Actigraphy is a non-invasive method used to monitor and assess human rest and activity cycles over extended periods. It typically involves the use of a small, wearable device called an actigraph, which is usually worn on the wrist like a watch. This device continuously records movement data, providing valuable insights into sleep patterns, physical activity levels, and circadian rhythms. Actigraphy is widely used in sleep research and clinical settings to evaluate sleep disorders, assess treatment efficacy, and study various health conditions, including anxiety disorders and cardiovascular health. The data collected through actigraphy can help healthcare professionals and researchers analyze sleep duration, timing, efficiency, and irregularity, offering a more objective and comprehensive understanding of an individual’s sleep-wake patterns compared to self-reported measures.
How Does Actigraphy Work?
Actigraphy works by using miniature motion sensors, typically accelerometers, to measure and record movement data, which is then used to infer various physiological states such as sleep and wakefulness. These devices, often worn on the wrist, detect gross and fine movements and convert them into digital signals through low pass filtering and quantization techniques. The accelerometers in actigraphy devices are capable of capturing a wide range of motion, from large movements to subtle biovibrations like heart rate and breathing. The collected data is processed using specialized software that applies algorithms to estimate sleep parameters and other activity metrics. This data is then interpreted to provide insights into sleep patterns, circadian rhythms, and even cognitive performance. Advanced signal processing techniques and machine learning approaches can further enhance the accuracy of pattern recognition and data interpretation, making actigraphy a valuable tool in both clinical and research settings.
Actigraphy vs. Polysomnography
Differences in Technology and Purpose
Actigraphy and polysomnography (PSG) are both used to study sleep, but they differ significantly in technology and purpose. Actigraphy involves wearing a wristwatch-like device that measures movement to infer sleep patterns over extended periods, making it suitable for long-term monitoring in natural settings. In contrast, PSG is a comprehensive method that records multiple physiological parameters, including brain waves (EEG), eye movements (EOG), and muscle activity (EMG), to provide detailed information about sleep stages and disorders in a controlled environment. While PSG is considered the gold standard for diagnosing sleep disorders, actigraphy is more practical for assessing sleep variability and circadian rhythms.
Pros and Cons of Each Method
Actigraphy is less expensive, less cumbersome, and allows for continuous monitoring over long periods, making it ideal for studying sleep patterns in everyday settings. However, it is less accurate than PSG, particularly in detecting wakefulness and specific sleep stages. Polysomnography, on the other hand, provides detailed and accurate data on sleep architecture and is essential for diagnosing complex sleep disorders like sleep apnea and periodic limb movement disorder. The main drawbacks of PSG are its high cost, complexity, and the need for a controlled laboratory environment, which can disrupt natural sleep patterns.
When to Choose Actigraphy over Other Methods
Actigraphy is particularly useful when long-term monitoring of sleep patterns is required, such as in the assessment of circadian rhythm disorders, insomnia, and the effectiveness of sleep treatments. It is also beneficial for populations less likely to tolerate PSG, such as infants, elderly patients with dementia, and individuals with chronic insomnia. Actigraphy is recommended for evaluating sleep variability and treatment effects in natural settings, where the convenience and cost-effectiveness of the method outweigh the need for the detailed data provided by PSG.
