to improve for up to six months post-surgery, indicating that a prolonged rehabilitation period is necessary for optimal recovery. The variability in rehabilitation protocols highlights the need for individualized treatment plans based on the patient’s specific condition and response to therapy.
Returning to Activity
Guidelines for returning to normal activities or sports after an Achilles tendon injury emphasize a gradual and controlled approach to prevent re-injury. Early functional rehabilitation, which includes early weightbearing and ankle mobilization, has been associated with a quicker return to pre-injury activities. Physical therapists play a crucial role in monitoring the patient’s progress and adjusting the rehabilitation protocol based on clinical findings. Typically, patients can begin light activities and exercises within the first few weeks post-injury, with a gradual increase in intensity and complexity over several months. Full return to high-impact sports or strenuous activities is generally recommended only after achieving near-normal strength and range of motion, which can take up to a year.
FAQs
1. Can I prevent Achilles tendon injuries through diet and nutrition?
Yes, maintaining a healthy diet rich in collagen, vitamin C, and other essential nutrients that support tendon health can potentially help prevent Achilles tendon injuries. Staying hydrated and avoiding excessive intake of inflammatory foods may also contribute to tendon health.
2. Are Achilles tendon injuries more common in men or women?
Achilles tendon injuries are more common in men, particularly in middle-aged athletes. Hormonal differences and activity levels may play a role in this disparity.
3. How does aging affect the Achilles tendon?
As people age, the Achilles tendon becomes less flexible and more prone to degeneration, leading to a higher risk of tendinopathy or rupture, especially in individuals who remain active.
4. Can Achilles tendon issues be hereditary?
While there is no direct evidence that Achilles tendon injuries are hereditary, factors such as the shape of the foot, gait, and tendon structure, which can influence injury risk, may have genetic components.
5. Can I still exercise with an Achilles tendon injury? Depending on the severity of the injury, low-impact exercises such as swimming or cycling may be possible. Always consult a medical professional to determine appropriate activities during recovery.
6. Are custom orthotics helpful for Achilles tendon issues?
Yes, custom orthotics can help manage Achilles tendon problems by providing proper foot alignment and reducing stress on the tendon during movement.
7. What is the difference between Achilles tendinitis and tendinopathy?
Achilles tendinitis refers to the inflammation of the tendon, usually due to acute overuse. Tendinopathy, on the other hand, refers to a more chronic condition characterized by degeneration of the tendon fibers.
8. How do footwear choices impact Achilles tendon health?
Wearing shoes with insufficient support or heels that place excessive strain on the Achilles tendon can increase the risk of injury. Shoes with proper cushioning and arch support are recommended to protect the tendon.
9. Can Achilles tendon injuries be linked to other medical conditions?
Certain conditions, such as rheumatoid arthritis or diabetes, can increase the risk of developing Achilles tendon issues due to systemic inflammation or poor blood flow to the tendons.
10. Can Achilles tendon injuries reoccur after recovery?
Yes, there is a risk of re-injury if rehabilitation is not properly followed, or if the tendon does not fully heal. Strengthening exercises, proper footwear, and gradual return to activity can help prevent recurrence.