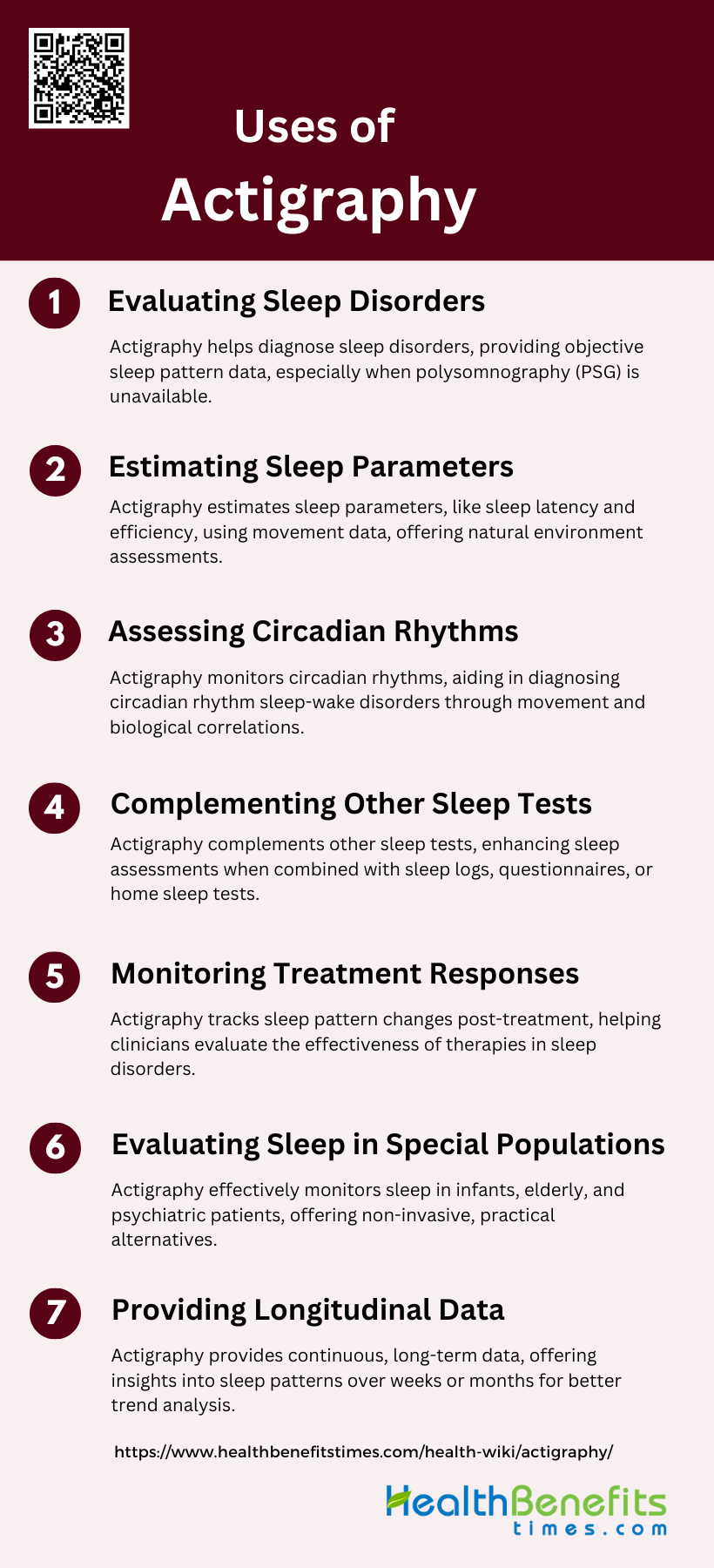
Uses of Actigraphy
Actigraphy is a valuable tool in sleep medicine, providing insights into sleep patterns and circadian rhythms through non-invasive monitoring. It is widely used in both clinical and research settings to enhance the understanding and management of sleep-related conditions. Below are several key applications of actigraphy.
1. Evaluating Sleep Disorders
Actigraphy is a valuable tool in the evaluation of various sleep disorders. It is particularly useful for diagnosing conditions such as advanced sleep phase syndrome (ASPS), delayed sleep phase syndrome (DSPS), and shift work disorder. Actigraphy provides an objective measure of sleep patterns and can be used when polysomnography (PSG) is not available, offering an estimate of total sleep time in patients with obstructive sleep apnea. Additionally, it is effective in assessing sleep variability in patients with insomnia, providing insights into night-to-night variations in sleep patterns. This makes actigraphy a practical alternative to more invasive and expensive diagnostic methods.
2. Estimating Sleep Parameters
Actigraphy is widely used to estimate various sleep parameters, including sleep latency, total sleep time, sleep efficiency, and daytime napping. By continuously recording movement data, actigraphy can infer sleep/wake cycles, making it a reliable method for assessing sleep in natural settings. The data collected can be analyzed using specialized software to derive a range of sleep parameters, which are crucial for understanding sleep patterns and diagnosing sleep disorders. Despite its limitations compared to PSG, actigraphy provides consistent and objective data that are often unique from patient-reported sleep logs.
3. Assessing Circadian Rhythms
Actigraphy is particularly effective in assessing circadian rhythms, making it a valuable tool for diagnosing circadian rhythm sleep-wake disorders. It can identify rhythms by correlating actigraphic recordings with measurements of melatonin and core body temperature rhythms. This capability is especially useful for diagnosing conditions such as delayed or advanced sleep phase syndrome, non-24-hour sleep-wake syndrome, and evaluating sleep disturbances in shift workers. Actigraphy provides a non-invasive and cost-effective method for monitoring circadian patterns, which is essential for both clinical and research applications.
4. Complementing Other Sleep Tests
While actigraphy is not as comprehensive as polysomnography, it serves as a valuable complement to other sleep tests. It can be integrated with home sleep apnea test devices to estimate total sleep time during recording, especially when other objective measurements are not available. Actigraphy is also useful in conjunction with sleep logs and questionnaires, providing a more complete picture of a patient’s sleep patterns and aiding in the diagnosis and management of sleep disorders. This complementary role enhances the overall accuracy and reliability of sleep assessments.
5. Monitoring Treatment Responses
Actigraphy is an effective tool for monitoring treatment responses in patients with sleep disorders. It can objectively measure changes in sleep patterns and circadian rhythms following interventions such as pharmacological treatments, light therapy, or continuous positive airway pressure (CPAP) therapy. By providing continuous data over extended periods, actigraphy allows clinicians to assess the stability and effectiveness of treatments, making it a valuable outcome measure in both clinical and research settings. This capability is particularly beneficial for evaluating the impact of treatments on sleep quality and overall health.
6. Evaluating Sleep in Special Populations
Actigraphy is especially useful for evaluating sleep in special populations, such as infants, children, older adults, and individuals with psychiatric disorders. In these groups, traditional sleep monitoring methods can be challenging, making actigraphy a practical alternative. For example, in patients with schizophrenia, actigraphy provides an objective measure of sleep patterns, circumventing the issues of unreliable self-reporting. Similarly, in older adults and pediatric populations, actigraphy helps delineate sleep patterns and document treatment responses, offering valuable insights into sleep health in these vulnerable groups.
7. Providing Longitudinal Data
One of the significant advantages of actigraphy is its ability to provide longitudinal data on sleep patterns and circadian rhythms. By continuously recording movement over extended periods, actigraphy offers a comprehensive view of sleep behavior, which is essential for understanding long-term trends and variations. This longitudinal data is invaluable for both clinical management and research, allowing for the assessment of chronic sleep issues and the long-term effects of treatments. The ability to monitor sleep over days, weeks, or even months makes actigraphy a powerful tool in sleep medicine.
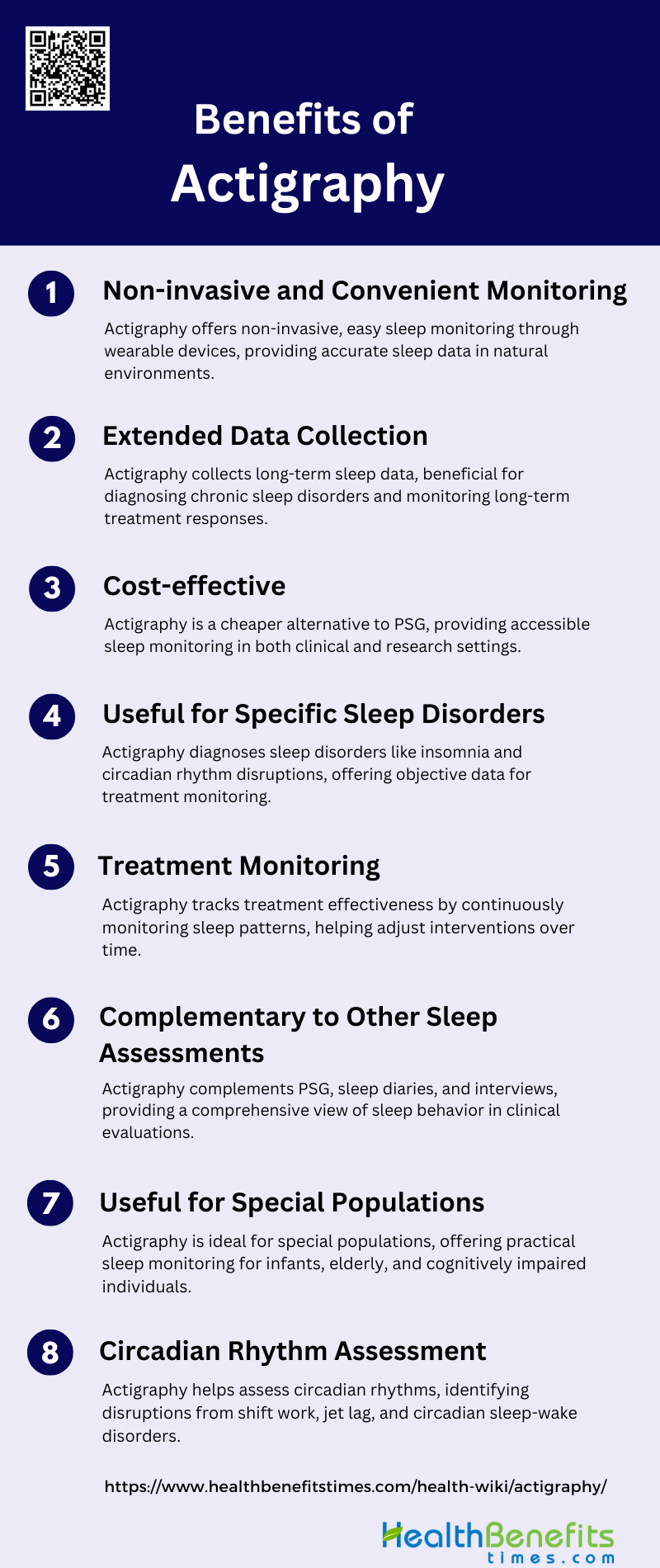
Benefits of Actigraphy
Actigraphy is a versatile and non-invasive method used to monitor sleep and activity patterns over extended periods. It provides valuable insights into sleep disorders and circadian rhythms, making it a cost-effective tool for both clinical and research applications. Below are several key benefits of using actigraphy:
1. Non-invasive and Convenient Monitoring
Actigraphy is a non-invasive and convenient method for monitoring sleep and activity patterns. Unlike polysomnography (PSG), which requires an overnight stay in a sleep lab and the attachment of multiple sensors, actigraphy involves wearing a small device, typically on the wrist, that records movement. This makes it easier for patients to use in their natural sleep environment, thereby providing more accurate and representative data on their sleep habits. The convenience of actigraphy is particularly beneficial for populations who may find traditional sleep studies cumbersome, such as children, the elderly, and individuals with severe psychiatric conditions.
2. Extended Data Collection
One of the significant advantages of actigraphy is its ability to collect data over extended periods. Unlike PSG, which is typically limited to one or two nights, actigraphy can monitor sleep and activity patterns continuously for days, weeks, or even months. This extended data collection allows for a more comprehensive assessment of sleep patterns and circadian rhythms, making it particularly useful for diagnosing chronic sleep disorders and evaluating long-term treatment outcomes. Continuous monitoring is especially beneficial for capturing variations in sleep patterns that may not be evident in short-term studies.
3. Cost-effective
Actigraphy is a cost-effective alternative to more expensive and resource-intensive sleep assessment methods like PSG. The devices are relatively inexpensive, and the data collection process does not require specialized facilities or extensive personnel. This makes actigraphy an accessible option for both clinical and research settings, allowing for broader application in diverse populations. The cost-effectiveness of actigraphy also makes it a viable option for large-scale epidemiological studies and long-term monitoring, which would be prohibitively expensive with traditional methods.
4. Useful for Specific Sleep Disorders
Actigraphy is particularly useful for diagnosing and managing specific sleep disorders, such as insomnia, circadian rhythm sleep-wake disorders, and sleep-related movement disorders. It provides objective data on sleep onset, duration, and efficiency, which are critical for diagnosing these conditions. Actigraphy is also valuable in assessing the impact of treatments for these disorders, offering a reliable outcome measure for evaluating therapeutic efficacy. For example, it can help identify patterns of delayed sleep phase syndrome or advanced sleep phase syndrome, which are often missed in short-term assessments.
5. Treatment Monitoring
Actigraphy is an effective tool for monitoring the progress and efficacy of treatments for various sleep disorders. By providing continuous, objective data on sleep patterns, it allows clinicians to track changes over time and adjust treatment plans accordingly. This is particularly useful for evaluating the impact of behavioral interventions, medications, and other therapeutic approaches. Actigraphy can also help identify any adverse effects of treatments, such as changes in sleep efficiency or increased wakefulness after sleep onset, thereby facilitating more personalized and effective care.
6. Complementary to Other Sleep Assessments
While actigraphy is not a replacement for PSG, it serves as a valuable complementary tool. It provides additional context and data that can enhance the overall assessment of sleep disorders. For instance, actigraphy can be used alongside sleep diaries and clinical interviews to provide a more comprehensive picture of a patient’s sleep patterns and behaviors. It is also useful in situations where PSG is not feasible, such as in-home settings or for long-term monitoring. By combining actigraphy with other assessment methods, clinicians can achieve a more accurate and holistic understanding of sleep disorders.
7. Useful for Special Populations
Actigraphy is particularly beneficial for special populations who may have difficulty with traditional sleep studies. This includes infants, young children, the elderly, and individuals with cognitive impairments or severe psychiatric conditions. For these groups, the non-invasive and unobtrusive nature of actigraphy makes it a more practical and acceptable option. It allows for continuous monitoring in naturalistic settings, providing valuable data that might otherwise be difficult to obtain. This makes actigraphy an essential tool for tailoring sleep interventions to the unique needs of these populations.
8. Circadian Rhythm Assessment
Actigraphy is highly effective for assessing circadian rhythms, which are crucial for understanding various sleep disorders and overall health. By continuously monitoring activity levels, actigraphy can identify disruptions in circadian patterns, such as those caused by shift work, jet lag, or circadian rhythm sleep-wake disorders. This information is invaluable for diagnosing these conditions and developing appropriate treatment plans. Actigraphy can also be used to monitor the effectiveness of interventions aimed at realigning circadian rhythms, such as light therapy or behavioral modifications.
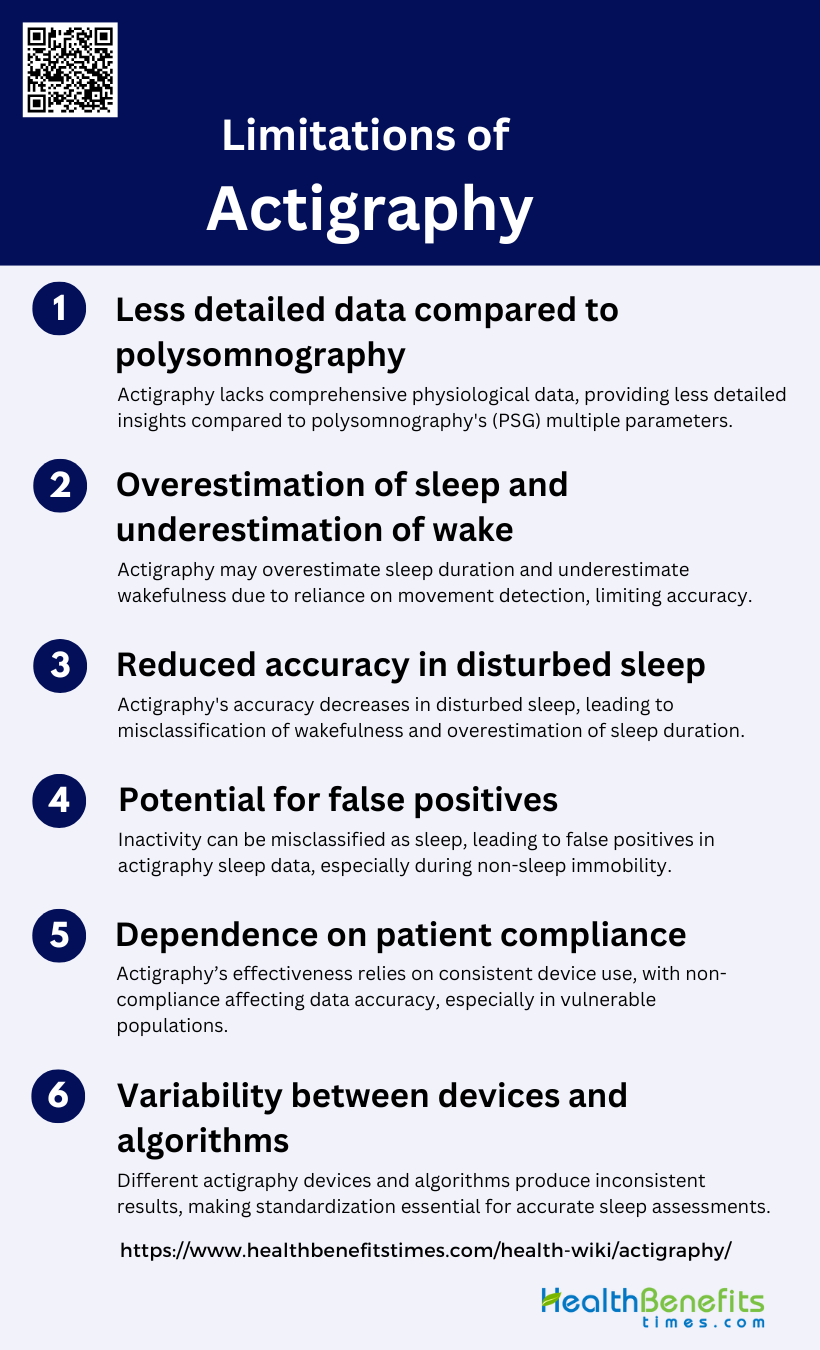
Limitations of Actigraphy
Despite its convenience and non-invasive nature, actigraphy has several limitations that can impact its effectiveness in sleep monitoring. Understanding these limitations is crucial for accurate data interpretation and effective use in clinical practice. Below are some of the key limitations associated with actigraphy.
1. Less detailed data compared to polysomnography
Actigraphy, while useful for long-term sleep monitoring, provides less detailed data compared to polysomnography (PSG). PSG is considered the gold standard for sleep studies as it records multiple physiological parameters such as brain activity (EEG), eye movements (EOG), and muscle activity (EMG), which collectively determine sleep stages and wakefulness. In contrast, actigraphy primarily measures movement, which can lead to less comprehensive data on sleep architecture and quality. This limitation is particularly evident in clinical settings where detailed sleep stage information is crucial for diagnosing sleep disorders.
2. Overestimation of sleep and underestimation of wake
Actigraphy tends to overestimate sleep duration and underestimate wakefulness, especially in conditions with fragmented sleep. This is due to its reliance on movement as a proxy for wakefulness; periods of immobility are often misclassified as sleep. Studies have shown that actigraphy has high sensitivity for detecting sleep but low specificity for detecting wakefulness, leading to an overestimation of total sleep time and sleep efficiency. This discrepancy is particularly problematic in populations with disturbed sleep, such as those with insomnia or sleep apnea.
3. Reduced accuracy in disturbed sleep
The accuracy of actigraphy significantly decreases in individuals with disturbed sleep patterns. For example, in patients with insomnia or those experiencing post-traumatic amnesia, actigraphy often fails to accurately detect wake episodes, leading to an overestimation of sleep duration and efficiency. This reduced accuracy is attributed to the device’s low specificity in detecting wakefulness, especially during long periods of wakefulness within sleep episodes. Consequently, actigraphy may not be reliable for assessing sleep quality in clinical populations with fragmented or disturbed sleep.
4. Potential for false positives
Actigraphy has a potential for false positives, where periods of inactivity are incorrectly classified as sleep. This issue arises because the device primarily relies on movement data to infer sleep states. In situations where an individual is awake but immobile, such as reading or watching TV, actigraphy may inaccurately record these periods as sleep. This limitation can lead to misleading conclusions about an individual’s sleep patterns and overall sleep quality. The potential for false positives underscores the need for complementary methods, such as sleep diaries or PSG, to validate actigraphy data.
5. Dependence on patient compliance
The accuracy of actigraphy is highly dependent on patient compliance. Patients must wear the device consistently and correctly for it to provide reliable data. Non-compliance, such as removing the device during sleep or not wearing it for the recommended duration, can result in incomplete or inaccurate data. This dependence on patient adherence is a significant limitation, particularly in populations that may have difficulty following instructions, such as children, elderly individuals with dementia, or patients with severe sleep disorders. Ensuring compliance is crucial for obtaining valid and reliable actigraphy data.
6. Variability between devices and algorithms
There is considerable variability between different actigraphy devices and the algorithms they use to analyze sleep data. Studies have shown that different devices and scoring algorithms can yield varying results for the same sleep parameters, such as total sleep time and wake after sleep onset. For instance, the Cole-Kripke algorithm may be more sensitive to detecting sleep but less specific for wakefulness compared to the Sadeh algorithm. This variability can complicate the interpretation of actigraphy data and highlights the need for standardization in device calibration and algorithm selection to ensure consistency and accuracy in sleep assessments.
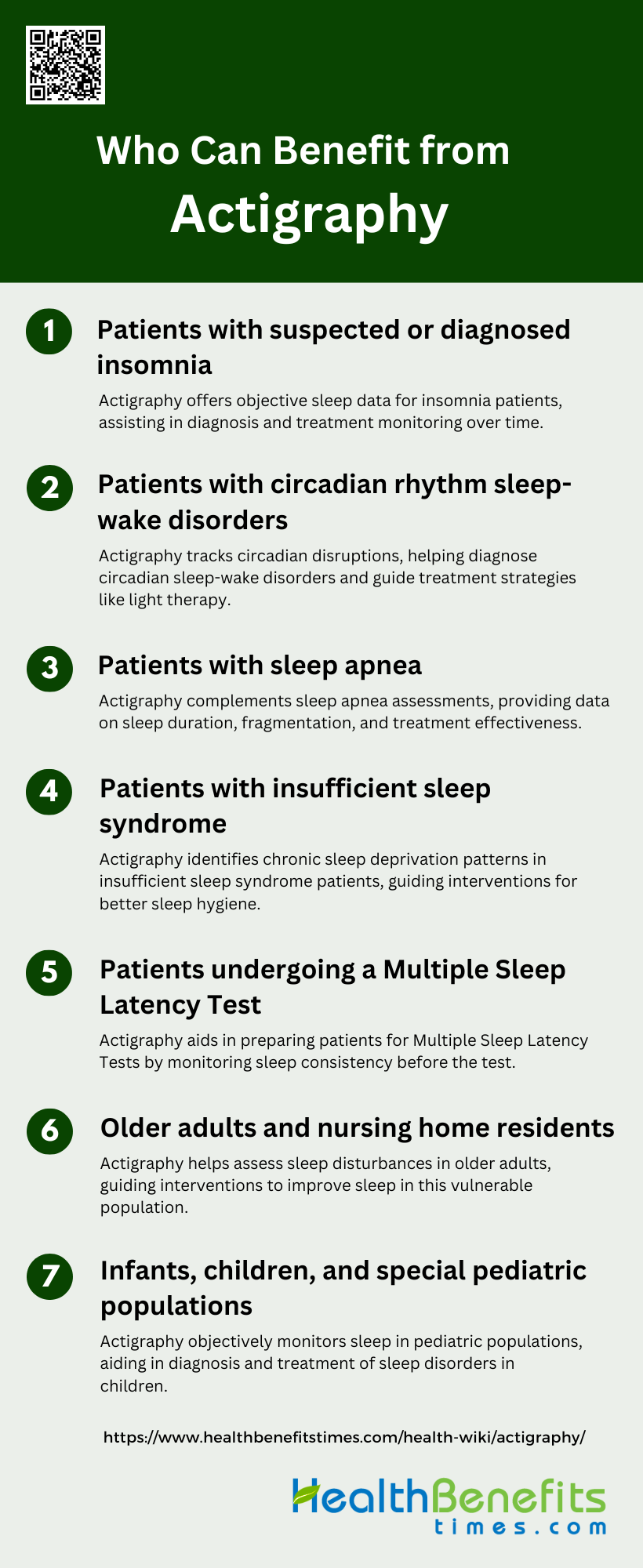
Who Can Benefit from Actigraphy?
Actigraphy provides a non-invasive and effective way to monitor sleep and activity patterns, making it a valuable tool for various patient groups. Its ability to track sleep over extended periods offers insights that are beneficial for both diagnosis and treatment. Below are some of the key populations who can benefit from actigraphy.
1. Patients with suspected or diagnosed insomnia
Actigraphy provides objective data on sleep patterns for individuals with insomnia, offering insights that may differ from self-reported sleep logs. This non-invasive method can help clinicians assess sleep duration, efficiency, and timing, which are crucial for diagnosing and monitoring insomnia. By providing a more accurate picture of sleep-wake cycles over extended periods, actigraphy aids in tailoring treatment plans and evaluating the effectiveness of interventions for insomnia patients.
2. Patients with circadian rhythm sleep-wake disorders
For those with circadian rhythm sleep-wake disorders, actigraphy is particularly valuable in objectively measuring sleep-wake patterns over time. This data helps clinicians identify misalignments between a patient’s internal clock and the external environment. Actigraphy can reveal irregular sleep schedules, delayed or advanced sleep phases, and other circadian disruptions. This information is crucial for diagnosing specific circadian rhythm disorders and guiding appropriate treatment strategies, such as light therapy or chronotherapy.
3. Patients with sleep apnea
While polysomnography remains the gold standard for diagnosing sleep apnea, actigraphy can play a complementary role in assessing sleep patterns in these patients. It can provide valuable information about sleep duration, fragmentation, and overall sleep quality, which are often affected by sleep apnea. Actigraphy may also be useful in monitoring treatment adherence and effectiveness, particularly for patients using continuous positive airway pressure (CPAP) therapy, by tracking changes in sleep patterns over time.
4. Patients with insufficient sleep syndrome
Actigraphy is an effective tool for objectively measuring sleep duration and timing in patients with insufficient sleep syndrome. By continuously recording activity levels over extended periods, it can reveal patterns of chronic sleep deprivation that patients may not be aware of or accurately report. This data helps clinicians differentiate between insufficient sleep and other sleep disorders, guiding appropriate interventions to improve sleep hygiene and duration.
5. Patients undergoing a Multiple Sleep Latency Test
Actigraphy can be a valuable adjunct to the Multiple Sleep Latency Test (MSLT) for patients being evaluated for disorders of central hypersomnolence, such as narcolepsy. By providing objective data on sleep patterns in the days leading up to the MSLT, actigraphy helps ensure that patients have adequate and consistent sleep prior to the test. This information is crucial for accurately interpreting MSLT results and making correct diagnoses of sleep disorders characterized by excessive daytime sleepiness.
6. Older adults and nursing home residents
Actigraphy is particularly useful for assessing sleep patterns in older adults and nursing home residents, who may have difficulty accurately reporting their sleep. It can help identify sleep disturbances common in this population, such as frequent nighttime awakenings or irregular sleep-wake cycles. In nursing home settings, actigraphy can assist in evaluating the prevalence of sleep-disordered breathing and guide interventions to improve sleep quality and overall health in this vulnerable population.
7. Infants, children, and special pediatric populations
Actigraphy is a valuable tool for assessing sleep patterns in pediatric populations, including infants and children with special needs. It provides objective data on sleep duration, timing, and quality, which can be challenging to obtain through traditional methods like sleep diaries, especially in non-verbal or cognitively impaired children. Actigraphy helps clinicians diagnose sleep disorders, evaluate treatment effectiveness, and guide interventions to improve sleep in these young patients, potentially impacting their overall development and well-being.
Types of Actigraphy Devices
Actigraphy devices come in various forms, each offering unique features and capabilities to suit different research and clinical needs. These devices are designed to monitor sleep and activity patterns, providing valuable data for assessing health and wellness. Below are some of the notable actigraphy devices available in the market.
1. Fibion SENS
The Fibion SENS is a sophisticated actigraphy device designed for personalized health and fitness monitoring. It fits well within the Internet of Medical Things (IoMT) paradigm, offering efficient data acquisition and storage capabilities. The device employs a low-level signal encoding method that enhances signal clarity and pattern classification accuracy. This encoding method results in significant improvements in signal-to-noise ratio (SNR) and space savings, making it a highly efficient tool for monitoring daily human activities and health. The Fibion SENS is particularly noted for its ability to retain vital movement information even at lower quantization levels, which contributes to its high pattern recognition accuracy.
2. ActiGraph LEAP
The ActiGraph LEAP is a wrist-worn actigraphy device primarily used for sleep monitoring. It records movements to estimate sleep parameters using specialized algorithms. The device has gained popularity in clinical settings due to its ability to provide objective information on sleep habits in a patient’s natural environment. ActiGraph LEAP is well-validated for estimating nighttime sleep parameters across various age groups, although its accuracy in estimating sleep-onset latency and daytime sleeping is limited. It is particularly useful for documenting sleep patterns before multiple sleep latency tests, evaluating circadian rhythm sleep disorders, and assessing treatment outcomes.
3. Condor ActTrust 2
The Condor ActTrust 2 is an advanced actigraphy device known for its accuracy in measuring light exposure in non-laboratory settings. It is highly portable and has a long battery life, making it ideal for real-world applications. However, the device has a limited illuminance operating range, which can affect its accuracy under different lighting conditions. Studies have shown that the ActTrust 2 tends to underestimate illuminance levels, but correction factors can be applied to improve its accuracy. Despite these limitations, the device performs well in monitoring the temporal patterning of light, which is crucial for evaluating the effects of light intensity on human health and behaviors.
4. GeneActiv
The GeneActiv is a versatile actigraphy device used for both physical activity and light exposure monitoring. It is particularly noted for its performance in measuring light exposure, although it has some limitations in accurately recording high illuminance levels. The device tends to underestimate illuminance, especially under natural sunlight conditions. Despite this, the GeneActiv is effective in monitoring the temporal patterns of light exposure, which is essential for understanding its impact on human health. The device’s portability and long battery life make it suitable for extended monitoring in real-world conditions.
5. MotionWatch 8
The MotionWatch 8 is a widely used actigraphy device in pediatric sleep research. It provides an objective measure of sleep-wake patterns, which is more reliable than parent-reported data. The device is popular for its ability to monitor sleep-wake patterns over extended periods in a child’s natural environment. However, it has been noted for its poor specificity in detecting wake after sleep onset. Despite this limitation, the MotionWatch 8 remains a valuable tool in pediatric sleep research, offering comprehensive data on sleep patterns and aiding in the evaluation of sleep disorders and treatment outcomes.
6. Axivity AX3 and AX6
The Axivity AX3 and AX6 are advanced accelerometers used for measuring 24-hour movement behaviors, including sleep, sedentary behavior, and physical activity. These devices are known for their high feasibility and acceptability in free-living conditions. Studies have shown that the Axivity devices provide substantial agreement in measuring total physical activity and outstanding agreement for sedentary behavior and sleep. However, they are not interchangeable with other devices like the ActiGraph due to clinically relevant biases in the data. The Axivity devices are perceived as more practical for extended wear, making them suitable for long-term monitoring of movement behaviors.
How to Interpret Actigraphy Data
To interpret actigraphy data effectively, it is essential to understand the key parameters and methodologies used in the analysis. Actigraphy involves using a wrist-worn device to monitor movement, which is then analyzed to infer sleep-wake patterns. Key parameters include sleep onset, sleep offset, total sleep time, and sleep efficiency, among others. The data is typically processed using specialized software that applies algorithms to estimate these parameters from the raw movement data. It is crucial to pay attention to the methodological details such as the device model, placement, epoch length, and algorithms used, as these can significantly impact the results. Given the complexity and variability in actigraphy data, working with healthcare professionals is vital. They can provide expert interpretation, ensuring that the data is accurately understood and appropriately applied in clinical or research settings. This collaboration is particularly important for diagnosing and managing sleep disorders, where precise interpretation can guide effective treatment strategies.
FAQs
1. What types of conditions can actigraphy help monitor beyond sleep disorders?
Actigraphy can also be used to monitor conditions related to physical activity, circadian rhythm disturbances, and even anxiety or mood disorders. In some cases, it is used in cardiovascular health research to observe patterns in daily activity that might impact heart health.
2. Can actigraphy differentiate between different stages of sleep?
No, actigraphy primarily measures movement and is not able to differentiate between specific sleep stages, such as REM or deep sleep. For detailed sleep stage analysis, polysomnography (PSG) is required.
3. Is it possible for actigraphy to detect naps during the day?
Yes, actigraphy can detect daytime naps by monitoring periods of inactivity. However, its accuracy for shorter naps may not be as reliable as it is for full sleep cycles during the night.
4. Can actigraphy be used in combination with other health monitoring tools?
Yes, actigraphy is often used alongside other health monitoring tools such as heart rate monitors, sleep diaries, and questionnaires to give a more comprehensive view of an individual’s sleep and activity patterns.
5. How accurate is actigraphy compared to other sleep assessment methods?
While actigraphy is effective for monitoring sleep over long periods, it is less accurate than polysomnography (PSG), especially in distinguishing between wakefulness and sleep, and cannot provide detailed data on sleep stages.
6. Are there any risks or side effects associated with wearing an actigraphy device?
Actigraphy devices are generally safe and non-invasive. The most common issues are mild discomfort from wearing the device or skin irritation in rare cases.
7. Can actigraphy data be affected by environmental factors or user behavior?
Yes, factors such as the user’s physical activity, the type of environment (e.g., lighting conditions), and how consistently the device is worn can influence the data collected. Periods of immobility when awake, like sitting still or reading, might be incorrectly classified as sleep.
8. How long can an actigraphy device be worn continuously?
Most actigraphy devices can be worn continuously for days, weeks, or even months, depending on the device’s battery life and data storage capacity. This makes it particularly useful for long-term monitoring.
9. What should I do if I forget to wear the actigraphy device?
It’s important to wear the device consistently for accurate results. However, missing a few hours or a day may not drastically affect long-term data collection. Consult your healthcare provider if multiple sessions are missed.
10. How does actigraphy help in understanding treatment effects?
By monitoring sleep patterns and circadian rhythms over time, actigraphy can track changes in response to treatments like medications, light therapy, or cognitive behavioral therapy, helping healthcare providers assess the effectiveness of interventions.